Abstract
Condylar hyperplasia (CH) is a bone disease characterized by the increased development of one mandibular condyle. It regularly presents as an active growth with facial asymmetry generally without pain. Statistically it affects more women in adolescence, although it does not discriminate by age or gender. Its best-known consequence is asymmetric facial deformity (AFD), which combined with alteration of the dental occlusion with unilateral crossbite or open bite. It is not known when CH begins and how long it lasts; diagnostic examinations are described and are efficient in some research about diagnosis. Protocol treatment is not well studie and depends on the criteria described in this paper. The aim of this research is to provide up-to-date information about the diagnosis of this disease and to analyze the treatment protocol, visualizing the CH and AFD presented.
Keywords: Condylar hyperplasia, facial asymmetry, TMJ
Introduction
Excessive unilateral condylar growth is a well-known phenomenon that has been previously described [1]. Condylar hyperplasia (CH) can be defined as the excessive growth of one condyle over the contralateral, causing an increase in bone mass of varying degree in instances where the subject’s growth has decreased or ceased [2].
Norman & Painter [1] conducted a historical review of CH and in 1980 published a series of cases that were previously described by Robert Adams in 1836, George Humphry in 1856 and others that demonstrate knowledge of the disease, emphasizing the facial deformity and chin displacement as the main characteristics.
The diagnosis of this pathology is initially made with facial analysis and imaging; the patient frequently consults for dental alterations, motivated by the use of corrective orthodontic devices [3]. Asymmetric facial deformities (AFD) and malocclusion are a clear consequence of CH. Generally, there is no pain associated with the affected joint, although joint noises linked to CH and deviation of the mouth opening towards the contralateral side have been described [2].
From the point of view of facial analysis, the patient with CH and AFD are initially evaluated by means of a central line drawn up from the tip of the glabella, passing through the pronasal point to the end of the chin, where both hemifacial areas are identified in order to ascertain the difference in size and position between them [4]. There is generally a deviation of the chin towards the contralateral side of the condyle with CH [5]. From the dental point of view, the difference between interincisive midlines and the unilateral posterior inverted occlusion or the unilateral posterior open bite also enable the presence of the disease to be established [6].
Etiology and diagnosis of CH
TMJ and specifically the condyle are responsible for most postnatal facial asymmetries; the pathologies are known as osteochondromas, condylar resorptions, infection-related growth deficiencies, trauma or CH [3]. One way to recognize facial asymmetries caused by condylar growth alterations in prenatal or postnatal origin is that the latter cranial asymmetries are not observed [7]; cranial asymmetry deformity is caused by alterations before 5 years of age, when he cranial base takes to form completely [8], placing CH in the postnatal category.
CH has an unknown etiology and is characterized by a progressive and independent growth, causing greater bone volume of one condyle over the other side. It generally appears in subjects in the growth phase, mainly in adolescence [3]. A systematic review by Raijmakers [9] assessed 10 articles published with a total of 275 patients diagnosed with CH; in the sample a statistically significant tendency was observed that women present with CH more frequently with 0.64% more than men.
In terms of age and given that etiology is definitively unknown, it has not been possible to define an absolute age of presentation [2,3,9]. It is estimated that subjects in adolescence or young adults can present with the active pathology, although it has also been seen that subjects over 50 can also exhibit CH in progress [3]. With the current information in the literature, it is not possible to define the date at which CH begins or ends.
Nitzan [3] and Raijmakers [9] indicated that the severity of the asymmetry was also statistically associated with age and gender; the type of condylar deformity (morphological characteristics of the condyle) was not related to the type of asymmetry [6], presenting horizontal in 53%, vertical in 31% and combined in 16%. In the group of 36 patients of Villanueva-Alcojol [2] 66.7% presented cross-sectional pathology, 22.2% vertical and 11.1% was a combination of the two; as a result, the highest incidence of the cross-sectional pathologies is observed.
Bone scintigram and diagnostic methods
Although the diagnosis of CH is essentially clinical, there are supporting studies that determine the activity and morphology of the condyle affected. Without a doubt, computerized tomography (CT) has contributed to establishing the pathology and condylar morphology (comparing both condyles), making it possible to recognize and classify the different degrees of the disease [10] (Table 1); in the tomographic images of condyles with CH, limited cortical areas are observable in the upper pole, characteristic of zones with active bone metabolism [11] (Figure 1). Before CT, radiographs were protocoled how serial image in follow-up, which enabled the size and shape of the condyle to be compared at 6-month intervals to determine whether the CH was growing or if this growth had stopped [12].
Table 1.
Characteristics of some relevant studies performed on patients with condylar hyperplasia (CH)
| Authors | Aim | n | Age (years) | Female/Male | Diagnosis | Treatment | Follow-up (years) |
|---|---|---|---|---|---|---|---|
| Hampf, 1985 [39] | Analysis of treatment of patients with CH | 35 (in active CH in 9 cases) | 15.6 (7-30 years) | 24/11 | -Clinical | Condylar surgery (34 cases) with other osteotomies (mandibula. maxilla) and/or extractions | 0.5 (0.1-3) |
| 5 patients under 15 years | -Radiography | ||||||
| -Scintigram (23 cases) | |||||||
| Slootweg and Müller 1986 [20] | Clinical and pathological analysis of patients with CH | 22 | 24.5 (14-59 years) | 16/6 | -Clinical | Condylectomy and maxillary and mandibular osteotomies | - |
| -Radiography | |||||||
| -Scintigram (12 cases) | |||||||
| Iannetti, 1989 [34] | Analysis of treatment of patients with CH | 12 | 23.5 | - | -Clinical | Orthognatic surgery | 4.6 (3-8) |
| -Radiography | |||||||
| Gray, 1990 [19] | Study relation between histology and scintigram | 20 | 25.8 (15-55 years) | 15/5 | -Clinical | Condylectomy | - |
| -Radiography | |||||||
| -Scintigram | |||||||
| Mutoh, 1991 [10] | Analysis of condylar morphology with CT | 6 | 15-20 | 1/5 | -Clinical | - | - |
| -Radiography | |||||||
| -CT | |||||||
| Motamedi, 1996 [31] | Analysis of treatment of patients with CH | 13 | 25.8 (19-37 years) | 1/12 | -Clinical | Orthognatic surgery with unilateral (6 cases) or bilateral (7 cases) mandibular osteotomy | 4.5 (0.7-10) |
| -Radiography | |||||||
| -Scintigram in some cases | |||||||
| Wolford, 2002 [33] | Comparison of treatments in patients with CH | 25 | 16.7 (13-24 years) | 12/13 | -Clinical | High condylectomy with disc reposition and simultaneous orthognatic surgery | 5.3 (2.8-16.9) |
| -13 unilateral | -Serialized radiographs with superposition | ||||||
| -12 bilateral | |||||||
| Eslami, 2003 [21] | Comparison of normal and hyperplastic condyles through histological methods | 9 | 20.4 | - | -Scintigram | High condylectomy | - |
| Pripatnanont, 2005 [14] | Evaluation of SPECT in CH diagnosis. | 21 | 12-46 | 7/14 | -Clinical | - | - |
| -Radiography | |||||||
| -Dental models | |||||||
| -Scintigram | |||||||
| Saridin, 2007 [15] | Analysis of scintigram evaluation methods | 20 | 21.5 | 12/8 | -Clinical | - | - |
| -Radiography | |||||||
| -Scintigram | |||||||
| Lippold, 2007 [23] | Analysis of treatment of patients with CH | 6 | 27±3 | 4/2 | -Clinical | Condylectomy together with orthognatic surgery | 3.1±1.2 |
| -Radiographic | |||||||
| -Scintigram | |||||||
| Nitzan, 2008 [3] | Analysis of condylar morphology and characteristics of patients with CH | 61 | 27.8 (11-80 años) | 46/15 | -Clinical | - | - |
| -Panoramic and lateral radiography | |||||||
| -Scintigram at presentation and at 6 months | |||||||
| Saridin, 2010 [13] | Analysis of mandibular function after condylectomy | 32 | 26.7 (19-48 años) | 18/15 | -Scintigram | High condylectomy | 4.3 |
| Villanueva-Alcojol, 2010 [2] | Evaluation of diagnosis and treatment of patients with CH | 36 | 22.7 años (11-42 años) | 11/25 | -Clinical | High condylectomy and orthognatic surgery in 6 cases | 4.3 |
| -Radiographic | |||||||
| SPECT (24 cases) | |||||||
| Brusati, 2010 [38] | Evaluation of the functional TMJ results before and after high condylectomy | 15 | 22 (12-42 años) | - | -Clinical | High condylectomy with simultaneous orthognatic surgery in some cases (does not indicate how many) | 4.5 (1-8) |
| -Dental models | |||||||
| -Panoramic, posteroanterior and lateral radiography | |||||||
| -Scintigram | |||||||
| Jones and Tier 2011 [25] | Evaluation of surgical treatment of patients with CH | 16 | - | 15/1 | -Clinical | High condylectomy and simultaneous orthognatic surgery | - |
| -Dental models | |||||||
| -Panoramic, lateral and posteroanterior radiography | |||||||
| -Scintigram |
Research obtained from database in english and spanish literature between january, 1980 and january, 2012.
Figure 1.
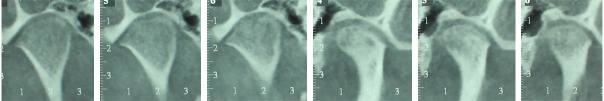
Cone beam CT image comparing different serial sections at a thickness of 1 mm of the condyle from right to left. The right condyle exhibits active growth and a greater volume than its contrateral.
Nevertheless, it is the nuclear medicine studies that are most associated with the diagnosis of CH; these consist of an exploration of the bone structure that can detect the bone metabolism and its activity. To do this, Technetium-99m is administered with methylene diphosphonate, which is absorbed by hydroxyapatite crystals and calcium from the bone tissue so that the fixation intensity is proportional to the degree of osteoblast activity; the examination that obtains the scanned bone is called “single photon emission computed tomography” (SPECT) and it determines the percentage of absorption by the condyle quantitatively, by comparing it with the contralateral side [13]. 0 to 5% differences in capture are observed between the condyles in healthy subjects; differences greater than 10% (pixel count) between the two condyles have been considered as active unilateral growth, establishing the presence of CH on the affected side; these are related positively to increases in the patient’s dental and facial asymmetry [14] (Figure 2A and 2B).
Figure 2.
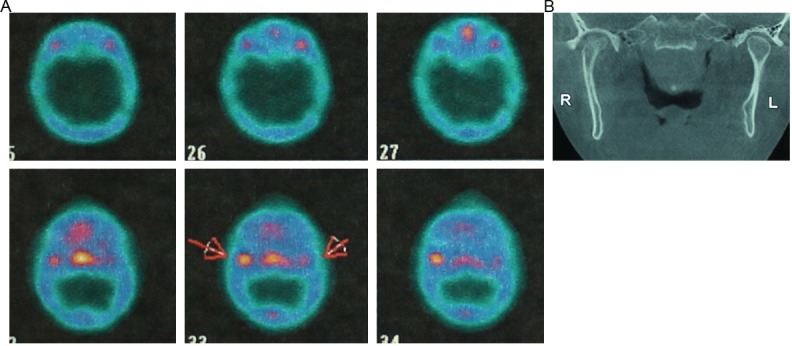
A: Image obtained by SPECT where a greater capture of the isotope is observed in the left condyle, represented by a more intense red. B: Cone beam CT image showing differences in condylar volume in acoording to the SPECT image.
No other quantitative method has shown the same efficiency as the results of the comparison between condyles using SPECT [15,16]. Other fluids have also been studied to determine the active growth of a condyle [17], which, using the same technique, are showing good results.
Histological characteristics of CH
Histologically 4 layers have been characterized as being present in condylar morphology: 1) connective tissue (fibrous joint layer), 2) undifferentiated mesenchymal layer (proliferative), 3) transitional layer and 4) hypertrophic cartilage layer [18].
In 20 condyles of patients with positive SPECT for CH, Gray [19] demonstrated the presence of a fibrous layer approximately 0.31 mm, a layer of undifferentiated mesenchymal cells with an average of 0.29 mm; the layer of hypertrophic cartilage was on average 0.52 mm. In addition, cartilaginous islands were observed inside the bone tissue, which was related to the level of capture that the affected condyle displayed in the SPECT, a situation already identified by Slootweg & Müller [20]. They also described a probable link between the origin of the pathology and the age group of the patient; thus, according to Sllotweg & Müller [20], in adolescence there is an idiopathic form and in adulthood a reactive consequence to some previous pathology or trauma. What is certain is that no matter the patient’s age, CH does not have a described cause and is possibly linked to situations such as trauma, infection or other localized alteration.
Another contribution by Slootweg & Müller [20] was the creation of a histological classification where they described 4 types of CH, with type I being the slightest and type IV being the most serious in terms of condylar size and tissue invasion. The classification is based on the amount of condylar bone structure involved and cartilaginous growth. Villanueva-Alcojol [2] described 36 patients, of which 44.4% presented with type I, 16.7% type II and 38.9% type III. Nevertheless, it was not possible to find any link between histological finding, SPECT finding and the patient’s age [2].
Eslami [21] indicated that significant differences were observed in the layer of hyperplastic cartilage in hyperplastic condyles (located in the upper pole of the condyle), whereas no differences were observed between the other layers studied in healthy condyles.
Analysis performed with AgNOR (Argyrophilic Nuclear Organizer Region) has endeavored to quantify CH; Fariña [22] reported an absence of correlation between the AgNOR results and the presence of CH, whereas Eslami [21] indicated that AgNOR was associated with the classification of the type of hyperplasia proposed by Slootweg & Müller [20], demonstrating a significant correlation. Lippold [23], in an interesting investigation, found a direct link between the histological findings with signs of arthritis and the greatest SPECT capture, which would set the basis for a condylar osteotomy of the upper segment of the condyle to limit its anomalous growth.
Facial asymmetry as a result of CH
CH determines the existence of a facial asymmetry [3]. Obwegeser & Makek [6] classified AFD in three groups: 1) vertical asymmetries, where there is no occlusal alteration of the midline but a vertical growth of the mandibular ramus is observed with a posterior open bite on the affected side, 2) horizontal asymmetries, where there is an alteration between the interincisive midlines and a cross-sectional displacement of one side of the jaw towards the contralateral side and 3) a combination of the two. Elsewhere, Hwang [24] defined 5 groups of patients with AFD with different degrees of alteration; of 8 different characteristics proposed to separate each group, only 3 criteria established clear differences in each group: 1) deviation of the chin, 2) discrepancy between dental apical midlines and 3) the vertical difference between the right and left gonion point (position of the angle of the mandible). These points are clearly linked to the initial proposal by Obwegeser & Makek [6] vertically and horizontally (Figure 3A and 3B).
Figure 3.

A: Facial characteristics of a patient with active CH which shows the deviation of the chin towards the contralateral side, differences in the right and left hemifacial and uneven position of the bilateral gonion, B: Dental characteristics of the patient with a posterior unilateral crossbite and deviation of the lower midline 5 mm to the right.
CH involves unilateral condylar growth, which determines not only the growth of the bone structure of the affected side, but also a large part of the soft tissues of the sector including ligaments, muscles and the bone structures related to this mandibular position, which determines the presence of total facial asymmetry together to the technical difficulty for surgical correcting of residual AFD [25].
The dental and occlusal analyses also makes it possible to define facial asymmetries; maxillary cant (deviation of the occlusal plane being higher or lower on one side than the other) is also associated with facial asymmetries [26]; in the detection of this alteration, the degree of the cant is more important than the experience of the observer, who not being a trained clinician, may perceive facial asymmetries associated with the maxillary cant; 4° of occlusal cants are detected by 90% of the observers, whereas 3° of cants are detected by almost 50% of the observers [27].
For other hand, Hwang [26] indicated that the position of the chin and the cant of the occlusal plane influence the position of the lip significantly, showing it to be asymmetrical when the indicated points differ from the midline. Kwon [28] also reported that in patients with asymmetries, differences in the muscular architecture have been identified in relation to the medial pterygoid muscle due to the decrease or increase of the distance from the origin and insertion of this muscle. Relatively vertical muscles like the masseter did not present greater differences in the origin and insertion of the different sides of the asymmetrical patient. The angulation of the muscle from the axial axis is one of the reasons that explain this difference in the medial pterygoid muscle.
Tratment oportunity
Based on the existing information, two different but related clinical situations can be defined as cause - effect: on the one hand CH and its progressive growth and on the other hand AFD as a consequence of CH; the two elements can be approached jointly or separately, depending essentially on the patient’s age and the activity or inactivity of the CH [2]. Thus, the proposed treatment options range from the simplest to the most complex surgical and non-surgical procedures [29] (Table 1).
Interestingly, the study by Naini [30] concluded that as the degree of asymmetry increases, the subjects determine a greater need for surgery that repairs esthetics and function, indicating that when the chin asymmetry deviates 10 mm from the midline, there is a high demand to correct it surgically; this demand decreases in proportion to the increase in the patient’s age and to the decrease in the perception of facial esthetics. It was also concluded that with just 5 mm deviation of the chin from the midline, there is already a perception by any observer that there is facial asymmetry.
In 1996, was presented a series of patients with CH diagnosed using clinical and radiographic studies (without SPECT or CT analysis) [31]; the patients were treated with unilateral mandibular osteotomy (the affected side), performing a mandibular rotation at the expense of the healthy condyle. This technique was complemented in some cases with a LeFort I osteotomy. In the event of inadequate follow-up, the main doubt in these patients lies in the stability of the condyle with CH and in the fact that the rotation towards the medial side of the “healthy” condyle can be altered and involved in its movement, since the disc and muscular insertions might present a change in its orientation, which could generate functional deficiencies in the TMJ and limited postoperative stability of the executed movement.
Another treatment option was presented by Choung & Nam [32], who reported a series of 4 patients with CH, where a vertical and sagittal intraoral osteotomy of the ramus was performed, enabling the complete extraction of the condylar segment and the remodeling of condyle with drills. This was then re-installed in the articular fossa and stabilized with osteosynthesis plates. According to the authors, in a follow-up of 3 years, no accentuated resorption of the condyle or any type of necrosis was observed, with total functionality.
The group of patients of Villanueva-Alcojol [2] presented a mean age of 22.7 years with a range between 11 and 42. In all the patients a high condylectomy was performed (4 mm to 5 mm from the upper pole of the condyle) (Figure 4) and in only 6 of these was performed a second procedure with orthognatic surgery to correct the resulting facial defect. The 5 mm resection of the upper pole of the condyle limits the progressive growth that CH presents [23,33].
Figure 4.
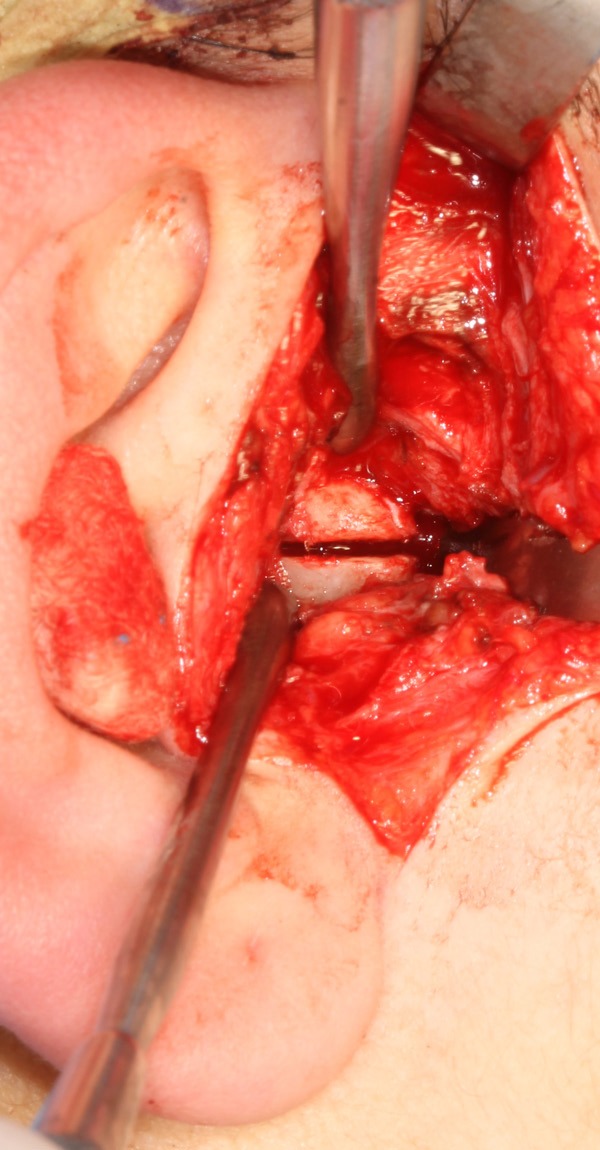
Intraoperative image of the condylectomy process performed with ultrasonic systems through an endaural approach.
The series of patients in the study by Wolford [33] showed that the high condylectomy in conjunction with orthognatic surgery was acceptable to treat the functional and esthetic problems. In addition, it indicated that performing orthognatic surgery without condylar treatment would not limit subsequent condylar growth, and that recurrence and new surgical procedures were possible. Jones & Tier [25] reported a study where 17 patients were operated on, treating the condylar pathology via a high condylectomy of the affected side with simultaneous orthognatic surgery. The authors used the term “satisfactory” to define the postoperative subjective results in the medium follow-up.
One of the few studies that does not advocate the high condylectomy as a treatment was conducted by Iannetti [34] (with deficiencies in their system for diagnosis since it does not have the necessary complementary examinations); the authors presented a series of 12 patients with facial asymmetry linked to CH diagnosed clinically and radiographically. The patients presented with an average age of 23.5 years and bimaxillary surgery was performed with genioplasty or mandibular basal osteotomy in almost all cases.
Yamashita [35] treated 17 patients with facial asymmetry associated with CH that had ceased (evaluated with multiple SPECT images), where there was a vertical difference in the labial commissure of 3.48 mm; after the orthognatic surgery the vertical difference was 0.46 mm. The inclination of the labial plane was reduced from 2.7° to 0.5°, which was accompanied by the chin reposition that went from 6 mm deviation to be centered to just 0.4 mm deviation, appearing clinically symmetrical. Ko [36] indicated that in their sample of 27 patients with facial asymmetries, most presented with a class III dentofacial deformity and were treated with bimaxillary orthognatic surgery to correct the occlusal cant, the axial tooth position and the midline of the chin. Correction of the maxillary cant was with slight drop on the side that presented the vertical deficiency (using LeFort I osteotomy), providing surgical postoperative stability.
The studies that deal with CH and that have defined therapeutic aspects of the disease can be observed in Table 2, where the surgical criterion of the condylectomy in cases of active CH is clearly defined. After these considerations, the treatment options supported by the literature are: 1) high condylectomy of the condyle with CH, 2) high condylectomy of the condyle with CH and bimaxillary orthognatic surgery, 3) orthognatic surgery of the residual facial deformity or 4) cosmetic procedures associated with orthodontic compensation. In light of the variability in protocols, our service has adopted the treatment criteria described in Tables 2 and 3. Together with the proposed protocol, some analysis criteria must be included in order to determine the course of action in each case, these being 1) level of facial asymmetry, 2) psycho-social implications of the facial alteration, 3) presence of pain and functional alterations of the TMJ with CH and the contralateral and 4) masticatory deficiency due to malocclusion. These criteria could cause a modification in the proposed treatment options.
Table 2.
Treatment protocols used on patients with CH using SPECT result for treatment decision*
| Patient | SPECT | Treatment options |
|---|---|---|
| Patient under 18 years | 1st-positive | -Follow-up to a 3rd SPECT |
| 2nd-positive | -High condylectomy | |
| -High condylectomy + compensatory orthodontics + surgical cosmetic camouflage after 18 years of age. | ||
| -High condylectomy and wait until 18 years of age to perform orthognatic surgery. | ||
| Patient over 18 years | 1st-positive | -High condylectomy + compensatory orthodontics + surgical cosmetic camouflage |
| 2nd-positive | -High condylectomy + orthognatic surgery | |
| Patient over 18 years | negative | -Compensatory orthodontics + surgical cosmetic camouflage |
| -Orthognatic surgery |
Considering the patient’s motivation, level of facial asymmetry, alterations in dental function and functional alterations and psicological condition.
Table 3.
Summary of 12 publications oriented to treatment of the patient with CH
| Treatment scheme | N° publications | N° patients |
|---|---|---|
| High condylectomy | 5 | 112 |
| High condylectomy + orthognatic surgery (in the same procedure) | 5 | 104 |
| Orthognatic surgery | 2 | 25 |
The postoperative facial condition (proportions and symmetry) of patient is difficult to visualize preoperatively. It is highly complex to solve a facial asymmetry integrally in such a way that the correction with some types of osteotomy and the installation of facial implants collaborates with the cosmetic camouflage of the case [25].
Another therapeutic condition has been reported by some professionals who have suggested patient follow-up until the CH is inactive; this follow-up is done with SPECT. When the SPECT appears inactive would be the time to select the type of treatment [37]. This conditioning involves difficulties such as: 1) the condyle and the altered hemifacial sector continue to grow, increasing the AFD, 2) the surgical correction of the residual AFD is more complex, 3) requires continual SPECT, 4) the point at which the CH will cease is unknown.
TMJ function after the condylectomy
Limited studies report postoperative function in patients who have undergone a condylectomy. From the functional point of view, the mandibular dynamic is maintained with no significant changes when the high condylectomy is performed [23,38]. In a follow-up study of 15 patients undergoing a high condylectomy that presented no significant differences between the pre- and postoperative stages in either the objective or the subjective evaluations, Brusati [38] determined excellent function in 53.3%, only good in 40% owing to the partially reduced laterality of the side affected, whereas in one patient (6.7%) a function characterized as sufficient was observed because this patient abandoned the kinesic treatment that is the protocol for patients in the postoperative stage. Saridin [13] observed that patients undergoing condylectomy for CH presented no differences in disc displacement or myofacial pain when compared to patients without CH; however, the patients who underwent surgery had higher rates of TMJ osteoarthritis, which could be linked either to the nature of the disease or to the surgical procedure. Nevertheless, this clinical condition did not affect the daily activities of the patients studied.
Conclusion
CH is defined in terms of presentation and consequences. The treatment options have been only partially defined because the long-term functional condition needs to be specified. Research oriented to know the causes of CH is necessary for better diagnosis and treatment. If the onset and duration could be defined, CH could be treated more safely.
Disclosure of conflict of interest
The authors declare that they have no competing financial interests.
References
- 1.Norman J, Painter D. Hyperplasia of the mandibular condyle. J Maxillofac Surg. 1980;8:161–175. [PubMed] [Google Scholar]
- 2.Villanueva-Alcojol L, Monje F, González-García R. Hyperplasia of the mandibular condyle: clinical, histopathologic, and treatment considerations in a series of 36 patients. J Oral Maxillofac Surg. 2011;69:447–455. doi: 10.1016/j.joms.2010.04.025. [DOI] [PubMed] [Google Scholar]
- 3.Nitzan D, Katsnelson A, Bermanis I, Brin I, Casap N. The clinical characteristics of condylar hiperplasia: experience with 61 paients. J Oral Maxillofac Surg. 2008;66:312–318. doi: 10.1016/j.joms.2007.08.046. [DOI] [PubMed] [Google Scholar]
- 4.Vig KD, Ellis E 3rd. Diagnosis and treatment planning for the surgical-orthodontic patient. Dent Clin N Am. 1990;34:361–384. [PubMed] [Google Scholar]
- 5.Wolford LM, Morales-Ryan C, García-Morales P, Perez D. Surgical management of mandibular condylar hiperplasia type 1. Proc (Bayl Univ Med Cent) 2009;22:321–329. doi: 10.1080/08998280.2009.11928546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Obwegeser H, Makek M. Hemimandibular hiperplasia – Hemimandibular elongation. J Maxillofac Surg. 1986;14:183–208. doi: 10.1016/s0301-0503(86)80290-9. [DOI] [PubMed] [Google Scholar]
- 7.Baek SH, Cho IS, Chang YI, Kim MJ. Skeletodental factors affecting chin point deviation in female patients with class III malocclusion and facial asymmetry: a three-dimensional analysis using computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:628–639. doi: 10.1016/j.tripleo.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 8.Sgouros S, Natarajan K, Hockely AD, Goldin JH, Wake M. Skull base growth in childhood. Pediatr Neurosurg. 1993;31:259–268. doi: 10.1159/000028873. [DOI] [PubMed] [Google Scholar]
- 9.Raijmakers P, Karssemakers L, Tuinzing D. Female predominance and effect of gender on unilateral condylar hiperplasia: a review and meta-analysis. J Oral Maxillofac Surg. 2012;70:e72–6. doi: 10.1016/j.joms.2011.05.026. [DOI] [PubMed] [Google Scholar]
- 10.Mutoh Y, Ohashi Y, Uchiyama N, Terada K, Hanada K, Sasaki F. Three dimensional analysis of condylar hiperplasia with computed tomography. J Craniomaxillofac Surg. 1991;19:49–55. doi: 10.1016/s1010-5182(05)80606-7. [DOI] [PubMed] [Google Scholar]
- 11.Nah KS. Condylar bon in patients with temporomandibular disorders: a CBCT study. Imaging Sci Dent. 2012;42:249–53. doi: 10.5624/isd.2012.42.4.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hovinga J, Kraal ER, Roorda LAM. Difficulties in and indications for the treatment of facial asymmetry. Int J Oral Surg. 1974;3:234–238. doi: 10.1016/s0300-9785(74)80053-0. [DOI] [PubMed] [Google Scholar]
- 13.Saridin C, Gilijamse M, Kuik D, te Veldhuis E, Tuinzing D, Lobbezoo F, Becking A. Evaluation of temporomandibular function after high partial condilectomy because of unilateral condylar hyperactivity. J Oral Maxillofac Surg. 2010;68:1094–1099. doi: 10.1016/j.joms.2009.09.105. [DOI] [PubMed] [Google Scholar]
- 14.Pripatnanont P, Vittayakittipong P, Markmanee U, Thongmak S, Yipintsol T. The use of SPECT to evaluate growth cessation of the mandible in unilateral condylar hiperplasia. Int J Oral Maxillofac Surg. 2005;34:364–368. doi: 10.1016/j.ijom.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 15.Saridin CP, Raijmakers P, Becking AG. Quantitative analysis of planar bone scintigraphy in patients with unilateral condylar hiperplasia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:259–263. doi: 10.1016/j.tripleo.2006.08.018. [DOI] [PubMed] [Google Scholar]
- 16.Saridin CP, Raijmakers PG, Al Shamma S, Tuinzing DB, Becking AG. Comparison of different analytical methods used for analyzing SPECT scans of patients with unilateral condylar hyperactivity. Int J Oral Maxillofac Surg. 2009;38:942–946. doi: 10.1016/j.ijom.2009.04.019. [DOI] [PubMed] [Google Scholar]
- 17.Laverick S, Bounds G, Wong WL. [18F] –fluoride positrón emission tomography for imaging condylar hiperplasia. Br J Oral Maxillofac Surg. 2009;47:196–199. doi: 10.1016/j.bjoms.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 18.Hansson T, Oberg T, Carlsson GE, Kopp S. Thickness of the soft tissue layers and the articular disk in the temporomandibular joint. Acta Odontol Scand. 1977;35:77–83. doi: 10.3109/00016357709055993. [DOI] [PubMed] [Google Scholar]
- 19.Gray RJM, Sloan P, Quayle AA, Carter DH. Histopathological and scintigraphic features of condylar hiperplasia. Int J Oral Maxillofac Surg. 1990;19:65–71. doi: 10.1016/s0901-5027(05)80196-1. [DOI] [PubMed] [Google Scholar]
- 20.Slootweg P, Müller H. Condylar hiperplasia. A clínico-pathological analysis of 22 cases. J Maxillofac Surg. 1986;14:209–214. doi: 10.1016/s0301-0503(86)80291-0. [DOI] [PubMed] [Google Scholar]
- 21.Eslami B, Behnia H, Javadi H, Khiabani S, Shoja Saffar A. Histopathologic comparison of normal and hyperplastic condyles. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:711–717. doi: 10.1016/s1079-2104(03)00379-2. [DOI] [PubMed] [Google Scholar]
- 22.Fariña R, Becar M, Plaza C, Espinoza I, Franco ME. Correlation between single photon emission computed tomography, AgNOR count, and histomorphologic features in patients with active mandibular condylar hiperplasia. J Oral Maxillofac Surg. 2011;69:356–361. doi: 10.1016/j.joms.2010.06.184. [DOI] [PubMed] [Google Scholar]
- 23.Lippold C, Kruse-Losler B, Danesh G, Joos U, Meyer U. Treatment of hemimandibular hiperplasia: the biological basis of condylectomy. Br J Oral Maxillofac Surg. 2007;45:353–360. doi: 10.1016/j.bjoms.2006.10.011. [DOI] [PubMed] [Google Scholar]
- 24.Hwang HS, Youn IS, Lee KH, Lim HJ. Classification of facial asymmetry by cluster analysis. Am J Orthod Dentofacial Orthop. 2007;132:279, e1–6. doi: 10.1016/j.ajodo.2007.01.017. [DOI] [PubMed] [Google Scholar]
- 25.Jones RHB, Tier G. Correction of facial asymmetry as a result of unilateral condylar hiperplasia. J Oral Maxillofac Surg. 2012;70:1413–1425. doi: 10.1016/j.joms.2011.03.047. [DOI] [PubMed] [Google Scholar]
- 26.Hwang HS, Min YS, Lee SC, Sun MK, Lim HS. Change of lip-line cant after 1-jaw orthognathic surgery in patients with mandibular asymmetry. Am J Orthod Dentofacial Orthop. 2009;136:564–569. doi: 10.1016/j.ajodo.2007.10.060. [DOI] [PubMed] [Google Scholar]
- 27.Padwa BL, Kaiser MO, Kaban LB. Occlusal cant in the frontal plane as a reflection of facial asymmetry. J Oral Maxillofac Surg. 1997;55:811–816. doi: 10.1016/s0278-2391(97)90338-4. [DOI] [PubMed] [Google Scholar]
- 28.Kwon TG, Lee KH, Park HS, Ryoo HM, Kim HJ, Lee SH. Relationship between the masticatory muscles and mandibular skeleton in mandibular prognathism with and without asymmetry. J Oral Maxillofac Surg. 2007;65:1538–1543. doi: 10.1016/j.joms.2006.09.024. [DOI] [PubMed] [Google Scholar]
- 29.Kahnberg KE. Correction of maxilofacial asymmetry using orthognathic surgical methods. J Craniomaxillofac Surg. 1997;25:254–260. doi: 10.1016/s1010-5182(97)80062-5. [DOI] [PubMed] [Google Scholar]
- 30.Naini F, Donaldson AN, McDonald F, Cobourne M. Assessing the influence of asymmetry affecting the mandible and chin point on perceived attractiveness in the orthognathic patient, clinician, and layperson. J Oral Maxillofac Surg. 2012;70:192–206. doi: 10.1016/j.joms.2010.12.055. [DOI] [PubMed] [Google Scholar]
- 31.Motamedi MH. Treatment of condylar hiperplasia of the mandible using unilateral ramus osteotomies. J Oral Maxillofac Surg. 1996;54:1161–1169. doi: 10.1016/s0278-2391(96)90341-9. [DOI] [PubMed] [Google Scholar]
- 32.Choung PH, Nam IW. An intraoral approach to treatment of condylar hiperplasia or high condylar process fractures using the intraoral vertico-sagittal ramus osteotomy. J Oral Maxillofac Surg. 1998;56:563–570. doi: 10.1016/s0278-2391(98)90452-9. [DOI] [PubMed] [Google Scholar]
- 33.Wolford LM, Mehra P, Reiche-Fischel O, Morales-Ryan C, García-Morales P. Efficacy of high condylectomy for mangement of condylar hiperplasia. Am J Orthod Dentofacial Orthop. 2002;121:136–151. doi: 10.1067/mod.2002.118403. [DOI] [PubMed] [Google Scholar]
- 34.Iannetti G, Cascone P, Belli E, Cordaro L. Condylar hiperplasia: cephalometric study, treatment planning, and surgical correction (our experience) Oral Surg Oral Med Oral Pathol. 1989;68:673–681. doi: 10.1016/0030-4220(89)90154-0. [DOI] [PubMed] [Google Scholar]
- 35.Yamashita Y, Nakamura Y, Shimada T, Nomura Y, Hirashita A. Asymmetry of the lips of orthognathic surgery patients. Am J Orthod Dentofacial Orthop. 2009;136:559–563. doi: 10.1016/j.ajodo.2007.10.057. [DOI] [PubMed] [Google Scholar]
- 36.Ko EWC, Huang CS, Chen YR. Characteristics and corrective outcome of face asymmetry by orthognathic surgery. J Oral Maxillofac Surg. 2009;67:2201–2209. doi: 10.1016/j.joms.2009.04.039. [DOI] [PubMed] [Google Scholar]
- 37.Marchetti C, Cocchi R, Gentile L, Bianchi A. Hemimandibular hiperplasia: treatment strategies. J Craniofac Surg. 2000;11:46–53. doi: 10.1097/00001665-200011010-00009. [DOI] [PubMed] [Google Scholar]
- 38.Brusati R, Pedrazzoli M, Colletti G. Functional results after concylectomy in active laterognathia. J Craniomaxillofac Surg. 2010;38:179–184. doi: 10.1016/j.jcms.2009.04.010. [DOI] [PubMed] [Google Scholar]
- 39.Hampf G, Tasanen A, Nordling S. Surgery in mandibular condylar hiperplasia. J Maxillofac Surg. 1985;13:74–78. doi: 10.1016/s0301-0503(85)80020-5. [DOI] [PubMed] [Google Scholar]


