Abstract
Background
Both outdoor air pollution and extreme temperature have been associated with daily mortality; however, the effect of their interaction is not known.
Methods
This time-series analysis examined the effect of the interaction between outdoor air pollutants and extreme temperature on daily mortality in Shanghai, China. A generalized additive model (GAM) with penalized splines was used to analyze mortality, air pollution, temperature, and covariate data. The effects of air pollutants were stratified by temperature stratum to examine the interaction effect of air pollutants and extreme temperature.
Results
We found a statistically significant interaction between PM10/O3 and extreme low temperatures for both total nonaccidental and cause-specific mortality. On days with “normal” temperatures (15th–85th percentile), a 10-µg/m3 increment in PM10 corresponded to a 0.17% (95% CI: 0.03%, 0.32%) increase in total mortality, a 0.23% (0.02%, 0.44%) increase in cardiovascular mortality, and a 0.26% (−0.07%, 0.60%) increase in respiratory mortality. On low-temperature days (<15th percentile), the estimates changed to 0.40% (0.21%, 0.58%) for total mortality, 0.49% (0.13%, 0.86%) for cardiovascular mortality, and 0.24% (−0.33%, 0.82%) for respiratory mortality. The interaction pattern of O3 with lower temperature was similar. The interaction between PM10/O3 and lower temperature remained robust when alternative cut-points were used for temperature strata.
Conclusions
The acute health effects of air pollution might vary by temperature level.
Key words: air pollution, climate change, extreme temperature, interaction, time-series
INTRODUCTION
Short-term exposure to outdoor air pollution has been linked to adverse health effects, including increased mortality, higher rates of hospital admissions and emergency department visits, exacerbation of chronic respiratory conditions (eg, asthma), and decreased lung function.1 Temperature can also affect human health. The association between daily mortality and temperature has been extensively observed.2 Typically, a U-shaped relationship between mortality risk and temperature level is noted: mortality risk decreases from the lowest temperature to an inflection point and then increases with higher temperature.3 Basu and Samet maintained that the effect of temperature on morality might differ in areas with different weather patterns, latitudes, air pollution levels, and prevalence of air-conditioning systems.2
The rapid buildup of greenhouse gases is expected to increase not only mean temperature but also temperature variability. This change adds urgency to the need to better understand the health impact of extreme temperature, as well as its interaction with other environmental stresses.4,5 The interaction between outdoor pollution and extreme temperature was investigated as early as 1972.6 Since then, however, only a few studies have examined this issue. Katsouyanni et al analyzed the potential interaction between air pollution and high temperature and found evidence of an interaction effect.7 Roberts suggested that the interaction between daily particulate air pollution and daily mean temperature should be considered in epidemiologic studies of air pollution.8 Recent analyses of the season-specific effects of air pollution highlight the need for comprehensive investigation of the interaction between air pollution and temperature, because season is obviously related to temperature.9–14
Epidemiologic evidence of an interaction between air pollution and extreme temperature is scarce and the question remains unanswered. In this time-series analysis we examined the effect of the interaction between outdoor air pollutants—ie, particulate matter less than 10 µm in diameter (PM10), sulfur dioxide (SO2), nitrogen dioxides (NO2), and ozone (O3)—and extreme temperature on daily mortality in Shanghai, China.
METHODS
Data
Shanghai, the most populous city in China, is located at the tip of the Yangtze River Delta in eastern China. The city has a moderate subtropical climate, with 4 distinct seasons and abundant rainfall. The demographic characteristics of our study population have been described elsewhere.11,14
In this analysis, daily mortality data (excluding injuries and accidents) for residents living in the 9 urban districts of Shanghai from 1 January 2001 through 31 December 2004 were collected from the database of the Shanghai Municipal Center of Disease Control and Prevention (SMCDCP), which is the government agency in charge of health data collection in Shanghai. Consistent with previous literature,15 we did not analyze deaths from injuries or accidents because they are assumed to be unrelated to air pollution. The death reporting system in Shanghai was implemented in 1951 and has been computerized since 1990. In Shanghai, all deaths must be reported to appropriate authorities before cremation. Physicians complete the death certificate cards for both in-home and in-hospital deaths. The information on the cards is then sent to SMCDCP through their internal computer network. As required by law, the causes of death for 2001 and 2002–2004 were coded according to the International Classification of Diseases, Revision 9 (ICD-9) and Revision 10 (ICD 10), respectively. In addition to total nonaccidental deaths (ICD-9, <800; ICD-10, A00–R99), mortality data were classified into deaths due to cardiovascular diseases (ICD-9, 390–459; ICD-10, I00–I99) and respiratory diseases (ICD-9, 460–519; ICD-10, J00–J98).
Daily data on levels of PM10, SO2, NO2, and O3 from 1 January 2001 through 31 December 2004 in metropolitan Shanghai were retrieved from the database of the Shanghai Environmental Monitoring Center (SEMC). The daily concentrations of each pollutant were averaged from the available monitoring results of 6 fixed-site stations located in urban areas of Shanghai and overseen by China National Quality Control. We abstracted the 24-hour average concentrations of PM10, SO2, NO2, and 8-hour (from 10 AM to 6 PM) average concentration of O3. The maximum 8-hr mean was used because the World Health Organization (WHO) has indicated that the 8-hr mean reflects the greatest health-relevant exposure to O3.16 When calculating the 24-hour average concentrations of PM10, SO2, and NO2 and the 8-hour average O3 concentration, at least 75% of the 1-hour values had to be available for that particular day.
We obtained daily meteorological data (including minimum, maximum, and mean temperature and relative humidity) from the Shanghai Meteorological Bureau. The weather data were measured at a fixed-site station located in the Xuhui District of Shanghai.
Data on mortality, pollutants, and meteorological variables were validated by an independent auditing team, which checked a sample of the original death certificates and monitoring records and validated the process for generating data on mortality, weather, and air pollution used in this time-series analysis.
Statistical analysis
We used a generalized additive model (GAM) with penalized splines to analyze data on mortality, air pollution, and covariates. Because daily mortality counts typically follow a Poisson distribution, the core analysis was a GAM with log link and Poisson error, which accounted for smooth fluctuations in daily mortality. Consistent with several recent time-series studies,17–19 we used the penalized spline model in our analysis.
We first built the basic models for various mortality outcomes without including air pollution or weather variables. We incorporated smoothed spline functions of time, which accommodate nonlinear and nonmonotonic patterns between mortality and time, thus offering a flexible modeling tool. The partial autocorrelation function (PACF) was used to guide the selection of df until the absolute values of the sum of PACF for lags up to 30 reached a minimum. In this way, 4, 4, and 5 df per year were used for the time trend in our basic models for total, cardiovascular, and respiratory mortality, respectively. Day of the week (DOW) was included as a dummy variable in the basic models. Residuals of the basic models were also examined to check whether there were discernable patterns and autocorrelation by means of residual plots and partial autocorrelation function (PACF) plots.
After we established the basic models, we introduced the pollutant and weather variables and analyzed their effects on mortality outcomes. Based on the previous literature,20–22 3 df (whole period of study) for mean temperature and relative humidity could satisfactorily control for their effects on mortality and was thus used in the model.
To examine the effect of the interaction between air pollutants and extreme temperature, we stratified the effects of air pollutants by temperature. As compared with other methods used to detect interaction effects, temperature stratification requires fewer parameters and yields a simple, quantitative comparison of the estimated effects of pollutants in various temperature strata.8 As in a prior study,8 we set the upper (U) and lower (L) temperature cut-points equal to the 85th and 15th percentiles of temperature, respectively. Due to this inherently arbitrary choice of cut-point values, a sensitivity analysis was performed to address the sensitivity of the estimated effects of air pollutants to the choice of cut-point values (95th and 5th, 90th and 10th, 80th and 20th, 75th and 25th). We tested the statistical significance of differences between effect estimates of the temperature strata (eg, the effect of PM10 on “normal” temperature vs low temperature days) by calculating the 95% confidence interval (95% CI) as , where and are the estimates for the 2 categories and and are their respective standard errors.23
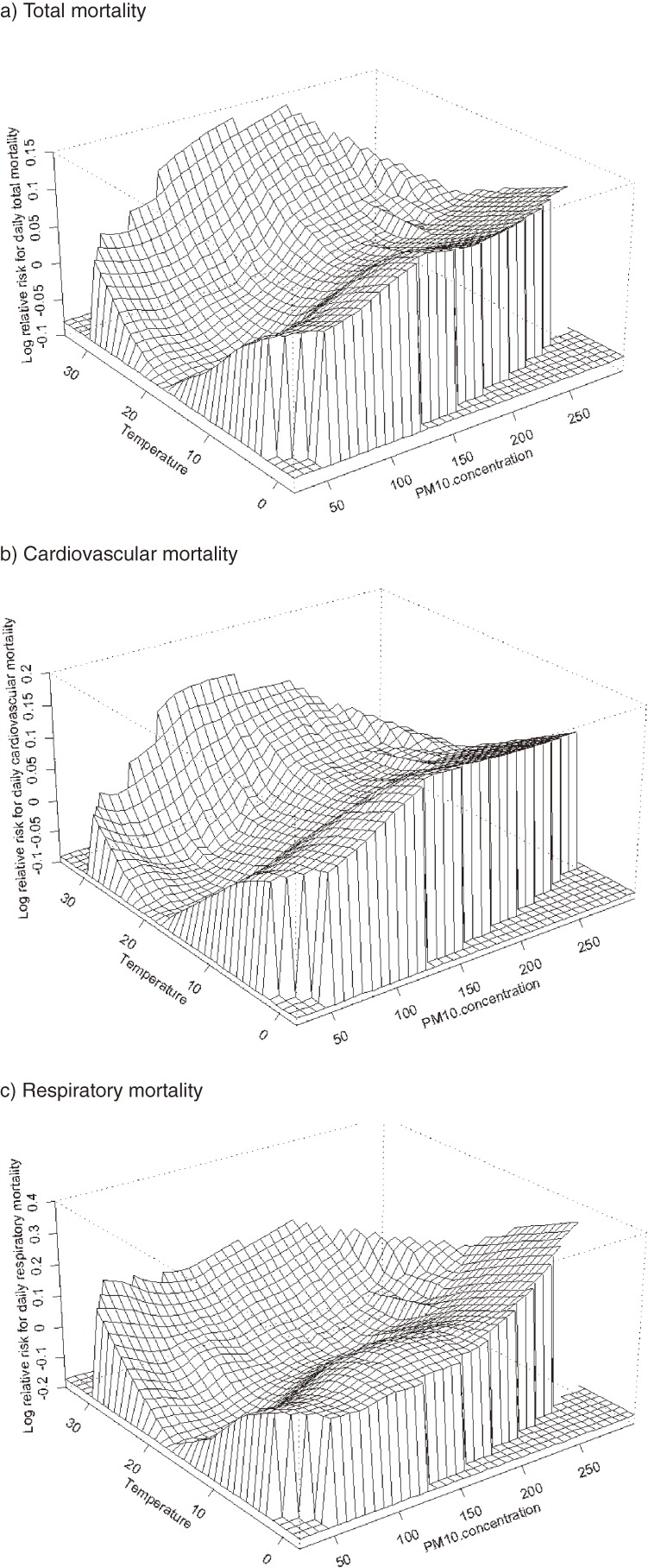
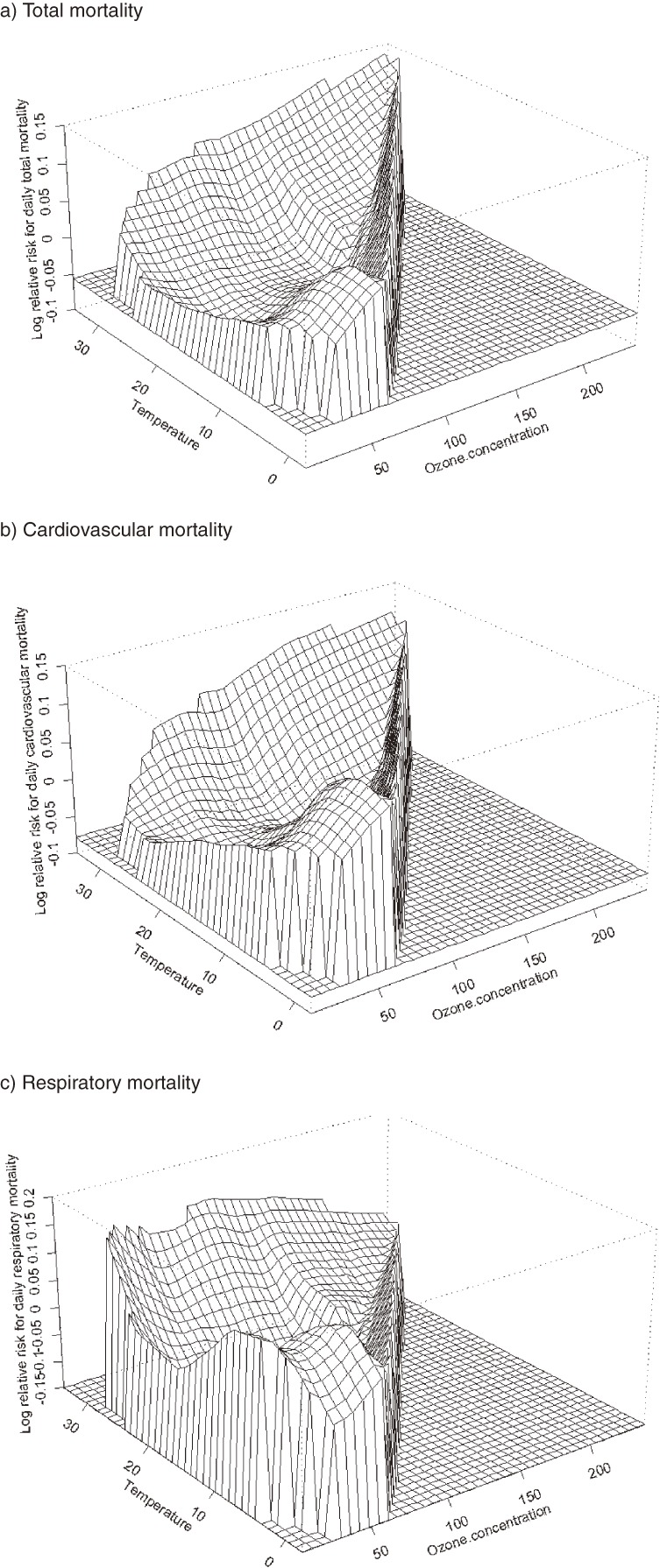
To graphically illustrate the interaction between air pollution and extreme temperature, we fitted nonparametric response surface models to identify the joint effects of air pollution and temperature on daily mortality. We used a GAM to fit a response surface that captured the relation between the 2 main independent variables and the dependent variable, without assuming linearity.24,25 All analyses were conducted using R 2.10.1 and the MGCV package.
RESULTS
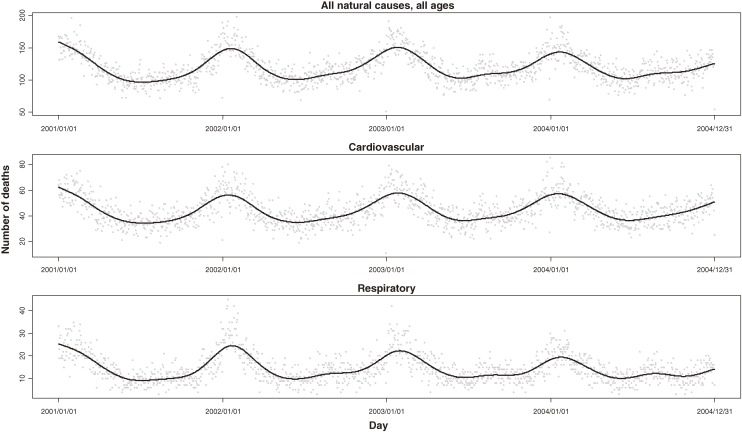
Our research population included approximately 6.3 million residents, and the number remained stable during our research period. From 2001 through 2004 (1461 days), 173 911 nonaccidental deaths were recorded in the study population. On average, there were 119.0 nonaccidental deaths per day in the target population, including 44.2 from cardiovascular diseases and 14.3 from respiratory diseases (Figure 1 ). Cardiopulmonary diseases accounted for 49.1% of all nonaccidental deaths among urban residents of Shanghai.
Figure 1. Time-series of total nonaccidental, cardiovascular, and respiratory mortality in Shanghai, 2001–2004. Solid lines are smoothing splines with 5 df/yr.
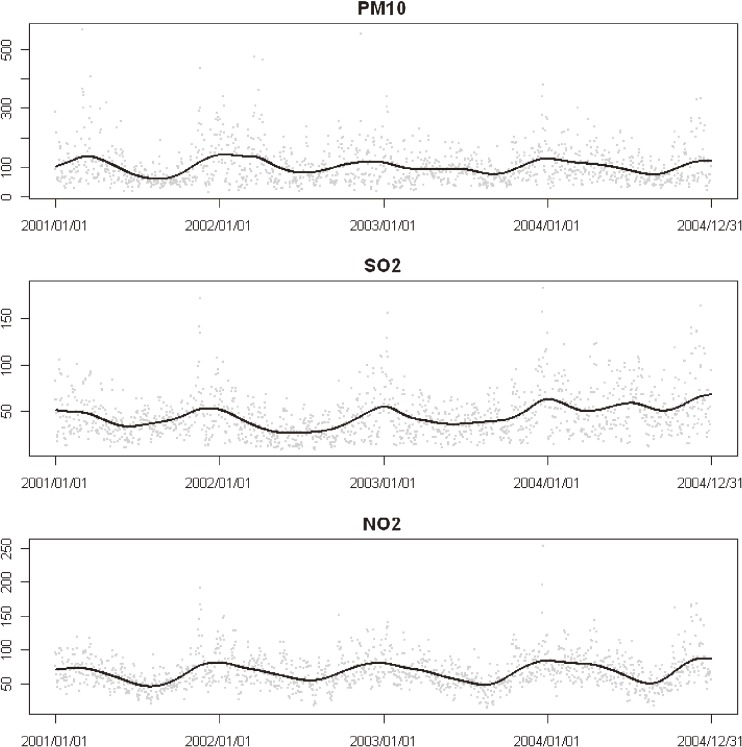
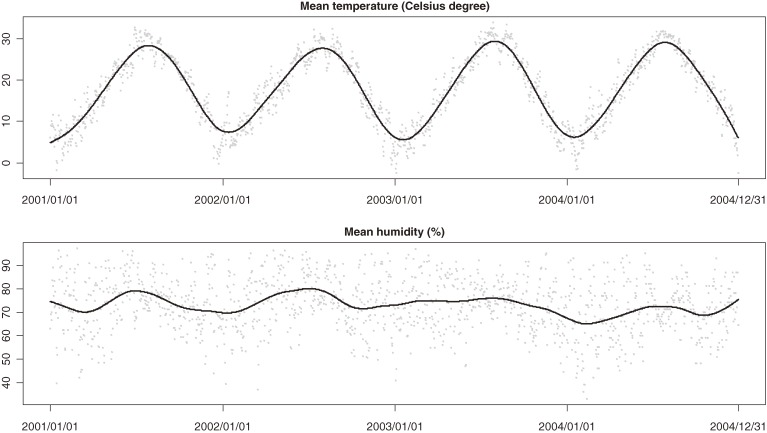
The mean air pollution levels were 101.9 µg/m3 for PM10, 44.7 µg/m3 for SO2, 66.6 µg/m3 for NO2, and 63.5 µg/m3 for O3 (Figure 2 ). The data were 100% complete for all variables except O3 (7 missing days). Meanwhile, the mean daily average temperature and humidity were 17.7°C and 72.9%, reflecting the subtropical climate in Shanghai (Figure 3 ).
Figure 2. Time-series of monitor-averaged pollutant concentrations (µg/m3) in Shanghai, 2001–2004. Solid lines are smoothing splines with 5 df/yr.
Figure 3. Time-series of temperature (°C) and relative humidity (%) in Shanghai, 2001–2004. Solid lines are smoothing splines with 5 df/yr.
Figures 4 and 5 show joint response surfaces that illustrate the potential interactive effects of PM10/O3 and temperature on total, cardiovascular, and respiratory mortality. Tables 1 to 3 describe the results of a regression analysis of air pollutants stratified by temperature stratum. In general, the effect of the interaction between PM10 and extreme low temperature was statistically significant for both total and cause-specific mortality. For example, on “normal” temperature (15th–85th percentile) days, a 10-µg/m3 increment in PM10 corresponded to a 0.17% (95% CI: 0.03%, 0.32%) increase in total mortality, a 0.23% (0.02%, 0.44%) increase in cardiovascular mortality, and a 0.26% (−0.07%, 0.60%) increase in respiratory mortality. On low-temperature (<15th percentile) days, the estimates increased to 0.40% (0.21%, 0.58%) for total mortality (P = 0.01 compared with normal temperature days), 0.49% (0.13%–0.86%) for cardiovascular mortality (P = 0.04), and 0.24% (−0.33%, 0.82%) for respiratory mortality (P = 0.04). On high-temperature (>85th percentile) days, the numbers were 0.30% (−0.01%, 0.63%), 0.30% (−0.17%, 0.79%), and 0.35% (−0.49%, 1.19%) for total, cardiovascular, and respiratory mortality respectively, and none of these estimates significantly differed from those for normal temperature days. The interaction pattern of O3 with low temperature was similar (Tables 1–3). There was no significant interaction for SO2 or NO2. The use of alternative cut-points for temperature strata yielded similar trends.
Figure 4. Bivariate response surfaces of temperature and PM10 for total (a), cardiovascular (b), and respiratory mortality (c) in Shanghai, 2001–2004.
Figure 5. Bivariate response surfaces of temperature and O3 for total (a), cardiovascular (b), and respiratory mortality (c) in Shanghai, 2001–2004.
Table 1. Percent change (95% CI) in total mortality per 10-µg/m3 increment in air pollutants at different temperature strata.
| Percentile cut-points for temperature (L, U) |
PM10 | SO2 | NO2 | O3 | |||||
| % | P valuea | % | P valuea | % | P valuea | % | P valuea | ||
| (5–95) | 5% L | 0.46 (0.21, 0.72) | 0.03b | 1.56 (0.95, 2.16) | 0.05 | 1.25 (0.71, 1.79) | 0.15 | 1.78 (0.84, 2.73) | <0.01b |
| 95% U | 0.44 (0.07, 0.82) | 0.18 | 1.05 (0.31, 1.79) | 0.94 | 1.04 (0.33, 1.75) | 0.73 | 0.54 (0.15, 0.92) | 0.77 | |
| 5%–95% | 0.20 (0.06, 0.34) | 1.03 (0.63, 1.43) | 0.92 (0.54, 1.31) | 0.58 (0.25, 0.92) | |||||
| (10–90) | 10% L | 0.42 (0.20, 0.64) | 0.04b | 1.30 (0.78, 1.82) | 0.29 | 1.17 (0.69, 1.66) | 0.20 | 2.06 (1.21, 2.91) | <0.01b |
| 90% U | 0.39 (0.02, 0.76) | 0.29 | 0.91 (0.15, 1.67) | 0.70 | 0.95 (0.23, 1.66) | 0.95 | 0.47 (0.08, 0.86) | 0.39 | |
| 10%–90% | 0.19 (0.05, 0.33) | 1.04 (0.63, 1.46) | 0.93 (0.54, 1.32) | 0.62 (0.29, 0.96) | |||||
| (15–85) | 15% L | 0.40 (0.21, 0.58) | 0.01b | 1.31 (0.84, 1.77) | 0.16 | 1.20 (0.77, 1.64) | 0.05 | 2.17 (1.46, 2.88) | <0.01b |
| 85% U | 0.30 (−0.01, 0.63) | 0.41 | 0.78 (0.05, 1.52) | 0.52 | 0.81 (0.20, 1.42) | 0.78 | 0.42 (0.05, 0.79) | 0.19 | |
| 15%–85% | 0.17 (0.03, 0.32) | 1.01 (0.58, 1.44) | 0.89 (0.49, 1.29) | 0.66 (0.32, 1.00) | |||||
| (20–80) | 20% L | 0.30 (0.13, 0.47) | 0.12 | 1.18 (0.73, 1.63) | 0.54 | 1.07 (0.65, 1.50) | 0.25 | 1.66 (1.03, 2.29) | <0.01b |
| 80% U | 0.36 (0.07, 0.65) | 0.20 | 1.03 (0.34, 1.71) | 0.93 | 0.99 (0.44, 1.55) | 0.70 | 0.51 (0.16, 0.85) | 0.55 | |
| 20%–80% | 0.18 (0.03, 0.33) | 1.05 (0.62, 1.49) | 0.90 (0.50, 1.30) | 0.61 (0.25, 0.96) | |||||
| (25–75) | 25% L | 0.32 (0.15, 0.49) | 0.05 | 1.20 (0.76, 1.64) | 0.43 | 1.09 (0.66, 1.51) | 0.22 | 1.44 (0.88, 2.00) | <0.01b |
| 75% U | 0.29 (0.02, 0.56) | 0.35 | 0.91 (0.25, 1.57) | 0.68 | 0.93 (0.41, 1.45) | 0.92 | 0.47 (0.13, 0.80) | 0.46 | |
| 25%–75% | 0.16 (0.01, 0.32) | 1.04 (0.59, 1.49) | 0.91 (0.50, 1.31) | 0.59 (0.22, 0.96) | |||||
Abbreviations: PM10, particulate matter less than 10 microns in diameter; SO2, sulfur dioxide; NO2, nitrogen dioxides; O3, ozone.
aP value for lower and upper temperature stratum compared with normal temperature.
bStatistically significant (P < 0.05).
Table 3. Percent change (95% CI) in respiratory mortality per 10-µg/m3 increment in air pollutants at different temperature strata.
| Percentile cut-points for temperature (L, U) |
PM10 | SO2 | NO2 | O3 | |||||
| % | P valuea | % | P valuea | % | P valuea | % | P valuea | ||
| (5–95) | 5% L | 0.24 (−0.33, 0.82) | 0.95 | 1.53 (0.11, 2.95) | 0.74 | 1.30 (0.03, 2.57) | 0.75 | 0.98 (−1.22, 3.19) | 0.86 |
| 95% U | 0.22 (−0.74, 1.19) | 0.94 | 1.64 (−0.28, 3.58) | 0.92 | 1.05 (−0.80, 2.91) | 0.64 | 0.63 (−0.38, 1.65) | 0.72 | |
| 5%–95% | 0.26 (−0.07, 0.60) | 1.73 (0.74, 2.72) | 1.46 (0.50, 2.42) | 0.79 (−0.07, 1.67) | |||||
| (10–90) | 10% L | 0.37 (−0.13, 0.88) | 0.56 | 1.57 (0.33, 2.80) | 0.72 | 1.56 (0.40, 2.71) | 0.70 | 2.34 (0.39, 4.29) | 0.10 |
| 90% U | 0.23 (−0.74, 1.20) | 0.99 | 1.65 (−0.36, 3.67) | 0.90 | 1.10 (−0.76, 2.97) | 0.74 | 0.42 (−0.62, 1.46) | 0.33 | |
| 10%–90% | 0.23 (−0.10, 0.57) | 1.76 (0.74, 2.79) | 1.39 (0.42, 2.36) | 0.88 (0.00, 1.75) | |||||
| (15–85) | 15% L | 0.55 (0.11, 0.99) | 0.04b | 2.01 (0.90, 3.11) | 0.26 | 1.82 (0.78, 2.87) | 0.06 | 2.79 (1.13, 4.46) | <0.01b |
| 85% U | 0.35 (−0.49, 1.19) | 0.60 | 1.38 (−0.56, 3.33) | 0.95 | 1.27 (−0.33, 2.88) | 0.84 | 0.53 (−0.46, 1.53) | 0.56 | |
| 15%–85% | 0.13 (−0.22, 0.48) | 1.44 (0.36, 2.53) | 1.12 (0.12, 2.12) | 0.81 (−0.09, 1.72) | |||||
| (20–80) | 20% L | 0.32 (−0.07, 0.72) | 0.48 | 1.70 (0.62, 2.79) | 0.99 | 1.55 (0.53, 2.57) | 0.48 | 2.11 (0.60, 3.62) | 0.04b |
| 80% U | 0.38 (−0.38, 1.14) | 0.62 | 1.62 (−0.19, 3.43) | 0.92 | 1.28 (−0.18, 2.74) | 0.97 | 0.64 (−0.28, 1.57) | 0.82 | |
| 20%–80% | 0.19 (−0.17, 0.56) | 1.71 (0.61, 2.81) | 1.30 (0.29, 2.31) | 0.75 (−0.19, 1.69) | |||||
| (25–75) | 25% L | 0.51 (0.12, 0.90) | 0.01b | 2.16 (1.09, 3.23) | 0.08 | 1.90 (0.88, 2.93) | 0.02 | 2.31 (0.93, 3.69) | <0.01b |
| 75% U | 0.14 (−0.56, 0.86) | 0.79 | 0.73 (−1.01, 2.47) | 0.52 | 0.72 (−0.63, 2.09) | 0.51 | 0.46 (−0.43, 1.35) | 0.45 | |
| 25%–75% | 0.05 (−0.31, 0.43) | 1.26 (0.12, 2.41) | 1.10 (0.09, 2.12) | 0.79 (−0.19, 1.77) | |||||
Abbreviations: PM10, particulate matter less than 10 microns in diameter; SO2, sulfur dioxide; NO2, nitrogen dioxides; O3, ozone.
aP value for lower and upper temperature strata compared with normal temperature.
bStatistically significant (P < 0.05).
Table 2. Percent change (95% CI) in cardiovascular mortality per 10-µg/m3 increment in air pollutants at different temperature strata.
| Percentile cut-points for temperature (L, U) |
PM10 | SO2 | NO2 | O3 | |||||
| % | P valuea | % | P valuea | % | P valuea | % | P valuea | ||
| (5–95) | 5% L | 0.49 (0.13, 0.86) | 0.20 | 1.70 (0.82, 2.58) | 0.18 | 1.48 (0.70, 2.26) | 0.43 | 1.66 (0.28, 3.04) | 0.17 |
| 95% U | 0.72 (0.16, 1.29) | 0.11 | 1.45 (0.33, 2.57) | 0.58 | 1.68 (0.61, 2.76) | 0.36 | 0.88 (0.31, 1.46) | 0.60 | |
| 5%–95% | 0.26 (0.06, 0.47) | 1.16 (0.58, 1.75) | 1.22 (0.65, 1.79) | 0.75 (0.25, 1.24) | |||||
| (10–90) | 10% L | 0.45 (0.13, 0.77) | 0.20 | 1.43 (0.67, 2.19) | 0.42 | 1.32 (0.61, 2.03) | 0.73 | 1.81 (0.56, 3.05) | 0.07 |
| 90% U | 0.80 (0.24, 1.36) | 0.08 | 1.64 (0.49, 2.79) | 0.36 | 1.83 (0.76, 2.90) | 0.23 | 0.91 (0.33, 1.50) | 0.51 | |
| 10%–90% | 0.25 (0.05, 0.46) | 1.15 (0.55, 1.76) | 1.22 (0.65, 1.80) | 0.74 (0.24, 1.23) | |||||
| (15–85) | 15% L | 0.51 (0.23, 0.79) | 0.03b | 1.63 (0.96, 2.31) | 0.07 | 1.56 (0.92, 2.19) | 0.15 | 2.57 (1.53, 3.62) | <0.01b |
| 85% U | 0.30 (−0.17, 0.79) | 0.75 | 0.64 (−0.46, 1.75) | 0.42 | 0.91 (−0.0, 1.82) | 0.46 | 0.62 (0.06, 1.18) | 0.33 | |
| 15%–85% | 0.23 (0.02, 0.44) | 1.06 (0.43, 1.70) | 1.22 (0.63, 1.80) | 0.88 (0.37, 1.40) | |||||
| (20–80) | 20% L | 0.44 (0.20, 0.69) | 0.08 | 1.66 (1.00, 2.31) | 0.04b | 1.59 (0.97, 2.20) | 0.07 | 2.37 (1.45, 3.29) | <0.01b |
| 80% U | 0.16 (−0.26, 0.60) | 0.75 | 0.47 (−0.56, 1.50) | 0.23 | 0.78 (−0.04, 1.61) | 0.25 | 0.56 (0.04, 1.09) | 0.10 | |
| 20%–80% | 0.23 (0.01, 0.45) | 1.06 (0.42, 1.69) | 1.20 (0.62, 1.79) | 0.98 (0.45, 1.52) | |||||
| (25–75) | 25% L | 0.38 (0.14, 0.63) | 0.36 | 1.45 (0.80, 2.09) | 0.57 | 1.44 (0.82, 2.05) | 0.59 | 1.87 (1.05, 2.70) | 0.02b |
| 75% U | 0.13 (−0.27, 0.54) | 0.47 | 0.49 (−0.50, 1.49) | 0.09 | 0.87 (0.09, 1.65) | 0.17 | 0.54 (0.04, 1.05) | 0.07 | |
| 25%–75% | 0.28 (0.05, 0.50) | 1.28 (0.62, 1.94) | 1.32 (0.73, 1.91) | 1.03 (0.47, 1.59) | |||||
Abbreviations: PM10, particulate matter less than 10 microns in diameter; SO2, sulfur dioxide; NO2, nitrogen dioxides; O3, ozone.
aP value for lower and upper temperature strata compared with normal temperature.
bStatistically significant (P < 0.05).
DISCUSSION
In this community-based time-series analysis we found a statistically significant interaction between air pollution and lower temperature in their effects on daily mortality. Our findings were limited to PM10 and O3. Unlike previous studies,26,27 we did not find a significant interaction between air pollution and higher temperature.
Although the underlying mechanism is unclear, previous studies have shown that extreme temperature might increase the workload of the cardiopulmonary system and induce adverse cardiopulmonary events.28,29 For example, sudden inhalation of cold air was found to be associated with the release of inflammatory mediators associated with mast cells in a human study.30 In addition, marked changes in ambient temperature can cause physiologic stress and alter a person’s physiologic response to toxic agents, perhaps making them more susceptible to the effects of air pollutants.31,32 Moreover, most air pollution-related deaths occur in elderly adults,33 who have a lower capacity for thermoregulation34 and a higher sweating threshold as compared with younger persons.35 Therefore, an interaction between PM10/O3 and extreme temperature is biologically plausible.
As mentioned earlier, a number of studies,10,12,13 including our own,11,14 have investigated the interaction between air pollution and season. The present study did not investigate seasonality; instead, we focused on the related issue of the interaction between air pollution and extreme temperature, since temperature and season are associated. Our finding of a stronger association between air pollution and daily mortality on extremely cold days confirms those of 3 earlier seasonal analyses in Hong Kong, Shanghai, and Athens,12,14,36,37 but conflicts with those of several other reports that noted greater effects during the warm or hot season.21,38–43 In London, for example, the effects of NO2 and SO2 were stronger in the warm season than in the cool season.38 A combined analysis of data from 9 European cities also showed that SO2 had a slightly stronger effect during the warm season than during the cool season.44 For O3, which usually reaches higher concentrations in the warm season, several recent meta-analyses and multi-city analyses also found that the effect was evident only during the warm season.39,41,43
Our observation of stronger effects of air pollution on extremely cold days might be due to the larger sample size of daily numbers of deaths on cold days (Figure 1). Moreover, mean PM10 concentrations on cold days were higher than on days with normal or high temperatures. These 2 factors might have increased the power of the analyses of cold days. Because pollutant levels are correlated, the greater effects of air pollution observed on cold days may also be due to the effects of other pollutants that were also at higher levels on those days.37 Another potential explanation for the temperature-specific effects of PM10 is that levels of the most toxic particles might reach a maximum during the cool season in Shanghai. Unlike gaseous pollutants, the constituents of PM10 might vary by season as a complex mixture.45
Previous studies in both Wuhan27 and Tianjin26 showed that high temperatures might increase the health effects of air pollution. However, our analysis in Shanghai did not find a significant interaction between air pollution and extremely high temperature. We assume that exposure patterns contribute to various temperature-specific health effects in different cities. Shanghai receives considerable rainfall in summer. During those days of high temperatures, Shanghai residents tend to use air conditioning more frequently because of the higher temperature and humidity, thus reducing their indoor exposure. For example, in a survey of 1106 families in Shanghai, 32.7% never turned on an air conditioner during winter, as compared with 3.7% in the summer.46 Heavy rain in the summer may reduce time outdoors, thus decreasing personal exposure. In contrast, the winter in Shanghai is drier and less variable, so people are more likely to go outdoors and open windows.
The system for death coding may have had an impact on the effect estimates of air pollution on mortality.47 We did not consider deaths due to injuries or accidents because they are not believed to be associated with air pollution.15 Moreover, the causes of death for 2001 and 2002–2004 in Shanghai were coded according to the ICD-9 and ICD-10, respectively. However, a previous study in Wuhan showed that the change in ICD coding did not significantly affect the estimated effects of time-series studies of air pollution.47
Extreme temperature is related to global warming and other climate phenomena, such as El Niño. The possibility that extreme low temperatures intensify the health hazards of exposure to air pollution could spark new interest in the correlations between weather, air pollution, and health. Of course, our findings require replication, especially in areas with different weather patterns; but if substantiated, they provide insight into the health impact of both air pollution and climate change.
ACKNOWLEDGMENTS
The study was supported by the National Basic Research Program (973 program) of China (2011CB503802), the Gong-Yi Program of the China Ministry of Environmental Protection (201209008 and 200809109), the National Natural Science Foundation of China (30800892), and the Program for New Century Excellent Talents in University (NCET-09-0314).
Conflicts of interest: The authors declared no competing financial interests.
REFERENCES
- 1.Goldberg MS , Burnett RT , Stieb D. A review of time-series studies used to evaluate the short-term effects of air pollution on human health . Rev Environ Health. 2003;18(4):269–303 10.1515/REVEH.2003.18.4.269 [DOI] [PubMed] [Google Scholar]
- 2.Basu R , Samet JM. Relation between elevated ambient temperature and mortality: a review of the epidemiologic evidence . Epidemiol Rev. 2002;24(2):190–202 10.1093/epirev/mxf007 [DOI] [PubMed] [Google Scholar]
- 3.Kan HD , Jia J , Chen BH. Temperature and daily mortality in Shanghai: a time-series study . Biomed Environ Sci. 2003;16(2):133–9 [PubMed] [Google Scholar]
- 4.Kan H Climate change and human health in China . Environ Health Perspect. 2011;119(2):A60–1 10.1289/ehp.1003354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kan H , Chen R , Tong S. Ambient air pollution, climate change, and population health in China . Environ Int. 2011. doi:10.1016/j.envint.2011.03.003 [DOI] [PubMed] [Google Scholar]
- 6.Goldstein IF Interaction of air pollution and weather in their effects on health . HSMHA Health Rep. 1972;87(1):50–5 10.2307/4594426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Katsouyanni K , Pantazopoulou A , Touloumi G , Tselepidaki I , Moustris K , Asimakopoulos D , et al. Evidence for interaction between air pollution and high temperature in the causation of excess mortality . Arch Environ Health. 1993;48(4):235–42 10.1080/00039896.1993.9940365 [DOI] [PubMed] [Google Scholar]
- 8.Roberts S Interactions between particulate air pollution and temperature in air pollution mortality time series studies . Environ Res. 2004;96(3):328–37 10.1016/j.envres.2004.01.015 [DOI] [PubMed] [Google Scholar]
- 9.Welty LJ , Zeger SL. Are the acute effects of particulate matter on mortality in the National Morbidity, Mortality, and Air Pollution Study the result of inadequate control for weather and season? A sensitivity analysis using flexible distributed lag models . Am J Epidemiol. 2005;162(1):80–8 10.1093/aje/kwi157 [DOI] [PubMed] [Google Scholar]
- 10.Peng RD , Dominici F , Pastor-Barriuso R , Zeger SL , Samet JM. Seasonal analyses of air pollution and mortality in 100 US cities . Am J Epidemiol. 2005;161(6):585–94 10.1093/aje/kwi075 [DOI] [PubMed] [Google Scholar]
- 11.Kan H , London SJ , Chen G , Zhang Y , Song G , Zhao N , et al. Season, sex, age, and education as modifiers of the effects of outdoor air pollution on daily mortality in Shanghai, China: The Public Health and Air Pollution in Asia (PAPA) Study . Environ Health Perspect. 2008;116(9):1183–8 10.1289/ehp.10851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Touloumi G , Samoli E , Katsouyanni K. Daily mortality and “winter type” air pollution in Athens, Greece—a time series analysis within the APHEA project . J Epidemiol Community Health. 1996;50Suppl 1:s47–51 10.1136/jech.50.Suppl_1.s47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wagner BM Air pollution and daily mortality in two U.S. counties: season-specific analyses and exposure-response relationships . Inhal Toxicol. 2004;16(2):113; author reply 114 [PubMed] [Google Scholar]
- 14.Zhang Y , Huang W , London SJ , Song G , Chen G , Jiang L , et al. Ozone and daily mortality in Shanghai, China . Environ Health Perspect. 2006;114(8):1227–32 10.1289/ehp.9014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brunekreef B , Holgate ST. Air pollution and health . Lancet. 2002;360(9341):1233–42 10.1016/S0140-6736(02)11274-8 [DOI] [PubMed] [Google Scholar]
- 16.World Health Organization. Air Quality Guideline for Europe. Copenhagen; 2000.
- 17.Ostro B , Broadwin R , Green S , Feng WY , Lipsett M. Fine particulate air pollution and mortality in nine California counties: results from CALFINE . Environ Health Perspect. 2006;114(1):29–33 10.1289/ehp.8335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peng RD , Dominici F , Louis TA. Model choice in time series studies of air pollution and mortality . J R Stat Soc [Ser A]. 2006;169(2):179–203 10.1111/j.1467-985X.2006.00410.x [DOI] [Google Scholar]
- 19.Samoli E , Aga E , Touloumi G , Nisiotis K , Forsberg B , Lefranc A , et al. Short-term effects of nitrogen dioxide on mortality: an analysis within the APHEA project . Eur Respir J. 2006;27(6):1129–38 10.1183/09031936.06.00143905 [DOI] [PubMed] [Google Scholar]
- 20.Dominici F , Peng RD , Bell ML , Pham L , McDermott A , Zeger SL , et al. Fine particulate air pollution and hospital admission for cardiovascular and respiratory diseases . JAMA. 2006;295(10):1127–34 10.1001/jama.295.10.1127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bell ML , McDermott A , Zeger SL , Samet JM , Dominici F. Ozone and short-term mortality in 95 US urban communities, 1987–2000 . JAMA. 2004;292(19):2372–8 10.1001/jama.292.19.2372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Samet JM , Zeger SL , Dominici F , Curriero F , Coursac I , Dockery DW , et al. The National Morbidity, Mortality, and Air Pollution Study. Part II: Morbidity and mortality from air pollution in the United States . Res Rep Health Eff Inst. 2000;94(Pt 2):5–70; discussion 1–9 [PubMed] [Google Scholar]
- 23.Zeka A , Zanobetti A , Schwartz J. Individual-level modifiers of the effects of particulate matter on daily mortality . Am J Epidemiol. 2006;163(9):849–59 10.1093/aje/kwj116 [DOI] [PubMed] [Google Scholar]
- 24.Ren C , Williams GM , Morawska L , Mengersen K , Tong S. Ozone modifies associations between temperature and cardiovascular mortality: analysis of the NMMAPS data . Occup Environ Med. 2008;65(4):255–60 10.1136/oem.2007.033878 [DOI] [PubMed] [Google Scholar]
- 25.Ren C , Williams GM , Tong S. Does particulate matter modify the association between temperature and cardiorespiratory diseases? Environ Health Perspect. 2006;114(11):1690–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li G , Zhou M , Cai Y , Zhang Y , Pan X. Does temperature enhance acute mortality effects of ambient particle pollution in Tianjin City, China . Sci Total Environ. 2011;409(10):1811–7 10.1016/j.scitotenv.2011.02.005 [DOI] [PubMed] [Google Scholar]
- 27.Qian Z , He Q , Lin HM , Kong L , Bentley CM , Liu W , et al. High temperatures enhanced acute mortality effects of ambient particle pollution in the “oven” city of Wuhan, China . Environ Health Perspect. 2008;116(9):1172–8 10.1289/ehp.10847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Imai Y , Nobuoka S , Nagashima J , Awaya T , Aono J , Miyake F , et al. Acute myocardial infarction induced by alternating exposure to heat in a sauna and rapid cooling in cold water . Cardiology. 1998;90(4):299–301 10.1159/000006862 [DOI] [PubMed] [Google Scholar]
- 29.Haines A , Patz JA. Health effects of climate change . JAMA. 2004;291(1):99–103 10.1001/jama.291.1.99 [DOI] [PubMed] [Google Scholar]
- 30.Togias AG , Naclerio RM , Proud D , Fish JE , Adkinson NF Jr , Kagey-Sobotka A , et al. Nasal challenge with cold, dry air results in release of inflammatory mediators. Possible mast cell involvement . J Clin Invest. 1985;76(4):1375–81 10.1172/JCI112113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gordon CJ , Leon LR. Thermal stress and the physiological response to environmental toxicants . Rev Environ Health. 2005;20(4):235–63 10.1515/REVEH.2005.20.4.235 [DOI] [PubMed] [Google Scholar]
- 32.Noyes PD , McElwee MK , Miller HD , Clark BW , Van Tiem LA , Walcott KC , et al. The toxicology of climate change: environmental contaminants in a warming world . Environ Int. 2009;35(6):971–86 10.1016/j.envint.2009.02.006 [DOI] [PubMed] [Google Scholar]
- 33.Bateson TF , Schwartz J. Who is sensitive to the effects of particulate air pollution on mortality?: a case-crossover analysis of effect modifiers . Epidemiology. 2004;15(2):143–9 10.1097/01.ede.0000112210.68754.fa [DOI] [PubMed] [Google Scholar]
- 34.Kenney WL , Hodgson JL. Heat tolerance, thermoregulation and ageing . Sports Med. 1987;4(6):446–56 10.2165/00007256-198704060-00004 [DOI] [PubMed] [Google Scholar]
- 35.Foster KG , Ellis FP , Doré C , Exton-Smith AN , Weiner JS. Sweat responses in the aged . Age Ageing. 1976;5(2):91–101 10.1093/ageing/5.2.91 [DOI] [PubMed] [Google Scholar]
- 36.Wong CM , Ma S , Hedley AJ , Lam TH. Does ozone have any effect on daily hospital admissions for circulatory diseases? J Epidemiol Community Health. 1999;53(9):580–1 10.1136/jech.53.9.580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wong CM , Ma S , Hedley AJ , Lam TH. Effect of air pollution on daily mortality in Hong Kong . Environ Health Perspect. 2001;109(4):335–40 10.1289/ehp.01109335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Anderson HR , Ponce de Leon A , Bland JM , Bower JS , Strachan DP. Air pollution and daily mortality in London: 1987–92 . BMJ. 1996;312(7032):665–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bell ML , Dominici F , Samet JM. A meta-analysis of time-series studies of ozone and mortality with comparison to the national morbidity, mortality, and air pollution study . Epidemiology. 2005;16(4):436–45 10.1097/01.ede.0000165817.40152.85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bremner SA , Anderson HR , Atkinson RW , McMichael AJ , Strachan DP , Bland JM , et al. Short-term associations between outdoor air pollution and mortality in London 1992–4 . Occup Environ Med. 1999;56(4):237–44 10.1136/oem.56.4.237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ito K , De Leon SF , Lippmann M. Associations between ozone and daily mortality: analysis and meta-analysis . Epidemiology. 2005;16(4):446–57 10.1097/01.ede.0000165821.90114.7f [DOI] [PubMed] [Google Scholar]
- 42.Ostro B , Sanchez JM , Aranda C , Eskeland GS. Air pollution and mortality: results from a study of Santiago, Chile . J Expo Anal Environ Epidemiol. 1996;6(1):97–114 [PubMed] [Google Scholar]
- 43.Schwartz J How sensitive is the association between ozone and daily deaths to control for temperature? Am J Respir Crit Care Med. 2005;171(6):627–31 10.1164/rccm.200407-933OC [DOI] [PubMed] [Google Scholar]
- 44.Zmirou D , Schwartz J , Saez M , Zanobetti A , Wojtyniak B , Touloumi G , et al. Time-series analysis of air pollution and cause-specific mortality . Epidemiology. 1998;9(5):495–503 10.1097/00001648-199809000-00005 [DOI] [PubMed] [Google Scholar]
- 45.Environmental Protection Agency (US). Air quality criteria for particulate matter (fourth external review draft). (EPA publication nos. EPA/600/P-99/002aD and EPA/600/P-99/002bD). Research Triangle Park, NC: National Center for Environmental Assessment; 2003. [Google Scholar]
- 46.Long W, Zhong T, Zhang B. China: the issue of residential air conditioning (http://www.iifiir.org/en/doc/1056.pdf). 2007.
- 47.Qian Z , He Q , Lin HM , Kong L , Liao D , Gong J , et al. Exploring uncertainty of the change from ICD-9 to ICD-10 on acute mortality effects of air pollution . Environ Int. 2008;34(2):248–53 10.1016/j.envint.2007.08.006 [DOI] [PubMed] [Google Scholar]