Abstract
Background and Aims: Melasma is a treatment-resistant and acquired pigmentary facial skin condition of uncertain etiology particularly prevalent in the older Asian female. Traditional bleaching agents have offered some success. Intense pulsed light (IPL), fractionated nonablative and more recently ablative laser technology have also been used, but were associated with postoperative hyperpigmentation in the Asian skin. The present study examined the consecutive application of 2 modes of the 1064 nm Nd:YAG laser in the ‘dual toning’ process.
Subjects and Methods: Thirty females, mean age 41.4 ± 11.96 yr, Fitzpatrick skin type IV, participated in the prospective uncontrolled study. All subjects were treated with the 1064 nm Nd:YAG laser, first with the 5 ns Q-switched mode, 1.2 J/cm2, 8 mm collimated handpiece with multiple passes and then immediately after with the micropulsed mode, 300 µs, 7.0 J/cm2, 5 mm handpiece, multiple passes. Mild and even erythema was the endpoint. Treatments were given every other week until maximum improvement was obtained. Improvement was rated at a final assessment 6 weeks after the final treatment on a 5 point scale where 1 was little or no improvement and 5 was maximum improvement.
Results: At the final treatment session and at the 6-week assessment, 20 of the 30 patients (67%) saw a fair to excellent degree of improvement, 7 (23%) had visible improvement and little or no improvement was seen in 3 (10%) patients. There were no unexpected side effects in any patients.
Conclusions: The dual toning technique using the 1064 nm Nd:YAG laser was safe and effective, and well-tolerated by all patents without anesthesia. Larger controlled studies are merited with more objective measurement techniques to confirm the results of this preliminary study.
Keywords: Micropulsed laser, Q-switched laser, pulse stacking, subcellular selective photothermolysis
Introduction
Melasma is an acquired cutaneous pigmentary disorder particularly but not exclusively seen in older females of the darker Oriental skin types, recognized as local bilateral areas of hypermelanosis seen as light- to dark-brown patches on sun-exposed facial skin.1–3) The patches can be large and homogeneous in distribution, appear as pigmented flecks, or present anywhere in between these extremes. The dyschromic lesions are found in the mandibular/mental regions and/or centro-facial and malar areas. There are basically two types of melasma classified by its distribution, and clearly visible under a Wood's lamp, even when latent and invisible to the naked eye: the epidermal type, existing in the epidermis; and the mixed type, existing in both the epidermis and dermis where the melanin particles exist in dermal melanophores. It is extremely unusual to see melasma existing only in the dermis. The actual etiology of melasma remains largely unknown, but its appearance has been associated with, among others, age, eccrine, paracrine and hormonal factors, genetic predisposition, pregnancy, use of oral contraception, stress, and exposure to solar or other UV radiation.1–4) More recently, the molecular signaling mechanisms responsible for upregulating and downregulating the genetic pathways leading to hypermelanogenesis have been identified including the Wnt pathway, c-kit and the role of dermal stem cells, although what actually triggers the respective signaling process remains to be elucidated.5,6)
A large variety of topical therapeutic approaches has been reported including bleaching agents (hydroquinone and kojic acids) and chemical peels (retinol, trichloroacetic or kojic acid), but although some success has been reported with these, the results are somewhat inconsistent with undesirable side effects such as unwanted pigmentary changes and dermatitis,7) and their efficacy appears to decrease with long-term use. In the past few years, intense pulsed light (IPL) systems have been reported in the treatment of mild melasma in the Japanese skin,8) and pigment-selective visible light lasers, but the results were less than expected with side effects related to excess photothermal damage to the epidermis and dermis associated with these systems, particularly post-inflammatory secondary hyperpigmentation (PIH).9–11) In the case of the Q-switched ruby laser, Tse et al.12) have reported that the Q-switched ruby laser showed no effect in the investigation of 20 patients, although he also found little effect with the Q-switched Nd:YAG at the parameters used. The Q-switched ruby laser has a wavelength of 694 nm, which has melanin as a chromophore. Despite this, poor results or recurrence in the early stages after treatment have been reported in most studies.12,13) Recently, a few reports have appeared on the use of the so-called ‘resurfacing lasers’ for melasma treatment (Er:YAG and CO2 plus Q-switched alexandrite lasers), but in darker skin types such as the Asian phenotypes, the risk of PIH is high.14) Even more recently, the modality of nonablative fractionated laser resurfacing was introduced in melasma treatment to help avoid the side effects of the full resurfacing systems, especially the prolonged downtime.15–18) Several treatments were required, however, with few patients showing total clearance and recurrence at 6 weeks to 2 months after the final treatment.
Goldberg and Metzler first suggested the concept of ‘laser toning’ in 1999,19) whereby multiple passes with a low-fluence Q-switched Nd:YAG laser produced beneficial changes in photoaged skin. In clinical practice, however, some more recent articles have reported that undesirable fibrosis in the papillary dermis is induced by Q-switched Nd:YAG laser toning.20) Hypopigmentation has also been reported in a series of Asian patients treated with laser toning.21) To avoid this, the so-called ‘Genesis technique’, which uses the quasi-long pulsed or micropulsed Nd:YAG laser mode, with pulse widths in the µs domain, may be the optimum adjunctive treatment method for laser toning, adding the advantage of skin rejuvenation employing multi-pass lasing with the benefit of a short patient downtime.22) Guidelines in published studies suggest a 5 mm spot size, 300 ms pulse duration and a fluence of around 13 J/cm2. The Genesis technique minimizes erythema and downtime, and maximizes the effect of skin rejuvenation with a reported increase in collagen synthesis following good neocollagenesis, and good dermal remodeling.18) The present study was designed to assess the efficacy of combining the Q-switched and micropulsed modes of the Nd:YAG laser, applied sequentially in the same treatment session, for the treatment of melasma in Fitzpatrick skin type IV Korean females.
Subjects and Methods
Thirty Korean females, ages ranging from 25 to 65 yr (mean 41.4 ± 11.96 yr) and all Fitzpatrick skin type IV were recruited for the study in the author's institute during the period of May 1st 2010 to April 30th 2011. Patient demographics are shown in Table 1. Nineteen subjects had melsama alone, and melasma complicated with another condition in 10 others (wrinkles and acne in 3 each, lentigines in 2 and ephelides and ABNOM [acquired bilateral nevus of Ohta-like macules] in 1 each). The remaining patient had latent melasma and wanted general skin rejuvenation. Having had the purpose and protocol of the study explained to them, all patients gave written informed consent to participate in the study, and for use of their clinical photography. The study protocol was in accordance with the World Medical Association-backed Declaration of Helsinki as amended in 2008.
Table 1: Patient demographics, disease breakdown and final score (VS).
| Case No | Age | Sex | Condition | VS |
| 1 | 45 | F | melasma, freckles | 4 |
| 2 | 38 | F | melasma | 5 |
| 3 | 40 | F | melasma | 2 |
| 4 | 48 | F | melasma | 3 |
| 5 | 62 | F | melasma, wrinkles | 2 |
| 6 | 53 | F | melasma | 4 |
| 7 | 52 | F | melasma, fine wrinkles | 3 |
| 8 | 28 | F | aging ? | 2 |
| 9 | 34 | F | melasma | 3 |
| 10 | 46 | F | melasma, ABNOM | 1 |
| 11 | 42 | F | melasma | 4 |
| 12 | 33 | F | acne, melasma | 4 |
| 13 | 35 | F | melasma | 3 |
| 14 | 36 | F | melasma | 4 |
| 15 | 34 | F | melasma | 4 |
| 16 | 27 | F | melasma, acne | 5 |
| 17 | 62 | F | melasma, SK, lentigines | 2 |
| 18 | 27 | F | melasma | 3 |
| 19 | 43 | F | melasma | 5 |
| 20 | 27 | F | melasma | 3 |
| 21 | 36 | F | melasma | 4 |
| 22 | 46 | F | melasma | 2 |
| 23 | 25 | F | melasma | 4 |
| 24 | 36 | F | melasma | 2 |
| 25 | 63 | F | melasma, wrinkles | 3 |
| 26 | 65 | F | melasma, lentigines | 1 |
| 27 | 33 | F | melasma | 3 |
| 28 | 52 | F | melasma | 4 |
| 29 | 43 | F | melasma | 2 |
| 30 | 28 | F | melasma, acne | 1 |
Visual scale (VS) gradings: 1, little or no improvement (0–10%);
2, Noticeable improvement (11–25%);
3, Fair improvement (26–50%); 4, Good improvement (51–75%); and 5, excellent improvement (>76%).
The treatment protocol was as follows: following thorough cleansing of the face, the 1064 nm Nd:YAG laser (SPECTRA™, Lutronic, Goyang, South Korea) was applied in the Q-switched mode, 5 ns pulse width, 1.2 J/cm2 pulse energy, 8 mm collimated handpiece, 10 Hz pulse repetition rate. Two to 3 passes were made over the entire face with a 15–20% overlap. Immediately after this, the laser was set in the micropulsed Spectra mode for the Genesis technique: 2 to 3 passes with a 300 µs pulse width, pulse energy 7.0 J/cm2, 5 mm collimated handpiece, rep rate 10 Hz. The lower pulse energy of 7 J/cm2 was selected rather than the 13 J/cm2 suggested in the previous literature because the Nd:YAG system used in the present study delivers a flat-top beam profile with higher efficacy than previous transverse beam modes. Multiple passes were made to stack pulses, with the desired endpoint being mild and even erythema of the whole face. No anesthesia was applied. A cooling pack was applied after the dual toning session, and patients were able to return immediately to their usual activities of daily living. Patients were instructed to apply a UVA/B sunscreen with an SPF of at least 30 on a daily basis, which was to be continued throughout the treatment and follow-up period. Patients received a total of 10 – 12 treatments repeated every other week.
Improvement was assessed from the clinical photography after the final session and at 6 weeks thereafter on a 5-point scale as follows: 1, little or no improvement (0–10%); 2, noticeable improvement (11–25%); 3, fair improvement (26–50%); 4, good improvement (51–75%); and 5, excellent improvement (>76%). Assessment was performed by two independent and experienced dermatologists.
Results
All patients completed the study successfully, and no adverse or unexpected side effects were seen in any patient. Erythema was mild and transient, lasting for 3–5 days and easily camouflaged with makeup. No patient reported excess pain during either component of the dual toning treatment, and no patient required anesthesia. A prickling or mild stinging was reported to be felt during the Q-switched mode and a mild heating sensation was often noticed during the Genesis technique.
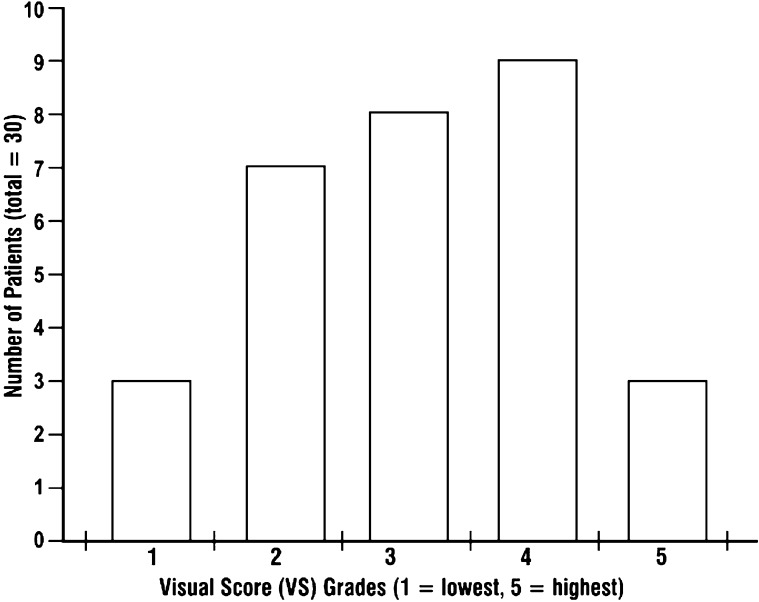
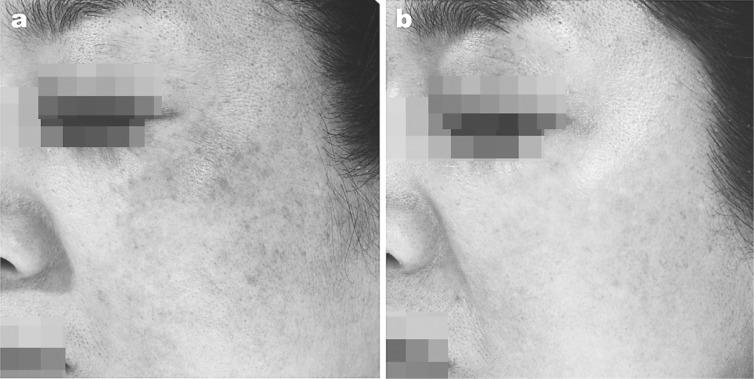
Of the 30 patients, 20 (67%) reported at least fair improvement, 7 (23%) had noticeable improvement and 3 (10%) had little or no improvement at their final treatment session (Table 1, Figure 1). These scores were maintained up till the 6-week assessment with no recurrence. All patients expressed willingness to repeat the treatment protocol if required. Furthermore, some patients reported significant improvement in the overall appearance of their skin following treatment, as typically seen in one 43-year-old female (patient No 19) with melasma at baseline and at 6 weeks after dual toning (VS of 5, Figure 2).
Fig. 1:
Visual scale grades (see the text for an explanation) broken down by patient numbers. The majority of the patients had a fair or better clearance of their melasma.
Fig. 2:
Clinical findings in a 43 year-old female patient (Patient No 19). a: Baseline condition. b: Findings 6 weeks after dual toning with the 1064 nm Nd:YAG laser, showing very good clearance of the melasma and improved general skin condition including reduced pore size and disappearance of the fine periocular lines.
Discussion
Parrish and Anderson's concept of selective photothermolysis (SP) forms the basis of most aspects of photosurgery,23) and calls for the selective destruction of pigments and the cells containing these pigments through the use of an appropriate wavelength, high peak powers and a pulse width shorter than the coefficient of thermal relaxation of the target materials. SP has been the cornerstone for the selective removal of pigmented lesions, including melasma. However, melasma in the Asian skin type can remain refractory to the normal SP approach since destruction of the melanin in the daughter keratinocytes and the melanosomes in the melanocytes is accompanied by destruction of, or at least severe damage to, the cells containing the pigment. Melanosmes in Korean melasma patients have been shown to be at stage IV, large and discrete,24) so SP-mediated destruction of the melanocyte containing them is more or less assured. However, repopulation of melanocytes from hair bulge stem cells can occur after 6 weeks with the recurrence of enlarged melanosome production,5) and new daughter keratinocytes are swiftly manufactured by the mother keratinocytes in the basal layer, ready to phagocytose melanin granules from the dendrites of the migrated melanocytes, resulting in treatment failure and repigmentation.
The high peak powers and ultrashort pulse width of the 5 ns Q-switched laser with low fluence offered an answer to this problem, and was demonstrated first in zebrafish25) and then in human melasma patients,24) whereby the target melanin was selectively destroyed in the melanophores in the zebrafish and human keratinocytes, melanocytes and dermal melanophores through the ultrashort acting radiant heat effect, but the cells containing the melanin were left alive. This was termed subcellular selective photothermolysis,24,25) and underpins the application of laser toning and its efficacy in the Asian skin without causing PIH, as inflammation is kept to a minimum due to the low pulse fluence.
Following sequential laser toning sessions resulting in subcellular selective photothermolysis, human melanocytes were shown through 3-D tomography and high-voltage electron microscopy to be melanosome-free but alive, and looked as if they had undergone a ‘dendrectomy’.24) Furthermore, levels of PAR-2, an essential substance mediating the transfer of melanin from melanocyte to daughter keratinocyte were decreased, likewise for tyrosinase-related proteins TRP-1 and −2, part of the oxidization process which turns clear melanosomes dark as they proceed along the dendrites. Taken together, these data suggest a much longer latency for the decreased production of melanin, but this has yet to be confirmed in a long-term follow-up although recurrence-free follow-up terms of 3 months are being reported.
Q-switched laser toning quite obviously affects the epidermis and very superficial dermis, but when this mode is combined with the micropulsed 300 µs mode of the Nd:YAG with multiple passes and pulse stacking, a deep-reaching tissue heating is additionally achieved with a minimally invasive approach. The micropulsed mode delivers a controlled photothermal effect into the deep dermis, which is enhanced by the pulse stacking and induces the wound healing process together with heat shock proteins, reduction of proinflammatory interleukin (IL)8 and the induction of wound healing mediator transforming growth factor (TGF)-ß.22) Active collagenesis results, followed by the remodeling process so the dual toning technique not only removes the melasma, it also tones and refreshes the patient's skin.
To go one step further, the enhanced efficacy of dual toning followed by TriLuma® cream has been reported.26) From my recent experience, this approach can be enhanced even more with the addition of a 50% glycolic acid peel and application of Kligman's formula after the dual toning session, what the second author (JHK) refers to as his modified Triple Combination Treatment, and an ongoing study will report on this in detail with an extended followup period.
Another potential adjunctive technique which may well add to the proven efficacy of the dual toning is the application immediately after the procedure of 830 nm LED phototherapy, which has been shown both to lighten Asian skin and also to have good efficacy in skin rejuvenation.27) Trials of this totally non-invasive adjunctive approach are planned in the near future.
This study had four limitations. First, although prospective, it was not controlled and that must be addressed in future studies, with the split-face approach being the ideal: however, it was only a preliminary study, and the results are sturdy enough to merit future studies with a controlled element. Secondly, efficacy was made based on visual assessment of the clinical photography. Future studies should include histopathological assessments, should use in addition an objective machine assessment such as the Mexameter™ and/or a Dermatospectrometer, and should also employ the melasma area severity index (MASI) scale. Thirdly, statistical examination of the results in larger patient populations will add power to the findings. Fourthly, the 6-week period of this preliminary study is potentially too short to rule out the possibility of later recurrence. However, from the authors' and others personal experience, with other treatment approaches recurrence is often seen within this period. A much longer follow-up period will be a requisite of following studies, in combination with rectifying the other limitations listed above.
Conclusions
The dual toning technique offers a good solution to the problem of treating melasma in the Asian skin, achieving both bleaching or whitening of the skin together with skin rejuvenation to restore a youthful appearance and well-organized architecture to both the dermis and very importantly, the epidermis. The approach is effective, side-effect free, well-tolerated and minimally invasive with practically no downtime for the patient. The efficacy may be improved even further with adjunctive techniques such as peels, creams or LED phototherapy.
References
- 1.Newcomer VD, Lindbert MC, Stenbert TH: A melanosis of the face (‘chloasma’). Arch Dermatol, 1961. 83: 284–297 [DOI] [PubMed] [Google Scholar]
- 2.Kang WH, Yoon KH, Lee E-S, Kim J, Lee KB. et al: Melasma: histopathological characteristics in 56 Korean patients. British J Derm, 2002. 146: 228–237 [DOI] [PubMed] [Google Scholar]
- 3.Ortonne J-P, Bisset DL: Latest insights into skin hyperpigmentation. J Invest Dermatol Symp Proc, 2008. 13: 10–14 [DOI] [PubMed] [Google Scholar]
- 4.Kim H, Kim YC, Lee ES, Kang HY: The vascular characteristics of melasma. J Dermatol Science, 2007. 46: 111–116 [DOI] [PubMed] [Google Scholar]
- 5.Kang HY, Hwang JS, Lee JY, Ahn JH, Kim JY. et al: The dermal stem cell factor and c-kit are overexpressed in melasma. Br J Dermatol, 2006. 154: 1094–1099 [DOI] [PubMed] [Google Scholar]
- 6.Kang HY, Suzuki I, Lee DJ, Ha J, Reiniche P. et al: Transcriptional Profiling Shows Altered Expression of Wnt Pathway- and Lipid Metabolism-Related Genes as Well as Melanogenesis-Related Genes in Melasma. J Invest Dermatol, 2011 May 12. [Epub ahead of print] [DOI] [PubMed]
- 7.Gupta AK, Gover MD, Nouri K, Taylor S. The treatment of melasma: A review of clinical trials. J Am Acad Dermatol, 2006. 55: 1048–1065 [DOI] [PubMed] [Google Scholar]
- 8.Negishi K, Kushikata N, Tezuka Y, Takeuchi K, Miyamoto E, Wakamatsu S: Study of the incidence and nature of “very subtle epidermal melasma” in relation to intense pulsed light treatment. Dermatol Surg 2004; 30:881–886 [DOI] [PubMed] [Google Scholar]
- 9.Taylor CR, Anderson RR. Ineffective treatment of refractory melasma and postinflammatory hyperpigmentation by Q-switched ruby laser. J Dermatol Surg Oncol 1994; 20:592–597 [DOI] [PubMed] [Google Scholar]
- 10.Stratigos AJS, Dover JS, Arndt KA: Laser treatment of pigmented lesions-2000. How far have we gone? Arch Dermatol, 2000. 136: 915–921 [DOI] [PubMed] [Google Scholar]
- 11.Railan D, Kilmer S: treatment of benign pigmented cutaneous lesions. Cutaneous and Cosmetic laser Surgery. Ed. Goldman MP. ed. Mosby Elservier Inc. Phyladelphia (USA) 2006: 93–108 [Google Scholar]
- 12.Tse Y, Levine VJ, McClain SA. et al: The removal of cutaneous pigmented lesions with the Q-switched ruby laser and the Q-switched neodymium: yttrium- aluminum- garnet laser: a comparative study. J Dermatol Surg Oncol 1994. 20: 795–800 [DOI] [PubMed] [Google Scholar]
- 13.Taylor CR, Anderson RR. Ineffective treatment of refractory melasma and postinflammatory hyperpigmentation by Q-switched ruby laser. J Dermatol Surg Oncol 1994. 20: 592–597 [DOI] [PubMed] [Google Scholar]
- 14.Angsuwarangsee A, Polnikorn N: Combined Ultrapulse CO2 laser and Q-switched alexandrite laser compared with Q-switched alexandrite laser alone for refractory melasma. Dermatol Surg, 2003. 29: 59–64 [DOI] [PubMed] [Google Scholar]
- 15.Rokhsar CK, Fitzpatrick RE,. The treatment of melasma with fractional photothermolysis: A pilot study. Dermatol Surg, 2005. 31: 1645–1650 [DOI] [PubMed] [Google Scholar]
- 16.Tannous ZS, Astner S. Utilizing fractional resurfacing in the treatment of therapy-resistant melasma. J Cosmet Laser Ther, 2005. 7: 39–43 [DOI] [PubMed] [Google Scholar]
- 17.Goldberg DJ, Berlin AI, Phelps R. Histologic and ultrastructural analysis of melasma after fractional resurfacing. Lasers Surg Med, 2008. 40: 134–138 [DOI] [PubMed] [Google Scholar]
- 18.Barysch M, Rümmelein B, Kolm I, Karpova M, et al. (2011): Split-face study of melasma patients treated with non-ablative fractionated photothermolysis (1540 nm). J Eur Acad Dermatol Venereol. 2011 Apr 27. [Epub ahead of print] [DOI] [PubMed]
- 19.Goldberg D, Metzler C. (1999): Skin resurfacing utilizing a low-fluence Nd:YAG laser. J Cutan Laser Ther, 1 23–27 [DOI] [PubMed] [Google Scholar]
- 20.Goldberg DJ, Silapunt S. (2001): Histologic evaluation of a Q-switched Nd:YAG laser in the non ablative treatment of wrinkles. Dermatol Surg, Dermatol Surg: 744–746 [DOI] [PubMed] [Google Scholar]
- 21.Chan NP, Ho SG, Shek SY, Yeung CK, Chan HH. (2010): A case series of facial depigmentation associated with low fluence Q-switched 1,064 nm Nd:YAG laser for skin rejuvenation and melasma. Lasers Surg Med, Lasers Surg Med: 712–719 [DOI] [PubMed] [Google Scholar]
- 22.Schmults CD, Phelps R, Goldberg DJ. (2004): Nonablative facial remodeling: erythema reduction and histologic evidence of new collagen formation using a 300-microsecond 1064-nm Nd:YAG laser. Arch Dermatol, Arch Dermatol: 1373–1376 [DOI] [PubMed] [Google Scholar]
- 23.Parrish JA, Anderson RR, Harrist T. et al (1983): Selective thermal effects with pulsed irradiation from lasers: from organ to organelle. J Invest Dermatol, 80 (Suppl): 75s–80s [PubMed] [Google Scholar]
- 24.Mun JY, Jeong SY, Kim JH, Han SS, Kim IH. (2011) A low fluence Q-switched Nd:YAG laser modifies the 3D structure of melanocyte and ultrastructure of melanosome by subcellular-selective photothermolysis. J Electron Microsc (Tokyo), J Electron Microsc (Tokyo): 11–18 Epub 2010 Oct 11. [DOI] [PubMed] [Google Scholar]
- 25.Kim JH, Kim H, Park HC, Kim IH. (2010): Subcellular Selective Photothermolysis of Melanosomes in Adult Zebrafish Skin Following 1064-nm Q-Switched Nd:YAG Laser Irradiation. J Invest Derm, 130: 2333–2335 Epub 13 May 2010. [DOI] [PubMed] [Google Scholar]
- 26.Jeong SY, Shin JB, Yeo UC, Kim WS, Kim IH. (2010): Low-fluence Q-switched neodymiumdoped yttrium aluminum garnet laser for melasma with pre- or post-treatment triple combination cream. Dermatol Surg, Dermatol Surg: 909–918 Epub 2010 Apr 1. [DOI] [PubMed] [Google Scholar]
- 27.Lee SY, Park KH, Choi JW, Kwon JK, et al.: A prospective, randomized, placebo-controlled, double-blinded, and split-face clinical study on LED phototherapy for skin rejuvenation: Clinical, profilometric, histologic, ultrastructural, and biochemical evaluations and comparison of three different treatment settings. J Photochem Photobiol (B), 2007. 88: 51–67 (available online as Epub ahead of print). [DOI] [PubMed] [Google Scholar]