Abstract
Background and aims: Enlarged facial pores remain one of the major cosmetic concerns among Asian females. This study attempted to assess and compare the efficacy of a combination of the Q-switched and quasi long-pulsed (micropulsed) Nd:YAG laser to reduce the size of the enlarged pores with and without an exogenous photoenhancer.
Methods: In twenty five female subjects mean age 34.04 yr and skin type II-IV, a carbon lotion as a photoenhancer was applied on one side of the face (Method 1) and the other side was used as the control (Method 2). The entire face was then treated with a single pass of the 1064 nm Nd:YAG laser in the micropulsed mode, pulse fluence and width of 2.3 J/cm2 and 300 µsec, respectively. Multiple passes were then delivered in the Q-switched mode (2.5 J/cm2 and 5 nsec).
Results: Three weeks after the final treatment, 75% of the subjects showed improvement with method 1 whereas 67% showed improvement with method 2. No adverse side effects were reported with either method.
Conclusions: Although histological confirmation was not performed, we were able to prove both subjectively and objectively that the use of the combination of the micropulsed and Q-switched modes of the Nd:YAG laser was useful in reducing pore size, and that the photoenhancer improved the efficacy.
Keywords: Nd:YAG laser, quasi long-pulsed mode, Q-switched mode, enlarged pores, exogenous photoenhancer
Introduction
Enlarged or dilated pores, usually considered as an aspect of photoaging in the literature,1–6) are of significant cosmetic concern in Asians. However, the number of patients with enlarged pores who seek treatment has increased recently and they are usually young without any signs photodamage. A variety of different treatments have been used for the reduction of pore size, including intense pulsed light,1,2) tazarotene cream,3) radiofrequency,4) oral isotretinoin,5) micro-dermabrasion,6) isotretinoin iontophoresis,7) and glycolic acid peeling.8) However, these reports did not focus on pore size but regarded them simply as a component of photoaging1–6) or only partially mentioned the reduction of pore size in the context of the improvement of acne scarring.7,8)
The Q-switched Nd:YAG laser has been used in cosmetic laser dermatology for pigmented and vascular lesions, and for the removal of tattoo or unwanted hair, when used in combination with an exogenously applied photoenhancer, namely a topical carbon suspension.9,10) In addition, it has been shown that the 1064 nm Q-switched Nd:YAG laser provided satisfactory clinical results in the treatment of periocular and perioral rhytides.9) Another clinical study using topical carbon solution showed an improvement in post-acne scarring and facial wrinkles.11) At a meeting of the American Society of Lasers in Medicine and Surgery (ASLMS), Fujimoto reported that topical carbon suspension-assisted Nd:YAG laser treatment combining the 300 µm micropulse and Q-switched modes offered a safe cosmetic method of improving skin texture, especially pore size reduction.12) In a case report on the combined modes of the Nd:YAG laser with a photoenhancer for active acne treatment, Chun and Calderhead stated that pore size was also reduced in addition to successful improvement of the acne lesions.13) However, neither of these studies used objective parameters to measure the pore size. The purpose of our study was to evaluate the efficacy of a technique combining the Q-switched and quasi long-pulsed Nd:YAG laser modes in pore size reduction, with and without an exogenous photoenhancer, but employing an objective measurement of pore size improvement in addition to the usual subjective methods.
METHODS
Patients
Twenty-five female volunteers with enlarged pores were included in this study. Their mean age was 34.04 years, ranging from 25 to 44. The volunteers had Fitzpatrick skin types III-IV. The whole face was treated with a dual mode 1064 nm Nd:YAG laser (SPECTRA, Lutronic Corp., Goyang, South Korea), except for the upper eyelids, eyebrows, and lips. Exclusion criteria consisted of active herpes simplex or herpes zoster, bacterial folliculitis, current use of isotretinoin, history of keloid scarring, and photosensitivity disorders. Informed consent was obtained from each patient prior to participation for participation in the study and for the use of clinical photography. The study was approved by the Ethics Committee of Yonsei University School of Medicine and carried out in accordance with the principles of Good Clinical Practice (GCP) originating from the World Medical Association's Declaration of Helsinki.
Treatment
Preoperative skin preparation was performed with a sheet type nose pack (Charcoal nose pack, Nesura, Korea). Following a thorough face wash, the nose and cheeks were left wet. With dry hands, a clear sheet of film was then applied to the wet areas which adhered completely, conforming to the contour of the areas. The sheet was allowed to dry for about 20 minutes to remove as many keratotic plugs from enlarged pores as possible. After the removal of the sheet, a warm wet towel was placed on the patient's face for 1 minute to open up the pores.
Topical carbon suspension as a photoenhancer was then applied to one half of the face (Method 1), except the upper eyelid, eyebrow, and lips. Table 1 shows the components of the lotion. The photoenhancer was not applied to the other side (Method 2). The carbon suspension was massaged into the skin and left for 20 min to be absorbed. Excess solution was then gently wiped away with a sheet of gauze.
Table 1: Details of the carbon lotion photoenhancer and source laboratory.
| Item | Comment |
| Laboratory | Telsar, Wood River IL USA |
| FDA site reg. No | 1423368 |
| Description | Facial peel lotion (Part No Z-10102-90017) |
| Ingredients | Light mineral oil (Pariffinum liquidum, 90% by volume) |
| Graphite (40 µm, 10% by volume) | |
Laser treatment was then performed over both sides of the face and nose with the dual mode 1064 nm Nd:YAG laser, offering both a micropulsed mode, pulse width 300 µs and pulse fluence 2.3 J/cm2, and a Q-switched mode, pulse width 5 ns at the same pulse fluence. Both modes were delivered through the same 7 mm collimated handpiece at a pulse repetition rate of 10 Hz. Eyelids were protected with external plastic shields. As the first step, laser treatment in one pass was performed over the entire face in the micropulsed mode, avoiding beam overlap as much as possible. Then in the Q-switched mode multiple passes were delivered with an overlap of around 10% − 20%. At this high peak power setting the carbon particles literally exploded, producing a clearly audible cracking or popping sound with each single shot until the carbon particles were completely removed and the popping sound could no longer be heard. After the treatment, the face was cooled down with cold compresses. Patients were treated 5 times at a 3 week interval.
Assessment
Photographs were taken using a digital camera (CoolPix 990, Nikon, Japan) prior to each treatment and 3 and 12 weeks after the last treatment. In addition, pictures of the nose and cheek surfaces were taken with a dermoscope video camera (Coscam CCL-205, Sometech Cosmetic, Korea) at a magnification of × 100 and at a fixed distance. Using the magnified images, 30 to 40 randomly selected enlarged pores from each side were measured with an image analysis program (Simple PCIp®, Compix Inc., C-Imaging Systems, PA, USA), using the program-calculated area as an indicator of the pore size. Reduction in pore size was classified under one of the following five categories: no improvement, 1–25%, 26–50%, 51–75%, or 76–100%, and all the participants were rated at 3 and 12 weeks after the final treatment. Other parameters were also checked: skin moisture content (hydration) with a Corneometer (CM 820 PC, Courage-Khazaka, Köln, Germany); sebum expression levels with a Sebumeter (SM 815, Courage-Khazaka,); and degree of melanin synthesis with a Mexameter14) (MX-18, Courage-Khazaka) at baseline, and at 3 and 12 weeks after the last treatment. Subjects were asked to evaluate subjectively the degree of change visible on their skin for pore size reduction and state their preference of treatment between Methods 1 and 2, as well as reporting any adverse outcomes. At the 12-week assessment, patients completed an anonymous satisfaction questionnaire in which they rated their perceived improvement and satisfaction on a 1–5 scale (1, worse; 2, little or no improvement; 3, mild improvement; 4, moderate improvement; and 5, significant improvement).
Statistical analysis
ANOVA, ANCOVA, and paired t-tests were used to compare pore size reduction, sebum production, pigmentation, and hydration at baseline, and at 3 and 12 weeks after the final treatment.
Results
Degree of improvement
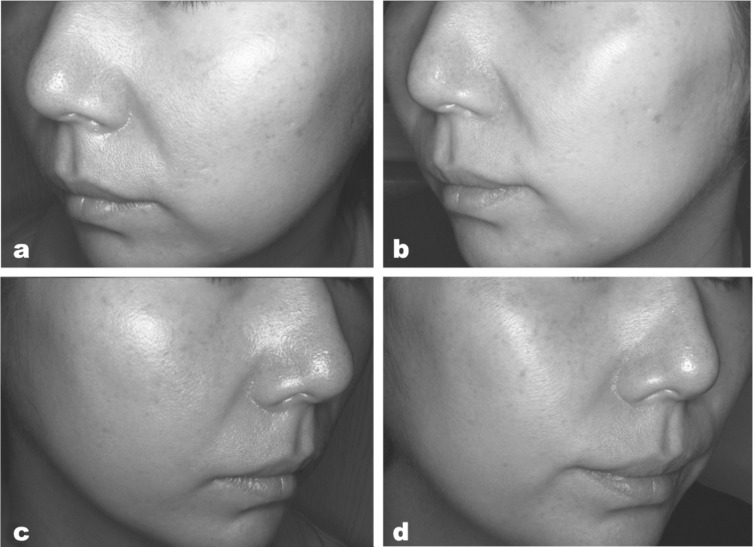
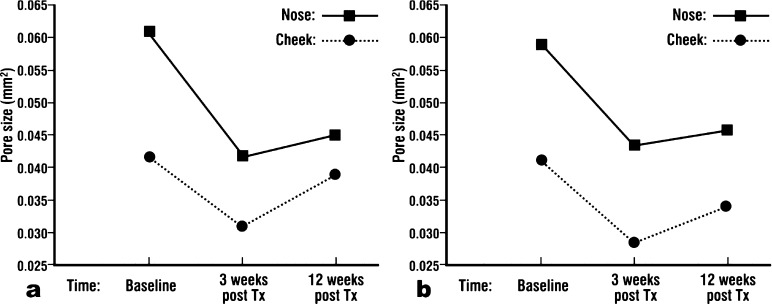
Of the 25 subjects who participated in this study, 24 completed the series of treatments and five were unavailable to answer the questionnaire 12 weeks after the last treatment. Figure 1 illustrates the clinical findings for both Methods in a representative subject who showed an excellent response. As can be seen in Table 2, 75% of the subjects treated with method 1 (18/24) showed more than 50% improvement whereas 67% of the subjects treated with method 2 (16/24) showed over 50% improvement. Figure 2a demonstrates that a statistically significant (P<0.001) reduction of pore size was achieved using method 1 three weeks after the last treatment, but the pore size increased somewhat 12 weeks after the last treatment. Although the increase was statistically significant when compared to the findings 3 weeks after the last treatment, the maintenance of improvement was also significant as compared to the pore sizes at baseline (P<0.05). Method 2 also resulted in a similar pattern of statistically significant improvement and re-enlargement (Figure 2a). The pore size reduction tended to be greater on the nose than the cheeks (Figure 3a, 3b).
Fig. 1:
Typical clinical photography in a subject whose results were rated as excellent. Significant visual improvement in the pore size is seen for both methods before treatment (a) and 3 weeks after the final treatment (b) using Method 1 (combined modes with enhancer); and before treatment (c) and 3 weeks after the final treatment (d) using method 2 (combined modes, no enhancer). Note also the lower reflectance from the cheek and nose in the posttreatment findings for both Methods, indicative of lowered sebum production.
Table 2: Comparison of improvement achieved by Methods 1 and 2 at 3 weeks after last treatment.
| Rating | Method 1 | Method 2 |
| Improvement | 18 (75%) | 16 (67%) |
| 76–100% | 2 (8%) | 4 (17%) |
| 51–75% | 10 (42%) | 9 (38%) |
| 26–50% | 5 (21%) | 2 (8%) |
| 1–25% | 1 (4%) | 1 (4%) |
| No improvement | 6 (25%) | 8 (33%) |
| Total | 24 (100%) | 24 (100%) |
Fig. 2:
Decrease in mean pore size compared between Method 1 and Method 2. a: Measurement of mean pore size (based on the image analysis program-computes pore area as described in the text) before treatment, and at 3 and 12 weeks after final treatment using Method 1. b: Measurement of pore size before treatment, and at 3 and 12 weeks after the final treatment using Method 2.
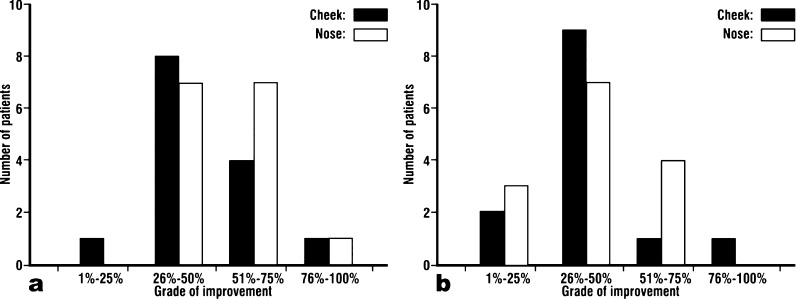
Fig. 3:
Grade of improvement at 3 weeks compared between Method 1 (a) and Method 2 (b).
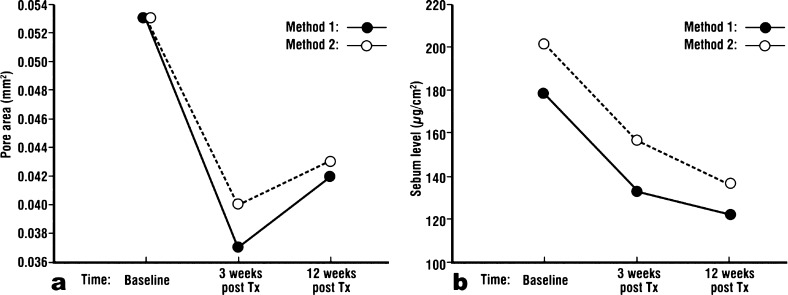
Comparison of the two methods
When the two methods were compared, Method 1 showed more improvement than method 2 at 3 weeks after the last treatment, but neither could maintain the level of improvement until 12 weeks after the final treatment (Figure 4), although the level of improvement at the 12-week assessment was still significantly better in both modes than at baseline.
Fig. 4:
a: Measurement of pore size at baseline, 3 and 12 weeks after the final treatment comparing Method 1 and Method 2. b: Sebum levels compared for Methods 1 and 2 measured with a Sebumeter at baseline, 3 and 12 weeks after the final treatment.
Mexameter, Corneometer, and Sebumeter measurements
M (Melanin) and E (Erythema) values measured by the Mexameter did not show any difference before and after the treatment for either method. However, sebum production after both treatments decreased significantly. Furthermore, unlike pore size, sebum production 12 weeks after the last treatment was less than 3 weeks after the last treatment (Figure 5). Corneometer readings for areas treated with both Method 1 and 2 showed a statistically significant decrease 12 weeks after the last treatment compared to before the treatment. However, no decrease was observed 3 weeks after the last treatment.
Fig. 5:
Patient satisfaction evaluated at 3 and 12 weeks after the final treatment.
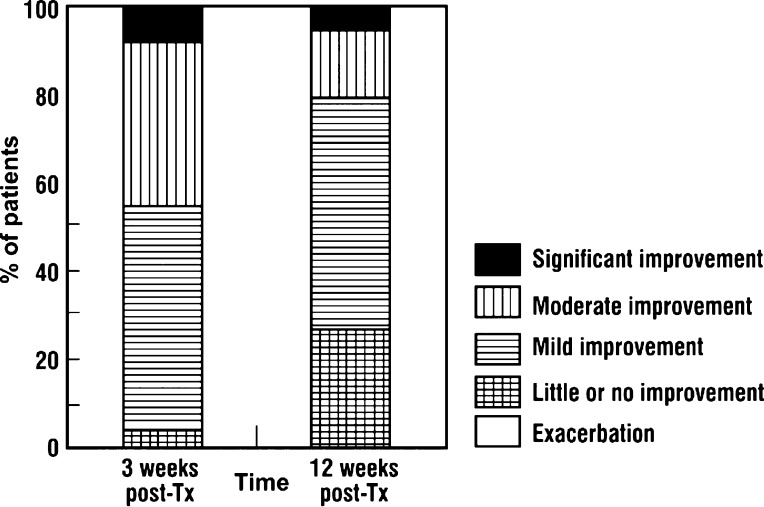
Patient Satisfaction
Upon being asked which treatment they preferred, taking into account overall effectiveness and discomfort, at 3 weeks after the last treatment, 23 subjects (95.8%) reported at least a mild improvement (Figure 5). Twenty-two subjects (91.7%) reported they would recommend this treatment to others. Twenty of the 24 subjects (83%) stated a preference for the carbon suspension-assisted method (Method 1), while the remaining subjects (17%) stated that both methods seemed to have the same degree of improvement.
Complications
Whereas immediate erythema and swelling were common on the side treated with Method 1, these conditions generally resolved within 12–48 hours after the treatment. Mild desquamation developed 3 days after the treatment and resolved within 7 days. These side effects were so mild that subjects did not experience any limitations in their daily work or social activities. Seven subjects reported transient vesicle formation on the side treated with Method 1. Folliculitis developed in three patients and aggravation of the pre-existing melasma occurred in one subject, but they were observed on both sides, independent of the treatment methods.
DISCUSSION
Recent economic development has increased the number of people who desire cosmetic procedures for better appearance and enlarged facial pores are one of the most common cosmetic problems in Asian adults. However, previous reports regarded enlarged pores as a phenomenon of photoaging1–6) and some reports briefly mentioned the pore size reduction effect while focusing on the acne scar treatment.7,8) Admittedly, enlarged pores are one manifestation of photoaging. Solar elastotic collagen damage produces a sallow skin tone, dilated pore structure, crepe-paper like inelasticity of the eyelids and rhytids.15) However, patients with enlarged pores do not always have other photoaging phenotypes, such as pigmented lesions, vascular lesions, or rhytides. In general, Korean women are reluctant to expose themselves to sunlight due to easy development of melasma and, therefore, severe photo-damage in the younger population is a rarity. Our subjects were all in the younger age groups with no evident manifestations of photodamage. This study was intended to objectively investigate the efficacy of a new application of a combination of the Q-switched and micropulsed Nd:YAG laser for the treatment of enlarged pores. We took pictures at magnification × 100 with a dermoscopic video camera and then measured and analyzed the areas of 30 to 40 randomly selected enlarged pores from each side with an image analysis program. To validate the accuracy of this method, we measured pores of 20 patients who did not receive any treatment and measured pore sizes 4 times in 2-weeks interval. There was no statistical difference in the baseline pore size among the 4 measurements (p<0.05, data not shown).
Two treatment methods, one with and one without topical carbon suspension, were used. The results showed that both methods were very effective overall, showing a significant reduction of pore size in about 70% of the subjects. Our results also showed that using topical carbon suspension was more effective in reducing the pore size, and the majority of the participants also preferred using it. The pulse fluence of 2.3 J/cm2 for both Methods 1 and 2 used in this study was the maximally tolerable dose without causing an actual burn. The order of treatment deserves comment. Under normal circumstances, it would make photobiological sense to start with the 3 ns Q-switched mode and follow with the 300 µs micropulsed mode, the former having its greatest photothermal effect on the epidermis and very superficial dermis, and the latter in the deeper dermis. However, we were comparing the combination with and without a carbon lotion photoenhancer, and as was shown in the previous studies employing such an enhancer with a Q-switched beam,9–13) the 3 ns beam removed the carbon particles completely. Moreover, the micropulsed beam had its penetration limited by the presence of the photoenhancer, but left it intact on the stratum corneum. Thus we applied the micropulsed beam first, followed by the Q-switched beam in both arms of the study as the study was in fact comparing the effect with and without the carbon particles, so we needed to retain the same order for both arms.
Although all subjects experienced erythema and desquamation, recovery occurred within a week and the conditions were mild so as not to disrupt everyday life. However, due to the hemifacial nature of this study, the nasal tip was prone to overlapping laser beams from the two modes which occasionally resulted in blisters. In a subject with melasma, careful adjustment of the laser fluence is needed as melasma can be aggravated, which happened in one of our subjects. Overall, a series of laser treatments using the combined modes with and without the carbon lotion photoenhancer is safe and readily tolerated by subjects with minimal adverse effects, minimal downtime, and no risk of scarring.
Though the exact mechanism of the effect of the laser is not clear, the mechanism of method 1 is assumed to be as follows. The Nd:YAG laser at 1064 nm has no specific really strong chromophore in the skin although the major absorptive chromophore in the epidermis is melanin, which weakly absorbs laser energy at this wavelength. The topical carbon suspension contains purified carbon particles in a base of mineral oil and it serves as an exogenous artificial chromophore, or photoenhancer.13) Nd:YAG laser light has been shown to be strongly absorbed by carbon in contrast to other cutaneous chromophores such as melanin.10) When carbon suspension is applied and excess solution is wiped away, the remaining carbon particles remain as thin film on the stratum corneum and larger numbers are lodged in the enlarged pores. At the Q-switched setting used in the present study, the peak irradiance per pulse was 520 MW/cm2, giving an extremely peak power per pulse of around 200 MW. When carbon particles absorb high peak powers of laser energy in an ultrashort pulse such as 5 ns with very high photon intensity in the MW/cm2 range, they undergo a rapid temperature rise with radiant head-mediated explosive destruction: the particles are literally blasted off the skin, thereby generating kinetic energy which damages the stratum corneum, the pore walls and surrounding structures, resulting in general freshening of the skin and tightening of the pores. This proposed mechanism is identical to previous reports, in which unwanted hairs were removed with an Nd:YAG laser used with a topical carbon suspension as a photoenhancer.10,20) In addition, in the present study sebum levels also significantly decreased after laser treatment and this effect was more prominent in the area treated by Method 1. However, Method 2 also showed good efficacy and effective decrease in sebum production but the mechanism of this direct photothermal effect of laser on the pore size reduction and sebum production remains to be fully elucidated As mentioned before, the micropulsed mode of the 1064-nm Nd:YAG laser has been used clinically to improve rhytid formation.9) Histological evaluation of the effect of this laser revealed that collagen formation occurred at the level of the reticular dermis.16) Other reports evaluating Q-switched Nd:YAG laser treatment showed slight fibrosis in the superficial papillary dermis with unremarkable epidermal changes.17) Recently, Schmults et al. reported that microsecond Nd:YAG lasers, with an identical pulse duration to the micropulsed Nd:YAG laser mode in the present study, could also produce new collagen formation in the papillary dermis.18) No previous reports mentioned changes in or around the hair follicles. Therefore, we suggest that collagen formation in the reticular dermis or superficial papillary dermis could shrink pores, especially due to perifollicular collagen formation. Further investigation to confirm this effect using histologic study is needed. One limitation of the present study is that we did not perform any histopathological analysis.
We combined the micropulsed and the Q-switched modes of the Nd:YAG laser instead of using either mode in monotherapy, because we thought the combination treatment would result in more improvement. The pulse duration of quasi long-pulsed Nd:YAG laser was 300 µsec, whereas that of Q-switched Nd:YAG laser was 5 nsec. As two different pulse durations were used, the reaction of surrounding tissue was thought to be different for each sequential mode. Chun and Calderhead postulated a purely photothermal effect occurred in the micropulsed mode, especially with the addition of the photoenhancer, with formation of heat shock proteins in the deeper dermis. This was followed by a pure explosive radiant heat effect with photoacoustic and photoosmotic reactions inducing mild damage at the stratum corneum and pore walls.13)
Chryslain et al reported that dermal coagulation depth was linearly related to the function of pulse duration.17) Therefore, we assumed that the micropulsed laser beam might react with deeper dermis and the Q-switched laser beam might react with the more superficial dermis. In addition, we suggest an association between the size of the carbon particles as exogenous chromophores and the pulse duration of the laser. Due to the thermal relaxation time, the micropulsed laser beam causes a secondary photothermal effect conducted from the heated, but intact, carbon particles into the deeper dermis, whereas the Q-switched mode causes explosion and complete clearance of the carbon particles. Accordingly, the synergy of the two different mechanisms was thought to increase the efficacy of the combination treatment.
Though it is not known whether additional treatments beyond the five described in this study would produce substantially greater results, our results suggest that some form of maintenance therapy would be desirable, since the pore size at 12 weeks was larger than at 3 weeks after the last treatment, although still smaller than at baseline.
CONCLUSIONS
Based on this pilot study, we have determined that the combination of the micropulsed and Q-switched modes of the 1064 nm Nd:YAG laser was safe and effective in reducing the size of enlarged pores, and the use of a topical carbon suspension as a photoenhancer augmented the effect of the laser.
REFERENCES
- 1.Brazil J, Owens P. (2003): Long-term clinical results of IPL photorejuvenation. J Cosmet Laser Ther; 5: 168–74 [DOI] [PubMed] [Google Scholar]
- 2.Bitter PH. (2000): Noninvasive rejuvenation of photodamaged skin using serial, full-face intense pulsed light treatments. Dermatol Surg; 26: 835–42 [DOI] [PubMed] [Google Scholar]
- 3.Phillips TJ, Gottlieb AB, Leyden JJ. et al (2002): Efficacy of 0.1% tazarotene cream for the treatment of photodamage: a 12-month multicenter, randomized trial. Arch Dermatol; 138: 1486–93 [DOI] [PubMed] [Google Scholar]
- 4.Abraham M, Chiang S, Keller G. et al. Clinical evaluation of non-ablative radiofrequency facial rejuvenation. Cosmet Laser Ther 2004; 6: 136–44 [DOI] [PubMed] [Google Scholar]
- 5.Hernandez-Perez E, Khawaja HA, Alvarez TY. (2000): Oral isotretinoin as part of the treatment of cutaneous aging. Dermatol Surg; 26: 649–52 [DOI] [PubMed] [Google Scholar]
- 6.Perez E, Ibiette E. (2001): Gross and microscopic findings in patients undergoing microdermabrasion for facial rejuvenation. Dermatol Surg; 27: 637–40 [DOI] [PubMed] [Google Scholar]
- 7.Schmidt JB, Donath P, Hannes J. et al (1999): Tretinoin-iontophoresis in atrophic acne scars. Int J Dermatol; 38: 149–53 [DOI] [PubMed] [Google Scholar]
- 8.Grimes PE. (1999): The safety and efficacy of salicylic acid chemical peels in darker racial-ethnic groups. Dermatol Surg; 25: 18–22 [DOI] [PubMed] [Google Scholar]
- 9.Goldberg DJ, Whitworth J. (1997): Laser skin resurfacing with the Q-switched Nd:YAG laser. Dermatol Surg; 23: 903–6 [DOI] [PubMed] [Google Scholar]
- 10.Goldberg DJ, Littler CM, Wheeland RG. (1997): Topical suspension-assisted Q-switched Nd:YAG laser hair removal. Dermatol Surg; 23: 741–5 [DOI] [PubMed] [Google Scholar]
- 11.Cisneros JL, Rio R, Palou J. (1998): The Q-switched neodymium (Nd):YAG laser with quadruple frequency. Clinical histological evaluation of facial resurfacing using different wavelengths. Dermatol Surg; 24: 345–350 [PubMed] [Google Scholar]
- 12.Fujimoto T, Terashima Y, Tsuji J. (2004): Non-ablative skin rejuvenation utilizing a combination of Q-switched and long pulse Nd:YAG laser, assisted with carbon suspended lotion. Lasers. Surg. Med. Supplement 16, No 59 [Google Scholar]
- 13.Chun SI, Calderhead RG. (2011): Carbon assisted Q-switched Nd:YAG laser treatment with two different sets of pulse width parameters offers a useful treatment modality for severe inflammatory acne: a case report. Photomed Laser Surg; Photomed Laser Surg;: 131–135 Epub Dec 2010. [DOI] [PubMed] [Google Scholar]
- 14.Lipper GM, Anderson RR. Lasers in Dermatology. In: Fitzpatrick's Dermatology in General Medicine. (Freedberg IM, Eisen AZ, Wolff K, et al), 6th edn, vol 2 New York: McGraw Hill, 2003; 2493–515 [Google Scholar]
- 15.Yaar M, Gilchrest BA. Aging of skin. In: Fitzpatrick's Dermatology in General Medicine. (Freedberg IM, Eisen AZ, Wolff K, et al), 6th edn, vol 2 New York: McGraw Hill, 2003; 1386–98 [Google Scholar]
- 16.Dayan S, Damrose JF, Bhattacharyya TK. et al. Histological evaluations following 1,064-nm Nd:YAG laser resurfacing. Lasers in Surgery and Medicine 2003; 33: 126–31 [DOI] [PubMed] [Google Scholar]
- 17.Goldberg DJ, Silapunt S. (2001): Histologic evaluation of a Q-switched Nd:YAG laser in the nonablative treatment of wrinkles. Dermatol Surg; 27: 744–6 [DOI] [PubMed] [Google Scholar]
- 18.Schmults CD, Phelps R, Goldberg DJ. (2004): Nonablative facial remodeling: erythema reduction and histologic evidence of new collagen formation using a 300-microsecond 1064-nm Nd:YAG laser. Arch Dermatol; 140: 1373–6 [DOI] [PubMed] [Google Scholar]
- 19.Sumian CC, Pitre FB, Gauthier BE. et al (1999): Laser skin resurfacing using a frequency doubled Nd:YAG laser after topical application of an exogenous chromophore. Lasers Surg Med; 25: 43–50 [DOI] [PubMed] [Google Scholar]
- 20.Nanni CA, Alster TS. (1997): Optimizing treatment parameters for hair removal using a topical carbon-based solution and 1064-nm Q-switched neodymium: YAG laser energy. Arch Dermatol; 133: 1546–9 [PubMed] [Google Scholar]