Abstract
Nursing documentation is crucial to high quality, good and safe nursing care. According to earlier studies nursing documentation varies and the nursing classifications used in electronic patient records (EPR) is not yet stable internationally nor nationally. Legislation on patient records varies between countries, but they should contain accurate, high quality information for assessing, planning and delivering care. A unified national model for documenting patient care would improve information flow, management between multidisciplinary care teams and patient safety. Nursing documentation quality, accuracy and development needs can be monitored through an auditing instrument developed for the national documentation model. The results of the auditing process in one university hospital suggest that the national nursing documentation model fulfills nurses’ expectations of electronic tools, facilitating their important documentation duty. This paper discusses the importance of auditing nursing documentation and especially of giving feedback after the implementation of a new means of documentation, to monitor the progress of documentation and further improve nursing documentation.
Introduction
Nursing documentation constitutes an integral part of the nurse’s daily work (1). Meticulous nursing documentation is an important part of multiprofessional patient care. The delivery of good care and the ability to communicate effectively about patient care depends on the quality of information available to all health care professionals. One important part of this information is nursing documentation in nursing care plans (2). The use of EPR and nursing documentation have been more quality, comprehensive and patient-oriented than paper-based nursing documentation (3,4). In standardized electronic nursing documentation, the structure includes the use of nursing process and of standardized terminologies in the various phases of the nursing process (5). The evaluation of the content of standardized electronic nursing documentation is crucial in order to reuse valid data to measure patient outcomes (3).
The purpose of this paper is to discuss the importance of auditing nursing documentation. Crucial aspects include feedback after the implementation of a new means of documentation, monitoring the progress of documentation and improving nursing documentation further.
Background
The nursing process model has been used as a framework for nursing and nursing documentation. The nursing process model involves assessing, planning, implementing and evaluating patient situations, with the ultimate goal of preventing or resolving problematic situations (6). American Nurses Association defines nursing process six steps: assessment, diagnosis, outcomes, identifications, planning, implementation and evaluation (7). In earlier studies, electronic nursing documentation included at least needs assessment, making the nursing diagnoses and determining care aims, planning and delivering nursing interventions, and the evaluation of outcomes (8,9,10–16). Earlier studies have reported that nursing documentation has conformed to the nursing process (15), and the use of the nursing process has been shown to improve legislative compliance and completeness of nursing documentation (8). At the same time, studies have also reported deficiencies in nursing documentation according to the nursing process (9, 14, 16, 17). In addition to the use of nursing process, classifications are needed in order to standardize nursing documentation (18). Standardization of nursing diagnoses and nursing interventions for documentation purposes has been shown to make the contribution of nursing visible and quantifiable (13, 19).
In Finland a national model for documenting nursing care has been developed during the period 2005 – 2009 (20). The model includes the nursing process model by the WHO and nursing classifications developed from the Clinical Care Classification by Dr. Saba (21). The Finnish Care Classification FinCC includes Nursing Diagnoses, Nursing Intervention and Nursing Outcomes Classifications. The national model has been implemented in various EPR in hospitals and health centers. The results of using this model are promising. Nurses have adopted this means of documentation although the interoperability and usability of the systems has not been validated. (20)
The gradual introduction of EPR at Kuopio University Hospital (KUH) took place between 1998 and 2007. KUH was involved in national EPR projects. The model for systematic documentation was introduced in stages 2005–2010 in all treating units of KUH with the exception of emergency and intensive care. Nursing documentation is a written proof of nursing implemented and should show what information nursing decisions are based on and what outcomes were achieved. (5) Evaluating the quality of nursing documentation makes it possible to demonstrate the quality level. Saranto & Kinnunen (2009) concluded that the use of structured nursing terminology promotes the standardization of nursing documentation. This will also pave the way to extend the scope of documentation research from assessing the quality of documentation to measuring patient outcomes. They argued in their review that there was not a single internationally collaborative study assessing nursing documentation using the same audit instrument. Audit instrument were mainly developed for local or regional purposes and used to evaluate retrospectively nursing documentation at organizational level (3). Paans et al (2010) in their study to proved that the D-Catch instrument (Cat-ch-Ing instrument and the Scale for Degrees of Accuracy in Nursing Diagnoses) is a valid and reliable measurement instrument to assess nursing documentation in general hospital settings, using the VIPS (Swedish words for Well-being, Integrity, Prevention and Security) model (16, 22).
Aims of the study
In the national project in Finnish nursing the aim of the audit of the nursing documentation model was set as maintaining documentation according to the model gradually introduced in KUH 2005–2010. The aim of the KUH audits 2010–2011 was:
To test if the nursing documentation audit model was appropriate for evaluating nursing documentation in a university hospital
To ascertain the level of nursing documentation in KUH at unit, service group and organizational level
To identify development points in nursing documentation at unit, service group and organizational level and to prepare detailed development plans.
Materials and methods
An audit instrument was developed in the national development project for electronic nursing documentation. An evaluation form was used in the audit containing entries for 20 different patients of one unit for one day’s treatment/visit. The form includes evaluation according to the stages of the treatment process. Patient documents were evaluated from the nursing perspective, whether the patient’s care needs were documented in the care record, the objective, intended helping methods, implementation of nursing and evaluation. Assessment was made of whether the patient’s need for care and objective were patient centred and whether the need and objective and the objective and nursing implementation were in relation to each other. Whether the nursing implemented was part of the care plan and whether the outcome was evaluated in relation to the patient’s individual objective. Entries on helping methods were also evaluated. The result of the audit is achieved when each aspect to be evaluated is rated on the form (= no entry, 1 = entry made). A value of 1 scores 0.05 points. When entries are to be found for all the 20 patients of the unit, for example, from the point need for nursing, the total for the row is 1.00. The result of the audit of nursing entries yields a numerical result for which a verbal assessment is given - not accepted, weak, satisfactory, good and excellent. When the audit is made according to the audit form the qualitative evaluation of the content of documentation is possible.
Research permission to conduct the audit was obtained in 2009 from the steering group of the systematic nursing documentation project. The audit was conducted in all nursing units which had been using the national nursing documentation model for at least six months. Audit data was gathered through the nurse managers and nursing documentation mentors, who were asked to randomly select for audit the treatment day/visit entries for 20 different patients. Patients’ personal details were removed from the material before it was sent to the auditors. Audit data was gathered for 2010 (67 units) and 2011 (81 units). Data for 2010 amounted to N = 1,274 and in 2011 to N = 1,366 treatment day/visit entries. The result for each separate unit was added to the service units as a whole and these yielded, for example, the result for the Coronary Care Unit. The entire data were combined into one result for the entire KUH. The nursing documentation audit was conducted by two auditors, which was considered to increase its reliability. Further, a systematic survey instrument was developed to gather data on nurses, experiences of the documentation model. This paper describes the results of the auditing process in one university hospital and presents more detailed results of special unit – the Coronary Care Unit (CCU). Thus the outcomes are presented on unit and organization levels.
Results
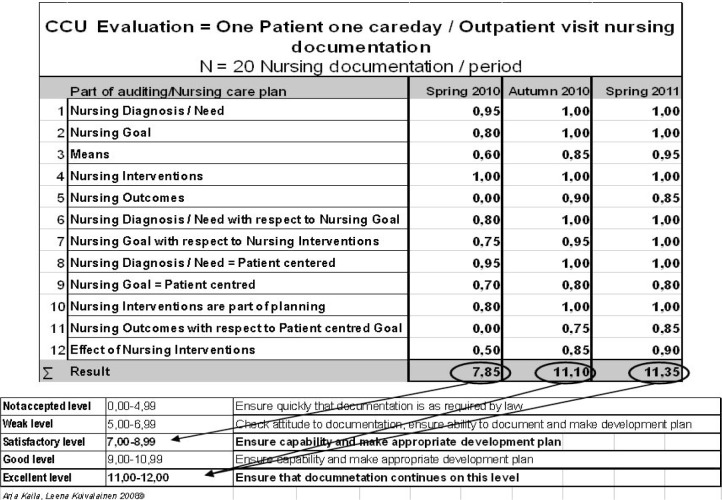
According to an audit (N = 60 records) conducted 2010–2011 in the CCU, the nursing documentation was on a satisfactory level in spring 2010 with a result of 7.85 (Figure 1). The results were processed at the unit’s departmental meeting after which personnel were offered training in documentation according to the nursing process. A development plan was made in the unit on the basis of the audit. The audit was repeated in autumn 2010 with a result for the unit of 11.10 – an improvement from satisfactory to excellent level. The development area in the CCU in spring 2010 was documentation of nursing need, its documentation in relation to goals set and documentation of the effects of helping methods. The audit of autumn 2010 shows that all documentation subareas improved although the development plan only concerned the aforementioned subareas. An audit was conducted in summer 2011 of the CCU nursing documentation and the result for the unit was 11.35; the level excellent had been maintained. Development was discernible in various subareas of documentation, for example, documentation of helping methods further improved. As documentation according to the CCU nursing process improved the content of nursing documentation became qualitatively more patient-centred, meticulous and logical. According to the survey of the CCU personnel (N = 20) they were also satisfied with the qualitative improvement in content documentation.
Figure 1.
Results of the audits of CCU nursing documentation in spring 2010, autumn 2010 and spring 2011.
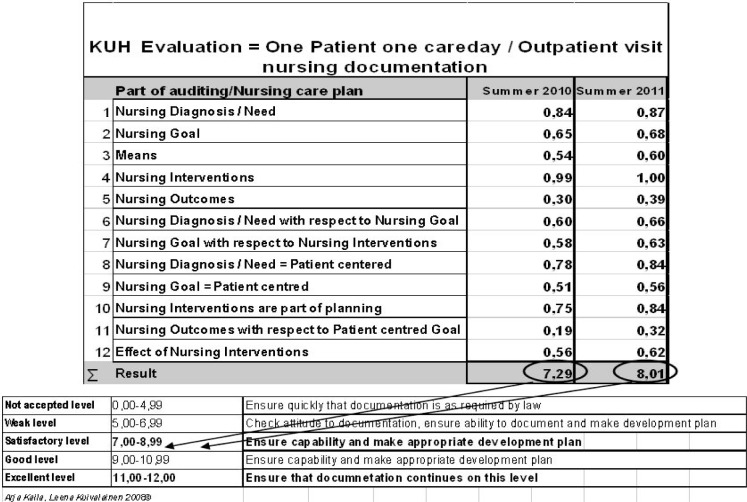
In light of the spring 2011 audit in KUH the level of systematic documentation assessed using this method is satisfactory (N = 81 units) 8.01 (Figure 2) for the organization as a whole. The corresponding result for 2010 (N = 67 units) was 7.29. Compared to the findings of the auditing between 2010 and 2011 the overall level of documentation remained satisfactory. The findings show, however, that there was an improvement in documentation in all subareas, particularly in the documentation of helping methods in 2011 and in documentation of nursing in relation to goals set.
Figure 2.
Results of the audits of KUS nursing documentation audits in 2010 and 2011.
Discussion
The results of this study describe nursing documentation developments in one university hospital. Thus the results should be interpreted with caution. However, the hospital represents the present situation in university hospitals and health centers in Finland which have implemented the Finnish model of standardized nursing documentation. In light of the audit method for nursing documentation it appears that the systematic documentation model is appropriate in various operating environments regardless of the field of specialization. Häyrinen et al 2010 report that the national model for electronic nursing documentation is suitable for the documentation of patient care in nursing care plans (23). In addition to the results of Häyrinen et al 2010 study, the nursing documentation was based on the nursing process model, but not all phases of the nursing process were documented. These findings are consistent with previous studies reporting adherence to the nursing process in nursing documentation (9, 15, 23). Clear and logical overall descriptions of the main information on the patients’ condition, nursing and changes therein are beneficial to all professional groups participating in treatment. The results of this study are consistent with those of Häyrinen et al 2010, in which all phases of the nursing process were used, and in these cases the nursing process was easy to follow (23). If the treatment plan implementation of nursing and evaluation do not match, information on the nursing implemented is illogical and fragmentary. Structured information enables a more precise scrutiny of nursing provided.
Nursing documentation should show what information nursing decisions were based on and what was achieved with nursing measures. By combining helping methods in nursing with the nursing outcome, the effectiveness of practical nursing can be demonstrated in the process of caring for the patient. The results of this study show that nurses rarely documented the patients’ outcomes in patients’ records. This result concurs with those in Törnvall et al. (2004) (16). The classification of nursing outcomes which can be used to determine the changes occurring in the patients’ condition has three levels: improved, stabilized or deteriorated. In future it will be interesting to research whether documentation of care evaluation improves as the classification is adopted. Use, monitoring and evaluation of the documentation model make it possible to develop the process of patient care, the quality of nursing and patient safety. Quality assessment of nursing documentation serves to identify development areas in nursing documentation and so through improved information transfer to improve the information flow between professional groups participating in the care of the patient, in the patient’s best interests.
Conclusion
The national nursing documentation instrument is appropriate for various operating environments regardless of field of specialization. The audit method developed for the nursing documentation instrument describes the level of documentation at the level of unit, service unit and organization. The results of the audit clearly reveal the unit’s development areas in nursing documentation. Utilizing the knowledge generated in the development of evidence-based nursing for improved information flow and knowledge management is possible.
References
- 1.Heartfield M. Nursing documentation and nursing practice: a discourse analysis. J adv nurs. 1996;24:98–103. doi: 10.1046/j.1365-2648.1996.15113.x. [DOI] [PubMed] [Google Scholar]
- 2.Urquhart C, Currell R, Grant MJ, Hardiger NR. Nursing record systems: effects on nursing practise and healthcare outcomes. Cochrane database syat. rev. 2009;(1) doi: 10.1002/14651858. art. no.;cd002099.pub2. [DOI] [PubMed] [Google Scholar]
- 3.Saranto K, Kinnunen U-M. Evaluating nursing documentation – research designs and methods: systematic review. Journal of advanced nursing. 65(3):464–476. doi: 10.1111/j.1365-2648.2008.04914.x. [DOI] [PubMed] [Google Scholar]
- 4.Waneka R, Spetz J. Hospital information technology systems, impact on nurses and nursing care. The journal of nursing administration. 40(12):509–515. doi: 10.1097/NNA.0b013e3181fc1a1c. [DOI] [PubMed] [Google Scholar]
- 5.Häyrinen K, Saranto K, Nykänen P. Definition, structure, content, use and impacts of electronic health records. International journal of medical informatics. 2008;79:291–304. doi: 10.1016/j.ijmedinf.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 6.Yura H, Walsh M. The nursing process: assessing, planning, implementing, evaluating. third ed. appleton-century-crofts; New York: 1978. [Google Scholar]
- 7.Saba VK, McCormick KA. Essentials of Nursing Informatics. Fifth edition. The McGraw-Hill Companies; 2011. [Google Scholar]
- 8.Ammenwerth E, Eichstadter R, Haux R, Pohl U, Rebel S, Ziegler S. A randomized evaluation of a computer-based nursing documentation system. Methods inf. med. 2001;40:61–68. [PubMed] [Google Scholar]
- 9.Mahler C, Ammenwerth E, Wagner A, Tautz A, Happek T, Hoppe B, Eichstadter R. Effects of a computer-based nursing documentation system on the quality of nursing documentation. J. med. syst. 2007;31:274–282. doi: 10.1007/s10916-007-9065-0. [DOI] [PubMed] [Google Scholar]
- 10.Pryor TA. Computerized nurse charting. Int. j. clin. monit. comput. 1989;6:173–179. doi: 10.1007/BF01721030. [DOI] [PubMed] [Google Scholar]
- 11.Holzemer WL, Henry SB. Computer-supported versus manually-generated nursing care plans: a comparison of patient problems, nursing interventions, and AIDS patient outcomes. Comput. nurs. 1992;10:19–24. [PubMed] [Google Scholar]
- 12.Larrabee JH, Boldreghini S, Elder-Sorrells K, Turner ZM, Wender RG, Hart JM, Lenzi PS. Evaluation of documentation before and after implementation of a nursing information system in a acute care hospital. Combut. nurs. 2001;19:56–65. quiz 66–8. [PubMed] [Google Scholar]
- 13.Daly JM, Buckwalter K, Maas M. Written and computerized care plans, organizational process and effect on patient outcomes. J. gerontol. nurs. 2002;28:14–23. doi: 10.3928/0098-9134-20020901-05. [DOI] [PubMed] [Google Scholar]
- 14.Björvell C, Wredling R, Thorell-Ekstrand I. Long-term increase in quality of nursing documentation: effects of a comprehensive intervention. Scan. j. caring sci. 2002;16:34–42. doi: 10.1046/j.1471-6712.2002.00049.x. [DOI] [PubMed] [Google Scholar]
- 15.Ehrenberg A, Birgersson C. Nursing documentation of leg ulcers: Adherence to clinical guidelines in a Swedish primary health care district. Scand. j. caring sci. 2003;17:278–284. doi: 10.1046/j.1471-6712.2003.00231.x. [DOI] [PubMed] [Google Scholar]
- 16.Törnvall E, Wilhelmsson S, Wahren LK. Electronic nursing documentation in primary health care. Scan. j. caring sci. 2004;18:310–317. doi: 10.1111/j.1471-6712.2004.00282.x. [DOI] [PubMed] [Google Scholar]
- 17.Törnvall E, Wahren LK, Wilhelmsson S. Impact of primary care management on nursing documentation. J. nurs. manag. 2007;15:634–642. doi: 10.1111/j.1365-2834.2007.00729.x. [DOI] [PubMed] [Google Scholar]
- 18.Averill CB, Marek KD, Zielstorff R, Kneeddler J, Delaney C, Milholland DK. ANA standards for nursing data sets in information systems. Comput. nurs. 1998;16:157–161. [PubMed] [Google Scholar]
- 19.Park M, Delaney C, Maas M, Reed D. Using a nursing minimum data set with older patients with dementia in an acute care setting. J. adv. nurs. 2004;47:329–339. doi: 10.1111/j.1365-2648.2004.03097.x. [DOI] [PubMed] [Google Scholar]
- 20.Tanttu K, Ikonen H. Nationally standardized electronic nursing documentation in Finland by the year 2007. Stud health technol inform. 2006;122:501–1. [PubMed] [Google Scholar]
- 21.McCormick KA, Lang N, Zielstorff R, Milholland K, Saba V, Jacox A. Toward standard classification schemes for nursing language: recommendations of the American Nurses Association Steering Committee on Databases to support clinical nursing practice. Journal of the american medical informatics association. 1994;1(6):421–7. doi: 10.1136/jamia.1994.95153431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Paans W, Sermeus W, Nieweg Roos MB, van der Schans Cees P. D-Catch instrument: development and psychometric testing of a measurement instrument for nursing documentation in hospitals. J. adv. nurs. 2010:1388–1400. doi: 10.1111/j.1365-2648.2010.05302.x. [DOI] [PubMed] [Google Scholar]
- 23.Häyrinen K, Lammintakanen J, Saranto K. Evaluation of electronic nursing documentation – Nursing process model and standardized terminologies as key to visible and transparent nursing. International journal of medical informatics. 2010;79:554–564. doi: 10.1016/j.ijmedinf.2010.05.002. [DOI] [PubMed] [Google Scholar]