Abstract
The growth of Internet applications has substantially broadened the potential for its use in global telehealth. This pilot project used the virtual reality world of Second Life for diabetic patients to meet with their nurse practitioners for their maintenance visits. Using avatars and the online patient portal, these scheduled visits were designed to meet the needs of the patients as determined by the results from a questionnaire completed by patients prior to the visit. The virtual visits took place in the replicated building where patients typically receive their care, the Eskind Diabetes Clinic. Orientation sessions to Second Life were made available prior to the actual visit, and additional online resources were made available after the visit was over. Although only seven pilot patients have currently completed visits, data illustrate the positive potential use of this treatment modality for future study.
Introduction
Intensive management and support of individuals with diabetes is required to maintain the glycemic control that is needed to avert complications, however, access to care is a major barrier to maintaining good glycemic control. In just the first quarter of 2009, our no show rate at the Vanderbilt Eskind Diabetes Clinic increased by nearly 40% for those patients who had recently achieved good glycemic control. Clearly alternate strategies that complement the face-to-face interaction are needed during these difficult economic times when often the cost of transportation is alone an impediment to an individual seeking out clinical care. Little is known about the maintenance “dose” of diabetes care needed to prevent relapse. Assessing the type, duration and frequency of such efforts is needed to sustain an important attribute of successful longitudinal diabetes care.
The primary purpose of this project was to educate and support both healthcare providers and participants with diabetes about how to interact within the virtual reality world of Second Life (SL) in order to participate in maintenance healthcare activities. Three phases were required: 1) construction and programming for the SL facility in which the diabetes clinical care was provided; 2) training and orientation activities for both healthcare providers and patients; and 3) ongoing technical support for both healthcare providers and patients.
Background
There currently exist a number of virtual reality environments, but Second Life (SL) is by far the most widely used and affordable solution. Second Life (SL) is a 3D virtual world, created by its residents. The world is driven by the interactions of real-world individuals and their “inworld” residents or “avatars”. Thus, every avatar has a live person behind it manipulating the movements, words, actions, etc. in SL. Using SL requires only an Internet connection and working computer with headset. User accounts are free, but developers lease islands on which to build their graphical depictions of reality. These islands are then registered with names, and become either private or public.
“Real” world follow-up or maintenance appointments for healthcare require leaving school or work in order to allow for the time for the face-to face appointment. In addition, there is time spent in travel to the appointment site as well as the parking and other travel expenses. For those in the outskirts of the regional area, this travel might even require overnight accommodations. Particularly after an episode of acute hospitalization, it is not surprising that patients choose to forgo the maintenance visits with their healthcare providers even though they understand the risks of having the disease of diabetes. Today’s economy faces patients with the additional challenge of making choices that were never before thought to be in the realm of possibility. Healthcare needs frequently are not first priority. As a result, it is time for healthcare providers to think “outside the box” (by using the “box” – computer) in order to provide alternative treatment modalities for their patients with chronic disease.
Much has been written about education within the virtual reality environment of Second Life (SL) but few attempts have been made to deliver actual patient care in SL.1 Probable reasons for this are concerns related to privacy as well as practical issues of orientation, documentation, liability, and billing. Watson et. al. present a framework that demonstrates how applications within SL can be constructed to meet the needs of patients with diabetes, allowing them to attend group visits, learn more about lifestyle changes, and foster a sense of support and emotional well-being. They note that addressing concerns relating to privacy and liability is a necessary first step to engage providers in this new approach to patient care and acknowledge that very little literature exists regarding the impact of virtual worlds on the care of people with diabetes. Linton et al. described a project to determine if methods known to elicit the Relaxation Response can be successfully taught to subjects in group sessions in SL.2 They concluded that it is feasible to translate a real life clinical practice into a virtual world, although close collaboration between the technical and clinical teams help to identify aspects of the real practice that had a higher propensity for virtual adaptation. With over 15 million current users in SL, the potential impact for the provision of healthcare to its residents is yet untapped.
Project Phases
Phase 1: Customization of the outpatient care facility to meet the needs of the diabetic patients and healthcare providers was the first step in the process. The Eskind Diabetes Clinic had been replicated in the SL environment as part of grant activities by Dr. Weiner’s team on a $1.6 million HRSA Innovative Nurse Education Technology grant. The intent of that grant was to teach nursing faculty how to manage clinical simulations for nursing students, with no live clinical care provided in that environment. However, an acute care facility, a nursing home facility, a clinic facility, and several private homes were constructed as varied sites in which faculty can deliver geriatric simulations. The designed clinic facility was re-located to a leased SL island space for this pilot project with some following revisions made to the facility in order to accommodate the delivery of live patient care under the Vanderbilt brand.
New users to SL typically start their experience on Orientation Island, but there have been many reports of sexual predators harassing new avatars with inappropriate offensive behaviors. This is in spite of community standards and a well-designed infrastructure to report abuse within SL. In order to shield patients from this experience, an elevated orientation course was developed on our private island, therefore allowing participants to skip the Orientation Island experience.
Another concern was the issue of privacy. In the SL environment, private audio conversations between two residents are not encrypted. However, the call does not pass through any Linden Lab (makers of SL) or Vivox (partner specializing in an integrated voice platform for the web) servers; they are conducted on a peer-to-peer basis between the two computers involved. On the other hand, public voice chat with people who are near other avatars inworld, is processed and mixed on servers maintained by Vivox. Linden Labs reports that they are currently working toward introducing an encryption option for all voice channels in order to ensure the privacy of all voice communication. Until this encryption option is available, there were some approaches that could be implemented that made it far more difficult to breech. Since the audio range limitation is 60 meters, identical patient care rooms were created that could be accessed by the patient and clinician transporting to the replicated room using a privacy button. These replicated rooms were suspended between 100 and 300 meters above the ground, well out of audio eavesdropping range from the ground. To prevent someone from flying up to just outside the room, flight was disabled on this island once it is committed to the research study. Furthermore, the clinician was advised to launch the minimap which gave a two dimensional view of anyone within 65 meters of their x, y coordinates. Patients were advised to select relatively obtuse avatar names that cannot be reverse engineered to determine who the person actually was in real life to anyone except the clinician and the clinician's immediate staff. Once the visit was completed, the privacy “off” button teleported the patient and clinician back down to the original building in order to complete any post visit activities and exit the facility. Admittance to the island was restricted by accounts to care givers, identified patients, and technical support personnel. The general public was not able to access the island.
Text communication was privatized by the participants using the SL chat feature that recorded what each person typed. Once the session was completed, this text was cut and pasted into the notes section of the Vanderbilt electronic health record. Should audio only be preferred by the healthcare provider, then a summary of the outcomes of the visit was recorded in a separate login to the Vanderbilt electronic health record. This was the same documentation process used for face-to-face clinical visits at the Eskind Diabetes Center.
Additional features added to the virtual clinic facility tracked movement of the avatars. An object can be specified (such as the front door of the clinic) that tracks who enters the facility. A patient registration process was replicated so that an additional record is kept of participation by patients. This registration process included verification of avatar names against actual patient data. Avatar movements of healthcare providers were also logged in order to determine their activity as an outcome. Logs were maintained as to what diabetes educational resources are accessed from the Electronic Resource Room and by whom.
Once entering the SL environment, participants were able to go to any area of the SL “Eskind Diabetes Care” island. If it was a designated appointment, then the patient checked into the system using a virtual screen that ran parallel to the kiosk check-in systems in use in multiple Vanderbilt University Medicine Center clinics. The patient then met his/her healthcare provider next to the registration kiosk and was accompanied back to his/her office. The SL Electronic Resource Room remained open 24 hours. Patient support groups could use SL meeting space and support staff during pre-set hours.
Phase 2: Both patients and providers required orientation activities to the SL platform. Video sessions and one-on-one orientation sessions ensured that all participants reached pre-determined competency levels in this environment. Competencies included the following: 1. Getting Started Tasks (setting up an account in SL, selecting a name and password; installing the SL client; creating an avatar, altering appearance, altering clothing; going to a SL URL; learning how to walk, run, fly, land, sit, turn around, teleport, altering your viewpoint, using gestures; selecting and configuring of headset; bringing up and using audio chat); 2. Intermediate Tasks (using search tool; adding a “friend”; instant messaging a friend); 3. Social Tasks (awareness of how to teach and learn within this environment; how to identify and report abuse; how to document care in this environment; how to get technical help).
Web pages describing the project were developed and included an introduction to the project team, an overview of Second Life with pre-recorded videos illustrating the SL environment, and an online test to check for adequacy of both hardware and network resources for the use of SL. Users could either design their own avatars or be assigned one with a username and password to use in Second Life. After practicing with their avatars on the private island, users were then met with one of the project coordinators who watched them navigate the orientation course and evaluated their competencies prior to allowing them to participate in their scheduled appointments.
Phase 2 activities also included the development of digital resources to be placed in the Electronic Resource Room. Dr. Weiner and her team worked with the healthcare providers to digitally replicate current diabetes learning resources. Additional web sites were also designated by the healthcare team to be included, including any SL addresses that could also be used for learning resources. Furthermore, development of these digital resources has been ongoing since they can also be used by the clinic patients and staff outside the SL environment by accessing the resources via web pages.
Once SL competencies were met, users then completed a self-assessment questionnaire designed to collect data regarding their healthcare activities. This was submitted electronically to the healthcare providers who then focused on specific areas of need during the visit in SL. Visit details were recorded in the same electronic health record system used for face-to-face visits. Patients could view these records through the patient portal called “My Health at Vanderbilt.” Completing the visit was an evaluation form that was answered by the patient in the virtual lobby kiosk upon exiting the island.
Phase 3: Technical support was ongoing throughout the project through phone, e-mail, instant messaging, and designated office hours in SL. Revisions were made as deemed necessary.
Key Lessons
Early in the pilot, the team noted that the participants were having difficulty with many of the SL competencies. The most difficult skill was learning how to manage the camera in order to alter the avatar’s viewpoint. Many had difficulty flying. As a result, the competencies were modified to reflect the most basic of avatar skills deemed necessary to complete a healthcare visit.
Orientation times to master SL competencies varied. A few of the patients were very practiced in virtual reality use, and already had avatars. They required little to no orientation. Others struggled and took as much as 90 minutes to become oriented. Scaling back the SL competencies and providing users with already made avatars decreased this time to a more practical 30 minutes.
Using the self-assessment questionnaire provided structure to the visit in such a way that the nurse practitioners were able to capitalize on that time to really meet the needs of the patient. They immediately wanted to include the same questionnaire with their face-to-face patients, but since comparative studies have not yet taken place (virtual versus face-to-face visits) the team did not want to contaminate the treatments.
Many other resources could have been added to this virtual care environment (such as a nutrition center, an exercise center, etc.) that could have been used to enhance patient care outside of the appointment times. These suggestions have been added to current grant requests seeking further funding to more fully evaluate the impact of the virtual visits.
Discussion
Seven patients have completed initial visits with healthcare providers in the designated SL environment. The majority of the responders described the overall visit as excellent, and somewhat more effective than face-to-face. In addition, they were able to navigate and receive answers to their questions, and had no difficulty navigating in this environment. They reported that they would use SL again to seek nutrition counseling, access electronic resources about diabetes, participate in group sessions, and access exercise resources. The majority of respondents also noted that they would recommend this type of visit to others. One patient outlier found the experience to be fair and somewhat less effective than face to face. Although the patient was able to receive answers to any questions, the respondent did not want to access SL for any other resources nor would the person recommend this type of visit to others.
This paper describes only one aspect of the evaluation of providing maintenance care to diabetic patients as it relates to the development and use of the virtual environment. Further grant requests have also included aims to assess the relative effectiveness of this diabetes maintenance care strategy against those delivered in traditional face-to-face visits and to examine the differences in interactions between providers and patients in face-to-face encounters and SL encounters, including the identification of factors related to SL interactions that produce meaningful clinical encounters.
Conclusion
Initial data with these pilot patients illustrate that this virtual reality approach will not be a solution for all patients. However, a virtual visit may just be the solution for those that are disabled or have difficulty in finding transportation to the actual clinic environment. Additional feedback from the pilot patients resulted in streamlining the orientation process, clarifying directions, and refining the data collection tools proposed for the SL visit so that the treatment can be expanded for future funding with other global participants. Questions still remain concerning the ethical and legal implications of providing treatment outside the original region of the local healthcare providers.
Figure 1.
Entrance and Hallways of Eskind Diabetes Clinic in SL
Figure 2.
Office Environment for Clinical Visit
Figure 3.
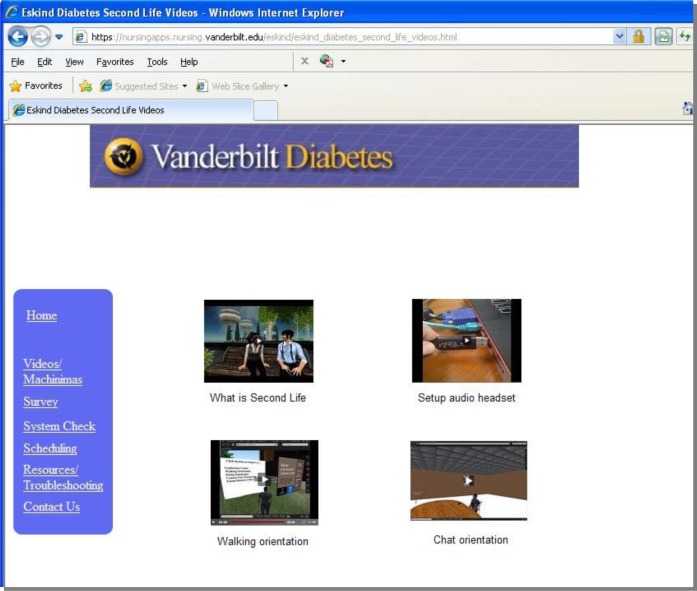
Orientation Machinimas for Pilot Project
References
- 1.Watson AJ, Grant RW, Bellow H, Hoch DB. Brave new worlds: How virtual environments can augment traditional care in the management of diabetes. J Diabetes Sci Technol. 2008;2(4):697–702. doi: 10.1177/193229680800200422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Linton D, Senelly M, Baim M, Bello H, Millik MT, Watson A, Hoch DB. Translating medical practice from the real to the virtual: Adapting an existing clinical program to a virtual world. AMIA Symposium Proceedings. 2008:1026. [PubMed] [Google Scholar]