Abstract
The Swedish health care system stands before an implementation of standardized language. The first classification of nursing diagnoses translated into Swedish, The NANDA, was released in January 2011. The aim of the present study was to examine whether the usage of the NANDA classification affected nursing students’ choice of nursing interventions. Thirty-three nursing students in a clinical setting were divided into two groups. The intervention group had access to the NANDA classification text book, while the comparison group did not. In total 78 nursing assessments were performed and 218 nursing interventions initiated. The principle findings show that there were no statistical significant differences between the groups regarding the amount, quality or category of nursing interventions when using the NANDA classification compared to free text format nursing diagnoses.
Introduction
Standardized nursing diagnoses, when integrated in the electronic health record, have been stated to play an important role in obtaining nursing data, facilitating systematic analysis for measures and comparison within and between healthcare organizations1,2. The Swedish National Board of Health and Welfare3 states that nurses shall independently apply the nursing process by observing, assessing, identifying nursing diagnosis, planning nursing interventions and evaluating the outcome and patient response to nursing care. Furthermore, all health professionals shall, as far as possible, document patient data using standardized terminology, statistical classifications and coding systems agreed upon on a national and international level4,5.
The NANDA-International classification
The classification developed by North American Nursing Diagnoses Association – International (NANDA) is internationally the most widely implemented classification of nursing diagnoses6 and since January 2011 the first classification of nursing diagnoses available in Swedish. The translation is also mapped to the Swedish version of SNOMED-CT5. The NANDA Taxonomy II consists of 212 approved nursing diagnoses divided in 47 classes sorted in 13 domains. The NANDA domains are: 1. Health Promotion, 2. Nutrition, 3. Elimination and Exchange, 4. Activity/Rest, 5. Perception/Cognition, 6. Self-Perception, 7. Role Relationships, 8. Sexuality, 9. Coping/Stress Tolerance, 10. Life Principles, 11. Safety/Protection, 12. Comfort, 13. Growth/Development7.
The VIPS-model
Since the mid 1990’s nursing documentation in Sweden has been structured according to the VIPS model8. VIPS, an acronym for the Swedish terms for Well-being, Integrity, Prevention and Safety, is a model for documentation of the nursing process using keywords (categories). The model consists of categories at two levels, the first level follows the nursing process; nursing history, patient status, nursing diagnoses, expected outcome, nursing interventions and nursing outcome. The nursing history, nursing status and nursing interventions have a second level of categories. The categories for nursing interventions are; Participation, Information/Education, Support, Environment, General Care, Training, Observation/Surveillance, Special Care, Drug Administration and Coordination. While the choice of nursing intervention is guided by the nursing diagnosis and expected outcome, the choice of category for a nursing intervention is determined by the purpose of the intervention9.
The assessment part of the nursing process is relatively well documented in the patient record, although the analysis resulting in a nursing diagnosis, in Sweden written in free text format, generating a useful care plan is virtually non-existent8. Although the nursing process and nursing diagnosis have a prominent position in the curricula of most institutions of higher education for nursing, it appears difficult to apply in clinical practice10. Nursing interventions have been shown often to be performed based on reasons other than individually identified patient needs, for example ward routine procedures or non-reflective experience-based knowledge of the individual care giver or in a workgroup11. Lunney12 argue that nurses who use critical thinking and analyze nursing data can offer more individualized care than those only carrying out interventions based on routine.
Several studies13,14 indicate that introducing standardized nursing language such as NANDA, have improved the quality of nursing documentation in the patient record. However, since these interventions often have included educational strategies for strengthening the nurse as diagnostician, it is unclear whether the results are actually derived from the use of standardized nursing language, or just the fact that participating nurses are encouraged to use analytic thinking. Since the Swedish health care system is about to implement standardized language, it is important to study the effects of such a use in clinical practice. The aim of this study was to examine whether the use of a classification for nursing diagnoses affects nursing students’ choice of nursing interventions.
Materials and Methods
Participants and setting
The study took place at a Clinical Education Ward in a university hospital in Stockholm, Sweden during ten weeks in the spring 2011. The ward had eight beds and treated orthopedic patients with elective surgery of mainly hip and knee replacements. Nursing students in the last semester of their education were responsible for planning and delivering nursing care, supervised by Registered Nurses. All nursing students (n=42) who during the time of the study were appointed a one to two weeks clinical practice at the ward, were asked to participate. Five students declined, leaving 37 participants. The study started with the comparison group for five weeks, followed by the intervention group for five weeks. The participants answered a questionnaire on background data; educational level, previous experience of nursing diagnostics and previous knowledge of the NANDA classification. All stated that they had had some education in nursing diagnostics (free text format) and practiced the use of free text format nursing diagnoses in at least one previous clinical setting. Most of them had heard of the NANDA classification but no one had read the NANDA text book. With reference to the collected background data four students were excluded: one foreign exchange program student with a different education level and three students because they had worked with NANDA in previous clinical setting. After exclusion the intervention group consisted of 19 students and the comparison group of 14 students.
Procedure
A pre-written paper form designed for this study was used, consisting of the headings; Nursing diagnoses, Defining characteristics, Related factors (etiology), Nursing interventions (listed by the VIPS categories for interventions), patient’s age, gender and reason for admission. The participants of both groups received the same 30 minutes introduction to nursing diagnostics and interventions on their first day at the ward. The intervention group also received a presentation of the NANDA classification and how to use the NANDA text book. At the end of each day shift, all participants were assigned 30 minutes in a room separated from the ward with instructions to identify and document nursing diagnoses and nursing interventions of the patients they had been responsible for during the shift. The intervention group had access to the NANDA classification text book. Both groups used the same paper form.
Data analysis
The nursing interventions, described in free text format by the participants, were categorized using VIPS categories for nursing interventions. The quality of the interventions was analyzed using a four point scale developed for this study by the authors. The maximum of 4 points were given to an intervention described in such a way, that it was clear; What to do, How to do it, When to do it and by Whom. One point was subtracted from the maximum of 4 points for each of the above mentioned questions that were not clearly stated in the nursing intervention. The written interventions were analyzed separately by the two authors and then compared and discussed until consensus was reached regarding quality score and sorting in VIPS categories. Only the nurse-initiated interventions were analyzed. All other interventions were considered non-valid, e.g. physician-initiated interventions performed by nurses. Descriptive statistics were used to show the amount of diagnoses per NANDA domain, amount of nursing interventions and their quality score and the amount of interventions per VIPS category. With regards to the sample size and the ordinal data in this study Mann-Whitney U test was used to test for differences between the groups regarding frequencies and quality score. The computer software SPSS was used for these calculations.
Results
In total 78 patient assessments were performed by the participants, 36 by the intervention group and 42 by the comparison group. Of the 36 nursing diagnoses in the intervention group 27 were literally formulated as NANDA diagnoses, eight were very similar to NANDA diagnosis and one expressed more like a symptom. Of the 42 nursing diagnoses identified by the comparison group, 18 were literally formulated as NANDA diagnoses and 18 had structure and content close to NANDA diagnosis, leaving six which were formulated more like signs or symptoms than actual nursing diagnosis (Table 1).
Table 1.
Frequencies of nursing diagnoses (ND) and nursing interventions (NI) and the median quality score of the nursing interventions (NIQ) per ND sorted by NANDA domains 1–12 (D).
| Intervention Group | Comparison Group | |||||||
|---|---|---|---|---|---|---|---|---|
| D | Nursing Diagnoses |
ND (n=36) n |
NI (n=97) n |
NIQ md |
Nursing Diagnoses |
ND (n=42) n |
NI (n=121) n |
NIQ md |
| 1 | Ineffective self health care management* | 1 | 2 | 1,5 | Patient wants to give up smoking | 1 | 1 | 2 |
| 2 | Imbalanced nutrition: less than body requirements* | 3 | 10 | 2 | Risk for malnutrition | 3 | 9 | 2 |
| Risk for dehydration* | 1 | 2 | 1,5 | Risk for dehydration* | 1 | 3 | 2 | |
| Risk for unstable blood glucose level* | 1 | 3 | 3 | Risk for weight loss | 1 | 3 | 2 | |
| 3 | Constipation* | 3 | 7 | 2 | Constipation* | 3 | 7 | 2 |
| Risk for constipation* | 1 | 5 | 1 | Risk for constipation* | 8 | 29 | 3 | |
| 4 | Delayed surgical recovery* | 3 | 10 | 2 | Motivated to postoperative mobilization | 2 | 4 | 1 |
| Risk for delayed surgical recovery | 1 | 3 | 2 | Risk for delayed surgical recovery | 1 | 3 | 3 | |
| Disuse syndrome | 1 | 2 | 3 | Motivated to self-care | 1 | 4 | 2,5 | |
| Impaired bed motility* | 1 | 2 | 2 | Needs assistance to toilet | 1 | 1 | 1 | |
| Sleeping problem | 1 | 0 | ||||||
| 5 | Readiness for enhanced knowledge* | 1 | 3 | 3 | ||||
| 6 | Strong integrity | 1 | 1 | 3 | ||||
| 9 | Anxiety* | 2 | 5 | 2 | ||||
| 11 | Risk for falls* | 5 | 16 | 3 | Risk for decubitus | 6 | 24 | 2 |
| Risk for decubitus | 4 | 13 | 3 | Risk for falls* | 3 | 9 | 2,5 | |
| Risk for impaired skin integrity* | 3 | 6 | 3 | Impaired skin integrity* | 1 | 3 | 2 | |
| Impaired skin integrity* | 1 | 3 | 1 | Redness in sacrum | 1 | 4 | 2,5 | |
| Risk for infection* | 1 | 0 | Dry and sore skin in sacrum | 1 | 2 | 2,5 | ||
| Dry mouth | 1 | 4 | 3,5 | Risk for urinary infection | 1 | 2 | 2,5 | |
| 12 | Nausea* | 2 | 5 | 2 | Problem swallowing tablets | 1 | 0 | |
| Acute pain* | 1 | 1 | 3 | Risk for pain | 1 | 3 | 3 | |
| Pain problem | 1 | 2 | 3 | |||||
| Pain in movement | 1 | 2 | 2 | |||||
Diagnoses literally formulated as NANDA diagnoses.
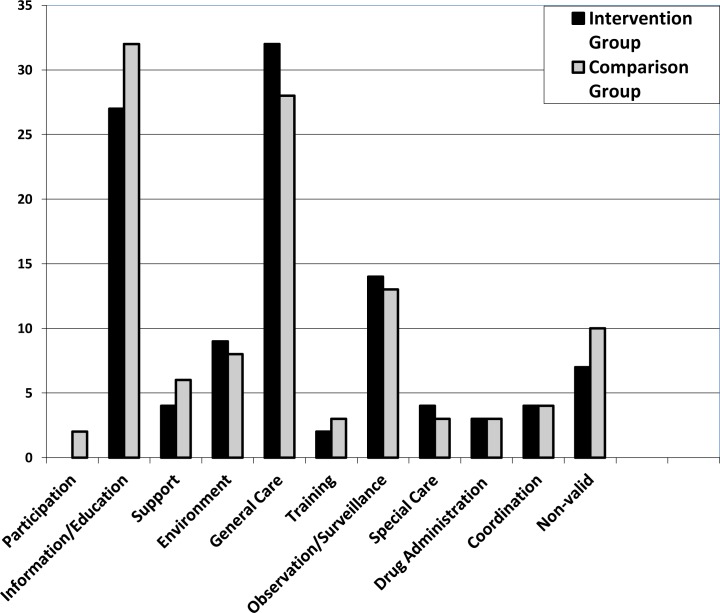
In the intervention group 97 nursing interventions were formulated, with a median of 3 nursing interventions per nursing diagnoses and with a median intervention quality score of 2 points. In the comparison group 121 nursing interventions were formulated, with a median of 2 nursing interventions per nursing diagnoses and with a median intervention quality score of 2 points. Seven non-valid nursing interventions were found in the intervention group while the corresponding value in the comparison group was 12 (Figure 1). There was no statistically significant difference between the two groups regarding frequencies of diagnoses or interventions in total or per NANDA and VIPS category respectively, nor regarding intervention quality score or the amount of non-valid nursing interventions (p=0,05).
Figure 1.
Percentage of the total amount of nursing interventions per group, as distributed according to the VIPS categories, together with non-valid interventions.
Discussion
The principle findings of this study are that there were no statistical significant differences in the amount of nurse initiated interventions, the amount of nursing interventions per VIPS category, the intervention quality score or the amount of non-valid nursing interventions when using the NANDA classification compared to free text format diagnoses. The focus of the detected patient problems formulated as nursing diagnoses did not differ between the groups, indicating that the nursing students were able to analyze patient data and formulate nursing care plans with, as well as without the help of the NANDA classification.
A strength of the study is that the participants of the groups were equal in experience and educational level, and that they were responsible for real patients in a clinical setting. Many studies addressing nurses’ and nursing student’s ability to analyze nursing data are performed with case studies, such as Paans et al.15 studying factors influencing nursing diagnoses accuracy with 96 nursing students in the Netherlands. Their study showed that access to knowledge sources, similar to those in our study, did not improve the accuracy of diagnoses while the factor that stood out significantly was the influence of reasoning skills.
There are some weaknesses in this study that should be pointed out. The sample size is small. For that reason we may not draw conclusions from our material and this study could be viewed upon as a pilot study, identifying topics for future research. For instance whether using a nursing classification or any nursing literature when producing a nursing care plan, will help directing the nurse towards nurse initiated interventions and distinguish nursing from other activities nurses do in their daily work. Research by Lunney16 and Farren17 indicates that NANDA could be of help for nursing students in identifying nursing concepts.
Since working conditions for nurses and incentives to use diagnostic reasoning in the planning of patient care vary between settings8,18 ,19 ,it was important that the students in our study had a scheduled time in a room separated from the ward. Different environmental and individual factors contributing to the prevalence and accuracy of nursing diagnoses documentation in clinical practice have been hypothesized to be inter-related, assuming that a single innovation such as an education program in diagnostics or implementation of standardized nursing language have limited effect without taking into account other factors that influence diagnosis documentation20. This is in coherence with our study indicating that access to the NANDA classification alone does not change the focus of nursing diagnoses and nursing interventions. Educational programs in diagnostic reasoning for nurses in clinical practice have improved the nursing documentation in the patient record with13,14 or without11,19,21 using standardized nursing language. To improving nursing documentation, the most important factor seems to be that nurses must have a clear understanding of the meaning of nursing concepts11,22,23.
A complementary finding in the study is the congruence in diagnostic statements between the groups, which would be valuable to further explore. Thoroddsen and Thorsteinsson24 analyzed 1217 patient records in an Icelandic hospital and found that 88% of the patient problems documented in free text by the Icelandic nurses concurred with the NANDA taxonomy. Our study indicates that the language in the NANDA taxonomy do represent how Swedish nursing students express nursing.
References
- 1.Welton JM, Halloran EJ. Nursing diagnoses, diagnosis-related group, and hospital outcomes. Journal of Nursing Administration. 2005;35(12):541–549. doi: 10.1097/00005110-200512000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Weir-Hughes D. Reviewing nursing diagnoses. Nursing Management. 2007;14(5):32–35. doi: 10.7748/nm2007.09.14.5.32.c4354. [DOI] [PubMed] [Google Scholar]
- 3. Socialstyrelsen. Kompetensbeskrivning för legitimerad sjuksköterska. Article number 2005-105-1. (Swedish National Board of Health and Welfare – in Swedish). 2005.
- 4. Socialstyrelsen. Socialstyrelsens föreskrifter om informationshantering och journalföring i hälso- och sjukvården. SOSFS 2008:14. Stockholm (Swedish National Board of Health and Welfare – in Swedish). 2008.
- 5.Swedish National Board of Health and Welfare An Interdisciplinary Terminology for Health and Social Care - Final Report. 2011. Article number 2011-8-17.
- 6.Muller-Staub M, Lavin MA, Needham I, Van Achterberg T. Meeting the criteria of a nursing diagnosis classification: Evaluation of ICNPs, ICF, NANDA and ZEFP. International Journal of Nursing Studies. 2007;44:702–713. doi: 10.1016/j.ijnurstu.2006.02.001. [DOI] [PubMed] [Google Scholar]
- 7.Herdman H, editor. NANDA International Nursing diagnoses: definitions and classification 2009–2011. Chichester: Wiley-Blackwell; 2009. [Google Scholar]
- 8.Florin J, Ehrenberg A, Ehnfors M. Quality of nursing diagnoses: Evaluation of an educational intervention. International Journal of Nursing Terminologies and Classifications. 2005;16(2):33–43. doi: 10.1111/j.1744-618X.2005.00008.x. [DOI] [PubMed] [Google Scholar]
- 9.Ehrenberg A, Ehnfors M, Thorell-Ekstrand I. Nursing documentation in patient records: Experience of the use of the VIPS-model. Journal of Advanced Nursing. 1996;24:853–867. doi: 10.1046/j.1365-2648.1996.26325.x. [DOI] [PubMed] [Google Scholar]
- 10.Carpenito-Moyet LJ. Teaching nursing diagnosis to increase utilization after graduation. International journal of nursing terminologies and classifications. 2010;21(3):124–33. doi: 10.1111/j.1744-618X.2010.01158.x. [DOI] [PubMed] [Google Scholar]
- 11.Darmer MR, Ankersen L, Nielsen BG, Landberger G, Lippert E, Egerod I. Nursing documentation audit--the effect of a VIPS implementation programme in Denmark. Journal of Clinical Nursing. 2006;15(5):525–34. doi: 10.1111/j.1365-2702.2006.01475.x. [DOI] [PubMed] [Google Scholar]
- 12.Lunney M. Use of critical thinking in the diagnostic process. International journal of nursing terminologies and classifications. 2010;21(2):82–8. doi: 10.1111/j.1744-618X.2010.01150.x. [DOI] [PubMed] [Google Scholar]
- 13.Müller-Staub M, Needham I, Odenbreit M, Lavin A, Van Achterberg T. Improved quality of nursing documentation: Results of a nursing diagnoses, interventions and outcomes implementation study. International Journal of Nursing Terminologies and Classifications. 2007;18(1):5–17. doi: 10.1111/j.1744-618X.2007.00043.x. [DOI] [PubMed] [Google Scholar]
- 14.Thorodssen A, Ehnfors M. Putting policy into practice: Pre- and posttests of implementing standardized languages for nursing documentation. Journal of Clinical Nursing. 2007;16(10):1820–1836. doi: 10.1111/j.1365-2702.2007.01836.x. [DOI] [PubMed] [Google Scholar]
- 15.Paans W, Sermes W, Nieweg R, Schans C. Determinants of the accuracy of nursing diagnoses: Influence of ready knowledge, knowledge sources, disposition toward critical thinking, and reasoning skills. Journal of Professional Nursing. 2010;26(4):232–241. doi: 10.1016/j.profnurs.2009.12.006. [DOI] [PubMed] [Google Scholar]
- 16.Lunney M. Helping nurses use NANDA, NOC, and NIC - novice to expert. Nurse Educator. 2006;31(1):40–46. doi: 10.1097/00006223-200601000-00011. [DOI] [PubMed] [Google Scholar]
- 17.Farren AT. An educational strategy for teaching standardized nursing languages. International Journal of Nursing Terminologies and Classifications. 2010;21(1):3–13. doi: 10.1111/j.1744-618X.2009.01139.x. [DOI] [PubMed] [Google Scholar]
- 18.Axelsson L, Björvell C, Mattiasson AC, Randers I. Swedish registered nurses’ incentives to use nursing diagnoses in clinical practice. Journal of Clinical Nursing. 2006;15:936–945. doi: 10.1111/j.1365-2702.2006.01459.x. [DOI] [PubMed] [Google Scholar]
- 19.Müller-Staub M, Needham I, Odenbreit M, Lavin A, van Achterberg T. Nursing diagnoses, interventions and outcomes – application and impact on nursing practice: a systematic literature review. Journal of Advanced Nursing. 2006;56(5):514–531. doi: 10.1111/j.1365-2648.2006.04012.x. [DOI] [PubMed] [Google Scholar]
- 20.Paans W, Sermes W, Nieweg R, Schans C. What factors influence the prevalence and accuracy of nursing diagnoses documentation in clinical practice? A systematic literature review. Journal of Clinical Nursing. 2011;20(17–18):2386–2403. doi: 10.1111/j.1365-2702.2010.03573.x. [DOI] [PubMed] [Google Scholar]
- 21.Björvell C, Wredling R, Thorell-Ekstrand I. Long-term increase in quality of nursing documentation: effects of a comprehensive intervention. Scandinavian Journal of Nursing Science. 2002;16:34–42. doi: 10.1046/j.1471-6712.2002.00049.x. [DOI] [PubMed] [Google Scholar]
- 22.Keenan G, Falan S, Heath C, Treder M. Establishing competency in the use of North American Nursing Diagnosis Association, Nursing Outcomes Classification, and Nursing Interventions Classification terminology. Journal of Nursing Measurement. 2003;11(2):183–98. doi: 10.1891/jnum.11.2.183.57286. [DOI] [PubMed] [Google Scholar]
- 23.Thoroddsen A, Ehnfors M, Ehrenberg A. Nursing specialty knowledge as expressed by standardized nursing language. International Journal of Nursing Terminologies and Classifications. 2010;21(2):69–79. doi: 10.1111/j.1744-618X.2010.01148.x. [DOI] [PubMed] [Google Scholar]
- 24.Thoroddsen A, Thorsteinsson H. Nursing diagnosis taxonomy across the Atlantic Ocean: congruence between nurses’ charting and the NANDA taxonomy. Journal of Advanced Nursing. 2002;37(4):372–381. doi: 10.1046/j.1365-2648.2002.02101.x. [DOI] [PubMed] [Google Scholar]