Abstract
Introduction
Brain abscess in pregnancy is very rare, which mostly progresses to neurological abnormalities.
Case Presentation
The patient is a 24-year-old pregnant woman. She was referred to Saitama hospital due to severe headache and nausea on October 2008. Brain MRI detected a 1.5 cm abscess mass with extensive edema in the right frontal lobe. We performed intensive therapy using some antibiotics that included cefotaxime and meropenem and depressants for intracranial pressure for six weeks. There was a good prognosis for the woman and her fetus without any sign of neurological abnormalities.
Conclusion
Early medical intervention is required before it is too late for brain abscess in pregnancy.
Keywords: Brain abscess, Magnetic Resonance Imaging (MRI), Pregnancy
Introduction
Brain abscess caused by bacterial infection has extremely low incidence, and a high mortality rate of 30%. It causes poor prognosis for both mother and fetus, regardless of the state of pregnancy. Unlike non-pregnant women, infection tends to be severe because the immunity power diminishes in pregnant women.
Case Presentation
A 24-year-old woman who lived in Saitama, Japan had three pregnancies, two childbirths, body mass index (BMI) of 22.3, and unremarkable past medical and family histories. Furthermore, her pre pregnancy weight was 55 kg and her height 163 cm.
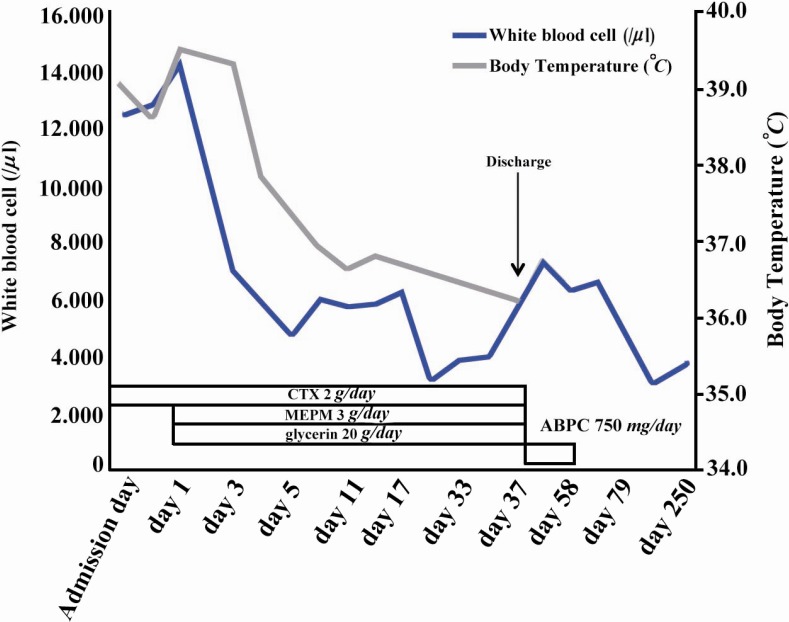
She also had an uneventful first trimester, but developed a fever of >39°C at 22nd week, 1st day of pregnancy. Because of prolonged headache and nausea, she was referred to our hospital in Saitama for complete physical examination on October 2008. On admission, she had blood pressure of 103/51 mmHg, heart rate of 100 beats per min (bpm), body temperature of 39.0°C, mild stiffness in the neck, and cold extremities. No neurological abnormalities, such as consciousness disturbance or paralysis, were observed. However, brain computed tomography (CT) for the prolonged headache revealed a 1.5 cm mass in the right frontal lobe, while hematological analysis showed an elevated white blood cell count of 12,400 cells/µl (neutrophils, 87.7%). Cerebrospinal fluid findings were positive for gram-positive bacteria, an increased cell count (especially for neutrophils) of 2,332 cells/µl, and a low glucose concentration of 30 mg/dl. Brain MRI revealed a 1.5 cm mass with a high intensity signal inside and a low intensity T2 signal on the margin in the deep white matter of the right frontal lobe. Based on the above findings and a high intensity zone surrounding the mass on diffusion-weighted images, she was immediately placed on intensive therapy with concurrent administration of antibiotics cefotaxime (2 g/day) and meropenem (3 g/day), as well as glycerin 20 g/day to reduce intracranial pressure. Table 1 shows a list of examinations performed in search of causal factors, while the results show the isolation of methicillin-sensitive Staphylococcus aureus (MSSA) from the throat. On the other hand, she had no dental problems. Because of unremarkable upper gastrointestinal endoscopy findings and a negative fecal occult blood test result, the possibility of brain metastasis of a malignant tumor was ruled out. After six weeks of intensive therapy with concurrent administration of two antibiotics and glycerin, the headache and nausea disappeared along with a reduction in the number of white blood cells. Subsequent brain MRI at 28th week, 4th day of pregnancy showed no enlargement of the abscess and disappearance of the surrounding edema, with no indication of puncture drainage. At this point, she was switched to oral administration of amoxicillin 750 mg/day for four weeks and was discharged at 29th week, 3rd day of pregnancy. Figure 1 shows the post admission course.
Table 1.
Causes of brain abscess
| Location | Method | Result |
|---|---|---|
| Pharynx | ||
| Culture | MSSA, Corynebacterium | |
| Antigen reaction | Influenza virus: negative | |
| Nasal discharge | Culture | CNS, Corynebacterium |
| Blood | Culture | Negative |
| Merigial flood | Culture | Negative, Cell count: 2352/µl, Glucose: 30 mg/dl |
| Unite | Culture | Negative |
| Vaginal discharge | Culture | Negative |
| Heart | Ultrasound | Infectious endocarditis: not detected |
| Tooth | CT | Dental caries: not detected |
| Lung | CT, Ultrasound | Abscess or inflammation: not detected |
MSSA: methicillin-sensitive staphylococcus aureus, CNS: coaglese negative staphylococcus
Figure 1.
Course of treatment. Body temperature slowed down after the day 7
She vaginally delivered a 2,890 g girl baby at 38th week, 5th day of pregnancy, with no abnormalities. No neurological abnormalities were evident during a five-year follow-up observation conducted over the phone.
MRI findings at the 22nd and 28th week of pregnancy are shown in Figure 2.
Figure 2.
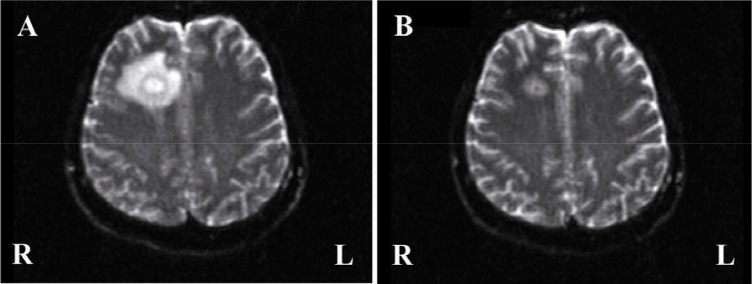
Magnetic resonance images of the brain abscess. Both images are taken by diffusion weighed imaging. A: Axial image at 22ne week of pregnancy shows the large right frontal abscess with severe edema. B: Axial image at 28th week of pregnancy shows no enlargement of the abscess and disappearance of the surrounding edema
Discussion
Despite the extremely low incidence, brain abscess caused by bacterial infection has a high mortality rate of 30% and is therefore a disease with poor prognosis for both mother and fetus, regardless of the state of pregnancy. Although we listed previous reports on brain abscess during pregnancy (Table 2), it should be noted that the number is extremely small (1–6). Approximately, 7% of the previous cases were related to dental treatment (7), but no dental abnormalities were observed in the present case. During the pregnancy, maternal immunity is reduced due to a hormonal imbalance, and according to Lanciers et al., 26.6% of pregnant women, as opposed to 11.0% of non-pregnant women, are significantly infected with Helicobacter pylori (8). It goes without saying that organisms with low pathogenicity under normal circumstances can cause serious infection during pregnancy. In this case, the clear source of infection was not identified. It seems that the pregnant woman whose immunity was diminished is vulnerable to MSSA, which was extremely rare and considered as a serious case.
Table 2.
Brain abacess in pregnancy (Literature review)
| Author | Age | Diagnosis | Location of brain abscess | Cell culture | Internal treatment | Surgical treatment | Neurological prognosis |
|---|---|---|---|---|---|---|---|
| Braun TI (1991) | 25 | 16 GW | Left occipital lobe | Nocardia asteroids | Sulfisozazole, ampicillin, ceftriaxone | Left occipital craniotomy | No residual neurologic deficit |
| Baxi LV | 36 | 10 GW | Left basal ganglion | Propionobacterium acnes, staphylococcus capitis | Cefotaxime, ceftazine, vancomycin | None | Residual hemipares, amenorrhea |
| Wax (2004) | 36 GW | Left temporal lobe | Not detected | Cefepime, vancomycin, metronidazole, dexamethasone, phosphenytion | None | No influence | |
| Kim HC (2007) | 38 | 30 GW | Pituitary | Streptococcus viridians | None | Transsphenoidal microsurgical removal | No influence |
| Jacob CE (2009) | 23 | 35 GW | Left cerebellar hemisphere | Pseudomonas aeruginosa | Penicillin, ciprofloxacin, trimethoprim/sufamethaxaxole | Partial excision of the abscess, modified radical mastoidectomy | Dry left ear, with no residual hearing |
| Hobson DT(2011) | 35 | 21 GW | Left frontal, temporal and parietal lobe | Bacteroides fragilis, Wolinella species, campylobacter gracilis, Prevotella buccae | Dexamethasone, ampicillin, cefotaxime, metronidazole, levetiracetam | Drainage, Lobectomy | Neurologic deficits which included broca's aphasia and apraxia with righ hemiplegia |
| Yoshida M(2013) | 24 | 22 GW | Right frontal lobe | Methicillin sensitives staphylococcus aureus (MSSA) | Cefotaxime, meropenem, amoxicillin, glycerin | None | No influence |
GW: gestational week
The symptoms of brain abscess include headache, nausea, and localized neurological abnormalities (9). Headache is the most common symptom, occurring in 75% of pregnant women, followed by 67% of neurological abnormalities and 58% of altered consciousness (10). Diagnostic imaging is useful for the diagnosis of a brain abscess. Although no adverse effects of MRI have been reported (11, 12), the CT should be avoided as much as possible because there are some problems about the degree of radiation exposure in pregnant women. Therefore, MRI may be a safer and is a highly sensitive diagnostic imaging modality for use in pregnancy (13). Yet, because of potential thermal tissue damage due to the high magnetic field, the National Radiological Protection Board recommends that pregnant women avoid MRI examination during the first trimester.
To treat a brain abscess, it is necessary to select antibiotics capable of effectively crossing the blood brain barrier and their sensitivity should be proven in bacterial culture. The use of steroidal drug is also recommended to prevent an increase in intracranial pressure and the development of brain edema (13). However, because intensive therapy for a brain abscess with antibiotics and steroidal drugs takes somewhere between six to eight weeks, its effect on the fetus is a huge concern. Betamethasone and dexamethasone, which are transported via the placenta, should be avoided because they may affect the development of the fetal central nervous system. Furthermore, the early administration of antiepileptic drugs is recommended because 70% of patients with a brain abscess develop epilepsy (13).
Conclusion
Even infection by vulnerable bacteria becomes serious and early treatment intervention is desirable because immunity power diminishes during the pregnancy.
Acknowledgement
We would like to acknowledge the contributions of many friends and colleagues. For this treatment, we would like to express our thanks to Dr. Masafumi Kato, Dr. Tadashi Aoyama.
To cite this article: Yoshida M, Matsuda H, Furuya K. Successful Prognosis of Brain Abscess during Pregnancy. J Reprod Infertil. 2013;14(3):152-155.
Conflict of Interest
There is no potential conflict of interest for any of the authors. No financial support was received for the treatment. Our treatment obtained ethics approval from the regional ethics committee responsible for human experimentation and conformed to the provisions of the Declaration of Helsinki.
References
- 1.Braun TI, Kerson LA, Eisenberg FP. Nocardial brain abscesses in a pregnant woman. Rev Infect Dis. 1991;13(4):630–2. doi: 10.1093/clinids/13.4.630. [DOI] [PubMed] [Google Scholar]
- 2.Baxi LV, Mayer SA, Mansukhani M. Cerebral abscess and thrombophilia in pregnancy. A case report. J Reprod Med. 2001;46(6):606–8. [PubMed] [Google Scholar]
- 3.Wax JR, Blackstone J, Mancall A, Cartin A, Pinette MG. Sinogenic brain abscess complicating pregnancy. Am J Obstet Gynecol. 2004;191(5):1711–2. doi: 10.1016/j.ajog.2003.12.011. [DOI] [PubMed] [Google Scholar]
- 4.Kim HC, Kang SG, Huh PW, Yoo do S, Cho KS, Kim DS. Pituitary abscess in a pregnant woman. J Clin Neurosci. 2007;14(11):1135–9. doi: 10.1016/j.jocn.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 5.Jacob CE, Kurien M, Varghese AM, Aleyamma TK, Jasper P, Prabu K, et al. Treatment of otogenic brain abscess in pregnancy. Otol Neurotol. 2009;30(5):602–3. doi: 10.1097/MAO.0b013e3181b04d6b. [DOI] [PubMed] [Google Scholar]
- 6.Hobson DT, Imudia AN, Soto E, Awonuga AO. Pregnancy complicated by recurrent brain abscess after extraction of an infected tooth. Obstet Gynecol. 2011;118(2 Pt 2):467–70. doi: 10.1097/AOG.0b013e31822468d6. [DOI] [PubMed] [Google Scholar]
- 7.Pallasch TJ, Slots J. Antibiotic prophylaxis and the medically compromised patient. Periodontol 2000. 1996;10:107–38. doi: 10.1111/j.1600-0757.1996.tb00071.x. [DOI] [PubMed] [Google Scholar]
- 8.Lanciers S, Despinasse B, Mehta DI, Blecker U. Increased susceptibility to Helicobacter pylori infection in pregnancy. Infect Dis Obstet Gynecol. 1999;7(4):195–8. doi: 10.1002/(SICI)1098-0997(1999)7:4<195::AID-IDOG6>3.0.CO;2-R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang SY. Brain abscess: a review of 400 cases. J Neurosurg. 1981;55(5):794–9. doi: 10.3171/jns.1981.55.5.0794. [DOI] [PubMed] [Google Scholar]
- 10.Wax JR, Pinette MG, Blackstone J, Cartin A. Brain abscess complicating pregnancy. Obstet Gynecol Surv. 2004;59(3):207–13. doi: 10.1097/01.ogx.0000115861.54002.8b. [DOI] [PubMed] [Google Scholar]
- 11.Duncan KR. The development of magnetic resonance imaging in obstetrics. Br J Hosp Med. 1996;55(4):178–81. [PubMed] [Google Scholar]
- 12.Nicklas AH, Baker ME. Imaging strategies in the pregnant cancer patient. Semin Oncol. 2000;27(6):623–32. [PubMed] [Google Scholar]
- 13.Lu CH, Chang WN, Lui CC. Strategies for the management of bacterial brain abscess. J Clin Neurosci. 2006;13(10):979–85. doi: 10.1016/j.jocn.2006.01.048. [DOI] [PubMed] [Google Scholar]