Abstract
Background
Although substance use disorders are highly prevalent, resident preparation to care for patients with these disorders is frequently insufficient. With increasing rates of opioid abuse and dependence, and the availability of medication-assisted treatment, one strategy to improve resident skills is to incorporate buprenorphine treatment into training settings.
Methods
Residency faculty delivered our BupEd education and training program to 71 primary care residents. BupEd included: 1) a didactic session on buprenorphine, 2) an interactive motivational interviewing session, 3) monthly case conferences, and 4) supervised clinical experience providing buprenorphine treatment. To evaluate BupEd, we assessed: 1) residents' provision of buprenorphine treatment during residency, 2) residents' provision of buprenorphine treatment after residency, and 4) treatment retention among patients treated by resident versus attending physicians.
Results
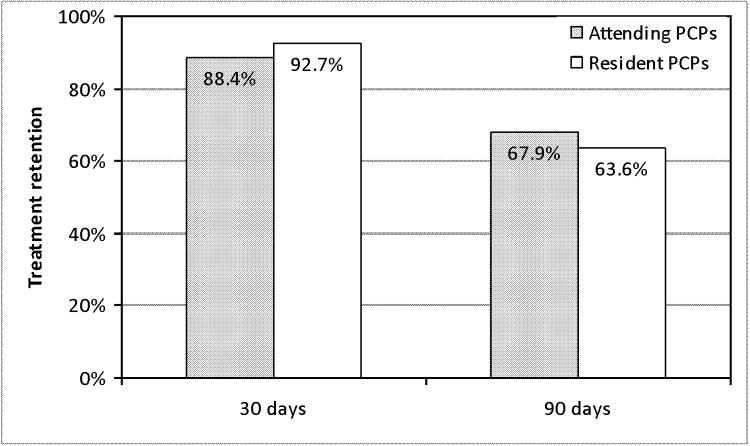
Of 71 residents, most served as a covering or primary provider to at least one buprenorphine-treated patient (84.5 and 66.2% respectively). Of 40 graduates, 27.5% obtained a buprenorphine waiver and 17.5% prescribed buprenorphine. Treatment retention was similar between patients cared for by resident PCPs versus attending PCPs ((90-day retention: 63.6% (n=35) vs. 67.9% (n=152), p=0.55)).
Conclusion
BupEd is feasible, provides residents with supervised clinical experience in treating opioid dependent patients, and can serve as a model to prepare primary care physicians to care for patients with opioid dependence.
Keywords: Opioid dependence, buprenorphine, substance abuse education
Background and Objectives
Opioid abuse and dependence is a growing problem in the United States, and a significant contributor to mortality (1-5). In the last decade, buprenorphine, a partial opioid agonist, was approved for the treatment of opioid dependence in general medical care, permitting physicians to offer medication-assisted treatment outside of specialized drug treatment settings. Access to buprenorphine has been slowly increasing; in 2009, a total of 640,000 patients received buprenorphine from 19,000 certified providers (6-8). Yet, need for treatment still exceeds access. With more than 2 million opioid-dependent people in the United States, the majority do not receive treatment with opioid agonist medications (2;4).
To realize buprenorphine's full potential in treating opioid dependence, additional providers are needed for its incorporation into general medical settings. Without adequate training to treat patients with opioid dependence, new physicians cannot be expected to use buprenorphine effectively. A further barrier to meeting treatment need is the requirement for buprenorphine prescribers to undergo eight hours of training to obtain a federal “waiver” to be able to prescribe buprenorphine for opioid dependence.
Despite the need for additional providers to care for a growing opioid-dependent population, residency programs continue to inadequately prepare trainees. A recent statement from an expert panel highlights the urgency of integrating substance abuse competencies into graduate medical education (9). The panel's specific training recommendations include that trainees be provided with the appropriate network of experienced faculty, a system to support desired clinical skills and behaviors, and multiple opportunities to practice desired clinical skills and behaviors. The panel also recommended that appropriate didactic and experiential curricula and personalized feedback are needed to support these skills and behaviors (10-12). These expert recommendations are consistent with studies of practicing physicians which have identified such barriers as lack of access to clinical expertise, and need for additional clinical experience as reasons for failure to incorporate buprenorphine into practice (13-18).
Consistent with these expert recommendations, and to address known barriers, we created “BupEd,” an education and training program for primary care residents. The objective of BupEd was to provide residents with didactic and experiential training in treating patients with buprenorphine for opioid dependence. We also conduct an evaluation of BupEd to: 1) examine residents' provision of buprenorphine treatment during their residency training, 2) examine residents' provision of buprenorphine treatment after completing their residency training, and 3) compare buprenorphine treatment retention among patients of resident physicians versus attending physicians.
Methods
Educational Setting
The educational setting for BupEd is a 30-resident Primary Care-Social Internal Medicine (PCSM) Program within an Internal Medicine residency program. The PCSM Program prepares residents for careers in primary care focused on caring for urban underserved populations. The PCSM Program includes 12 ambulatory (block) months during the 36-month residency training program. Each ambulatory block includes case-based teaching, didactics, and skills practice on ambulatory topics. The PCSM Program's pre-existing substance abuse curriculum included eight hours of didactic and experiential curriculum (in the PGYI year) that addresses the biology of addiction, the consequences and treatment of alcohol, opioid, and stimulant abuse and dependence, and skills practice in screening and brief counseling for patients with substance use disorders. In the PGY3 year, residents participate in a 3-5 day immersion training at a residential drug treatment program and a 4-hour substance abuse-specific objective structured clinical exam (19-21).
Clinical Setting
The clinical setting for our BupEd Program is the PCSM Program's ambulatory clinical site, a federally qualified health center (FQHC) located in the Bronx, NY. The neighborhood surrounding the FQHC has the highest rate of premature mortality of all New York City neighborhoods (22). Leading causes of premature mortality in the neighborhood are HIV/AIDS and drug use (22).
The FQHC provides comprehensive services including adult and pediatric medicine, obstetrics/gynecology, and other specialty and ancillary services. Of the 15,000 adult patients receiving care, over 65% have public insurance and most have incomes below the federal poverty line. All attending and resident physicians maintain continuity patient panels at the FQHC. All attending physicians also precept residents in their continuity practices. Of the 13 internal medicine attending physicians at the FQHC, six were waivered to prescribe buprenorphine at the time of this evaluation. A part-time buprenorphine care manager is available to provide patient education and supportive counseling, assist with patients' medication refills, and coordinate patient care.
BupEd: Buprenorphine Education and Training Curriculum
We designed BupEd, a didactic and case-based curriculum that focuses on buprenorphine treatment for opioid dependence to enhance the existing PCSM substance abuse curriculum [21]. The BupEd curriculum included four new components: 1) a new didactic 1-hour session on buprenorphine, 2) a 2-hour interactive session on motivational interviewing, 3) monthly 1-hour case conferences for residents on ambulatory rotations, and 4) supervised clinical experience providing buprenorphine treatment. Topics covered in the didactic session include indications for and contraindications to buprenorphine treatment in office-based settings, pharmacologic properties of buprenorphine, and unique challenges associated with buprenorphine inductions. The motivational interviewing session consists of two parts. In the first part, residents learn key principles of motivational interviewing in a didactic format. In the second part, residents practice key motivational interviewing skills including active listening, reflecting “change talk,” and negotiating a plan. Residents practice skills through structured group exercises and role plays. In case conferences, residents present patients with opioid use problems to several attending physicians experienced in providing buprenorphine treatment.
BupEd's fourth component provides residents with supervised clinical experiences providing buprenorphine treatment. Residents incorporate opioid-dependent patients interested in buprenorphine treatment into their continuity panels in two ways. In the first scenario, residents are referred new patients who enroll in the buprenorphine treatment program at the FQHC (23). In the second scenario, residents identify and offer their existing FQHC patients treatment with buprenorphine. Residents who indicate that they are interested in providing buprenorphine treatment are preferentially, but not exclusively, assigned newly referred patients. Waivered, experienced attending physicians are available to residents during clinical sessions to precept cases related to opioid-dependence, assess clinical appropriateness for buprenorphine treatment, and supervise induction or maintenance treatment with buprenorphine, including providing buprenorphine prescriptions. A part-time buprenorphine care manager is available to assist with patient follow-up, and counseling patients about substance use and relapse.
Evaluation of BupEd
To evaluate BupEd, we examined residents' provision of buprenorphine treatment during their residency training, determining the proportion of residents who served as a primary care provider (PCP) to a buprenorphine-treated patient, and who served as a covering provider to at least one buprenorphine-treated patient. We evaluated residents' provision of buprenorphine treatment after completing residency by determining the number of residents who obtained buprenorphine waivers and prescribed buprenorphine following graduation from the PCSM Program. Finally, we examined patient outcomes by comparing buprenorphine treatment retention of resident physicians' patients versus attending physicians' patients. The study was approved by the affiliated Institutional Review Board.
Measures and Data
Cohort and its characteristics
Using electronic medical records, we identified all patients who initiated buprenorphine treatment at our FQHC from 2006 through 2009. We then extracted these patients' demographic, visit and prescription data. Available demographic data included age, self-identified race/ethnicity (Hispanic, non-Hispanic black, non-Hispanic other), primary language (English, Spanish), and gender (male, female).
Primary care provider (PCP)
To determine each patient's primary care provider (PCP), we examined all visits by academic year (July–June), and calculated the number of visits each patient had with any given physician. The physician with whom the patient had had the majority of visits in a given academic year was defined as the PCP for that year. We then categorized each patient's PCP each year as either a resident or attending physician.
Post-residency experience
To determine post-residency experience with buprenorphine, we contacted all residents who graduated from the PCSM Program between 2006 and 2009 via email in 2011 to inquire whether they had obtained a buprenorphine waiver and whether they had prescribed buprenorphine in clinical practice. Two contact attempts were made; non-responders were assumed to have not obtained a waiver and have not prescribed buprenorphine.
Buprenorphine treatment retention
We defined 30-day retention as a visit or active buprenorphine prescription 30-60 days after the patient's initial buprenorphine prescription. We defined 90-day retention as a visit or active buprenorphine prescription 90-120 days after the patient's initial buprenorphine prescription.
Statistical Analysis
To examine residents' experiences with providing buprenorphine treatment during residency, we calculated simple frequencies to determine the number and proportion of residents who served as a PCP to a buprenorphine-treated patient and who served as a covering provider to a buprenorphine-treated patient. To determine residents' experiences with providing buprenorphine after completing residency, we calculated the number and proportion of graduates who had obtained waivers and prescribed buprenorphine. To examine patient outcomes, we compared characteristics and retention rates between patients with resident PCPs versus attending PCPs using chi-square, Fisher Exact, or student t tests as appropriate. Analyses were conducted using SAS, v9.2.
Results
From 2006 through 2009, of the 71 residents in the PCSM Program, all participated in the didactic portion of the BupEd Program. During that time period, 279 patients were treated with buprenorphine, representing 1.9% of the total adult patient population in the adult internal medicine practice at the FQHC. Forty seven (66.2%) residents served as a PCP to at least one buprenorphine-treated patient, and 60 (84.5%) residents served as a covering provider to at least one buprenorphine-treated patient. The median number of patients that each resident cared for as the PCP was 1, with a range of 0-13.
Of the 40 PCSM Program graduates from 2006-2009, 11 (27.5%) had obtained a buprenorphine waiver, and 7 (17.5%) had prescribed buprenorphine in practice.
Characteristics of 55 patients cared for by resident PCPs versus 224 patients cared for by attending PCPs did not differ, except for language (attending physicians were more likely than resident physicians to care for patients who were Spanish-speaking, see Table). Retention at 30 and 90 days did not differ between patients cared for by resident PCPs and patients cared for by attending PCPs. At 30 days, 51 (92.7%) patients cared for by resident PCPs and 198 (88.4%) patients cared for by attending PCPs were retained in buprenorphine treatment (p=0.35). At 90 days, 35 (63.6%) patients cared for by resident PCPs and 152 (67.9%) patients cared for by attending PCPs were retained in buprenorphine treatment (p=0.55) (see Figure).
Table. Characteristics of buprenorphine-treated patients with attending and resident physicians as primary care providers.
| Patient Characteristics | Attending as PCP (N=224) n (%) | Resident as PCP (N=55) n (%) |
|---|---|---|
|
| ||
| Mean age, years ± SD | 42.8 ± 10.1 | 45.4 ± 9.4 |
|
| ||
| Male gender | 161 (71.9) | 40 (72.7) |
|
| ||
| Race/ethnicity: | ||
| Hispanic | 153 (69.5) | 42 (77.8) |
| Non-Hispanic black | 39 (17.7) | 8 (14.8) |
| Non-Hispanic white | 16 (7.3) | 2 (3.7) |
| Non-Hispanic other | 12 (5.5) | 2 (3.7) |
|
| ||
| Spanish as preferred language | 62 (27.9)* | 9 (17.0) |
PCP= Primary care provider.
Percentages indicate column percentages.
Data are missing for race/ethnicity (n=5) and preferred language (n=4).
p<0.05.
Figure 1. 30-day and 90-day Buprenorphine treatment retention among patients with attending physicians versus resident physicians as primary care providers (PCPs).
Discussion
We developed and integrated a buprenorphine education and training curriculum, BupEd, into a primary care internal medicine residency program using didactic and experiential strategies. The majority of residents gained experience in providing buprenorphine treatment, and two-thirds had the opportunity to serve as a PCP to a buprenorphine-treated patient. Nearly one quarter of graduates obtained buprenorphine waivers following graduation, and 17% prescribed buprenorphine through June, 2011. Retention in buprenorphine treatment was similar between patients of resident and attending physicians.
Since buprenorphine's approval in 2002, physician uptake of prescribing buprenorphine has been gradual. Physicians who are not trained in addiction medicine are typically required to take an 8-hour training course, which then allows them to apply for a waiver to prescribe buprenorphine. This process may present a barrier to providing buprenorphine. To understand additional barriers to prescribing buprenorphine, a number of studies have queried potential buprenorphine prescribers as well as attendees of buprenorphine-waiver courses. These studies indicate that barriers to providing treatment for opioid dependence among practicing physicians are many, even among physicians electing to attend buprenorphine waiver courses. These barriers include lack of clinical experience, access to a substance abuse experts, concerns about difficulty of induction, and other logistics (13-17).
Based on previously identified barriers and the recognition that uptake of buprenorphine-prescribing has been slow, we developed and delivered BupEd, a buprenorphine education and training program for primary care residents, targeting physicians-in-training to promote adoption of this new clinical practice. Previous work has described and evaluated the incorporation of substance abuse teaching into residency curricula (19;20), or targeted chief residents to promote downstream dissemination (25). We are aware of two studies that examined buprenorphine treatment outcomes in clinics which included resident physicians (26;27). However, neither study described how residents were trained to provide buprenorphine treatment or the extent of residents' experiences providing buprenorphine treatment during and after their residency programs. To our knowledge, we are the first to describe a buprenorphine education and training curriculum for residents and to evaluate the impact of this curriculum on residents' experiences during and after residency and on patient outcomes.
In the context of a larger substance abuse curriculum, BupEd delivers specific didactic content and provides opportunities to provide buprenorphine treatment. It includes access to clinical experts on addiction, provides ongoing supervision and mentorship, and thereby seeks to address barriers previously identified (9;11;12;28). In addition, by focusing on physicians-in-training we targeted physicians at an early point in their medical career, when scope and patterns of practice are being developed. Only by increasing the number of physicians who are experienced in and willing to provide buprenorphine in primary care settings, will access to treatment for opioid dependence be meaningfully expanded.
Our study demonstrated that primary care residents receiving buprenorphine education and training to care for patients with opioid dependence can incorporate this aspect of medical care into practice during residency training. In addition, our education and training program attracted nearly one-fifth of graduated residents to prescribe buprenorphine in practice after completion of residency. Importantly, patient outcomes were not compromised, as we observed similar buprenorphine treatment retention rates as those found in other studies of buprenorphine treatment in primary care settings. Specifically, patients cared for by residents in our program had a 90-day treatment retention rate of 64%, which is comparable to retention rates of 50-93% over 90-180 days reported by others (27;29-32).
There are some important limitations to our findings. We conducted our program in a primary care-internal medicine training program. We believe that our outcomes are generalizable to other primary care training programs in family medicine and internal medicine, but also acknowledge that our PCSM program attracts a cohort of residents interested in providing care to urban underserved populations. Thus, our residents may be particularly amenable to incorporating substance abuse treatment into practice. In addition, we have a number of clinical faculty who are experienced in managing opioid-dependent patients and in providing medical education. An additional limitation is the absence of a comparison group of residents. Because the BupEd program was established at the same time the buprenorphine treatment program was established, we felt the use a historical cohort of residents would not strengthen our findings.
Having a buprenorphine care manager may have contributed to the positive retention rates – though she provided services to patients who were cared for by both residents and attendings. Because our administrative data could not capture her services, we could not assess whether patients of residents and attendings used her services differentially, and therefore differentially affected retention rates. Because data were extracted from electronic medical records, we were not able to fully characterize patients' and residents' characteristics, which could have been related to treatment outcomes. Finally, we did not examine patients' drug use. However, many studies have demonstrated a close association between treatment retention and abstinence (32-35).
Despite these limitations, we have described a successful program to incorporate buprenorphine education and training into internal medicine training. Our evaluation demonstrates patients with primary care residents as a PCP achieved retention rates similar to patients with attending physicians as a PCP. Our study suggests that integration of buprenorphine education into primary care residency is feasible and can be an effective strategy to facilitate physician adoption of buprenorphine treatment into medical practice. Furthermore, BupEd, which provides a supervised experience in caring for patients with substance use disorders, can serve as a model to prepare primary care physicians to care for patients with opioid dependence.
Acknowledgments
We would like to acknowledge the PCSM residents and waivered CHCC physicians who participated in this study.
Financial Support: Health Resources and Services Administration (HRSA), Residency Training in Primary Care Grant, D58HP10330; HRSA, HIV/AIDS Bureau, Special Projects of National Significance, grant 6H97HA00247; the Center for AIDS Research at the Albert Einstein College of Medicine and Montefiore Medical Center (NIH AI-51519); NIH R25DA023021; and the Robert Wood Johnson Foundation's Harold Amos Medical Faculty Development Program.
Footnotes
Presented in part at: Society of General Internal Medicine Annual Conference (April, 2009, Miami, FL) and the Annual Conference of the Association for Medical Education and Research in Substance Abuse (November 2010, Bethesda, MD)
References
- 1.Cicero TJ, Inciardi JA, Munoz A. Trends in abuse of Oxycontin and other opioid analgesics in the United States: 2002-2004. J Pain. 2005;6(10):662–72. doi: 10.1016/j.jpain.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 2.Substance Abuse and Mental Health Services Administration, Office of Applied Studies. Results from the 2007 National Survey on Drug Use and Health: National Findings. 2008 NSDUH Series H-34 DHHS Publication No. SMA 08-4343. [Google Scholar]
- 3.Substance Abuse and Mental Health Services Administration, Office of Applied Studies. Drug Abuse Warning Network, 2006: National Estimates of Drug-Related Emergency Department Visits. 2008 [Google Scholar]
- 4.Substance Abuse and Mental Health Services Administration, Office of Applied Studies. Highlights - 2007 National Admissions to Substance Abuse Treatment Services, DASIS Series: S-45 2009. Rockville,MD: Treatment Episode Data Set (TEDS) DHHS Publication No.(SMA)09-4360. [Google Scholar]
- 5.Paulozzi LJ, Budnitz DS, Xi Y. Increasing deaths from opioid analgesics in the United States. Pharmacoepidemiol Drug Saf. 2006;15(9):618–27. doi: 10.1002/pds.1276. [DOI] [PubMed] [Google Scholar]
- 6.Arfken CL, Johanson CE, di MS, Schuster CR. Expanding treatment capacity for opioid dependence with office-based treatment with buprenorphine: National surveys of physicians. J Subst Abuse Treat. 2010;39(2):96–104. doi: 10.1016/j.jsat.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 7.Clark HW. The State of Buprenorphine Treatment; Presented at: Buprenorphine in the Treatment of Opioid Addiction: Reassessment; 2010; Accessed at: http://buprenorphinesamhsagov/bwns/2010_presentations_pdf/01_Clark_508 pdf on February 4, 2011. [Google Scholar]
- 8.Fiellin DA. The first three years of buprenorphine in the United States: Experience to date and future directions. J Addict Med. 2007;1:62–7. doi: 10.1097/ADM.0b013e3180473c11. [DOI] [PubMed] [Google Scholar]
- 9.O'Connor PG, Nyquist JG, McLellan AT. Integrating addiction medicine into graduate medical education in primary care: the time has come. Ann Intern Med. 2011;154(1):56–9. doi: 10.7326/0003-4819-154-1-201101040-00008. [DOI] [PubMed] [Google Scholar]
- 10.el-Guebaly N, Toews J, Lockyer J, Armstrong S, Hodgins D. Medical education in substance-related disorders: components and outcome. Addiction. 2000;95(6):949–57. doi: 10.1046/j.1360-0443.2000.95694911.x. [DOI] [PubMed] [Google Scholar]
- 11.Seale JP, Shellenberger S, Clark DC. Providing competency-based family medicine residency training in substance abuse in the new millennium: a model curriculum. BMC Med Educ. 2010;10:33. doi: 10.1186/1472-6920-10-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jackson AH, Alford DP, Dube CE, Saitz R. Internal medicine residency training for unhealthy alcohol and other drug use: recommendations for curriculum design. BMC Med Educ. 2010;10:22. doi: 10.1186/1472-6920-10-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cunningham CO, Kunins HV, Roose RJ, Elam RT, Sohler NL. Barriers to obtaining waivers to prescribe buprenorphine for opioid addiction treatment among HIV physicians. J Gen Intern Med. 2007;22(9):1325–9. doi: 10.1007/s11606-007-0264-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Netherland J, Botsko M, Egan JE, Saxon AJ, Cunningham CO, Finkelstein R, et al. Factors affecting willingness to provide buprenorphine treatment. J Subst Abuse Treat. 2009;36(3):244–251. doi: 10.1016/j.jsat.2008.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Turner BJ, Laine C, Lin YT, Lynch K. Barriers and facilitators to primary care or human immunodeficiency virus clinics providing methadone or buprenorphine for the management of opioid dependence. Arch Intern Med. 2005;165(15):1769–76. doi: 10.1001/archinte.165.15.1769. [DOI] [PubMed] [Google Scholar]
- 16.Gunderson EW, Fiellin DA, Levin FR, Sullivan LE, Kleber HD. Evaluation of a combined online and in person training in the use of buprenorphine. Subst Abus. 2006;27(3):39–45. doi: 10.1300/J465v27n03_06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sullivan LE, Tetrault J, Bangalore D, Fiellin DA. Training HIV physicians to prescribe buprenorphine for opioid dependence. Subst Abus. 2006;27(3):13–8. doi: 10.1300/J465v27n03_03. [DOI] [PubMed] [Google Scholar]
- 18.Walley AY, Alperen JK, Cheng DM, Botticelli M, Castro-Donlan C, Samet JH, et al. Office-based management of opioid dependence with buprenorphine: clinical practices and barriers. J Gen Intern Med. 2008;23(9):1393–8. doi: 10.1007/s11606-008-0686-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Parish SJ, Ramaswamy M, Stein MR, Kachur EK, Arnsten JH. Teaching about Substance Abuse with Objective Structured Clinical Exams. J Gen Intern Med. 2006;21(5):453–9. doi: 10.1111/j.1525-1497.2006.00426.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stein MR, Parish SJ, Arnsten JH. The OSCE as a formative evaluation tool for substance abuse teaching. Med Educ. 2005;39(5):529–30. doi: 10.1111/j.1365-2929.2005.02147.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stein M, Arnsten JH, Parish SJ, Kunins HV. Evaluation of a substance use disorder curriculum for internal medicine residents. Subsst Abus. 2011;32(4):220–4. doi: 10.1080/08897077.2011.598408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Olson EC, Van WG, Kerker B, Thorpe L, Frieden TR. Take care Highbridge and Morrisania. NYC Community Health Profiles. (Second) 2006;6(42):16. [Google Scholar]
- 23.Cunningham C, Giovanniello A, Sacajiu G, Whitley S, Mund P, Beil R, et al. Buprenorphine treatment in an urban community health center: what to expect. Fam Med. 2008;40(7):500–6. [PMC free article] [PubMed] [Google Scholar]
- 24.Egan JE, Casadonte P, Gartenmann T, Martin J, Cance-Katz EF, Netherland J, et al. The Physician Clinical Support System-Buprenorphine (PCSS-B): a novel project to expand/improve buprenorphine treatment. J Gen Intern Med. 2010;25(9):936–41. doi: 10.1007/s11606-010-1377-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alford DP, Bridden C, Jackson AH, Saitz R, Amodeo M, Barnes HN, et al. Promoting substance use education among generalist physicians: an evaluation of the Chief Resident Immersion Training (CRIT) program. J Gen Intern Med. 2009;24(1):40–7. doi: 10.1007/s11606-008-0819-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Colameco S, Armando J, Trotz C. Opiate dependence treatment with buprenorphine: one year's experience in a family practice residency setting. J Addict Dis. 2005;24(2):25–32. doi: 10.1300/J069v24n02_03. [DOI] [PubMed] [Google Scholar]
- 27.Soeffing JM, Martin LD, Fingerhood MI, Jasinski DR, Rastegar DA. Buprenorphine maintenance treatment in a primary care setting: outcomes at 1 year. J Subst Abuse Treat. 2009;37(4):426–30. doi: 10.1016/j.jsat.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 28.Shellenberger S, Seale JP, Harris DL, Johnson JA, Dodrill CL, Velasquez MM. Applying team-based learning in primary care residency programs to increase patient alcohol screenings and brief interventions. Acad Med. 2009;84(3):340–6. doi: 10.1097/ACM.0b013e3181972855. [DOI] [PubMed] [Google Scholar]
- 29.Lee JD, Grossman E, DiRocco D, Gourevitch MN. Home buprenorphine/naloxone induction in primary care. J Gen Intern Med. 2009;24(2):226–32. doi: 10.1007/s11606-008-0866-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alford DP, LaBelle CT, Richardson JM, O'Connell JJ, Hohl CA, Cheng DM, et al. Treating homeless opioid dependent patients with buprenorphine in an office-based setting. J Gen Intern Med. 2007;22(2):171–6. doi: 10.1007/s11606-006-0023-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stein MD, Cioe P, Friedmann PD. Buprenorphine retention in primary care. J Gen Intern Med. 2005;20(11):1038–41. doi: 10.1111/j.1525-1497.2005.0228.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.O'Connor PG, Oliveto AH, Shi JM, Triffleman EG, Carroll KM, Kosten TR, et al. A randomized trial of buprenorphine maintenance for heroin dependence in a primary care clinic for substance users versus a methadone clinic. Am J Med. 1998;105(2):100–5. doi: 10.1016/s0002-9343(98)00194-6. [DOI] [PubMed] [Google Scholar]
- 33.Johnson RE, Chutuape MA, Strain EC, Walsh SL, Stitzer ML, Bigelow GE. A comparison of levomethadyl acetate, buprenorphine, and methadone for opioid dependence. N Engl J Med. 2000;343(18):1290–7. doi: 10.1056/NEJM200011023431802. [DOI] [PubMed] [Google Scholar]
- 34.Mintzer IL, Eisenberg M, Terra M, MacVane C, Himmelstein DU, Woolhandler S. Treating opioid addiction with buprenorphine-naloxone in community-based primary care settings. Ann Fam Med. 2007;5(2):146–50. doi: 10.1370/afm.665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mattick RP, Kimber J, Breen C, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev. 2004;(3):CD002207. doi: 10.1002/14651858.CD002207.pub2. [DOI] [PubMed] [Google Scholar]