Abstract
Rationale
Recently, products containing synthetic cannabinoids, collectively referred to as Spice, are increasingly being used recreationally.
Objectives
The availability, acute subjective effects—including self-reports posted on Erowid—laboratory detection, addictive potential, and regulatory challenges of the Spice phenomenon are reviewed.
Results
Spice is sold under the guise of potpourri or incense. Unlike THC, the synthetic cannabinoids present in Spice are high-potency, high-efficacy, cannabinoid-receptor full agonists. Since standard urine toxicology does not test for the synthetic cannabinoids in Spice, it is often used by those who want to avoid detection of drug use. These compounds have not yet been subjected to rigorous testing in humans. Acute psychoactive effects include changes in mood, anxiety, perception, thinking, memory, and attention. Adverse effects include anxiety, agitation, panic, dysphoria, psychosis, and bizarre behavior. Psychosis outcomes associated with Spice provide additional data linking cannabinoids and psychosis. Adverse events necessitating intervention by Poison Control Centers, law enforcement, emergency responders, and hospitals are increasing. Despite statutes prohibiting the manufacture, distribution, and sale of Spice products, manufacturers are replacing banned compounds with newer synthetic cannabinoids that are not banned.
Conclusions
There is an urgent need for better research on the effects of synthetic cannabinoids to help clinicians manage adverse events and to better understand cannabinoid pharmacology in humans. The reported psychosis outcomes associated with synthetic cannabinoids contribute to the ongoing debate on the association between cannabinoids and psychosis. Finally, drug-detection tests for synthetic cannabinoids need to become clinically available.
Keywords: synthetic cannabinoids, cannabinoids, CB1, cannabis, THC, Spice, K2
Introduction
A relatively recent phenomenon, Spice and its psychoactive constituents, synthetic cannabinoids, represent an increasingly popular trend in substance use for which researchers and clinicians have insufficient data. There have been several excellent reviews on the Spice phenomenon that have covered many of the important issues (Ashton 2012; Bhatty and Wu 2013; Castellanos and Thornton 2012; Fattore and Fratta 2011; Gunderson et al. 2012; Harris and Brown 2013; Loeffler et al. 2012; McGuinness and Newell 2012; Psychoyos and Vinod 2013; Seely et al. 2012). Building on existing reviews, our paper examines aspects not previously covered by including the rich, informative literature on the subjective effects of Spice posted on the Erowid website. To our knowledge this is the first time this data has been presented in the medical literature. The Erowid literature is critical, given the lack of any controlled data on Spice or its constituent cannabinoids.
Despite well-intentioned regulatory efforts, Spice use has increased along with its psychiatric, medical, and social consequences. Thus, there is a need for more research and controlled studies to investigate Spice and synthetic cannabinoids. Clinicians may be most interested in a review of Spice for its increasing popularity and abuse potential. However, reviewing the effects of the synthetic cannabinoids present in Spice may also enhance our knowledge of the brain’s cannabinoid system, since most of what we know is based on the effects of delta-9-tetrahydrocannabinol (THC)—a low-efficacy, partial agonist of brain-cannabinoid receptors.
The current review covers all known symptoms and ramifications of Spice use by synthesizing clinical reports, surveys, epidemiological data, and the unique subjective reports of users themselves documented in Erowid self-reports. Special emphasis is placed on psychotic symptoms, which are often the most obvious and disturbing consequences of acute and chronic Spice use.
1. What is Spice?
Spice refers to a group of commercially available psychoactive products containing one or more synthetic cannabinoids sprayed onto an herbal substrate. The name may be a reference to the intergalactic spice at the center of Frank Herbert’s novel, Dune (Ashton 2012; Vearrier and Osterhoudt 2010). These products are marketed under various names, some of which may denote the intensity or type of high a user might experience (Auwarter et al. 2009; Chainsaw 2009). Hereafter, Spice will be the catch-all term for these substances.
Manufacturers in the U.S. allegedly obtain synthetic cannabinoids from distributors overseas (Piggee 2009). The synthetic cannabinoids are then dissolved in a solvent and sprayed onto dried plant material. Once the solvent evaporates and the plant material is dried again, the product can be crushed and packaged (Musah et al. 2012). Spice is packaged either as a loose-leaf or pre-rolled product, though it has occasionally been sold in powder form (Kikura-Hanajiri et al. 2011). It is typically smoked through a conventional cannabis pipe, a water pipe, or in cigarette papers (Deluca et al. 2009). Various flavors have been added to Spice, possibly to justify the marketing of some Spice products as potpourri. Certain flavors may also correlate with specific synthetic cannabinoids and plant-based materials (Zuba et al. 2011).
1.1 History
Recreational use of Spice most likely started in Europe, where as early as 2004 it was sold over the internet and in head shops (Bryner 2010; Deluca et al. 2009). These “designer drugs” were introduced onto the drug-use market as “legal highs” or “herbal highs” (Zawilska 2011). Packages listed only herbal ingredients—some of which have known cannabis-like properties—and not synthetic cannabinoids, leaving users to speculate what the active agents were. It was not until 2008 that synthetic cannabinoids were formally detected in specimens (Deluca et al. 2009; Schifiano et al. 2009). The first formal report of Spice trafficking in the United States was in December 2008 (Leonhart 2012). Since then, reports of Spice abuse have increased exponentially.
1.2 Availability, Cost, Marketing, and Labeling
In Europe and the United States, a 3-gram packet of Spice typically sells for between 20 to 30 Euros and 30 to 40 dollars, respectively (Schifiano et al. 2009; Wehrman 2011). These products are primarily bought from head shops, gas stations, convenience stores, and over the internet (Vandrey et al. 2012). They are often marketed as incense, fragrance, and potpourri with labels stating “not for human consumption” and “not suitable for under 18” (Figure 1 & 2). The advertising for different brands suggests that consumers are aware the psychoactive effects are similar to products marketed as Spice (European Monitoring Centre for Drugs and Drug Addiction 2009).
Figure 1.
Spice Products
Figure 2.
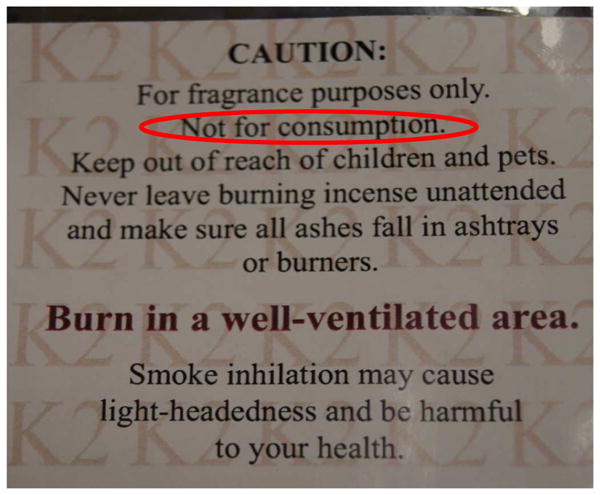
Deceptive Labeling of Spice Products
1.3 The Growing Phenomenon of Spice
In the U.S., Spice has become the second most frequently used illicit substance after cannabis (NIDA 2012). The synthetic drug industry that includes Spice is growing at an estimated $5 billion a year, according to Rick Broider, president of the North American Herbal Incense Trade Association (Rose 2012). The promise of a stronger high than cannabis, easy access, affordability, a perception that the products are legal, and the difficulty detecting these compounds in standard urine toxicology tests have likely contributed to Spice’s growing popularity and use. There is growing public awareness about serious negative psychiatric effects associated with Spice consumption that necessitate calls to Poison Control Centers, emergency care, and hospitalization (AAPCC 2011; Benford and Caplan 2011; Hoyte et al. 2012; McGuinness and Newell 2012; Van der Veer and Fiday 2011). According to the American Association of Poison Control Centers’ (AAPCC) National Poison Data System (NPDS) there were 112 calls concerning Spice in 2009 and 2,915 in 2010 (AAPCC 2011). Between January 2011 and April 2012 there have been 11,561 calls, clearly indicating a rapid increase (Wood 2013). The use of Spice is increasing amongst youth in the United States. In the most recent Monitoring the Future survey, 11.3% of high school seniors nationwide admitted to using Spice in the previous year, compared to 36.4% who admitted to using cannabis in the past year (NIDA 2012). In the AAPCC data, the most represented age group was 13–19 year olds, comprising 48.8% of the calls (Wood 2013).
1.4 Synthetic Cannabinoids: The principal psychoactive constituents of Spice
Phytocannabinoids, or plant-derived cannabinoids, include delta-9-tetrahydrocannabinol (THC), the principal psychoactive component of cannabis. THC is a low-efficacy partial agonist of cannabinoid (CB) receptors. There are at least two identified CB receptors, CB1R (CB1 receptors) and CB2R (CB2 receptors). CB1Rs are expressed primarily in the brain and are responsible for the psychoactive effects of cannabinoids. In contrast, CB2Rs are localized primarily in the periphery on immune cells where they mediate the immunomodulatory effects of cannabinoids (Devane et al. 1988; Pertwee 2008; Schatz et al. 1997). Over the last three decades, a number of cannabinoids have been synthesized. Unlike THC, the synthetic cannabinoids in Spice are high-potency full agonists at the brain CB1 receptor (see table 1) (Atwood et al. 2010; Atwood et al. 2011; Huffman and Padgett 2005; Huffman et al. 2005b; Lindigkeit et al. 2009; Marriott and Huffman 2008). The synthetic cannabinoids present in Spice are classic cannabinoids, naphtoylindoles, benzoylindones, or phenylacetylindoles (Table 1). Of note, the synthetic cannabinoids obtained from online vendors were of comparable purity to validated standards (Ginsburg et al. 2012). Furthermore, there is significant variability in the type and amount of synthetic cannabinoids between Spice products, between batches of the same product, and within a package (European Monitoring Centre for Drugs and Drug Addiction 2009). In addition to synthetic cannabinoids, Spice has been reported to contain preservatives, additives, fatty acids, amides, esters, the benzodiazepine phenazepam, and an active metabolite of Tramadol (Brown 2011; Dresen et al. 2010; Zuba et al. 2011). The psychotropic agents Salvia divinorum, Kratom, and cannabis have also been detected in a few Spice products (Ogata et al. 2013). It is unknown to what extent these added chemicals and excipients contribute to Spice’s effects.
Table 1.
Affinity of Cannabinoids present in Spice for CB1 and CB2 receptors
| Compound | Type | CB1 Ki (nM) | CB2 Ki (nM) |
|---|---|---|---|
| Delta-9-THC | Classic Cannabinoid | 41 | 36 ± 10 |
|
| |||
| HU-210 | Classic Cannabinoid | 0.061 | 0.17 |
| AM-694 | Benzoylindone | 0.08 | 1.4 |
| RCS-4* | Benzoylindone | unknown | unknown |
| WIN-48,098 | Benzoylindone | 3155 | unknown |
| CP-47,497 | Cyclohexylphenol | 2.2 ± 0.5 | none detected |
| JWH-018 | Naphtoylindole | 9 ± 5 | 2.9 ± 2.7 |
| JWH-019 | Naphtoylindole | 9.8 ± 2 | 5.55 ± 2 |
| JWH-073 | Naphtoylindole | 8.9 ± 1.8 | 38 ± 24 |
| JWH-081 | Naphtoylindole | 1.2 | 12.4 ± 2.3 |
| JWH-122 | Naphtoylindole | 0.7 ± 0.5 | 1.2 ± 1.2 |
| JWH-210 | Naphtoylindole | 0.5 | 0.7 |
| AM-2201 | Naphtoylindole | 1 | 2.6 |
| JWH-203 | Phenylacetylindole | 8 ± 1 | 7 ± 1.3 |
| JWH-250 | Phenylacetylindole | 11 ± 2 | 33 ± 2 |
| RCS-8** | Phenylacetylindole | unknown | unknown |
JWH-018 analog;
JWH-250 analog
1.5 The changing composition of Spice
One unique aspect of the Spice phenomenon is that its constituents seem to be changing over time (Ernst et al. 2012; Rosenbaum et al. 2012). This might be related to manufacturers staying one step ahead of legislation. The first generation of Spice contained CP-47,497-C8, JWH-018, and JWH-073. As first observed in the U.K., Germany, and Japan, when these compounds were banned they were replaced by structurally similar and pharmacologically active compounds that avoided regulations (Dargan et al. 2011; Kikura-Hanajiri et al. 2011; Lindigkeit et al. 2009). In March 2011, the U.S. Drug Enforcement Agency (DEA) placed JWH-018, JWH-073, JWH-200, CP-47,497, and (C8)-CP47,497—all compounds present in Spice—on the Schedule 1 list under 21 U.S.C. 811(h) of the Controlled Substances Act (1308 2011). In response, the banned compounds were replaced by structurally related ones not included within the ban (Jouvenal 2011).
2. Effects of Spice
There are no randomized controlled trials for Spice. Furthermore, few of the synthetic cannabinoids have been tested on humans (Auwarter et al. 2009). Most of the information on Spice is anecdotal—from internet forums, calls to emergency responders and Poison Control Centers, and case reports in the medical literature. To what extent the available literature accurately represents the phenomenon of Spice is unclear. The medical literature relies heavily on case reports from the Emergency Department, which tend to highlight the extreme and catastrophic reactions to Spice use.
Given the dearth of data, the Erowid self-reports may be a meaningful contribution to the medical literature on Spice, just as they have made meaningful contributions to the literature of other emerging substances of abuse (Addy 2007; Wood et al. 2010). The Erowid self-reports shed light on the effects users who do not come to medical attention experience and may help elucidate reasons for why people use Spice. Moreover, these self-reports enhance our knowledge of the similarities and differences between synthetic and phytocannabinoids. We acknowledge that there are methodological issues with the Erowid data. These reports are purely subjective and lack objective data. Also, there is no laboratory confirmation for any of the compounds discussed within these reports. However, the Erowid self-reports demonstrate how these products are bought, consumed, and experienced in real-life situations instead of within controlled laboratory settings. In the absence of any other credible sources of information, this literature provides an important insight for those studying the Spice phenomenon.
2.1 Onset and Duration of Effects
The emergence of symptoms is often unclear in patients presenting to medical attention hours after Spice consumption (Bebarta et al. 2012; Sobolevsky et al. 2010). However, symptoms can start immediately, minutes, or hours after use; duration of symptoms are variable but can last hours (Auwarter et al. 2009; Barratt et al. 2013; Benji 2010; Canning et al. 2010; coffeeman64 2008; Deluca et al. 2009; Dreaded--Joe 2010; Ellsworth and Stellpflug March, 2011; Hoyte et al. 2012; Jack 2009; Kratoman 2009; Lapoint et al. 2011; mixmaster 2009; Muller et al. 2010a; Riddirk 2008; Schneir and Baumbacher 2012; Schneir et al. 2011; Shruming--Human 2009; Simmons et al. 2011b; Various 2009; WelshSmoker 2009; Winstock and Barratt 2013; Young et al. 2012). Some users may experience residual effects that can last for several hours (Auwarter et al. 2009; Shakes 2008). Agitated delirium lasting for several days has been reported (Berry-Caban et al. 2013).
2.2 Acute Effects of Spice
While many of the acute effects of Spice are similar to those of cannabis, there are important differences in both the spectrum and intensity of effects. It is unknown whether these are related to the differences between synthetic and phytocannabinoids or to the non-cannabinoid components present in Spice. The effects of Spice include changes in mood, anxiety, perception, thinking, memory and attention, neurological function, cardiovascular function, and gastrointestinal function (see table 3).
Table 3.
Effects associated with Spice intoxication
2.2.1 Acute Psychoactive Effects
Typical acute psychoactive effects of Spice include euphoria, a feeling of well-being, calmness, relaxation, increased creativity, mild perceptual alterations, and mild memory and attentional impairments. Perceptual changes include peripheral numbness, tingling, migratory flushing or cooling, and altered depth perception (Benji 2010; Kratoman 2009; mixmaster 2009; Modern--Famicom. 2009; Nostalgia 2010; Riddirk 2008; Shakes 2008). However, similar to cannabis, effects at either end of the spectrum may occur including anxiolysis or anxiety, stimulation or sedation, and euphoria or dysphoria. Panic attacks following Spice use have been reported, as have suicidal ideation and attempts (Gay 2010; Hurst et al. 2011; Shanks et al. 2012; Van der Veer and Fiday 2011).
2.2.2 Psychotic Reactions
Psychosis related to Spice use has received particular attention both in the media and medical literature. Psychotic symptoms associated with Spice include perceptual alterations, illusions, auditory and visual hallucinations, paranoia, agitation, aggression, catatonia, depersonalization, and dissociation. Of note, users have reported vivid visual changes described as “fractals,” “trails,” “flashes of colour [sic],” and “geometric patterns—” hallucinations different from what are typically reported in endogenous psychosis (Dan 2009; Skipper09 2009; Various 2009).
The prevalence of psychotic reactions is not clear and surveys of Spice users have yielded inconsistent results (Barratt et al. 2013; Vandrey et al.). It is likely that most psychotic symptoms are transient and resolve spontaneously without medical intervention. However, psychotic reactions are also a common reason why Spice users seek medical attention or are brought in for emergency care (Forrester et al. 2011).
While psychotic symptoms typically last no more than hours, there have been a number of cases of prolonged psychotic symptoms. In one case report, a 36-year-old man exhibited a two-week history of odd behavior and irritability within the context of daily Spice use for four weeks. These symptoms resolved once he stopped his Spice habit and did not return with continued abstinence from Spice use (Tung et al. 2012). In a few cases persistent psychosis lasted for weeks or months, and in certain instances symptoms did not completely remit (Berry-Caban et al. 2013; Hurst et al. 2011; Van der Veer and Fiday 2011). Whether these instances of prolonged psychosis can be explained by some underlying predisposition to psychosis is unclear. However, there are reports in the medical literature of Spice precipitating psychosis in both users with and without a history of a psychotic disorder (Every-Palmer 2010; Hurst et al. 2011).
2.2.3 Acute neurological effects
A number of neurological effects of Spice have been reported including tremor, ataxia, nystagmus, fasciculations, hypertonicity, hyperflexion, and hyperextension (Benji 2010; Canning et al. 2010; Cohen et al. 2012; Donnelly 2010; Forrester et al. 2011; Nostalgia 2010; Scalzo 2010; Schneir et al. 2011). There are several instances of Spice use inducing seizures (European Monitoring Centre for Drugs and Drug Addiction 2009; Lapoint et al. 2011; Schneir and Baumbacher 2012; Simmons et al. 2011b; Steve 2011; Tofighi and Lee 2012). The most common cognitive effects of Spice are impairments in attention, concentration, memory, and operating machinery (Musshoff et al. 2013). These effects usually span the period of intoxication but have been known to last longer (Various 2009).
One notable case of altered consciousness involved a man who collapsed after smoking Spice, became nonverbal, and exhibited repetitive back-and-forth movements in his lower extremities. In the Emergency Department, he was hypertensive, bradycardic, hypoventilating, and unresponsive with a Glasgow Coma Scale of 7. He was intubated, sedated, and medicated for agitation. By the next day he recovered and was later discharged (Simmons, Skinner, et al., 2011).
2.2.4 Acute cardiovascular effects
The most common cardiovascular side effects are tachycardia and hypertension (Hoyte et al. 2012). Individuals can present with palpitations, chest pain, or arrhythmias (Bebarta et al. 2012; Cohen et al. 2012; Ellsworth and Stellpflug March, 2011; Gifford et al. 1999; Hermanns-Clausen et al. 2013; Lapoint et al. 2011; Schneir et al. 2011; Simmons et al. 2011a; Teske et al. 2010; The--Pilgrim 2013; WelshSmoker 2009; Young et al. 2012). Panic symptoms frequently accompany palpitations, and it can be difficult to differentiate to what extent these symptoms are due to anxiety (Various 2009). Even after the period of intense palpitations—which can last hours—has passed, residual irregularities may persist (Shruming--Human 2009). There is suspicion that Spice, in rare cases, may induce myocardial infarction and even death (Mir et al. 2011; St. James 2010; WYFF4.COM 2011).
2.2.5 Acute Gastrointestinal Effects
Spice can induce nausea and emesis as well as stimulate appetite (Canning et al. 2010; Hermanns-Clausen et al. 2013; Modern--Famicom 2009; Simmons et al. 2011b). However, users report Spice having less appetite-stimulating properties than cannabis (Winstock and Barratt 2013).
2.2.6 Other effects
Spice can also induce dry or “cotton” mouth, reddened conjunctiva, pupillary changes including miosis and mydriasis, blurry vision and light sensitivity, cough, and pulmonary inflammation and injury (Alhadi et al. 2013; Auwarter et al. 2009; Canning et al. 2010; coffeeman64 2008; Door--King 2009; Dr--Toata--Phikal 2013; Forrester et al. 2011; Jack 2009; Kratoman 2009; Loschner et al. 2011; mixmaster 2009; Modern--Famicom. 2009; Nostalgia 2010; Potty 2009; rev.MRC 2009; Riddirk 2008; Schneir et al. 2011; Shakes 2008; Shruming--Human 2009; Simmons et al. 2011a; Simmons et al. 2011b; Skipper09 2009; Sobolevsky et al. 2010; Teske et al. 2010). Other reported symptoms include hyperthermia, rhabdomyolysis, symptoms suggestive of anticholinergic effects, and tinnitus (Banerji et al. 2010; Forrester et al. 2011; Hermanns-Clausen et al. 2013; Vandrey et al. 2012). There are several documented cases of Spice users developing acute renal damage. While the precise cause of renal damage in these patients is unclear, one specific synthetic cannabinoid may be implicated (Bhanushali et al. 2013; CDC 2013).
2.2.7 Delayed Consequences (Hangover)
Hangover reactions the day after using Spice are described in the Erowid self-reports (Shootah 2008; Shruming--Human 2009). One writer described the feeling as similar to what follows a night of heavy drinking: headache, dizziness, nausea, and feeling “the room was spinning” (Dan 2009).
2.2.8 Tolerance, Dependence, and Withdrawal
There are examples of tolerance and withdrawal reactions from long-term Spice use in the medical literature and self-reports (JSB20102011; Riley 2012; S. Carter 2010; SpacedOUTonSPICE 2009; St. James 2010; Wells and Ott 2011). Spice use consistent with criteria for substance dependence has also been documented (Dr--Toata--Phikal 2013; The--Pilgrim 2013). The two case reports of withdrawal reactions in the medical literature document symptoms of diaphoresis, internal restlessness, tremor, somatic pain, palpitations, insomnia, tachycardia, hypertension, hyperventilation, headache, diarrhea, nausea, vomiting, and depressed mood. Most severe withdrawal symptoms resolved within a week, although there were longer-lasting residual symptoms (Rominger et al. 2013; Zimmermann et al. 2009).
2.3 Laboratory Detection
There are a number of unique challenges to the laboratory detection of synthetic cannabinoids present in the urine, oral fluid, and serum samples of people who have consumed Spice. Spice contains synthetic cannabinoids from different chemical classes and has a composition that is constantly changing. Therefore, a laboratory test that is to be of clinical utility would require a single or battery of tests that could detect cannabinoids or their metabolites belonging to several chemical classes. Several synthetic cannabinoids including JWH-018 and many of their downstream metabolites can be measured in the serum through liquid chromatography tandem mass spectrometry (LC-MS/MS) and gas chromatography mass spectrometry (GC/MS) (Chimalakonda et al. 2011a; Chimalakonda et al. 2011b; Dresen et al. 2011; Hudson and Ramsey 2011; Moran et al. 2011; Sobolevsky et al. 2010; Teske et al. 2010). However, LC-MS/MS and GC/MS methods require extraction, concentration, or derivatization techniques that are time consuming. While there are no commercially available laboratory tests for the detection of synthetic cannabinoids, there are a number of laboratories that can detect synthetic cannabinoids. However, these tests cannot be performed on-site at most institutions. Thus, the results would not be immediately available and would be unlikely to inform clinical decision-making.
2.4 Changes in Laboratory Parameters
In addition to psychiatric and physical symptoms, a number of acute changes in laboratory parameters have been reported in individuals who have sought medical attention related to Spice intoxication (see table 4).
Table 4.
Laboratory changes associated with Spice use
| Laboratory Parameter | Observed Values | References |
|---|---|---|
| Hyperglycemia | 170 to 220 mg/dL | (Bebarta et al. 2012; Canning et al. 2010; Hermanns-Clausen et al. 2013; Simmons et al. 2011b) |
| Hypokalemia | 2.3 to 3.5 mmol/L | (Canning et al. 2010; Heath et al. 2012; Hermanns- Clausen et al. 2013; Simmons et al. 2011a; Simmons et al. 2011b; Vearrier and Osterhoudt 2010) |
| Elevated Creatinine | 3.2–21.0 mg/dL | (Bhanushali et al. 2013; CDC 2013) |
| Acidosis | pH of 7.24 and a pCO2 of 63 | (Simmons et al. 2011a) |
| Elevated Creatinine Phosphokinase | 867 to 2649 U/L | (Heath et al. 2012; Hermanns-Clausen et al. 2013; Lapoint et al. 2011; Simmons et al. 2011a) |
| Elevated White Blood Cell Count | 13,000 to 19,000 cells per microliter | (Alhadi et al. 2013; Bebarta et al. 2012; Simmons et al. 2011a; Simmons et al. 2011b) |
2.5 Management
The limited data suggest that supportive and symptomatic treatments such as lorazepam or antipsychotics may be efficacious (see Table 5). There are no specific antidotes for the consequences of Spice use. In theory, CB1R antagonists might reverse the effects of the synthetic CB1 agonists present in Spice, but there are no commercially available CB1R antagonists.
Table 5.
Management of Spice–related adverse events
3. Spice Users
3.1 Demographics
Spice is an international phenomenon used primarily by adolescents and young adults (Barratt et al. 2013; Donnelly 2010; European Monitoring Centre for Drugs and Drug Addiction 2009; Forrester et al. 2011; Hoyte et al. 2012; Johnston et al. 2011; Vandrey et al. 2012). In the U.S., Spice use is most prevalent in the Southeast and Midwest regions (DEA 2011; Wood 2013). Surveys of Spice use reveal a gender gap, with men more than twice as likely to use Spice than women (Barratt et al. 2013; Forrester et al. 2011; Hoyte et al. 2012; Hu et al. 2011; Vandrey et al. 2012).
3.2 Reasons for Use
People use Spice because it cannot be detected with standard urine drug testing, it is perceived as safe and legal, is affordable, and promises a “high” similar to or stronger than cannabis (Barratt et al. 2013). That standard drug-screening assays are incapable of detecting Spice makes the drug popular among military personnel and those who are subjected to routine drug testing (Berry-Caban et al. 2012; Dresen et al. 2011; Every-Palmer 2011; Johnson et al. 2011). Habitual cannabis users may switch to Spice if they have to be regularly monitored for drugs (Hippieman420 2009; Sopris 2008). The internet and Spice’s legal status make this substance more available to teenagers (Ginsburg et al. 2012). Shiny packaging, adept marketing, and their innocuous scent allow users to avoid detection (Schifiano et al. 2009). Because it had been perceived as legal until recently and is touted as “synthetic marijuana,” some assume Spice is a safe alternative to cannabis (Every-Palmer 2011; Vandrey et al. 2012).
Most Spice users abuse other substances, with cannabis being the most frequently used (Barratt et al. 2013; Winstock and Barratt 2013). Other commonly used substances include tobacco, hallucinogens, prescription opiates, MDMA, benzodiazepines, amphetamines, cocaine, and Salvia divinorum (Castellanos et al. 2011; Hu et al. 2011; Vandrey et al. 2012; Winstock and Barratt 2013). Alcohol, cannabis, tobacco, and ketamine have reportedly been used in conjunction with Spice (Schifano et al. 2010; Vandrey et al. 2012).
3.3 Comparison to Cannabis
Given that both Spice and cannabis contain cannabinoids, and Spice is marketed as “synthetic marijuana,” the extent to which their effects overlap is an important question. However, to our knowledge there are no direct comparisons between Spice and cannabis or Spice and THC. The principal active component of cannabis, THC, is a low-efficacy partial agonist, while the cannabinoids present in Spice are potent, full- and high-efficacy agonists of cannabinoid receptors (Atwood et al. 2010; Atwood et al. 2011; Huffman and Padgett 2005; Huffman et al. 2005b; Lindigkeit et al. 2009; Marriott and Huffman 2008). Thus, one would expect Spice to produce more intense effects than cannabis.
Spice is often used as a substitute for cannabis. Internet forums associate Spice with the cannabis-like properties of feeling energized, euphoric, sedated, and uplifted (Deluca et al. 2009; Every-Palmer 2011). However, as the Erowid data demonstrate, there are conflicting reports as to the similarities and differences between the two with respect to their onset and duration of action, intensity and potency of effects, and anxiogenic properties (CitrusBlank1928 2009; coffeeman64 2008; Commando420 2009; Ellsworth and Stellpflug March, 2011; Flashback 2007; Gunderson et al. 2012; marianne 2008; mixmaster 2009; rev.MRC 2009; Riddirk 2008; Shootah 2008; Sobolevsky et al. 2010; Sopris 2008; Tung et al. 2012; Various 2009). However, Spice users overwhelmingly favor the effects of cannabis to Spice (Winstock and Barratt 2013).
Since Spice products hit the market, there seem to be more reports of catastrophic reactions associated with Spice use relative to cannabis use. This may explain the impetus to outlaw Spice in contrast to the growing momentum for legalizing cannabis. We speculate that the conflicting reports of similarity and dissimilarity between Spice and cannabis may be due to the aforementioned full-agonist nature of synthetic cannabinoids, while the presence of other cannabinoids, terpenoids, and flavonoids in herbal cannabis may modulate the effects of THC.
Unlike Spice, cannabis contains around 70 other cannabinoids and flavonoids, which may influence the net effect of THC. For example, cannabidiol (CBD), a cannabinoid shown to have anxiolytic and antipsychotic properties, could offset some of the anxiogenic and psychotomimetic effects of THC (Elsohly and Slade 2005; Leweke et al. 2012; Leweke et al. 2000; Zuardi et al. 1995; Zuardi et al. 1991; Zuardi et al. 1982). Leweke et al. showed CBD monotherapy to be as effective in the treatment of acute schizophrenia as a commercially available antipsychotic drug. Moreover, a recent laboratory study demonstrated that CBD attenuated the psychotomimetic, anxiolytic, and amnestic effects of THC in humans (Englund et al. 2013). Besides CBD, cannabivarin, another cannabinoid found in cannabis, may be a weak cannabinoid receptor antagonist (Pertwee 2008).
Not much is known about whether the excipients present in Spice have any pharmacological effects, but it is conceivable that these contribute to the differences of effects between Spice and cannabis. Recent evidence suggests that the metabolites of some of the commonly present synthetic cannabinoids in Spice may have antagonist effects at CB1 receptors, which may account for some of the differences between cannabis and Spice (Brents et al. 2012; Brents et al. 2011; Chimalakonda et al. 2012).
Finally, in discussing the similarities and differences between Spice and cannabis, it is important to note that the marketing and labeling of Spice as “synthetic marijuana” or a “marijuana substitute” is both inaccurate and potentially harmful. Such descriptions give the false impression that Spice is similar to cannabis in its constituents and effects, and that it is safer than the available data suggest.
4. Legislation
Prompted by the alarming growth of the Spice phenomenon, European nations passed laws in 2009 to control these substances (European Monitoring Centre for Drugs and Drug Addiction 2009). Other nations including the U.S. followed suit. (Dargan et al. 2011; Kikura-Hanajiri et al. 2011; Zimmermann et al. 2009). To date, 19 nations aside from the U.S. have bans on Spice products (Erowid 2013). However, as these laws went into effect, new synthetic cannabinoids not on the list of banned compounds appeared on the market (Kikura-Hanajiri et al. 2011; Kneisel et al. 2012; Lindigkeit et al. 2009). Moreover, some banned synthetic cannabinoids were still components of Spice, albeit on a lesser scale than before the laws were enacted (Dargan et al. 2011; Dresen et al. 2010).
The U.S. provides a good example of the legislative challenges surrounding Spice. Once aware of the Spice problem, states and the military passed laws prohibiting the manufacture and marketing of Spice (Erowid 2013; Forrester et al. 2011; Leonhart 2012; Seely et al. 2011). Unfortunately, these laws have had limited success curtailing consumption, and Spice use continues in areas where legislation against Spice has been passed (Boyle December 31, 2011; Vandrey et al. 2012). Meanwhile, as states passed laws against Spice, the ratio of reported synthetic cannabinoid exposures changed. In 2009, 86.67 percent of exposures were due to JWH-018 products, whereas in 2010 this had decreased to 63.39 percent. By 2010, other novel synthetic cannabinoid compounds began appearing on the market (DEA 2011).
On July 9, 2012, President Obama signed the Synthetic Drug Abuse Prevention Act of 2012 that adds 15 synthetic cannabinoids belonging to five distinct structural classes to Schedule I of the Controlled Substances Act. On July 26, 2012, the U.S. DEA conducted “Operation Log Jam,” seizing 18.4 million packets of synthetic cannabinoids, $36 million in cash, and arresting more than 90 people from 109 U.S. cities (DEA 2012). Although results from chemical analyses have not been disclosed, the DEA has mentioned that “many of the designer drugs… seized as part of Operation Log Jam are not specifically prohibited by the Controlled Substances Act,” but may be prosecuted under the Analogues Act if the chemicals are structurally or functionally similar to prohibited chemicals. The impact of this legislation is too early to predict, but new reports suggest that there are significant challenges to regulating these compounds. Whether manufacturers will produce new compounds that do not fall under the legislation or whether these drugs will be sold similarly to other illegal substances remains to be seen. Clearly, despite making it illegal to possess other street drugs such as cocaine and heroin, the use of these drugs is widespread.
5. Implications
The Spice phenomenon represents a new trend in substance abuse. Thus far, manufacturers and retailers have been successful in their attempts to circumvent law enforcement. The ever-changing nature of these substances means regulatory agencies are locked into a cat-and-mouse interplay with Spice manufacturers and consumers.
One important implication of the Spice phenomenon is how it informs the cannabinoid hypothesis of psychosis. There is growing evidence for a cannabinoid hypothesis of psychosis: that exposure to cannabis and cannabinoid agonists is associated with psychosis outcomes through activation of CB1R (Radhakrishnan et al. 2012; Sewell et al. 2010). The association may be classified according to duration, clinical significance of psychosis, and how soon after exposure psychosis occurs. Psychotic reactions can be grouped into immediate-onset, short-lived psychotic symptoms; immediate-onset, persistent psychotic states; and a late-occurring, persistent psychotic disorder.
The most compelling evidence for the cannabinoid hypothesis comes from studies of cannabis, but these have several limitations above and beyond the challenges in quantifying exposure to cannabis. THC, the principal active ingredient of cannabis, is suspected to be the main culprit of psychosis outcomes due to cannabis exposure. However, as discussed previously, other constituents of cannabis, notably cannabidiol (CBD), may in fact offset some of the effects of THC (Bhattacharyya et al. 2009; Bhattacharyya et al. 2010; Borgwardt et al. 2008; Fusar-Poli et al. 2010; Fusar-Poli et al. 2009; Morgan et al. 2010). Furthermore, there is considerable variability in the THC and CBD content of cannabis. Some forms of cannabis, such as sinsemilla or “skunk” cannabis, contain very high THC and low CBD content and are more associated with psychosis outcomes (Morgan and Curran 2008). These shortcomings make it difficult to accurately assess the full magnitude of the link between cannabis and psychosis outcomes.
Whereas THC is a weak partial agonist of the CB1R, the cannabinoids present in Spice are highly potent full agonists of CB1R (Table 1). This could explain why, despite how relatively recent the Spice phenomenon is, there are disproportionate numbers of cases in the media and medical literature of psychosis following Spice use. Moreover, Spice lacks cannabinoids such as CBD that are known to attenuate psychosis outcomes and may offset Spice’s psychosis-inducing effects. Thus, the cannabinoids in Spice may complement the existing evidence supporting a link between cannabinoids and psychosis.
Exposure to cannabis in adolescence is thought to contribute to an increased risk of psychosis later in life (Radhakrishnan et al. 2012; Sewell et al. 2010). Additionally, there appears to be a linear dose-response relationship, with greater exposure increasing the risk for psychosis. Given the higher potency of synthetic cannabinoids relative to THC, there is concern that the growing use of Spice may lead to new cases of psychosis and may precipitate psychosis in individuals with a psychotic disorder. Therefore, monitoring the impact of Spice on the rates of psychosis will be an important public health initiative.
6. Limitations and Future Directions
Much of the information about the effects of Spice is derived from case reports, which may reflect extreme examples, and self-reports, which may have limited reliability. The available literature is sparse, retrospective, and burdened with a number of limitations: selection bias, a reliance on the accuracy of the written record or subject recall, the uncontrolled nature of the evidence, the inadequate characterization of cases, the lack of standardized assessments, the confounding effects of other drugs used concomitantly with Spice, and the variable doses and routes of administration. Until controlled laboratory data becomes available, the Erowid data remain a crucial source of information on subjective drug effects, and are increasingly valued by researchers and regulatory agencies (Addy 2007; Coyle et al. 2012; European Monitoring Centre for Drugs and Drug Addiction 2002; 2005; 2006; Teltzrow and Bosch 2012). Most of the reports and studies of Spice exposure lack confirmation through laboratory analysis, and other substances concomitantly used with Spice may have their own risks. As noted by the National Institute of Drug Abuse (NIDA) in their 2011 description of Spice that has since been updated, “the compounds found in Spice have not been fully characterized for their effects and importantly, their toxicity, in humans.”
Adolescents and young adults continue to expose themselves to the known and unknown risks of Spice use. As a result, there is a need for controlled data on the acute pharmacology and toxicology of Spice in animals and humans. Achieving this goal will first involve extensive toxicology testing in animals, followed by slow, dose-escalation first-in-human studies. Such research will aid clinicians and emergency responders in recognizing Spice intoxication easier, and will facilitate the development of evidence-based treatments for Spice-induced side effects. There is also a need to characterize the behavioral, subjective, cognitive, and physiological effects of Spice; determine the constituents of Spice sold; and establish the relationship between drug effects and the blood and urine levels of parent cannabinoids and their metabolites. However, Spice manufacturers have no financial incentive to sponsor such research on products they market as “not for human consumption,” nor will Spice’s young-adult consumers urge Spice manufacturers to conduct this research. The only alternative is for government to sponsor toxicology testing of these drugs.
Urine drug tests for the synthetic cannabinoids present in Spice need to become more widely available. To bring awareness to clinicians, there should be a long-term surveillance program to monitor in real-time the available Spice products and their constituents. Epidemiological studies should be conducted to track the long-term impact of legislation. Finally, acute pharmacological and epidemiological research is needed to explore the acute and long-term effects of Spice use relative to cannabis use. Studying the consequences of Spice may shed further light on the association between cannabinoids and psychosis, since the synthetic cannabinoids present in Spice are much more potent than THC present in cannabis. Finally, characterizing the effects of these high-potency synthetic cannabinoids may also better characterize tolerance to cannabinoids and a cannabinoid-withdrawal syndrome.
Table 2.
Erowid Reports on Spice Effects
| Symptom | Number of Entries |
|---|---|
| Sensation Changes | 54 |
| Positive Mood Effects | 53 |
| Negative Mood Effects | 50 |
| Cognitive Effects | 43 |
| Palpitations | 33 |
| Thought Disorganization | 30 |
| Anxiety Reactions | 30 |
| Hallucinations/Illusions | 29 |
| Paranoia | 26 |
| Nausea/Emesis | 23 |
| Depersonalization/Disassociation | 21 |
| Xerostomia | 20 |
| Hangover Effects | 19 |
| Appetite Stimulation | 17 |
| Amnesic Effects | 13 |
| Ocular Changes | 12 |
| Throat and Respiratory Effects | 11 |
| Seizures | 2 |
| Losing Consciousness | 1 |
| Total Accounts | 110 |
Acknowledgments
Deepak Cyril D’Souza has in the past three years or currently receives research grant support administered through Yale University School of Medicine from Astra Zeneca, Abbott Laboratories, Eli Lilly Inc., Forest Laboratories, Organon, Pfizer Inc., and Sanofi; he is a consultant for Bristol Meyers Squibb and Johnson and Johnson.
References
- 1308 CP. Schedules of Controlled Substances. 2011;76:11075–11078. [Google Scholar]
- AAPCC. Synthetic Marijuana Data. 2011 http://www.aapcc.org/alerts/synthetic-marijuana/
- Addy P. Facilitating transpersonal experiences with dextromethorphan: Potential, cautions, and caveats. Journal of Transpersonal Psychology. 2007;39:1–22. [Google Scholar]
- Alhadi S, Tiwari A, Vohra R, Gerona R, Acharya J, Bilello K. High times, low sats: diffuse pulmonary infiltrates associated with chronic synthetic cannabinoid use. Journal of medical toxicology: official journal of the American College of Medical Toxicology. 2013;9:199–206. doi: 10.1007/s13181-013-0288-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashton JC. Synthetic cannabinoids as drugs of abuse. Current drug abuse reviews. 2012;5:158–68. doi: 10.2174/1874473711205020158. [DOI] [PubMed] [Google Scholar]
- Atwood BK, Huffman J, Straiker A, Mackie K. JWH018, a common constituent of ‘Spice’ herbal blends, is a potent and efficacious cannabinoid CB receptor agonist. British journal of pharmacology. 2010;160:585–93. doi: 10.1111/j.1476-5381.2009.00582.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atwood BK, Lee D, Straiker A, Widlanski TS, Mackie K. CP47,497-C8 and JWH073, commonly found in ‘Spice’ herbal blends, are potent and efficacious CB(1) cannabinoid receptor agonists. Eur J Pharmacol. 2011;659:139–45. doi: 10.1016/j.ejphar.2011.01.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aung MM, Griffin G, Huffman JW, Wu M, Keel C, Yang B, Showalter VM, Abood ME, Martin BR. Influence of the N-1 alkyl chain length of cannabimimetic indoles upon CB(1) and CB(2) receptor binding. Drug Alcohol Depend. 2000;60:133–40. doi: 10.1016/s0376-8716(99)00152-0. [DOI] [PubMed] [Google Scholar]
- Auwarter V, Dresen S, Weinmann W, Muller M, Putz M, Ferreiros N. ‘Spice’ and other herbal blends: harmless incense or cannabinoid designer drugs? J Mass Spectrom. 2009;44:832–7. doi: 10.1002/jms.1558. [DOI] [PubMed] [Google Scholar]
- Banerji S, Deutsch CM, Bronstein AC. SPICE Ain’t So Nice. 2010 http://rmpdc.org/Portals/23/Spice%20Poster%20Final%202010.pdf.
- Barratt MJ, Cakic V, Lenton S. Patterns of synthetic cannabinoid use in Australia. Drug and alcohol review. 2013;32:141–6. doi: 10.1111/j.1465-3362.2012.00519.x. [DOI] [PubMed] [Google Scholar]
- Bebarta VS, Ramirez S, Varney SM. Spice: A New “Legal” Herbal Mixture Abused by Young Active Duty Military Personnel. Substance Abuse. 2012;33:191–194. doi: 10.1080/08897077.2011.637610. [DOI] [PubMed] [Google Scholar]
- Benford DM, Caplan JP. Psychiatric sequelae of Spice, K2, and synthetic cannabinoid receptor agonists. Psychosomatics. 2011;52:295. doi: 10.1016/j.psym.2011.01.004. [DOI] [PubMed] [Google Scholar]
- Benji. More Than Meets the Eye. 2010 http://www.erowid.org/experiences/exp.php?ID=84194.
- Berry-Caban CS, Ee J, Ingram V, Berry CE, Kim EH. Synthetic Cannabinoid Overdose in a 20-Year-Old Male US Soldier. Substance abuse: official publication of the Association for Medical Education and Research in Substance Abuse. 2013;34:70–2. doi: 10.1080/08897077.2012.677754. [DOI] [PubMed] [Google Scholar]
- Berry-Caban CS, Kleinschmidt PE, Rao DS, Jenkins J. Synthetic cannabinoid and cathinone use among US soldiers. US Army Medical Department journal. 2012:19–24. [PubMed] [Google Scholar]
- Bhanushali GK, Jain G, Fatima H, Leisch LJ, Thornley-Brown D. AKI associated with synthetic cannabinoids: a case series. Clinical journal of the American Society of Nephrology: CJASN. 2013;8:523–6. doi: 10.2215/CJN.05690612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhattacharyya S, Fusar-Poli P, Borgwardt S, Martin-Santos R, Nosarti C, O’Carroll C, Allen P, Seal ML, Fletcher PC, Crippa JA, Giampietro V, Mechelli A, Atakan Z, McGuire P. Modulation of mediotemporal and ventrostriatal function in humans by Delta9-tetrahydrocannabinol: a neural basis for the effects of Cannabis sativa on learning and psychosis. Arch Gen Psychiatry. 2009;66:442–51. doi: 10.1001/archgenpsychiatry.2009.17. [DOI] [PubMed] [Google Scholar]
- Bhattacharyya S, Morrison PD, Fusar-Poli P, Martin-Santos R, Borgwardt S, Winton-Brown T, Nosarti C, CMOC, Seal M, Allen P, Mehta MA, Stone JM, Tunstall N, Giampietro V, Kapur S, Murray RM, Zuardi AW, Crippa JA, Atakan Z, McGuire PK. Opposite effects of delta-9-tetrahydrocannabinol and cannabidiol on human brain function and psychopathology. Neuropsychopharmacology. 2010;35:764–74. doi: 10.1038/npp.2009.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhatty S, Wu W. Organic and synthetic cannabinoid use in adolescents. Pediatric annals. 2013;42:31–5. doi: 10.3928/00904481-20121221-16. [DOI] [PubMed] [Google Scholar]
- Borgwardt SJ, Allen P, Bhattacharyya S, Fusar-Poli P, Crippa JA, Seal ML, Fraccaro V, Atakan Z, Martin-Santos R, O’Carroll C, Rubia K, McGuire PK. Neural basis of Delta-9-tetrahydrocannabinol and cannabidiol: effects during response inhibition. Biol Psychiatry. 2008;64:966–73. doi: 10.1016/j.biopsych.2008.05.011. [DOI] [PubMed] [Google Scholar]
- Boyle J. ‘Spice’ manufacturers change formula, sell drug again. 2011 Dec 31; http://www.middletownjournal.com/news/middletown-news/spice-manufacturers-change-formula-sell-drug-again-1306082.html Middletown Journal.
- Brents LK, Gallus-Zawada A, Radominska-Pandya A, Vasiljevik T, Prisinzano TE, Fantegrossi WE, Moran JH, Prather PL. Monohydroxylated metabolites of the K2 synthetic cannabinoid JWH-073 retain intermediate to high cannabinoid 1 receptor (CB1R) affinity and exhibit neutral antagonist to partial agonist activity. Biochem Pharmacol. 2012;83:952–61. doi: 10.1016/j.bcp.2012.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brents LK, Reichard EE, Zimmerman SM, Moran JH, Fantegrossi WE, Prather PL. Phase I hydroxylated metabolites of the K2 synthetic cannabinoid JWH-018 retain in vitro and in vivo cannabinoid 1 receptor affinity and activity. PloS one. 2011;6:e21917. doi: 10.1371/journal.pone.0021917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown K. New Zealand bans synthetic cannabinoids. BMJ. 2011;343:d5395. doi: 10.1136/bmj.d5395. [DOI] [PubMed] [Google Scholar]
- Bryner J. Fake Weed, Real Drug: K2 Causing Hallucinations in Teens. 2010 http://www.livescience.com/6149-fake-weed-real-drug-k2-causing-hallucinations-teens.html. Live Science Volume.
- Canning JC, Ruha AM, Pierce R, Torrey M, Reinhart SJ. Severe GI Distress After Smoking JWH018. Clin Toxicol. 2010;48:618. [Google Scholar]
- Castellanos D, Singh S, Thornton G, Avila M, Moreno A. Synthetic cannabinoid use: a case series of adolescents. The Journal of adolescent health: official publication of the Society for Adolescent Medicine. 2011;49:347–9. doi: 10.1016/j.jadohealth.2011.08.002. [DOI] [PubMed] [Google Scholar]
- Castellanos D, Thornton G. Synthetic cannabinoid use: recognition and management. Journal of psychiatric practice. 2012;18:86–93. doi: 10.1097/01.pra.0000413274.09305.9c. [DOI] [PubMed] [Google Scholar]
- CDC . Acute kidney injury asociated with synthetic cannabinoid use — multiple states, 2012. Morbidity and Mortality Weekly Report. 2013;62:93–98. [PMC free article] [PubMed] [Google Scholar]
- Chainsaw. Like Cold Lemonade. 2009 http://www.erowid.org/experiences/exp.php?ID=79040.
- Chimalakonda KC, Bratton SM, Le VH, Yiew KH, Dineva A, Moran CL, James LP, Moran JH, Radominska-Pandya A. Conjugation of synthetic cannabinoids JWH-018 and JWH-073, metabolites by human UDP-glucuronosyltransferases. Drug metabolism and disposition: the biological fate of chemicals. 2011a;39:1967–76. doi: 10.1124/dmd.111.040709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chimalakonda KC, Moran CL, Kennedy PD, Endres GW, Uzieblo A, Dobrowolski PJ, Fifer EK, Lapoint J, Nelson LS, Hoffman RS, James LP, Radominska-Pandya A, Moran JH. Solid-phase extraction and quantitative measurement of omega and omega-1 metabolites of JWH-018 and JWH-073 in human urine. Anal Chem. 2011b;83:6381–8. doi: 10.1021/ac201377m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chimalakonda KC, Seely KA, Bratton SM, Brents LK, Moran CL, Endres GW, James LP, Hollenberg PF, Prather PL, Radominska-Pandya A, Moran JH. Cytochrome P450-mediated oxidative metabolism of abused synthetic cannabinoids found in K2/Spice: identification of novel cannabinoid receptor ligands. Drug metabolism and disposition: the biological fate of chemicals. 2012;40:2174–84. doi: 10.1124/dmd.112.047530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CitrusBlank1928. Spice it Right. 2009 http://www.erowid.org/experiences/exp.php?ID=80091.
- coffeeman64. Nearly 100 Percent Comparable. 2008 http://www.erowid.org/experiences/exp.php?ID=66428.
- Cohen J, Morrison S, Greenberg J, Saidinejad M. Clinical presentation of intoxication due to synthetic cannabinoids. Pediatrics. 2012;129:e1064–7. doi: 10.1542/peds.2011-1797. [DOI] [PubMed] [Google Scholar]
- Commando420. Simply Amazing. 2009 http://www.erowid.org/experiences/exp.php?ID=78604.
- Coyle JR, Presti DE, Baggott MJ. Quantitative Analysis of Narrative Reports of Psychedelic Drugs. 2012. arXiv preprint arXiv:12060312. [Google Scholar]
- D’Ambra TE, Estep KG, Bell MR, Eissenstat MA, Josef KA, Ward SJ, Haycock DA, Baizman ER, Casiano FM, Beglin NC, et al. Conformationally restrained analogues of pravadoline: nanomolar potent, enantioselective, (aminoalkyl)indole agonists of the cannabinoid receptor. J Med Chem. 1992;35:124–35. doi: 10.1021/jm00079a016. [DOI] [PubMed] [Google Scholar]
- Dan. Unnatural and Unpleasant. 2009 http://www.erowid.org/experiences/exp.php?ID=79039.
- Dargan PI, Hudson S, Ramsey J, Wood DM. The impact of changes in UK classification of the synthetic cannabinoid receptor agonists in ‘Spice’. The International journal on drug policy. 2011;22:274–7. doi: 10.1016/j.drugpo.2011.02.006. [DOI] [PubMed] [Google Scholar]
- DEA; Agency DE, editor. Synthetic Cannabinoids and Synthetic Cathinones Reported in NFLIS, 2009–2010. National Forensic Laboratory Information System; 2011. [Google Scholar]
- DEA. DEA NEWS: Nationwide Synthetic Drug Takedown. US DOJ DEA; 2012. http://www.justice.gov/usao/id/news/images/dearelease07262012.pdf. [Google Scholar]
- Deluca P, Schifano F, Davey Z, Corazza O, di Furia L, Farre M, Flesland L, Mannonen M, Majava A, Valentina M, Pagani S, Peltoniemi T, Scherbaum N, Siemann H, Skutle A, Torrens M, Pezzolesi C, van der Kreeft P. Group PWMR, editor. Psychonaut Web Mapping Research Group: Spice report. Institute of Psychiatry, King’s College London; London, UK: 2009. [Google Scholar]
- Devane WA, Dysarz FA, 3rd, Johnson MR, Melvin LS, Howlett AC. Determination and characterization of a cannabinoid receptor in rat brain. Molecular pharmacology. 1988;34:605–13. [PubMed] [Google Scholar]
- Donnelly MT. Services MDoHaS, editor . Health advisory: K2 synthetic marijuana use among teenagers and young adults in Missouri. 2010. [Google Scholar]
- Door--King. Not Pot. 2009 http://www.erowid.org/experiences/exp.php?ID=77867.
- Dr--Toata--Phikal. Marijuana for K2 Withdrawal. 2013 http://www.erowid.org/experiences/exp.php?ID=94940.
- Dreaded--Joe. The Most Amazing Sense In The World! 2010 http://www.erowid.org/experiences/exp.php?ID=78012.
- Dresen S, Ferreiros N, Putz M, Westphal F, Zimmermann R, Auwarter V. Monitoring of herbal mixtures potentially containing synthetic cannabinoids as psychoactive compounds. J Mass Spectrom. 2010;45:1186–94. doi: 10.1002/jms.1811. [DOI] [PubMed] [Google Scholar]
- Dresen S, Kneisel S, Weinmann W, Zimmermann R, Auwarter V. Development and validation of a liquid chromatography-tandem mass spectrometry method for the quantitation of synthetic cannabinoids of the aminoalkylindole type and methanandamide in serum and its application to forensic samples. J Mass Spectrom. 2011;46:163–71. doi: 10.1002/jms.1877. [DOI] [PubMed] [Google Scholar]
- Ellsworth H, Stellpflug S. Déjà vu, Another Designer Drug: Synthetic Cannabinoids - Toxicology Section Newsletter. 2011 Mar; http://wsol.acep.org/Content.aspx?id=77201.
- Elsohly MA, Slade D. Chemical constituents of marijuana: The complex mixture of natural cannabinoids. Life Sci. 2005;78:539–48. doi: 10.1016/j.lfs.2005.09.011. [DOI] [PubMed] [Google Scholar]
- Englund A, Morrison PD, Nottage J, Hague D, Kane F, Bonaccorso S, Stone JM, Reichenberg A, Brenneisen R, Holt D, Feilding A, Walker L, Murray RM, Kapur S. Cannabidiol inhibits THC-elicited paranoid symptoms and hippocampal-dependent memory impairment. J Psychopharmacol. 2013;27:19–27. doi: 10.1177/0269881112460109. [DOI] [PubMed] [Google Scholar]
- Ernst L, Kruger K, Lindigkeit R, Schiebel HM, Beuerle T. Synthetic cannabinoids in “spice-like” herbal blends: First appearance of JWH-307 and recurrence of JWH-018 on the German market. Forensic science international. 2012;222:216–22. doi: 10.1016/j.forsciint.2012.05.027. [DOI] [PubMed] [Google Scholar]
- Erowid. Spice Product Legal Status. 2013 http://www.erowid.org/chemicals/spice_product/spice_product_law.shtml.
- European Monitoring Centre for Drugs and Drug Addiction E. Report on the risk assessment of GHB in the framework of the joint action on new synthetic drugs. Office for Official Publications of the European Communities; Luxembourg: 2002. [Google Scholar]
- European Monitoring Centre for Drugs and Drug Addiction E. Europol–EMCDDA Active Monitoring Report on a new psychoactive substance: 1-(3-chlorophenyl)piperazine (mCPP) Office for Official Publications of the European Communities; Lisbon: 2005. [Google Scholar]
- European Monitoring Centre for Drugs and Drug Addiction E. Thematic paper — Hallucinogenic Mushrooms: An Emerging Trend Case Study. Office for Official Publications of the European Communities; Lisbon: 2006. [Google Scholar]
- European Monitoring Centre for Drugs and Drug Addiction E. Thematic paper — Understanding the ‘Spice’ phenomenon. Office for Official Publications of the European Communities; Luxembourg: 2009. [Google Scholar]
- Every-Palmer S. Warning: legal synthetic cannabinoid-receptor agonists such as JWH-018 may precipitate psychosis in vulnerable individuals. Addiction. 2010;105:1859–60. doi: 10.1111/j.1360-0443.2010.03119.x. [DOI] [PubMed] [Google Scholar]
- Every-Palmer S. Synthetic cannabinoid JWH-018 and psychosis: an explorative study. Drug and alcohol dependence. 2011;117:152–7. doi: 10.1016/j.drugalcdep.2011.01.012. [DOI] [PubMed] [Google Scholar]
- Fattore L, Fratta W. Beyond THC: The New Generation of Cannabinoid Designer Drugs. Front Behav Neurosci. 2011;5:60. doi: 10.3389/fnbeh.2011.00060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flashback. Basically Cannabis, Minus the Fun. 2007 http://www.erowid.org/experiences/exp.php?ID=50226.
- Forrester MB, Kleinschmidt K, Schwarz E, Young A. Synthetic cannabinoid exposures reported to Texas poison centers. J Addict Dis. 2011;30:351–8. doi: 10.1080/10550887.2011.609807. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P, Allen P, Bhattacharyya S, Crippa JA, Mechelli A, Borgwardt S, Martin-Santos R, Seal ML, O’Carrol C, Atakan Z, Zuardi AW, McGuire P. Modulation of effective connectivity during emotional processing by Delta 9-tetrahydrocannabinol and cannabidiol. Int J Neuropsychopharmacol. 2010;13:421–32. doi: 10.1017/S1461145709990617. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P, Crippa JA, Bhattacharyya S, Borgwardt SJ, Allen P, Martin-Santos R, Seal M, Surguladze SA, O’Carrol C, Atakan Z, Zuardi AW, McGuire PK. Distinct effects of {delta}9-tetrahydrocannabinol and cannabidiol on neural activation during emotional processing. Arch Gen Psychiatry. 2009;66:95–105. doi: 10.1001/archgenpsychiatry.2008.519. [DOI] [PubMed] [Google Scholar]
- Gay M. Synthetic Marijuana Spurs State Ban. The New York Times. 2010 http://wwwnytimescom/2010/07/11/us/11k2html?_r=0.
- Gifford AN, Bruneus M, Lin S, Goutopoulos A, Makriyannis A, Volkow ND, Gatley SJ. Potentiation of the action of anandamide on hippocampal slices by the fatty acid amide hydrolase inhibitor, palmitylsulphonyl fluoride (AM 374) Eur J Pharmacol. 1999;383:9–14. doi: 10.1016/s0014-2999(99)00609-3. [DOI] [PubMed] [Google Scholar]
- Ginsburg BC, McMahon LR, Sanchez JJ, Javors MA. Purity of synthetic cannabinoids sold online for recreational use. J Anal Toxicol. 2012;36:66–68. doi: 10.1093/jat/bkr018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gould J. Legal high becomes ‘horrible dream.’. Army Times. 2010 http://wwwarmytimescom/news/2010/10/SATURDAYarmy-spice-became-horrible-dream-roudebush-100210w/
- Gunderson EW, Haughey HM, Ait-Daoud N, Joshi AS, Hart CL. “Spice” and “K2” herbal highs: a case series and systematic review of the clinical effects and biopsychosocial implications of synthetic cannabinoid use in humans. The American journal on addictions / American Academy of Psychiatrists in Alcoholism and Addictions. 2012;21:320–6. doi: 10.1111/j.1521-0391.2012.00240.x. [DOI] [PubMed] [Google Scholar]
- Harris CR, Brown A. Synthetic cannabinoid intoxication: a case series and review. The Journal of emergency medicine. 2013;44:360–6. doi: 10.1016/j.jemermed.2012.07.061. [DOI] [PubMed] [Google Scholar]
- Heath TS, Burroughs Z, Thompson AJ, Tecklenburg FW. Acute intoxication caused by a synthetic cannabinoid in two adolescents. The journal of pediatric pharmacology and therapeutics: JPPT: the official journal of PPAG. 2012;17:177–81. doi: 10.5863/1551-6776-17.2.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hermanns-Clausen M, Kneisel S, Szabo B, Auwarter V. Acute toxicity due to the confirmed consumption of synthetic cannabinoids: clinical and laboratory findings. Addiction. 2013;108:534–44. doi: 10.1111/j.1360-0443.2012.04078.x. [DOI] [PubMed] [Google Scholar]
- Hippieman420. Just Like the Real Thing. 2009 http://www.erowid.org/experiences/exp.php?ID=76286.
- Howlett AC, Barth F, Bonner TI, Cabral G, Casellas P, Devane WA, Felder CC, Herkenham M, Mackie K, Martin BR, Mechoulam R, Pertwee RG. International Union of Pharmacology. XXVII. Classification of cannabinoid receptors. Pharmacological reviews. 2002;54:161–202. doi: 10.1124/pr.54.2.161. [DOI] [PubMed] [Google Scholar]
- Hoyte CO, Jacob J, Monte AA, Al-Jumaan M, Bronstein AC, Heard KJ. A characterization of synthetic cannabinoid exposures reported to the National Poison Data System in 2010. Ann Emerg Med. 2012;60:435–8. doi: 10.1016/j.annemergmed.2012.03.007. [DOI] [PubMed] [Google Scholar]
- Hu X, Primack BA, Barnett TE, Cook RL. College students and use of K2: an emerging drug of abuse in young persons. Substance abuse treatment, prevention, and policy. 2011;6:16. doi: 10.1186/1747-597X-6-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson S, Ramsey J. The emergence and analysis of synthetic cannabinoids. Drug testing and analysis. 2011;3:466–78. doi: 10.1002/dta.268. [DOI] [PubMed] [Google Scholar]
- Huffman JW, Padgett LW. Recent developments in the medicinal chemistry of cannabimimetic indoles, pyrroles and indenes. Curr Med Chem. 2005;12:1395–411. doi: 10.2174/0929867054020864. [DOI] [PubMed] [Google Scholar]
- Huffman JW, Szklennik PV, Almond A, Bushell K, Selley DE, He H, Cassidy MP, Wiley JL, Martin BR. 1-Pentyl-3-phenylacetylindoles, a new class of cannabimimetic indoles. Bioorg Med Chem Lett. 2005a;15:4110–3. doi: 10.1016/j.bmcl.2005.06.008. [DOI] [PubMed] [Google Scholar]
- Huffman JW, Zengin G, Wu MJ, Lu J, Hynd G, Bushell K, Thompson AL, Bushell S, Tartal C, Hurst DP, Reggio PH, Selley DE, Cassidy MP, Wiley JL, Martin BR. Structure-activity relationships for 1-alkyl-3-(1-naphthoyl)indoles at the cannabinoid CB(1) and CB(2) receptors: steric and electronic effects of naphthoyl substituents. New highly selective CB(2) receptor agonists. Bioorg Med Chem. 2005b;13:89–112. doi: 10.1016/j.bmc.2004.09.050. [DOI] [PubMed] [Google Scholar]
- Hurst D, Loeffler G, McLay R. Psychosis associated with synthetic cannabinoid agonists: a case series. Am J Psychiatry. 2011;168:1119. doi: 10.1176/appi.ajp.2011.11010176. [DOI] [PubMed] [Google Scholar]
- Jack A. The story of Spice. The Financial Times Online. 2009 http://wwwftcom/cms/s/0/1721e2da-f8a0-11dd-aae8-000077b07658html#axzz2VDpo0fdr.
- Johnson LA, Johnson RL, Alfonzo C. Spice: a legal marijuana equivalent. Mil Med. 2011;176:718–20. doi: 10.7205/milmed-d-10-00356. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JED. Marijuana use continues to rise among US teens, while alcohol use hits historic lows. University of Michigan News Service; Ann Arbor, MI: 2011. Retrieved 04/29/2012 from http://www.monitoringthefuture.org. Marijuana use continues to rise among U.S. teens, while alcohol use hits historic lows, Ann Arbor, MI. [Google Scholar]
- Jouvenal J. ‘Spice’ makers change recipes to sidestep bans. USA Today. 2011 http://usatoday30usatodaycom/USCP/PNI/NEWS/2011-12-30-PNI1230wir-Spice_ST_Uhtm.
- JSB2010. It Needed to Be Respected But I Didn’t. 2011 http://www.erowid.org/experiences/exp.php?ID=92368.
- Kikura-Hanajiri R, Uchiyama N, Goda Y. Survey of current trends in the abuse of psychotropic substances and plants in Japan. Leg Med (Tokyo) 2011;13:109–15. doi: 10.1016/j.legalmed.2011.02.003. [DOI] [PubMed] [Google Scholar]
- Kneisel S, Westphal F, Bisel P, Brecht V, Broecker S, Auwarter V. Identification and structural characterization of the synthetic cannabinoid 3-(1-adamantoyl)-1-pentylindole as an additive in ‘herbal incense’. Journal of mass spectrometry: JMS. 2012;47:195–200. doi: 10.1002/jms.2059. [DOI] [PubMed] [Google Scholar]
- Kratoman. Really High for a Really Long Time. 2009 http://www.erowid.org/experiences/exp.php?ID=79674.
- Lapoint J, James LP, Moran CL, Nelson LS, Hoffman RS, Moran JH. Severe toxicity following synthetic cannabinoid ingestion. Clin Toxicol (Phila) 2011;49:760–4. doi: 10.3109/15563650.2011.609822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonhart M. Justice Do, editor . Schedules of Controlled Substances: Placement of Five Synthetic Cannabinoids Into Schedule I. 2012. [Google Scholar]
- Leweke FM, Piomelli D, Pahlisch F, Muhl D, Gerth CW, Hoyer C, Klosterkotter J, Hellmich M, Koethe D. Cannabidiol enhances anandamide signaling and alleviates psychotic symptoms of schizophrenia. Translational psychiatry. 2012;2:e94. doi: 10.1038/tp.2012.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leweke FM, Schneider U, Radwan M, Schmidt E, Emrich HM. Different effects of nabilone and cannabidiol on binocular depth inversion in Man. Pharmacol Biochem Behav. 2000;66:175–81. doi: 10.1016/s0091-3057(00)00201-x. [DOI] [PubMed] [Google Scholar]
- Lindigkeit R, Boehme A, Eiserloh I, Luebbecke M, Wiggermann M, Ernst L, Beuerle T. Spice: a never ending story? Forensic Sci Int. 2009;191:58–63. doi: 10.1016/j.forsciint.2009.06.008. [DOI] [PubMed] [Google Scholar]
- Loeffler G, Hurst D, Penn A, Yung K. Spice, bath salts, and the U.S. military: the emergence of synthetic cannabinoid receptor agonists and cathinones in the U.S. Armed Forces. Military medicine. 2012;177:1041–8. doi: 10.7205/milmed-d-12-00180. [DOI] [PubMed] [Google Scholar]
- Loschner A, Cihla A, Falali F, Ghamande S. Diffuse alveolar hemorrhage: add “greenhouse effect” to the growing list. Chest. 2011;140:149A. [Google Scholar]
- marianne. A Pleasant Cannabis Alternative. 2008 http://www.erowid.org/experiences/exp.php?ID=67062.
- Marriott KS, Huffman JW. Recent advances in the development of selective ligands for the cannabinoid CB(2) receptor. Curr Top Med Chem. 2008;8:187–204. doi: 10.2174/156802608783498014. [DOI] [PubMed] [Google Scholar]
- McGuinness TM, Newell D. Risky recreation: synthetic cannabinoids have dangerous effects. Journal of psychosocial nursing and mental health services. 2012;50:16–8. doi: 10.3928/02793695-20120703-04. [DOI] [PubMed] [Google Scholar]
- McQuade D, Hudson S, Dargan PI, Wood DM. First European case of convulsions related to analytically confirmed use of the synthetic cannabinoid receptor agonist AM-2201. European journal of clinical pharmacology. 2013;69:373–6. doi: 10.1007/s00228-012-1379-2. [DOI] [PubMed] [Google Scholar]
- Melvin LS, Milne GM, Johnson MR, Subramaniam B, Wilken GH, Howlett AC. Structure-activity relationships for cannabinoid receptor-binding and analgesic activity: studies of bicyclic cannabinoid analogs. Molecular pharmacology. 1993;44:1008–15. [PubMed] [Google Scholar]
- Mir A, Obafemi A, Young A, Kane C. Myocardial infarction associated with use of the synthetic cannabinoid K2. Pediatrics. 2011;128:e1622–7. doi: 10.1542/peds.2010-3823. [DOI] [PubMed] [Google Scholar]
- mixmaster. Nearly Identical to MJ But Longer Lasting. 2009 http://www.erowid.org/experiences/exp.php?ID=77872.
- Modern--Famicom. The Seller of Religions, and Hell. 2009 http://www.erowid.org/experiences/exp.php?ID=80051.
- Modern--Famicom. Spicehot. 2009 http://www.erowid.org/experiences/exp.php?ID=80223.
- Montauk. Anti-Escapism. 2010 http://www.erowid.org/experiences/exp.php?ID=80755.
- Moran CL, Le VH, Chimalakonda KC, Smedley AL, Lackey FD, Owen SN, Kennedy PD, Endres GW, Ciske FL, Kramer JB, Kornilov AM, Bratton LD, Dobrowolski PJ, Wessinger WD, Fantegrossi WE, Prather PL, James LP, Radominska-Pandya A, Moran JH. Quantitative measurement of JWH-018 and JWH-073 metabolites excreted in human urine. Anal Chem. 2011;83:4228–36. doi: 10.1021/ac201377m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan CJ, Curran HV. Effects of cannabidiol on schizophrenia-like symptoms in people who use cannabis. Br J Psychiatry. 2008;192:306–7. doi: 10.1192/bjp.bp.107.046649. [DOI] [PubMed] [Google Scholar]
- Morgan CJ, Freeman TP, Schafer GL, Curran HV. Cannabidiol attenuates the appetitive effects of Delta 9-tetrahydrocannabinol in humans smoking their chosen cannabis. Neuropsychopharmacology. 2010;35:1879–85. doi: 10.1038/npp.2010.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller H, Huttner HB, Kohrmann M, Wielopolski JE, Kornhuber J, Sperling W. Panic attack after spice abuse in a patient with ADHD. Pharmacopsychiatry. 2010a;43:152–3. doi: 10.1055/s-0029-1243252. [DOI] [PubMed] [Google Scholar]
- Muller H, Sperling W, Kohrmann M, Huttner HB, Kornhuber J, Maler JM. The synthetic cannabinoid Spice as a trigger for an acute exacerbation of cannabis induced recurrent psychotic episodes. Schizophrenia research. 2010b;118:309–10. doi: 10.1016/j.schres.2009.12.001. [DOI] [PubMed] [Google Scholar]
- Musah RA, Domin MA, Walling MA, Shepard JR. Rapid identification of synthetic cannabinoids in herbal samples via direct analysis in real time mass spectrometry. Rapid communications in mass spectrometry: RCM. 2012;26:1109–14. doi: 10.1002/rcm.6205. [DOI] [PubMed] [Google Scholar]
- Musshoff F, Madea B, Kernbach-Wighton G, Bicker W, Kneisel S, Hutter M, Auwarter V. Driving under the influence of synthetic cannabinoids (“Spice”): a case series. International journal of legal medicine. 2013 doi: 10.1007/s00414-013-0864-1. [DOI] [PubMed] [Google Scholar]
- NIDA. Drug Facts: Spice (Synthetic Marijuana) 2012 http://www.drugabuse.gov/publications/drugfacts/spice-synthetic-marijuana.
- Nostalgia. Only Physically Drunk. 2010 http://www.erowid.org/experiences/exp.php?ID=84664.
- Ogata J, Uchiyama N, Kikura-Hanajiri R, Goda Y. DNA sequence analyses of blended herbal products including synthetic cannabinoids as designer drugs. Forensic science international. 2013;227:33–41. doi: 10.1016/j.forsciint.2012.09.006. [DOI] [PubMed] [Google Scholar]
- Oluwabusi OO, Lobach L, Akhtar U, Youngman B, Ambrosini PJ. Synthetic cannabinoid-induced psychosis: two adolescent cases. Journal of child and adolescent psychopharmacology. 2012;22:393–5. doi: 10.1089/cap.2012.0004. [DOI] [PubMed] [Google Scholar]
- Pant S, Deshmukh A, Dholaria B, Kaur V, Ramavaram S, Ukor M, Teran GA. Spicy seizure. The American journal of the medical sciences. 2012;344:67–8. doi: 10.1097/MAJ.0b013e31824cf5c2. [DOI] [PubMed] [Google Scholar]
- Pertwee RG. The diverse CB1 and CB2 receptor pharmacology of three plant cannabinoids: delta9-tetrahydrocannabinol, cannabidiol and delta9-tetrahydrocannabivarin. Br J Pharmacol. 2008;153:199–215. doi: 10.1038/sj.bjp.0707442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piggee C. Investigating a not-so-natural high. Analytical chemistry. 2009;81:3205–7. doi: 10.1021/ac900564u. [DOI] [PubMed] [Google Scholar]
- Potty. Very Bad for My Lungs. 2009 http://www.erowid.org/experiences/exp.php?ID=79567.
- Psychoyos D, Vinod KY. Marijuana, Spice ‘herbal high’, and early neural development: implications for rescheduling and legalization. Drug testing and analysis. 2013;5:27–45. doi: 10.1002/dta.1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radhakrishnan R, Addy PH, Sewell RA, Skosnik PD, Ranganthan M, D’Souza DC. Cannabis, Cannabinoids, and the Association with Psychosis. In: Madras B, Kuhar MJ, editors. The Effects of Drug Abuse on the Human Nervous System. Neuroscience-Net, LLC; 2012. [Google Scholar]
- Resolute. Not What I Expected. 2009 http://www.erowid.org/experiences/exp.php?ID=79497.
- rev.MRC. My Cannabinoid Receptors Are Tingling. 2009 http://www.erowid.org/experiences/exp.php?ID=76971.
- Riddirk. Differing Body States. 2008 http://www.erowid.org/experiences/exp.php?ID=67444.
- Riley. Withdrawal from Herbal Incense. 2012 http://www.erowid.org/experiences/exp.php?ID=96302.
- Rodgman C, Kinzie E, Leimbach E. Bad Mojo: use of the new marijuana substitute leads to more and more ED visits for acute psychosis. The American journal of emergency medicine. 2011;29:232. doi: 10.1016/j.ajem.2010.07.020. [DOI] [PubMed] [Google Scholar]
- Rominger A, Cumming P, Xiong G, Koller G, Forster S, Zwergal A, Karamatskos E, Bartenstein P, La Fougere C, Pogarell O. Effects of acute detoxification of the herbal blend ‘Spice Gold’ on dopamine D receptor availability: A [F]fallypride PET study. European neuropsychopharmacology: the journal of the European College of Neuropsychopharmacology. 2013 doi: 10.1016/j.euroneuro.2013.01.009. [DOI] [PubMed] [Google Scholar]
- Rose J. Fake Pot Is A Real Problem For Regulators. National Public Radio News. 2012 http://m.npr.org/news/U.S./156615024.
- Rosenbaum CD, Carreiro SP, Babu KM. Here today, gone tomorrow...and back again? A review of herbal marijuana alternatives (K2, Spice), synthetic cathinones (bath salts), kratom, Salvia divinorum, methoxetamine, and piperazines. Journal of medical toxicology: official journal of the American College of Medical Toxicology. 2012;8:15–32. doi: 10.1007/s13181-011-0202-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- S.Carter. Possible Addiction. 2010 http://www.erowid.org/experiences/exp.php?ID=91493.
- Sage2240. Similar to but Different than Cannabis. 2009 http://www.erowid.org/experiences/exp.php?ID=76383.
- Scalzo A. K2 synthetic marijuana use among teenagers—Missouri, 2010. The Epidemic Information Exchange; 2010. http://wwwiowagov/odcp/docs/Spice/K2Marijuanapdf. [Google Scholar]
- Schatz AR, Lee M, Condie RB, Pulaski JT, Kaminski NE. Cannabinoid receptors CB1 and CB2: a characterization of expression and adenylate cyclase modulation within the immune system. Toxicol Appl Pharmacol. 1997;142:278–87. doi: 10.1006/taap.1996.8034. [DOI] [PubMed] [Google Scholar]
- Schifano F, Ricciardi A, Corazza O, Deluca P, Davey Z, Rafanelli C. New drugs of abuse on the Web: the role of the Psychonaut Web Mapping Project. Rivista di psichiatria. 2010;45:88–93. [PubMed] [Google Scholar]
- Schifiano F, Corazza O, Deluca P, Davey Z, Lucia DF, Farre M, Flesland L, Mannonen M, Pagani S, Peltoniemi T, Pezzolesi C, Scherbaum N, Siemann H, Skutle A, Torrens M, Van Der Kreeft P. Psychoactive drug mystical incense? Overview of the online available information on Spice products. International Journal of Culture and Mental Health. 2009;2:137–144. [Google Scholar]
- Schneir AB, Baumbacher T. Convulsions associated with the use of a synthetic cannabinoid product. Journal of medical toxicology: official journal of the American College of Medical Toxicology. 2012;8:62–4. doi: 10.1007/s13181-011-0182-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneir AB, Cullen J, Ly BT. “Spice” girls: synthetic cannabinoid intoxication. The Journal of emergency medicine. 2011;40:296–9. doi: 10.1016/j.jemermed.2010.10.014. [DOI] [PubMed] [Google Scholar]
- Seely KA, Lapoint J, Moran JH, Fattore L. Spice drugs are more than harmless herbal blends: a review of the pharmacology and toxicology of synthetic cannabinoids. Prog Neuropsychopharmacol Biol Psychiatry. 2012;39:234–43. doi: 10.1016/j.pnpbp.2012.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seely KA, Prather PL, James LP, Moran JH. Marijuana-based drugs: innovative therapeutics or designer drugs of abuse? Molecular interventions. 2011;11:36–51. doi: 10.1124/mi.11.1.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sewell RA, Skosnik PD, Garcia-Sosa I, Ranganathan M, D’Souza DC. Behavioral, cognitive and psychophysiological effects of cannabinoids: relevance to psychosis and schizophrenia. Rev Bras Psiquiatr. 2010;32(Suppl 1):S15–30. [PubMed] [Google Scholar]
- Shakes. Can’t Believe This Is Legal. 2008 http://www.erowid.org/experiences/exp.php?ID=74660.
- Shanks KG, Dahn T, Terrell AR. Detection of JWH-018 and JWH-073 by UPLC-MS-MS in postmortem whole blood casework. J Anal Toxicol. 2012;36:145–52. doi: 10.1093/jat/bks013. [DOI] [PubMed] [Google Scholar]
- Shootah. THC Substitute. 2008 http://www.erowid.org/experiences/exp.php?ID=74873.
- Shruming--Human. Notes on Some Legal Highs - Heart Problems. 2009 http://www.erowid.org/experiences/exp.php?ID=79488.
- Simmons J, Cookman L, Kang C, Skinner C. Three cases of “spice” exposure. Clin Toxicol (Phila) 2011a;49:431–3. doi: 10.3109/15563650.2011.584316. [DOI] [PubMed] [Google Scholar]
- Simmons JR, Skinner CG, Williams J, Kang CS, Schwartz MD, Wills BK. Intoxication from smoking “spice”. Ann Emerg Med. 2011b;57:187–8. doi: 10.1016/j.annemergmed.2010.08.039. [DOI] [PubMed] [Google Scholar]
- Skipper09. Can You Believe It’s Not Cannabis? 2009 http://www.erowid.org/experiences/exp.php?ID=79428.
- Sobolevsky T, Prasolov I, Rodchenkov G. Detection of JWH-018 metabolites in smoking mixture post-administration urine. Forensic science international. 2010;200:141–7. doi: 10.1016/j.forsciint.2010.04.003. [DOI] [PubMed] [Google Scholar]
- Sopris. It Really Is Like Cannabis. 2008 http://www.erowid.org/experiences/exp.php?ID=75825.
- SpacedOUTonSPICE. Excessive Cannabinoid Agonism. 2009 http://www.erowid.org/experiences/exp.php?ID=96704.
- St James J. Doctors concerned over possible link of K2, heart damage. 2010 http://www.wfaa.com/news/health/A-dangerous-link--100482134.html.
- Steve. Next-Night Seizures. 2011 http://www.erowid.org/experiences/exp.php?ID=89290.
- Teltzrow R, Bosch OG. Ecstatic anaesthesia: Ketamine and GHB between medical use and self-experimentation. Applied Cardiopulmonary Pathophysiology. 2012;16:309–321. [Google Scholar]
- Teske J, Weller JP, Fieguth A, Rothamel T, Schulz Y, Troger HD. Sensitive and rapid quantification of the cannabinoid receptor agonist naphthalen-1-yl-(1-pentylindol-3-yl)methanone (JWH-018) in human serum by liquid chromatography-tandem mass spectrometry. Journal of chromatography B, Analytical technologies in the biomedical and life sciences. 2010;878:2659–63. doi: 10.1016/j.jchromb.2010.03.016. [DOI] [PubMed] [Google Scholar]
- The--Pilgrim. Coming Out of the Haze. 2013 http://www.erowid.org/experiences/exp.php?ID=95740.
- Tofighi B, Lee JD. Internet highs--seizures after consumption of synthetic cannabinoids purchased online. Journal of addiction medicine. 2012;6:240–1. doi: 10.1097/ADM.0b013e3182619004. [DOI] [PubMed] [Google Scholar]
- Tung CK, Chiang TP, Lam M. Acute mental disturbance caused by synthetic cannabinoid: a potential emerging substance of abuse in Hong Kong. East Asian archives of psychiatry: official journal of the Hong Kong College of Psychiatrists = Dong Ya jing shen ke xue zhi: Xianggang jing shen ke yi xue yuan qi kan. 2012;22:31–3. [PubMed] [Google Scholar]
- Van der Veer N, Fiday J. Persistent psychosis following the use of Spice. Schizophrenia research. 2011;130:285–6. doi: 10.1016/j.schres.2011.04.022. [DOI] [PubMed] [Google Scholar]
- Vandrey R, Dunn KE, Fry JA, Girling ER. A survey study to characterize use of Spice products (synthetic cannabinoids) Drug Alcohol Depend. 2012;120:238–41. doi: 10.1016/j.drugalcdep.2011.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Various. Spice Experience Report Excerpts. 2009 http://www.erowid.org/chemicals/spice_product/spice_product_info1.shtml.
- Vearrier D, Osterhoudt KC. A teenager with agitation: higher than she should have climbed. Pediatr Emerg Care. 2010;26:462–5. doi: 10.1097/PEC.0b013e3181e4f416. [DOI] [PubMed] [Google Scholar]
- Wehrman J. Fake Marijuana Spurs More than 4,500 Calls to US Poison Centers. Alexandria, VA: American Association of Poison Control Centers; 2011. [Google Scholar]
- Wells DL, Ott CA. The “new” marijuana. The Annals of pharmacotherapy. 2011;45:414–7. doi: 10.1345/aph.1P580. [DOI] [PubMed] [Google Scholar]
- WelshSmoker. Horror Story. 2009 http://www.erowid.org/experiences/exp.php?ID=78880.
- Winstock AR, Barratt MJ. Synthetic cannabis: A comparison of patterns of use and effect profile with natural cannabis in a large global sample. Drug and alcohol dependence. 2013 doi: 10.1016/j.drugalcdep.2012.12.011. [DOI] [PubMed] [Google Scholar]
- Wood DM, Davies S, Puchnarewicz M, Button J, Archer R, Ovaska H, Ramsey J, Lee T, Holt DW, Dargan PI. Recreational use of mephedrone (4-methylmethcathinone, 4-MMC) with associated sympathomimetic toxicity. Journal of medical toxicology: official journal of the American College of Medical Toxicology. 2010;6:327–30. doi: 10.1007/s13181-010-0018-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood KE. Exposure to Bath Salts and Synthetic Tetrahydrocannabinol from 2009 to 2012 in the United States. The Journal of pediatrics. 2013 doi: 10.1016/j.jpeds.2012.12.056. [DOI] [PubMed] [Google Scholar]
- WYFF4.COM. Coroner: Synthetic Pot Killed College Athlete Anderson University Basketball Player Collapsed On Oct 4. 2011 http://www.wyff4.com/Coroner-Synthetic-Pot-Killed-College-Athlete/-/9324882/6133626/-/10gxauh/-/index.html#ixzz1yHFVkCK7.
- Young AC, Schwarz E, Medina G, Obafemi A, Feng SY, Kane C, Kleinschmidt K. Cardiotoxicity associated with the synthetic cannabinoid, K9, with laboratory confirmation. The American journal of emergency medicine. 2012;30:1320, e5–7. doi: 10.1016/j.ajem.2011.05.013. [DOI] [PubMed] [Google Scholar]
- Zawilska JB. “Legal highs” - new players in the old drama. Current drug abuse reviews. 2011;4:122–30. doi: 10.2174/1874473711104020122. [DOI] [PubMed] [Google Scholar]
- Zimmermann US, Winkelmann PR, Pilhatsch M, Nees JA, Spanagel R, Schulz K. Withdrawal phenomena and dependence syndrome after the consumption of “spice gold”. Deutsches Arzteblatt international. 2009;106:464–7. doi: 10.3238/arztebl.2009.0464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuardi AW, Morais SL, Guimaraes FS, Mechoulam R. Antipsychotic effect of cannabidiol. Journal of Clinical Psychiatry. 1995;56:485–6. [PubMed] [Google Scholar]
- Zuardi AW, Rodrigues JA, Cunha JM. Effects of cannabidiol in animal models predictive of antipsychotic activity. Psychopharmacology. 1991;104:260–4. doi: 10.1007/BF02244189. [DOI] [PubMed] [Google Scholar]
- Zuardi AW, Shirakawa I, Finkelfarb E, Karniol IG. Action of cannabidiol on the anxiety and other effects produced by delta 9-THC in normal subjects. Psychopharmacology. 1982;76:245–50. doi: 10.1007/BF00432554. [DOI] [PubMed] [Google Scholar]
- Zuba D, Byrska B, Maciow M. Comparison of “herbal highs” composition. Analytical and bioanalytical chemistry. 2011;400:119–26. doi: 10.1007/s00216-011-4743-7. [DOI] [PubMed] [Google Scholar]



