Abstract
Background
The Medicare accountable care organization (ACO) programs rely on delivery system integration and provider risk sharing to lower spending while improving quality of care.
Methods
Using 2009 Medicare claims and linked American Medical Association Group Practice data, we assigned 4.29 million beneficiaries to provider groups based on primary care use. We categorized group size according to eligibility thresholds for the Shared Savings (≥5,000 assigned beneficiaries) and Pioneer (≥15,000) ACO programs and distinguished hospital-based from independent groups. We compared spending and quality of care between larger and smaller provider groups and examined how size-related differences varied by 2 factors considered central to ACO performance: group primary care orientation (measured by the primary care share of large groups’ specialty mix) and provider risk sharing (measured by county health maintenance organization penetration and its relationship to financial risk accepted by different group types for managed care patients). Spending and quality of care measures included total medical spending, spending by type of service, 5 process measures of quality, and 30-day readmissions, all adjusted for sociodemographic and clinical characteristics.
Results
Compared with smaller groups, larger hospital-based groups had higher total per-beneficiary spending in 2009 (mean difference: +$849), higher 30-day readmission rates (+1.3% percentage points), and similar performance on 4 of 5 process measures of quality. In contrast, larger independent physician groups performed better than smaller groups on all process measures and exhibited significantly lower per-beneficiary spending in counties where risk sharing by these groups was more common (−$426). Among all groups sufficiently large to participate in ACO programs, a strong primary care orientation was associated with lower spending, fewer readmissions, and better quality of diabetes care.
Conclusions
Spending was lower and quality of care better for Medicare beneficiaries served by larger independent physician groups with strong primary care orientations in environments where providers accepted greater risk.
Keywords: delivery of health care, accountable care organizations, Medicare, health care costs, quality of health care, primary health care, aged, patient readmission
The Medicare accountable care organization (ACO) programs rely on both delivery system integration and provider risk sharing to lower Medicare spending while improving quality of care.1–4 Conceptually, large integrated groups of providers can realize efficiencies by managing care, coordinating care across specialties and settings, and controlling inputs of care such as specialty mix and service capacity.5–7 Under fee-for-service incentives, however, some forms of provider consolidation have instead promoted delivery of profitable specialty and supply-sensitive services.5,8–14 Thus, transitions to global payment arrangements, like those supported by ACO contracts, may be critical to achieving high-value care as providers consolidate.3,7,11,12,15
The ACO programs encourage providers to integrate into larger organizations, if not integrated already, to meet minimum size thresholds for participation. To establish market share and succeed under ACO-like risk contracts, organizations must also have or develop a substantial primary care workforce, because attribution of patients to ACOs is based on primary care use and because primary care practices typically serve as centers for care management and coordination. These key structural features have long been present among many provider groups, but with unclear clinical and economic consequences. Previous research suggests that larger physician organizations exhibit greater capacity for care management and quality improvement.16–21 Integration of physicians with hospitals, in contrast, has not been reliably associated with clinical systems to coordinate care.12,22–24 Although a strong foundation of primary care is considered essential to the success of ACOs, the evidence supporting this contention derives largely from area-level analyses of physician supply.25–29 Moreover, prior studies have not elucidated how organizational size relates to spending and outcomes,30,31 or how performance of larger groups on spending and quality measures varies by specialty mix and payment incentives.
Therefore, we used data from the American Medical Association (AMA) Group Practice File and linked Medicare claims to compare spending and quality of care for Medicare beneficiaries between larger and smaller provider groups. We distinguished hospital-based from independent groups and examined how size-related differences varied by the payment environment and primary care orientation of larger groups.
METHODS
Study Population and Data Sources
We analyzed 2009 Medicare claims for a random 20% sample of 5,867,482 traditional fee-for-service Medicare beneficiaries who were continuously enrolled in Parts A and B and received at least 1 primary care service during the year. Of these beneficiaries, we excluded 394,681 (6.7%) long-term nursing home residents identified by a validated algorithm,32 and 98,024 (1.7%) residents of U.S. territories or rural counties with fewer than 2,500 residents where there is little provider integration.33
For physicians in the AMA Physician Masterfile practicing in groups of ≥3, the AMA Group Practice File identifies their practice site(s) and parent organization if part of a larger group. It also characterizes practice sites as located at hospitals or not. We linked this information to Medicare claims via physicians’ National Provider Identifiers (NPIs). Of primary care physicians (PCPs) in the Masterfile serving Medicare beneficiaries in 2009 and practicing in groups of ≥3 physicians, 90% were linked to the Group Practice File (Appendix).
Study Variables
Characteristics of Assigned Provider Groups
Following the Medicare Shared Savings Program assignment rules, we attributed each beneficiary to the provider group accounting for the most allowed charges for primary care services among all groups providing primary care to the beneficiary (Appendix).2 To identify provider groups, we used both the AMA Group Practice File and tax identification numbers (TINs) indicating billing entities in Medicare claims. We applied the attribution algorithm to each beneficiary twice, using each of these 2 sources of group identifiers independently. For groups identified by the Group Practice File as members of larger organizations, we used the highest level of organization to which they were connected when assigning beneficiaries. Because TINs and AMA Group Practice data were complementary in identifying higher levels of provider organization, for each beneficiary we used the larger of the 2 assigned groupings for analyses, as determined by the number of PCPs affiliated with each (Appendix).
We categorized the size of provider groups according to eligibility for the two Medicare ACO programs: small groups ineligible for ACO programs (<5,000 assigned beneficiaries); medium-sized groups potentially eligible for the Shared Savings Program (5,000–14,999); and large groups potentially eligible for the Pioneer program (≥15,000), scaling eligibility thresholds to the 20% sample. Relative to the use of TINs alone, the incorporation of AMA Group Practice data increased the number of beneficiaries in the potentially ACO-eligible categories by 54% (Appendix), suggesting many larger groups bill at organizational levels below the highest levels identified in the Group Practice File. This finding is consistent with the operational definition of an ACO in the Shared Savings Program as a collection of TINs rather than a single TIN.2
From the Group Practice data, we characterized provider groups as hospital-based if ≥10% of a group’s practice sites were located at hospitals; 93.9% of groups with at least 1 hospital-based site were classified as hospital-based accordingly. We dichotomized this organizational characteristic to facilitate interpretation of results. We selected a threshold of ≥10% because large hospital systems or physician-hospital organizations may include many practices not located at hospitals, while large physician groups that are independent of hospitals may nevertheless include a few practices located at hospitals. In a validation analysis using claims, we calculated the proportion of spending on primary care services for each beneficiary that was billed by physicians employed by hospitals. This proportion was more than 50% greater for beneficiaries assigned to hospital-based groups than for other beneficiaries.
We excluded 1,083,781 beneficiaries (20.2% of those otherwise meeting inclusion criteria) who could not be assigned to a provider group in the Group Practice File, most of whom (74%) were excluded because their primary care physicians were not practicing in groups of ≥3. Thus, our study sample (N=4,290,996) represented approximately 94% of traditional Medicare beneficiaries receiving primary care from groups of ≥3 physicians (Appendix).
For each medium-sized and large group, we additionally determined the fraction of physicians who were PCPs (Appendix). To facilitate interpretation of results, we characterized groups as having a strong primary care orientation if this fraction exceeded 35% (a specialty to primary care ratio of roughly less than 2:1).
To focus the presentation of results on the most informative comparisons, we combined similar results for medium-sized and large hospital-based groups and omit results for a small group (8.8%) of beneficiaries assigned to small hospital-based groups. Thus, we compared small physician groups (the reference category) with 3 categories of provider groups sufficiently large for ACO program participation: 1) medium-sized independent physician groups; 2) large independent physician groups; and 3) hospital-based groups (medium-sized or large).
Payment Environments
We used health maintenance organization (HMO) market penetration to characterize county-level prevalence of provider risk sharing. From HealthLeaders InterStudy data and the Medicare enrollment database,34 we calculated for each county the fraction of Medicare and commercially insured residents combined who were in HMO plans in 2009. To ease interpretation, we grouped beneficiaries into 3 categories of county-level HMO penetration: <25% (48.9% of beneficiaries); 25–49% (38.3%); and ≥50% (12.8%).
Greater HMO market penetration has been associated with more frequent use of capitation arrangements between private payers and providers, and with lower fee-for-service Medicare spending.35–38 Lower Medicare spending also has been found for beneficiaries in highly capitated practices.39 Using data from the 2004–2005 Community Tracking Study (CTS) Physician Survey, we furthermore determined that the percentage of practice revenues from capitated payments increases with commercial HMO penetration substantially more for larger independent physician groups than for smaller or hospital-based groups (Table 1). These findings are consistent with larger groups’ greater capacity to bear risk and with hospital-based practices’ greater bargaining power and emphasis on service volume and specialty care.12,40–45 Accordingly, we hypothesized that higher HMO penetration would be more strongly associated with lower per-beneficiary spending for medium-sized and large independent physician groups than for small or hospital-based groups.
Table 1.
Association between commercial HMO penetration and capitation, by type of provider group*
| Community Tracking Study physician sample and type of provider group† | Mean percent of practice revenues from capitated payments | P value | |||||
|---|---|---|---|---|---|---|---|
| Commercial HMO penetration | Quartile 4-1 difference | Difference in quartile 4-1 difference relative to small | |||||
| Quartile 1 (0–35%) | Quartile 2 (36–42%) | Quartile 3 (43–53%) | Quartile 4 (>53%) | ||||
| Primary care physicians (N=2,233) | |||||||
| Small groups | 8.0 | 10.6 | 11.5 | 21.5 | +13.5 | - | - |
| Medium/large groups | 10.2 | 15.9 | 17.4 | 50.2 | +40.0 | +26.5 | <0.001 |
| Hospital-based groups | 5.4 | 15.2 | 24.3 | 16.6 | +11.2 | −2.3 | 0.51 |
| All physicians (N=4,354) | |||||||
| Small groups | 6.6 | 7.1 | 9.0 | 14.1 | +7.5 | - | - |
| Medium/large groups | 8.3 | 9.2 | 13.4 | 28.5 | +20.2 | +12.7 | <0.001 |
| Hospital-based groups | 10.6 | 12.2 | 15.5 | 13.0 | +2.4 | −5.1 | 0.07 |
Estimates are from the 2004–2005 Community Tracking Study (CTS) Physician Survey. HMO penetration was measured at the CTS site level. All estimates have been adjusted for the complex survey design.
Categories of group size as defined by the CTS: small = 1–10 physicians, medium/large = 11+ physicians.
Medical Spending and Utilization
For each beneficiary, we calculated total spending in 2009 for all services covered by Parts A and B by summing Medicare reimbursements, coinsurance amounts, and payments from other primary payers. We excluded indirect medical education (IME) and disproportionate share hospital payments. We categorized all spending broadly by type of claim and spending on physician and ancillary services more specifically by Berenson-Eggers Type of Service (BETOS) codes. We also analyzed annual counts of acute-care hospitalizations (excluding transfers), hospital outpatient department visits, and physician office visits.
Quality of Care
Among beneficiaries hospitalized in 2009, we estimated the fraction readmitted within 30 days of discharge at least once during the year. Because our study focused on integration of the outpatient delivery system, we excluded readmissions from nursing facilities. Results were similar when these readmissions were included.
We also constructed from claims several process measures of quality of care, adapted from the Healthcare Effectiveness Data and Information Set (HEDIS®): screening mammography in 2008 or 2009 for women ages 65–69; LDL cholesterol testing in 2009 for beneficiaries with a history of ischemic heart disease, myocardial infarction, or stroke; and 3 services for beneficiaries with diabetes, including hemoglobin A1c and LDL cholesterol testing in 2009 and a diabetic retinal exam in 2008 or 2009.
Beneficiary Characteristics
From Medicare enrollment files, we determined age, sex, race, disability upon enrollment in Medicare, presence of end-stage renal disease, and Medicaid eligibility. From U.S. Census data, we assessed additional socioeconomic characteristics of the elderly population in beneficiaries’ zip code tabulation areas (Table 2).46 Using information from the Chronic Condition Warehouse (CCW),47 we determined if beneficiaries had been diagnosed with any of 21 conditions prior to January 1, 2009 (Appendix Table 1). Because the CCW includes diagnoses since 1999 and focuses on chronic conditions, these indicators were arguably less sensitive to potential differences in coding practices among group types than risk scores derived from concurrent or recent claims.
Table 2.
Sociodemographic and clinical characteristics of Medicare beneficiaries assigned to different types of provider groups, adjusted for county of residence.
| Provider Group Type | ||||
|---|---|---|---|---|
| Small groups (reference category) (N=1,924,001) | Groups sufficiently large to participate in ACO programs | |||
| Medium-sized independent groups (N=678,004) | Large independent groups (N=524,950) | Hospital-based groups (N=785,795) | ||
| Number of organizations* | 19,838 | 584 | 138 | 391 |
| Number of physicians† | ||||
| No. physicians, mean | 12.5 | 95.0 | 457.8 | 546.7 |
| No. primary care physicians, mean | 6.8 | 43.4 | 217.4 | 194.1 |
| Beneficiary characteristics | ||||
| Age (years), mean | 72.8 | 72.9 | 72.7 | 72.0 |
| Female, % | 58.4 | 59.6 | 59.4 | 58.7 |
| Race/ethnicity, % | ||||
| White | 91.5 | 91.9 | 91.7 | 89.5 |
| Black | 5.6 | 5.6 | 5.8 | 7.7 |
| Hispanic | 0.9 | 0.7 | 0.7 | 0.9 |
| Other | 2.0 | 1.7 | 1.9 | 1.9 |
| Medicaid recipient,‡ % | 16.5 | 15.4 | 15.6 | 18.0 |
| Disabled,¶ % | 21.6 | 21.3 | 21.3 | 23.7 |
| ESRD, % | 1.2 | 1.1 | 1.1 | 1.6 |
| Conditions from Chronic Condition Warehouse§ | ||||
| 3+ conditions, % | 50.7 | 49.5 | 48.2 | 49.9 |
| 4+ conditions, % | 35.9 | 34.5 | 33.4 | 35.0 |
| 5+ conditions, % | 23.9 | 22.8 | 22.0 | 23.0 |
| Total no. conditions, mean | 2.9 | 2.9 | 2.8 | 2.9 |
| ZCTA-level characteristics, mean | ||||
| % below FPL | 10.4 | 10.3 | 10.2 | 10.5 |
| % with high school degree | 72.2 | 72.5 | 72.6 | 72.3 |
| % with college degree | 14.8 | 15.2 | 15.2 | 15.2 |
ACO = accountable care organization; ESRD = end-stage renal disease; ZCTA = zip code tabulation area.
Numbers of organizations presented for each category are based on the number of AMA Group Practice File group identifiers meeting the definition for each category. For groups sufficiently large to participate in ACO programs, we also included in these counts the number of TINs meeting categorical definitions with attributed populations of beneficiaries that were distinct from those of Group Practice File groups meeting categorical definitions (to identify the total number of distinct larger groups identified both by the Group Practice File and TINs).
These organizational characteristics (numbers of physicians per organizations) were ascertained for each beneficiary based on their assigned provider group and averaged across beneficiaries to weight a specific group’s contribution to the average by the number of beneficiaries assigned to it.
Medicaid eligibility is based on state buy-in indicators in Medicare enrollment files.
Disability is based on the original reason for Medicare eligibility (aged vs. disabled vs. ESRD).
See Appendix Table 1 for comparisons of each of the 21 conditions in the Chronic Condition Warehouse: diabetes, ischemic heart disease, myocardial infarction, congestive heart failure, atrial fibrillation, chronic kidney disease, stroke or TIA, COPD, depression, osteoarthritis or rheumatoid arthritis, osteoporosis, hip fracture, dementia, Alzheimer’s disease, breast cancer, colorectal cancer, prostate cancer, lung cancer, endometrial cancer, glaucoma, cataracts. Summary chronic condition counts do not include the two ophthalmologic conditions, glaucoma and cataracts.
Statistical Analysis
We fitted linear regression models predicting spending or quality of care for beneficiaries as a function of their assigned provider group category, omitting small physician groups as the reference category. We included in models the sociodemographic and clinical characteristics described above, as well as county fixed effects to adjust for geographic variation in health care markets, practice patterns, diagnostic coding, and Medicare fees.48–51 To allow non-additive effects of multiple conditions on spending, we also included in models 6 indicators of having ≥2 to ≥7 conditions.
Using these models, we compared each of the 3 group types meeting the size requirement for ACO program participation with the reference category of smaller groups. We then included interaction terms to allow differences between these larger and smaller groups to vary by 2 factors considered central to ACO performance: 1) provider risk sharing, as measured by county HMO penetration; and 2) the primary care orientation of larger groups.
We conducted several sensitivity analyses. First, we specified measures of hospital integration, HMO penetration, and PCP orientation as linear rather than categorical variables. Second, we adjusted for outpatient facility fees routinely charged by hospital-based providers (Appendix).12 Third, we explored whether the strength of provider groups’ affiliations with academic teaching hospitals could have contributed to spending differences among provider group categories (Appendix). Fourth, we assessed potential contributions of unobserved differences in case mix to spending differences among provider group categories. Specifically, we additionally adjusted for whether conditions had been newly diagnosed in 2008. We also explored the possibility that recent hospitalizations in 2008 could have shifted beneficiary assignments to hospital-based groups in 2009, thereby contributing to greater illness severity for hospital-based groups. Finally, we compared results before and after adjustment for CCW conditions.
Our main results were not substantively changed by use of log and logistic link functions when modeling spending and quality measures, respectively. All analyses were conducted with SAS, version 9.2 (SAS Institute, Cary, North Carolina). Our study protocol was approved by the Harvard Medical School Committee on Human Studies and Privacy Board of the Centers for Medicare and Medicaid Services.
RESULTS
In descriptive analyses adjusted for county of residence, beneficiaries assigned to hospital-based groups were slightly more likely than those assigned to other groups to be non-white, disabled, and Medicaid recipients (Table 2). Differences among provider group categories in chronic disease burden and other sociodemographic characteristics were small (see Appendix Table 1 for condition-specific comparisons).
Differences in Spending between Larger and Smaller Groups
Compared with small physician groups, total annual per-beneficiary spending was similar for medium-sized (−$69) and large (−$44) independent physician groups. Spending on procedures, imaging, and cardiac tests was consistently lower for beneficiaries assigned to these larger physician groups, whereas spending on other BETOS categories and hospital care was similar to small groups (Table 3).
Table 3.
Health care spending and quality for 2009 Medicare beneficiaries by provider group type
| Annual spending, utilization, or quality metric | Provider Group Type | |||
|---|---|---|---|---|
| Small groups (reference category) | Groups sufficiently large to participate in ACO programs | |||
| Medium-sized independent groups | Large independent groups | Hospital-based groups | ||
| Adjusted mean | Difference relative to reference category | Difference relative to reference category | Difference relative to reference category | |
| Total per-beneficiary medical spending, $ | 11,332 | −69 | −44§ | 849 |
| Spending by type of claim, $* | ||||
| Hospital facility | 3,722 | 22§ | 34§ | 455 |
| Physician/supplier | 3,441 | −100 | −168 | −29 |
| Hospital outpatient department | 2,285 | 29 | 52 | 355 |
| Skilled nursing facility | 751 | −21 | −1§ | 5§ |
| Spending on physician and ancillary services by BETOS category, $† | ||||
| Office visits | 643 | 1§ | 0§ | 39 |
| Specialty consultations | 286 | −3§ | −3§ | 1§ |
| Major procedures | 777 | −23 | −26 | 11§ |
| Minor and ambulatory procedures, endoscopy | 869 | −39 | −21 | 5§ |
| Imaging | 739 | −13 | −17 | 16 |
| Cardiac interventions and tests | 233 | −6 | −9 | 5 |
| Radiation therapy, chemotherapy and other Part B-covered drugs | 731 | 8§ | −17§ | 240 |
| Lab tests | 432 | −2§ | 0§ | 33 |
| Utilization, n | ||||
| Hospitalizations‡ | 0.37 | 0.00§ | 0.00§ | 0.02 |
| Physician office visits | 8.37 | −0.12 | −0.24 | −0.24 |
| Hospital outpatient department visits | 5.58 | 0.11 | 0.39 | 1.32 |
| Quality of Care, %¶ | ||||
| 30-day readmission | 16.1 | 0.3 | 0.3 | 1.3 |
| Screening mammography | 70.7 | 1.7 | 1.7 | 2.8 |
| Diabetes | ||||
| LDL cholesterol testing | 74.5 | 1.6 | 1.4 | −0.3§ |
| Hemoglobin A1c testing | 71.1 | 2.4 | 3.0 | 0.6 |
| Retinal exam | 73.6 | 0.7 | 1.1 | 0.3§ |
| All 3 services | 46.7 | 2.2 | 2.9 | 0.8 |
| Cardiovascular disease | ||||
| LDL cholesterol testing | 69.2 | 0.9 | 0.6 | −0.7 |
ACO = accountable care organization; BETOS = Berenson-Eggers Type of Service; LDL = low-density lipoprotein.
Does not include lesser contributions from spending on home health, durable medical equipment, and hospice care. Spending on physician/supplier services is totaled from the carrier claims file. Of note, hospital outpatient department spending (totaled from the outpatient file) contains some additional spending on physician services.
Includes claims for physician and ancillary (supplier) services appearing in the carrier file as well as claims for physician and ancillary services appearing in the hospital outpatient department claims file. Analyses of spending by BETOS categories were restricted to the 5% sample of Medicare beneficiaries, for whom we had both hospital outpatient department and carrier claims files. BETOS codes were grouped as follows: office visits (M1A-M1B); specialty consultations (M5A-M5D, M6); major procedures (P0, P4A-P4E, P1A-P3D except P2D); minor and ambulatory procedure and endoscopy (P5A-P5E, P6A-P6D, P8A-P8I); imaging (I1A-I1F, I2A-I2D, I3A-I3F); cardiac catheterization, testing, and imaging (I4A-I4B, P2D, T2A-T2D); radiation therapy, chemotherapy, and other drugs (P7A-P7B, O1D-O1E); lab tests (T1A-T1H).
Hospitalization counts exclude transfers.
Analyses of quality measures were restricted to the 5% sample of Medicare beneficiaries, for whom we had hospital outpatient department, inpatient facility, and carrier claims to assess receipt of key services. Readmissions were assessed among beneficiaries with at least one acute care hospitalization in 2009. We counted only one readmission per beneficiary annually in calculating 30-day readmission rates. Screening mammography was assessed among women ages 65–69 years. Diabetes services were assessed among beneficiaries with a history of diabetes prior to 2009. LDL testing for cardiovascular disease was assessed among beneficiaries with ischemic heart disease, history of myocardial infarction, or history of stroke or TIA present prior to 2009.
Denotes lack of statistically significant difference relative to reference category of small groups. All other estimates for potentially ACO-eligible group types differ significantly from small groups at least at the P<0.05 level.
In contrast, total per-beneficiary spending was $849 higher (P<0.001) for medium-sized or large hospital-based groups than for small physician groups (Table 3). This difference was explained by higher spending on both inpatient and outpatient care, including office visits, imaging, lab tests, cancer therapies, and other drugs covered by Part B. Outpatient facility fees contributed minimally to these differences (Appendix).
Differences in Quality of Care between Larger and Smaller Groups
Relative to small physician groups, medium-sized and large independent physician groups performed consistently better on process measures of quality of care but hospital-based groups did not (Table 3). Thirty-day readmission rates were 1.3 percentage points higher for hospital-based groups (P<0.001) but only slightly higher for medium-sized and large independent physician groups.
Effect Modification by HMO Penetration and Primary Care Orientation
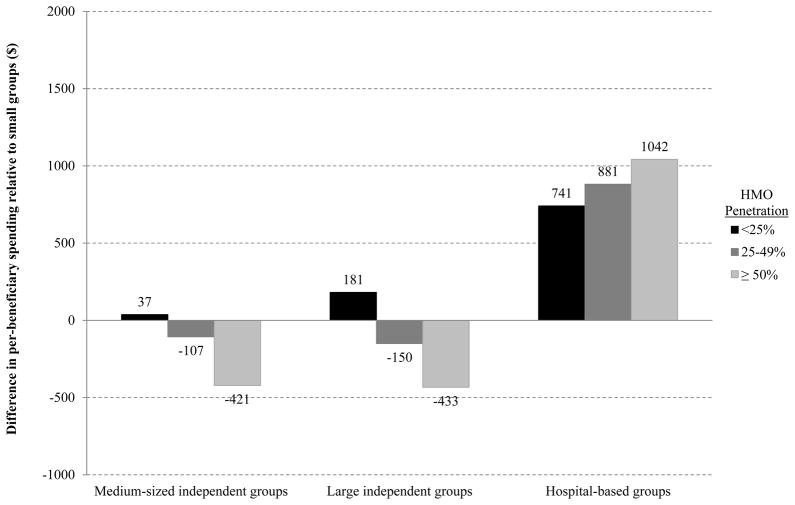
Higher HMO penetration was more strongly associated with lower total per-beneficiary spending for both medium-sized and large independent physician groups than for small groups (Figure 1). Total per-beneficiary spending was slightly higher for these larger physician groups than for small groups in counties with low HMO penetration, but substantially lower in counties with high HMO penetration (−$421 for medium-sized and −$433 for large independent physician groups; P<0.001). As expected from the weaker relationship between HMO penetration and financial risk sharing by hospital-based groups (Table 1), higher spending exhibited by hospital-based groups did not diminish with increasing HMO penetration (Figure 1).
Figure 1. Differences in total per-beneficiary spending between larger and smaller provider groups, by HMO penetration.
Differences between groups sufficiently large to participate in ACO programs and the reference category of small groups are displayed by HMO penetration. Increasing HMO penetration from low (<25%) to high (≥50%) was associated with decreases in total per-beneficiary spending for medium-sized and large independent physician groups, relative to small groups (differential reductions: −$458 for medium-sized and −$614 for large independent groups; P<0.001). In counties with high HMO penetration, total per-beneficiary spending was $421 to $433 lower (P<0.001) for these groups than for small groups. As expected from the weaker relationship between HMO penetration and financial risk sharing by hospital-based groups (Table 1), differences in spending between hospital-based and small groups did not diminish with increasing HMO penetration.
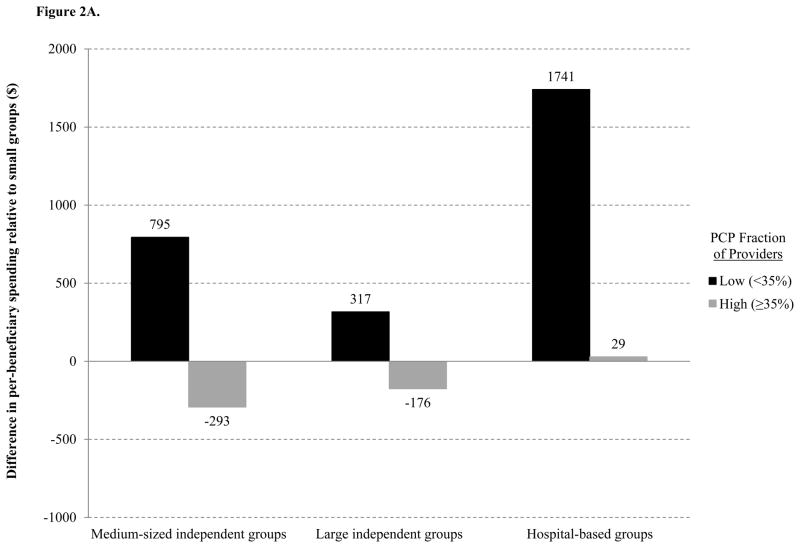
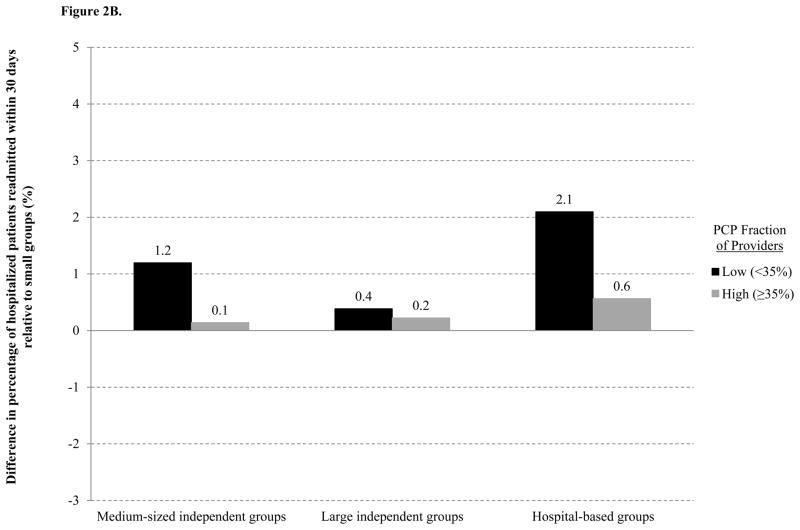
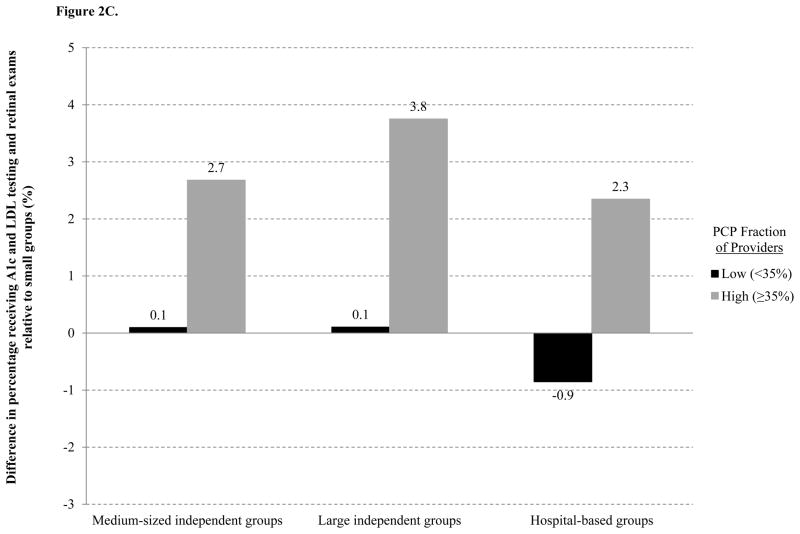
Relative to small groups, total per-beneficiary spending (Figure 2A) was $317 to $1741 higher for larger groups with low primary care fractions of physicians (P<0.001), but similar or lower for those with high primary care fractions (+$29 for hospital-based groups; P=0.48; −$293 for medium-sized and −$176 for large independent physician groups; P<0.001). Among larger groups, a specialty mix with a high primary care fraction was similarly associated with fewer readmissions and better quality of diabetes care (Figure 2B–C). (See Appendix Tables 2–3 for detailed results.)
Figure 2. Differences between larger and smaller provider groups in A) total per-beneficiary spending, B) 30-day readmission rates, and C) quality of diabetes care, by group primary care orientation.
Differences between groups sufficiently large to participate in ACO programs and the reference category of small groups are displayed by primary care orientation of larger groups’ specialty mix. Relative to small groups, total per-beneficiary spending was higher, 30-day readmission rates mostly higher, and quality of diabetes care similar or slightly worse for larger groups with low primary care fractions of physicians. In contrast, for groups with high primary care fractions of physicians, spending was similar or lower, readmission rates mostly similar, and quality of diabetes care consistently better. Thus, a specialty mix with a high primary care fraction was associated with (A) reduced differences between small and larger groups in total per-beneficiary spending (reduction in difference: −$492 to −$1,712; P<0.001), (B) reduced differences in 30-day readmission rates (−1.1 to −1.5 percentage points; P<0.001) except for large independent physician groups (−0.2 percentage points; P=0.61), and (C) increased differences indicating better quality of diabetes care (+2.6 to +3.6 percentage points in the fraction of beneficiaries receiving all three diabetes services; P<0.001).
Sensitivity Analyses
Results were substantively similar when measures of hospital integration, HMO penetration, and primary care orientation were specified as linear rather than categorical predictors. Adjusting for recency of diagnoses did not appreciably change results of any analysis. Hospitalization in 2008 was equally likely to predict a change in assignment from an independent physician group to a hospital-based group as the reverse. Adjustment for CCW conditions slightly increased the difference in total spending between hospital-based and small groups from $845 to $849 per beneficiary.
COMMENT
In this national study of spending and quality of care for Medicare beneficiaries, differences between larger and smaller provider groups varied substantially by larger groups’ specialty mix, payment environment, and structural relationship with hospitals. When not based at hospitals, larger groups performed modestly better on process measures of quality of care than smaller groups with similar adjusted per-beneficiary spending.
In contrast, spending was higher and quality of care not better for beneficiaries assigned to larger hospital-based groups than for those assigned to smaller physician groups, consistent with other studies of physician-hospital consolidation.12,24,40,52 Although integration between physicians and hospitals theoretically could support continuity during care transitions, readmission rates were highest for hospital-based groups. These findings were explained almost entirely by the specialty orientation of groups, as a strong primary care orientation was associated with substantially lower spending, fewer readmissions, and better quality of diabetes care among hospital-based groups.
For medium-sized and large independent physician groups, too, differences in spending relative to smaller groups varied substantially by specialty mix. Spending was lower for those with strong primary care orientations but higher for those with weak primary care orientations. Medium-sized and large groups with strong primary care orientations – hospital-based or not – also performed consistently better on process measures of quality of care than smaller groups. These findings suggest provider consolidation in a largely fee-for-service payment environment has been associated with slightly lower spending and modest gains in quality of care when centered on primary care but not when centered on specialty care.
For medium-sized and large independent physician groups, differences in spending relative to smaller groups were also related to HMO penetration. Per-beneficiary spending was slightly higher for these groups in counties with low HMO penetration but substantially lower in counties with high HMO penetration. This finding is consistent with evidence from the CTS suggesting larger independent physician groups are substantially more likely than small or hospital-based groups to accept financial risk in areas of high HMO penetration.
Our findings have several important policy implications. First, as hospitals employ increasing numbers of physicians,11,12,15 the specialty mix of their medical staffs may be an important predictor of quality and costs of care. Second, continued consolidation of specialists may contribute to higher Medicare spending in fee-for-service environments, as suggested by prior research,5,8,10,11 whereas efforts to strengthen primary care may be associated with lower spending.25–27,53,54 Third, consistent with recent studies,39,55–57 our results support the notion that promoting both delivery system integration and provider risk sharing may lower spending while improving quality of care, as intended by Medicare ACO programs. Fourth, our study provides no suggestion that organizational size will predict performance among ACOs. Both medium-sized and large independent physician groups exhibited lower spending on procedures, imaging, and tests, suggesting potentially less intensive and duplicative care. Moreover, greater provider risk sharing was associated with similarly reduced spending for these groups relative to smaller groups. Our findings do suggest, however, that ACOs with strong primary care orientations may perform better on ACO quality metrics.
Our study has several limitations, the most important of which is its observational design. Unobserved differences among beneficiaries assigned to different types of provider groups could have contributed to our results. Observed differences in chronic disease burden, however, were minimal. Compared with small groups, spending was substantially higher for hospital-based groups despite slightly fewer assigned beneficiaries with multiple conditions. Adjustment for observed conditions actually increased the spending difference between hospital-based and small groups slightly, suggesting adjustment for unobserved differences in case mix may have increased this difference further. Because assignments were driven largely by primary care received from PCPs, the lack of observed case-mix differences between independent physician groups oriented more toward primary care and hospital-based groups oriented more toward specialty care was not unexpected. For example, a beneficiary with a new condition requiring specialty care from a hospital-based group would not be assigned to that group if the beneficiary continued to receive primary care from a PCP at another group. The need for more intensive specialty care from one group might induce a switch to a new PCP at that group, but we found no evidence that hospitalization predicted net changes in assignment to hospital-based groups. In addition, controlling for newly diagnosed conditions did not materially affect our results.
We were unable to compare the relationship between provider risk sharing and spending for hospital-based vs. smaller groups, because the association between HMO penetration and capitation was equally weak for these groups. Thus, our findings provide no basis for predicting whether hospital-based groups might achieve greater or lesser savings as risk-bearing ACOs than independent groups. In addition, we relied on commercial and Medicare Advantage HMO enrollment to assess the relationship between provider risk sharing and spending for traditional fee-for-service beneficiaries. HMO penetration has been strongly associated with lower spending for traditional Medicare beneficiaries,37–39 but such spillover effects are likely to be smaller than effects of risk contracts directly involving traditional Medicare beneficiaries. Moreover, we could not distinguish effects of HMO penetration on provider risk sharing from effects of provider group efficiency and willingness to bear risk on HMO penetration.
Although the link between group size and structural capacity for care management and quality improvement has been robustly established,16–21 we lacked the necessary data to identify specific structural or cultural mediators of our findings. Finally, our analysis was limited to the Medicare population. Provider integration may increase prices paid by commercial insurers,13,23,24,58 thereby potentially negating reductions in spending for Medicare beneficiaries that might result from the growth of ACOs.45 Achieving higher value care for both publicly and privately insured populations may require the preservation of provider competition in ACO-dominated markets as well as the spread of both Medicare and commercial ACO contracts to align incentives across payers.
The impact of the Medicare ACO programs, as determined from quasi-experimental evaluations, will not be known for several years. Our observational findings from existing variation in organizational features and incentives are nevertheless consistent with the conceptual basis for these programs – namely, that policies coupling delivery system integration with provider risk sharing, while strengthening primary care, may lower spending and improve quality of care for Medicare beneficiaries.
Supplementary Material
Acknowledgments
We are grateful to Cynthia Saiontz-Martinez for statistical programming for secondary analyses of data from the Community Tracking Study Physician Survey, and to John Z. Ayanian, M.D., M.P.P., Thomas G. McGuire, Ph.D., and Joseph P. Newhouse, Ph.D. for helpful comments on an earlier draft of this manuscript.
Funding: Supported by grants from the Beeson Career Development Award Program (National Institute on Aging K08 AG038354 and the American Federation for Aging Research), Doris Duke Charitable Foundation (Clinical Scientist Development Award #2010053), and National Institute on Aging (P01 AG032952).
The sponsors played no role in the design or conduct of the study; in the collection, management, analysis, or interpretation of the data; or in the preparation, review, or approval of the manuscript.
APPENDIX
A. Linkage to American Medical Association (AMA) Group Practice File
The linkage of NPIs to the AMA Masterfile and Group Practice File was conducted by Medical Marketing Services, Inc., based on a finder file we submitted containing all NPIs with any physician specialty that appeared in 2009 Part B (carrier) claims for a 20% random sample of Medicare beneficiaries.
For physicians in the AMA Physician Masterfile practicing in groups of 3 or more, the AMA Group Practice File identifies their practice site(s) and, if part of a larger group, the position of member practices in larger organizational structures (as satellites of parent groups, parents to smaller practices, or both). For group practices identified as members of larger parent organizations, we used the highest level of organization to which they were connected (through up to 5 levels of hierarchical relationships) for analyses. For example, a practice site may be part of a multi-site group practice, which may be a member of a larger physician organization, which in turn may be part of a larger integrated delivery system. In that case, we focused only on the membership of linked NPIs to the larger integrated delivery system. Physician rosters and practice information in the Group Practice File are verified and updated every 9–12 months by the AMA Group Practice Unit via telephone and fax communications with practice managers and from provider group websites.
Using the following procedure, we determined that the AMA Group Practice File identified provider groups for approximately 90% of primary care physicians (PCPs) in the AMA Masterfile who were treating Medicare beneficiaries in 2009 and practicing in groups of 3 or more physicians. From 2009 Part B carrier claims for the 20% sample of beneficiaries, we identified 128,658 PCPs (Health Care Financing Administration (HCFA) provider specialty codes for general practice (01), family practice (08), internal medicine (11), or geriatric medicine (38)) actively providing outpatient primary care services (Current Procedural Terminology (CPT) codes 99201–99215 or G0402) to at least 5 Medicare beneficiaries, following the definitions of PCPs and outpatient primary care services used by the assignment rules for the Medicare Shared Savings Program (SSP) and Pioneer ACOs (Appendix Table 4).
Of these PCPs, 96.1% were linked via their NPIs to the AMA Physician Masterfile. We assumed PCPs without Group Practice File records who were billing primarily under tax identification numbers (TINs) associated with only 1 or 2 NPIs in Part B carrier claims were not likely to be practicing in groups of 3 or more. After excluding this group, 68.1% of PCPs in the AMA Masterfile were linked to the Group Practice File. We improved this linkage rate to 89.5% by inferring group practice affiliations for PCPs not linked to the Group Practice File who shared TINs with PCPs who were linked to the Group Practice File. Specifically, we defined each NPI’s primary office-based TIN as the TIN associated with the most allowed charges by that NPI for outpatient visits in Part B carrier claims. We then assigned each non-linked NPI to the parent group in the AMA Group Practice File to which other NPIs with the same primary office-based TIN were most frequently linked. We similarly inferred group practice affiliations for nurse practitioners and physician assistants (HCFA provider specialty codes 50 and 97) whose NPIs were not linked to the AMA Masterfile (because it only includes physicians) but who are recognized as providers in Medicare ACO assignment algorithms, as described below.
Among medical and surgical specialists identified in 2009 carrier claims, 90.8% were linked to the AMA Masterfile. Of those likely practicing in groups of 3 or more, we determined AMA group practice affiliations for 64.8% (51.7% via direct linkage and 13.1% via a similar inference procedure). These lower linkage rates for specialists were less consequential because beneficiary assignment under the SSP rules is driven primarily by receipt of primary care from PCPs, as described below. In addition, we would not expect some specialists (e.g., consulting proceduralists) to be identified by the Group Practice File or to contribute to beneficiary assignment, because of limited practice in office-based settings.
B. Assigning Beneficiaries to Provider Groups
Following the Medicare Shared Savings Program (SSP) rules, we assigned each beneficiary who received at least 1 primary care service from a PCP to the provider group accounting for the most allowed charges among all provider groups for primary care services provided by PCPs. Per the SSP rules, we then assigned the minority of beneficiaries (23.9%) who received no primary care services from a PCP to provider groups accounting for the plurality of allowed charges for primary care services provided by any provider, including physician extenders and specialists.
In both the Medicare SSP and Pioneer rules, the definition of primary care services includes physician visits at nursing facilities (Appendix Table 4). We excluded these services from the definition of primary care services when assigning beneficiaries to provider groups, because the inclusion of physician visits at nursing facilities causes the assignment of over 25% of community-dwelling beneficiaries receiving post-acute care to shift away from the provider group providing primary care to the group providing post-acute care.1
Using Part B carrier claims for physician services, we applied the SSP assignment algorithm to each beneficiary twice, separately using TINs and provider groups identified in the AMA Group Practice File. To characterize the size of each beneficiary’s assigned provider group, we used the larger of the two assigned groupings for analyses, as determined by the number of PCPs affiliated with each (and in the case of equal numbers of PCPs, the number of beneficiaries assigned to each). We did this because we found that TINs and AMA Group Practice data were complementary in identifying higher levels of provider organization. As described in Appendix Table 5, the incorporation of AMA Group Practice data increased the number of beneficiaries assigned to ACO-eligible groups by 54%. This increase suggests many large provider groups bill at organizational levels (identified by their TINs) below those identified in the AMA Group Practice File. Relative to the use of AMA Group Practice data alone, assignments to TINs increased the number of beneficiaries assigned to ACO-eligible groups by 4%, suggesting fewer cases in which TINs identified higher organizational levels.
We excluded 391,546 beneficiaries who could not be assigned to a TIN or provider group in the AMA Group Practice File because they used no primary care services. We excluded 1,083,781 beneficiaries (20.2% of those otherwise meeting inclusion criteria) who could not be assigned to a provider group in the AMA Group Practice File and for whom we consequently lacked information on hospital integration. Most in this group (we estimate 797,328 or 73.6%) were excluded because they received primary care from physicians who were not practicing in groups of 3 or more, as indicated by no more than 1 other NPI sharing their primary TIN and by their lack of linkage to the AMA Group Practice File. The remaining 286,453 beneficiaries could not be assigned to a provider group in the AMA Group Practice File because their primary care providers were not linked either to the Masterfile or to the Group Practice File despite actively providing care to Medicare beneficiaries and ostensibly practicing in groups of 3 or more. Thus, our study sample was representative of approximately 93.7% (4,290,996/(4,290,996 + 286,453)) of traditional Medicare beneficiaries receiving primary care from groups of 3 or more physicians.
C. Specialty Mix of Provider Groups
We ascertained the primary specialty for each physician by determining the HCFA specialty code most often associated with each NPI in Part B carrier claims. We then assigned each NPI to a primary TIN, defined as the TIN associated with the most allowed charges by that NPI in Part B claims. For each TIN and provider group in the AMA Group Practice File, we then counted the number of assigned or linked NPIs in each HCFA physician specialty category. From these counts, we calculated for each provider group the fraction of all physicians who had primary care specialties (HCFA specialty codes 01, 08, 11, 38).
D. Adjustment for Outpatient Facility Fees
Hospital-based physicians routinely charge facility fees for office visits and outpatient procedures that increase total reimbursements by amounts not directly specified in Medicare claims. They are able do so even if their practice is not located on a hospital campus, as long as they are employed by a hospital. These outpatient facility fees are paid by Medicare to hospital outpatient departments and contribute to payment amounts in the hospital outpatient department claims file rather than to payment amounts in the carrier (Part B physician/supplier claims) file. For hospital-based physicians who charge facility fees, Medicare pays reduced fees for the physicians’ services, and these reduced payments appear in the carrier file. For a given service, the combined outpatient facility fee and physician fees typically exceed the total allowed charges that would appear in the carrier file alone for a non-hospital-based physician.
Although we adjusted analyses for geographic variation in Medicare fees, spending on outpatient care may have differed between hospital-based and non-hospital-based providers in the same county because of these facility fees. Therefore, we calculated price-adjusted spending on outpatient care as follows. For each Healthcare Common Procedure Coding System (HCPCS) code appearing in the carrier and hospital outpatient department claims files, we determined the average allowed charge per service unit in the carrier file (a national standardized price). We then multiplied each claim by the corresponding HCPCS-specific standardized price. For each beneficiary, we identified claims with the same HCPCS code and similar dates appearing in both the carrier and outpatient files, and excluded these duplicative claims from the outpatient file (i.e. services for which a facility fee was presumably charged, contributing to practice fees in the outpatient file in addition to physician fees in the carrier file).
For each beneficiary, we then summed the price-adjusted amounts across all remaining claims in the carrier and hospital outpatient department files for services that occurred in outpatient settings (using place of service codes to distinguish outpatient from inpatient services in the carrier file). These price-adjusted amounts were lower than unadjusted amounts for two reasons. First, the standardization method removed charges attributable to hospital-based providers billing separately for the facility and physician fees (i.e. the method removed the outpatient facility fees as intended). Second, the standardized price for a given service was the average of A) the full allowed charge for both practice expense and professional components by non-hospital-based providers and B) the reduced charge for the professional component only by hospital-based providers. Thus, the standardized prices were lower than actual total payments minus the outpatient facility fee, particularly for services disproportionately provided by hospital-based providers charging outpatient facility fees. As a result, the method may have constituted an over-adjustment for facility fees.
We then compared differences in spending on outpatient care between hospital-based groups and the reference category of small groups before and after this adjustment. We conducted these comparisons as a sensitivity analysis, because we had access to outpatient claims only for a 5% sample of beneficiaries in 2009 (a subset of the 20% sample of beneficiaries). We had access to both carrier claims and the beneficiary annual summary file, which contains total spending amounts by type of service, for the 20% sample of beneficiaries analyzed in our main comparisons.
Before adjustment, per-beneficiary spending on outpatient care was $330 higher for hospital-based groups (mean: $5,306) than for small groups (mean: $4,976). After adjustment, this difference was reduced by $39 to $291 (price-adjusted means: $4,421 for hospital-based groups vs. $4,130 for small groups). Some of this reduction in the absolute spending difference may have been due to lower standardized prices applied to services as explained above. Thus, as a conservative estimate, outpatient facility fees explained at most 4.6% of the difference in total per-beneficiary spending ($849) between hospital-based and small groups.
E. Strength of Affiliation with Academic Teaching Hospitals
We used IME spending for hospitalized beneficiaries to measure the strength of provider group affiliations with academic teaching hospitals. Specifically, for each provider group category, we determined the percentage of hospitalized beneficiaries for whom IME spending was nonzero and thus suggestive of admission to a teaching hospital. As expected, this percentage was higher for hospitalized beneficiaries assigned to larger hospital-based groups than for those assigned to small groups (+8.1 percentage points), but this percentage was also higher for hospitalized beneficiaries assigned to larger independent groups (+4.1 for medium-sized and +4.6 for large groups). Mean IME spending for hospitalized beneficiaries followed a similar pattern across provider group types. Thus, stronger affiliations with teaching hospitals were not consistently correlated with total spending, which was much higher for larger hospital based groups but slightly lower for larger independent groups, relative to small groups (Table 3). In addition, compared with small physician groups, total per-beneficiary spending was substantially higher for small hospital-based groups (+$1024; P<0.001) but IME spending for hospitalized beneficiaries was nearly equivalent for small independent and hospital-based groups. We omitted results for the relatively small group of beneficiaries assigned to small hospital-based groups for parsimony, but they are notable in this context because they further suggest that stronger affiliations with teaching hospitals did not explain higher spending for beneficiaries served by hospital-based groups. Thus, strength of affiliation with teaching hospitals did not provide a consistent explanation for spending differences among provider group types.
Footnotes
Financial disclosures: The authors have no potential financial conflicts of interest to disclose.
Author contributions: see authorship forms. Dr. McWilliams and Mr. Hamed had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Financial disclosures: The authors have no potential conflicts of interest to disclose.
References
- 1.Center for Medicare and Medicaid Innovation. [Accessed March 6, 2013];Pioneer ACO Alignment and Financial Reconciliation Methods. 2011 http://innovations.cms.gov/Files/x/Pioneer-ACO-Model-Benchmark-Methodology-document.pdf.
- 2.Department of Health and Human Services and Centers for Medicare and Medicaid Services. Medicare program; Medicare Shared Savings Program: accountable care organizations. [Accessed March 6, 2013];Final rule. 2011 http://www.gpo.gov/fdsys/pkg/FR-2011-11-02/pdf/2011-27461.pdf.
- 3.Crosson FJ. Medicare: the place to start delivery system reform. Health Aff (Millwood) 2009;28:w232–234. doi: 10.1377/hlthaff.28.2.w232. [DOI] [PubMed] [Google Scholar]
- 4.Fisher ES, McClellan MB, Bertko J, et al. Fostering accountable health care: moving forward in Medicare. Health Aff (Millwood) 2009;28:w219–231. doi: 10.1377/hlthaff.28.2.w219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Robinson JC, Casalino LP. Vertical integration and organizational networks in health care. Health Aff (Millwood) 1996;15:7–22. doi: 10.1377/hlthaff.15.1.7. [DOI] [PubMed] [Google Scholar]
- 6.Medicare Payment Advisory Commission. [Accessed January 25, 2013];Report to the Congress: improving incentives in the Medicare program. 2009 http://www.medpac.gov/documents/jun09_entirereport.pdf.
- 7.Crosson FJ. 21st-century health care--the case for integrated delivery systems. N Engl J Med. 2009;361:1324–1325. doi: 10.1056/NEJMp0906917. [DOI] [PubMed] [Google Scholar]
- 8.Berenson RA, Bodenheimer T, Pham HH. Specialty-service lines: salvos in the new medical arms race. Health Aff (Millwood) 2006;25:w337–343. doi: 10.1377/hlthaff.25.w337. [DOI] [PubMed] [Google Scholar]
- 9.Robinson JC. More evidence of the association between hospital market concentration and higher prices and profits. National Institute for Health Care Management; 2011. [Accessed March 6, 2013]. http://nihcm.org/images/stories/NIHCM-EV-Robinson-Final.pdf. [Google Scholar]
- 10.Casalino LP, Pham H, Bazzoli G. Growth of single-specialty medical groups. Health Aff (Millwood) 2004;23:82–90. doi: 10.1377/hlthaff.23.2.82. [DOI] [PubMed] [Google Scholar]
- 11.Liebhaber A, Grossman JM. Physicians moving to mid-sized, single-specialty practices. Center for Studying Health System Change; 2007. Tracking report No. 18. [PubMed] [Google Scholar]
- 12.O’Malley AS, Bond AM, Berenson RA. Rising hospital employment of physicians: better quality and costs? Center for Studying Health System Change; 2011. Issue Brief No.136. [PubMed] [Google Scholar]
- 13.Robinson JC. Hospital market concentration, pricing, and profitability in orthopedic surgery and interventional cardiology. Am J Manag Care. 2011;17(6 Spec No):e241–248. [PubMed] [Google Scholar]
- 14.Wennberg JE, Fisher ES, Skinner JS. Geography and the debate over Medicare reform. Health Aff (Millwood) 2002;(Suppl Web Exclusives):W96–114. doi: 10.1377/hlthaff.w2.96. [DOI] [PubMed] [Google Scholar]
- 15.Kocher R, Sahni NR. Hospitals’ race to employ physicians--the logic behind a money-losing proposition. N Engl J Med. 2011;364(19):1790–1793. doi: 10.1056/NEJMp1101959. [DOI] [PubMed] [Google Scholar]
- 16.Rittenhouse DR, Casalino LP, Gillies RR, Shortell SM, Lau B. Measuring the medical home infrastructure in large medical groups. Health Aff (Millwood) 2008;27:1246–1258. doi: 10.1377/hlthaff.27.5.1246. [DOI] [PubMed] [Google Scholar]
- 17.Rittenhouse DR, Casalino LP, Shortell SM, et al. Small And medium-size physician practices use few patient-centered medical home processes. Health Aff (Millwood) 2011;30(8):1575–1584. doi: 10.1377/hlthaff.2010.1210. [DOI] [PubMed] [Google Scholar]
- 18.Rittenhouse DR, Shortell SM, Gillies RR, et al. Improving chronic illness care: findings from a national study of care management processes in large physician practices. Med Care Res Rev. 2010;67(3):301–320. doi: 10.1177/1077558709353324. [DOI] [PubMed] [Google Scholar]
- 19.Casalino L, Gillies RR, Shortell SM, et al. External incentives, information technology, and organized processes to improve health care quality for patients with chronic diseases. JAMA. 2003;289:434–441. doi: 10.1001/jama.289.4.434. [DOI] [PubMed] [Google Scholar]
- 20.Friedberg MW, Safran DG, Coltin KL, Dresser M, Schneider EC. Readiness for the Patient-Centered Medical Home: structural capabilities of Massachusetts primary care practices. J Gen Intern Med. 2009;24:162–169. doi: 10.1007/s11606-008-0856-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Burt CW, Sisk JE. Which physicians and practices are using electronic medical records? Health Aff (Millwood) 2005;24(5):1334–1343. doi: 10.1377/hlthaff.24.5.1334. [DOI] [PubMed] [Google Scholar]
- 22.Burns LR, Muller RW. Hospital-physician collaboration: landscape of economic integration and impact on clinical integration. Milbank Q. 2008;86(3):375–434. doi: 10.1111/j.1468-0009.2008.00527.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cuellar AE, Gertler PJ. Strategic integration of hospitals and physicians. J Health Econ. 2006;25(1):1–28. doi: 10.1016/j.jhealeco.2005.04.009. [DOI] [PubMed] [Google Scholar]
- 24.Gaynor M, Town R. The Synthesis Project. Robert Wood Johnson Foundation; 2012. [Accessed March 6, 2013]. The impact of hospital consolidation - update. http://www.rwjf.org/files/research/5973.74582.synthesisprojectupdate.hospitalconsolidation.pdf. [Google Scholar]
- 25.Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457–502. doi: 10.1111/j.1468-0009.2005.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Baicker K, Chandra A. Medicare spending, the physician workforce, and beneficiaries’ quality of care. Health Aff (Millwood) 2004;(Suppl Web Exclusives):W4–184–197. doi: 10.1377/hlthaff.w4.184. [DOI] [PubMed] [Google Scholar]
- 27.Chang C-H, Stukel TA, Flood AB, Goodman DC. Primary care physician workforce and Medicare beneficiaries’ health outcomes. JAMA. 2011;305(20):2096–2104. doi: 10.1001/jama.2011.665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rittenhouse DR, Shortell SM, Fisher ES. Primary care and accountable care -- two essential elements of delivery-system reform. N Engl J Med. 2009;361:2301–2303. doi: 10.1056/NEJMp0909327. [DOI] [PubMed] [Google Scholar]
- 29.Fisher ES. Building a medical neighborhood for the medical home. N Engl J Med. 2008;359:1202–1205. doi: 10.1056/NEJMp0806233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Casalino LP. Which type of medical group provides higher-quality care? Ann Intern Med. 2006;145(11):860–861. doi: 10.7326/0003-4819-145-11-200612050-00012. [DOI] [PubMed] [Google Scholar]
- 31.Friedberg MW, Coltin KL, Safran DG, Dresser M, Zaslavsky AM, Schneider EC. Associations between structural capabilities of primary care practices and performance on selected quality measures. Ann Intern Med. 2009;151:456–463. doi: 10.7326/0003-4819-151-7-200910060-00006. [DOI] [PubMed] [Google Scholar]
- 32.Yun H, Kilgore ML, Curtis JR, et al. Identifying types of nursing facility stays using Medicare claims data: an algorithm and validation. Health Serv Outcomes Res Method. 2010;10:100–110. [Google Scholar]
- 33.United States Department of Agriculture Economic Research Service. [Accessed March 6, 2013];Rural-Urban Continuum Codes. http://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx.
- 34.HealthLeaders InterStudy. [Accessed March 6, 2013];Health Plan Data & Analysis. http://hl-isy.com/hpda.
- 35.Robinson JC, Shortell SM, Li R, Casalino LP, Rundall T. The alignment and blending of payment incentives within physician organizations. Health Serv Res. 2004;39(5):1589–1606. doi: 10.1111/j.1475-6773.2004.00305.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zuvekas SH, Cohen JW. Paying physicians by capitation: is the past now prologue? Health Aff (Millwood) 2010;29(9):1661–1666. doi: 10.1377/hlthaff.2009.0361. [DOI] [PubMed] [Google Scholar]
- 37.Baker LC. The effect of HMOs on fee-for-service health care expenditures: evidence from Medicare. J Health Econ. 1997;16(4):453–481. doi: 10.1016/s0167-6296(96)00535-8. [DOI] [PubMed] [Google Scholar]
- 38.Baker LC. Association of managed care market share and health expenditures for fee-for-service Medicare patients. JAMA. 1999;281(5):432–437. doi: 10.1001/jama.281.5.432. [DOI] [PubMed] [Google Scholar]
- 39.Landon BE, Reschovsky JD, O’Malley AJ, Pham HH, Hadley J. The Relationship between physician compensation strategies and the intensity of care delivered to Medicare beneficiaries. Health Serv Res. 2011;46(6pt1):1863–1882. doi: 10.1111/j.1475-6773.2011.01294.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Devers KJ, Brewster LR, Casalino LP. Changes in hospital competitive strategy: a new medical arms race? Health Serv Res. 2003;38:447–469. doi: 10.1111/1475-6773.00124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Devers KJ, Casalino LP, Rudell LS, Stoddard JJ, Brewster LR, Lake TK. Hospitals’ negotiating leverage with health plans: how and why has it changed? Health Serv Res. 2003;38(1 Pt 2):419–446. doi: 10.1111/1475-6773.00123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lake T, Devers K, Brewster L, Casalino L. Something old, something new: recent developments in hospital-physician relationships. Health Serv Res. 2003;38(1 Pt 2):471–488. doi: 10.1111/1475-6773.00125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Casalino L, Robinson JC. Alternative models of hospital-physician affiliation as the United States moves away from tight managed care. Milbank Q. 2003;81(2):331–351. 173–334. doi: 10.1111/1468-0009.t01-2-00056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vogt WB. Hospital market consolidation: trends and consequences. National Institute for Health Care Management; 2009. [Accessed March 6, 2013]. http://nihcm.org/pdf/EV-Vogt_FINAL.pdf. [Google Scholar]
- 45.Berenson RA, Ginsburg PB, Kemper N. Unchecked provider clout in California foreshadows challenges to health reform. Health Aff (Millwood) 2010;29(4):699–705. doi: 10.1377/hlthaff.2009.0715. [DOI] [PubMed] [Google Scholar]
- 46.U.S. Census Bureau. [Accessed March 6, 2013];American Community Survey 5-year estimates. 2010 http://factfinder2.census.gov/faces/nav/jsf/pages/searchresults.xhtml?refresh=t.
- 47.Centers for Medicare and Medicaid Services Chronic Condition Data Warehouse. [Accessed March 6, 2013]; http://www.ccwdata.org/index.htm.
- 48.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 2: health outcomes and satisfaction with care. Ann Intern Med. 2003;138:288–298. doi: 10.7326/0003-4819-138-4-200302180-00007. [DOI] [PubMed] [Google Scholar]
- 49.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care. Ann Intern Med. 2003;138:273–287. doi: 10.7326/0003-4819-138-4-200302180-00006. [DOI] [PubMed] [Google Scholar]
- 50.Song Y, Skinner J, Bynum J, Sutherland J, Wennberg JE, Fisher ES. Regional variations in diagnostic practices. N Engl J Med. 2010;363(1):45–53. doi: 10.1056/NEJMsa0910881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sirovich B, Gallagher PM, Wennberg DE, Fisher ES. Discretionary decision making by primary care physicians and the cost of U.S. Health care. Health Aff (Millwood) 2008;27:813–823. doi: 10.1377/hlthaff.27.3.813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Madison K. Hospital-physician affiliations and patient treatments, expenditures, and outcomes. Health Serv Res. 2004;39(2):257–278. doi: 10.1111/j.1475-6773.2004.00227.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.National Committee for Quality Assurance Patient-Centered Medical Home Recognition Program. [Accessed March 6, 2013]; http://www.ncqa.org/tabid/631/Default.aspx.
- 54.Comprehensive Primary Care Initiative. Center for Medicare and Medicaid Innovation; [Accessed March 6, 2013]. http://www.innovations.cms.gov/initiatives/Comprehensive-Primary-Care-Initiative/index.html. [Google Scholar]
- 55.Song Z, Safran DG, Landon BE, et al. Health care spending and quality in year 1 of the alternative quality contract. N Engl J Med. 2011;365(10):909–918. doi: 10.1056/NEJMsa1101416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Song Z, Safran DG, Landon BE, et al. The ‘Alternative Quality Contract,’ based on a global budget, lowered Medical spending and improved quality. Health Aff (Millwood) 2012;31(8):1885–1894. doi: 10.1377/hlthaff.2012.0327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Weeks WB, Gottlieb DJ, Nyweide DJ, et al. Higher health care quality and bigger savings found at large multispecialty medical groups. Health Aff (Millwood) 2010;29(5):991–997. doi: 10.1377/hlthaff.2009.0388. [DOI] [PubMed] [Google Scholar]
- 58.Dunn A, Shapiro AH. Working paper 2012-6. Bureau of Economic Analysis; 2012. [Accessed March 6, 2013]. Physician market power and medical-care expenditures. http://www.bea.gov/papers/pdf/Physician_Market_Power_and_Medical_Care.pdf. [Google Scholar]
References
- 1.McWilliams JM, Chernew ME, Zaslavsky AM, Landon BE. Post-acute care -- who will be accountable? Health Serv Res. 2013 doi: 10.1111/1475-6773.12032. published in advance online. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.