Sir,
The first description of lipedema was in 1940 by Allen and Hines, who defined it as an abnormal deposit of adipose tissue in the lower limbs with the involvement of the feet that affects women with a family history of the disease.[1] Some characteristics of this physical condition are deposition of excess fat on the legs (described classically as an “Egyptian column” shape) and arms with a negative stemmer sign.[2]
A histological analysis of the tissue shows proliferation of progenitor cells derived from adipose tissue and an increase in adipogenesis leading to necrosis of adipocytes and hypoxia.[3] Studies evaluating changes in the lymphatic system in lipedema showed that lymphatic vessels are dilated in lipolymphedema and have obstructive features with dermal reflux and in lipedema the vessels are dilated but without signs of reflux.[4]
Cellulite is characterized by an accumulation of fluids in the cell interstice with progression in subsequent phases that suggests an increase in the concentrations of substances in this space, resulting in local reactions to these substances and an increased difficultly to exchange particles between the cell and the interstice.[5] The aim of this study was to demonstrate reductions in perimetric measurements in patients with lipedema and cellulite.
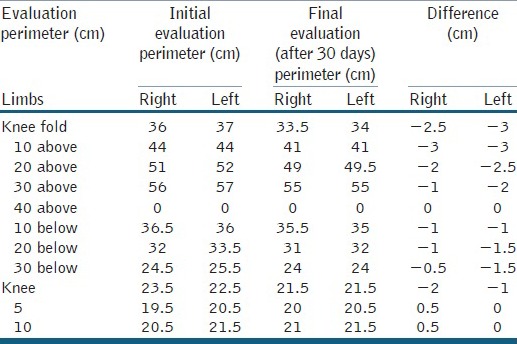
The case of a 31-year-old female patient, with a family history of “fat legs”, is reported. The patient complained of swelling in the lower limbs in the evening and at night since her adolescence, which worsened with the appearance of cellulite in the thigh region causing functional limitations due to pain. These symptoms worsened during the menstrual period. Lipedema of the lower limbs and grade III cellulite were diagnosed in the physical examination. A program was designed to treat the cellulite that included: Godoy and Godoy manual lymph drainage technique and mechanical lymph drainage device (Godoy) that performs passive flexion and extension of the tibiotarsal joint– for 1 h/day for 10 days over 2 weeks. A perimetric evaluation was performed at 10 cm intervals along the abdomen and legs. The patient presented perimetric reductions of up to 4 cm around the abdomen, 3 cm around the thigh and 1.5 cm below the knee [Tables 1 and 2].
Table 1.
Perimetric evaluation of the abdomen and hips
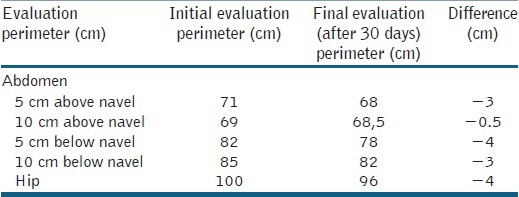
Table 2.
Perimetric evaluation of the legs
This study demonstrates that esthetic cellulite constitutes an aggravating factor in the perimetry of the legs and abdomen in patients with lipedema and indicates a new approach to reduce these dimensions in lipedema. As far as we know there are no published studies describing this approach. The treatment of any disease should consider the pathophysiological mechanisms responsible for its development. As a pathophysiology hypothesis, Godoy proposed that the lymphatic system is involved in the evolution of cellulite leading to regional lymphostasis.[6] A physical examination of patients strongly suggests this mechanism is part of the hypothesis.[5]
In respect to lipedema, the main aggravating factors are the necrosis of fat cells[3] and changes in the lymphatic system.[4] Therefore, similar aggravating pathophysiological mechanisms are seen both in lipedema and cellulite. Hence cellulite may constitute an aggravating factor for increases the perimetry of the legs and abdomen of patients with lipedema, with stimulation of the lymphatic system being indicated in treatment.
This approach, which takes into account pathophysiological mechanisms, offers new possibilities in the treatment of lipedema.
REFERENCES
- 1.Allen EV, Hines EA. Lipedema of the legs: A syndrome characterized by fat legs and orthostatic edema. Mayo Clin Proc. 1940;15:184–7. [Google Scholar]
- 2.Pereira De Godoy JM, De Moura Álvares R, Simon Torati JL, De Fátima Guerreiro Godoy M. Clinical aspects of advanced stage lipo-lymphedema: Case report. G Ital Dermatol Venereol. 2010;145:547–9. [PubMed] [Google Scholar]
- 3.Suga H, Araki J, Aoi N, Kato H, Higashino T, Yoshimura K. Adipose tissue remodeling in lipedema: Adipocyte death and concurrent regeneration. J Cutan Pathol. 2009;36:1293–8. doi: 10.1111/j.1600-0560.2009.01256.x. [DOI] [PubMed] [Google Scholar]
- 4.Lohrmann C, Foeldi E, Langer M. MR imaging of the lymphatic system in patients with lipedema and lipo-lymphedema. Microvasc Res. 2009;77:335–9. doi: 10.1016/j.mvr.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 5.de Godoy JM, de Godoy Mde F. Treatment of cellulite based on the hypothesis of a novel physiopathology. Clin Cosmet Investig Dermatol. 2011;4:55–9. doi: 10.2147/CCID.S20363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Godoy JM, de Godoy Mde F. Physiopathological hypothesis of cellulite. Open Cardiovasc Med J. 2009;3:96–7. doi: 10.2174/1874192400903010096. [DOI] [PMC free article] [PubMed] [Google Scholar]


