INTRODUCTION
Proximal femoral fractures (PFF) are common, with annual incidence in the UK of approximately 70,000 with a projected incidence of 91,500/year by 2015.[1] The majority occur in the elderly population.[1]
Mortality from PFF is high. Approximately, 10% of patients die within 1 month and about one third die within 1 year.[1] Early surgical fracture fixation (SFF) and prompt rehabilitation are paramount. Studies have shown that length of hospital stay, morbidity and mortality are directly related to time to SFF.[2,3]
The current UK expenditure for medical and social care for all hip fractures amounts to approximately 2 billion GBP.[1] In April 2010, the best practice tariff (BPT) for fragility hip fractures was introduced. This highlighted the need for early SFF and financially rewards National Health Service hospital trusts with uplift to the tariff price. There are six criteria that have to be satisfied to receive an uplifted tariff price and early SFF is one of these criteria. The BPT sets the standard of time to surgery (TTS) within 36 h from arrival in the emergency department or time of diagnosis if an inpatient, to the start of anaesthesia. If a Trust meets all the criteria they will receive an extra 890 GBP/patient.[4] Prior to the introduction of the BPT, the British Orthopaedic Association had published a Standard for Trauma (BOAST 1) and recommended that TTS should not be greater than 48 h from admission, unless there are clear reversible medical conditions.[5]
Patients with PFF commonly have comorbidity that affects peri-operative management. Whilst TTS of less than 36-48 h is the goal, it has to be timed with any pre-operative optimisation of the patient.
Pre-operative echocardiogram (POE) is a valuable imaging modality for assessing a patient's intravascular volume status, myocardial contractility/ventricular ejection fraction and valvular heart disease in the peri-operative period.[6,7] The aim of this audit was to assess if POE in patients with PFF presenting to our institution resulted in a delay to TTS beyond 48 h.
METHODOLOGY
A retrospective audit was performed at the Princess Royal Hospital in Telford, UK.
The hospital clinical coding system was searched for patients that received treatment for a PFF between 1st January 2009 and 31st December 2009. Further data searches were performed from theatre records and clinical notes. Patients that did not have surgical treatment for their PFF were excluded from the study.
From this dataset, patients who underwent POE were identified. The following details were recorded; time to echocardiogram (TTE) and TTS.
RESULTS
A total of 228 patients were admitted with PFF and underwent SFF during the study period. Of this group, 13 patients were investigated with POE.
Table 1 shows the TTE. The results show that 10 out of 13 patients who received a POE (76.9%) had to wait more than 48 h for their POE. This led to a breach in the BOAST 1 guideline.
Table 1.
Time to echocardiogram
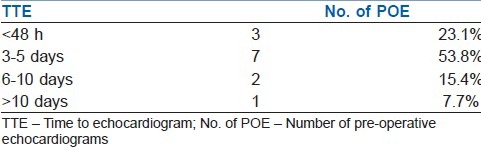
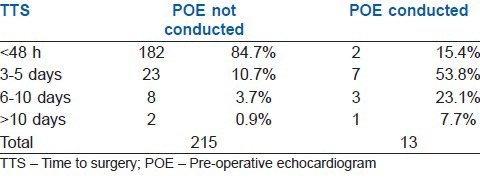
Table 2 shows the TTS for patients who underwent POE and in those who did not. 84.7% of patients that did not undergo POE had TTS within 48 h in accordance with the BOAST 1 guideline. In comparison, only 15.4% of patients that did undergo POE had TTS within 48 h. 15.3% of patients who did not undergo POE had a delay resulting in a TTS greater than 48 h, whereas 84.6% of patients who did undergo POE had a delay resulting in a TTS greater than 48 h.
Table 2.
Time to surgery
DISCUSSION
The results demonstrate that TTS were significantly longer in those patients who were investigated with POE. 84.6% of patients who underwent POE had a TTS greater than 48 h. In comparison, only 15.3% of patients who did not undergo a POE had a TTS greater than 48 h.
It has been shown that a delay in SFF of PFF results in increased hospital stay, morbidity and mortality.[2,3] This patient group frequently also have existing comorbid conditions and it is essential to ensure that these patients have been appropriately investigated and optimised prior to surgery. However, the potential delay that investigations may cause needs to be considered against the significant weight of evidence that supports early SFF. The role of POE in this patient group is not the aim of this study, but this study shows that requesting POE in patients with PFF resulted in a delay in TTS that breached national guidelines in our institution in a high income country.
If we are to meet national treatment targets, then appropriately requested POE needs to be sufficiently resourced to prevent any delay in TTS that can adversely impact upon patient outcome.
We are also aware that some of our colleagues in anaesthesia are performing focused POE in an attempt to obtain specific information that can influence peri-operative management whilst reaching a TTS within 48 h and our audit supports this development.
Limitations
We accept that changes have now have occurred such that this audit may not be applicable today in all health-care institutions within the UK health-care system.
We also accept that we cannot state that POE is the sole reason for delay in SFF as there may be other reasons for the delay in SFF that our data collection method did not capture.
CONCLUSIONS
We conclude that during our study period and at our institution, the use of POE in patients with PFF was associated with a delay in SFF that breached national targets and that this association is worthy of further audit and study.
REFERENCES
- 1.National Institute for Health and Clinical Excellence. London: NICE; 2011. Hip fracture: the management of hip fracture in adults; pp. 4–27. [Google Scholar]
- 2.Shiga T, Wajima Z, Ohe Y. Is operative delay associated with increased mortality of hip fracture patients? Systematic review, meta-analysis, and meta-regression. Can J Anaesth. 2008;55:146–54. doi: 10.1007/BF03016088. [DOI] [PubMed] [Google Scholar]
- 3.Bryson GL. Waiting for hip fracture repair-do outcomes and patients suffer? Can J Anaesth. 2008;55:135–9. doi: 10.1007/BF03016086. [DOI] [PubMed] [Google Scholar]
- 4.National Institute for Health and Clinical Excellence, The Management of Hip Fracture in Adults, National Institute for Health and Clinical Excellence. 2011. http://www.nice.org.uk/cg124 .
- 5.British Orthopaedic Association Standards for Trauma (BOAST) 1. Hip Fracture in the Older Person. British Orthopaedic Association. 2008. http://www.boa.ac.uk/LIB/LIBPUB/Documents/BOAST%201%20-%20Hip%20Fracture%20in%20the%20Older%20Person%20Version%201%20-%202008.pdf . [DOI] [PubMed]
- 6.Griffiths R, Alper J, Beckingsale A, Goldhill D, Heyburn G, et al. Anaesthesia. Vol. 67. Association of Anaesthetists of Great Britain and Ireland; 2012. Management of proximal femoral fractures 2011: Association of Anaesthetists of Great Britain and Ireland; pp. 85–98. [DOI] [PubMed] [Google Scholar]
- 7.Kearns RJ, Moss L, Kinsella J. A comparison of clinical practice guidelines for proximal femoral fracture. Anaesthesia. 2013;68:159–66. doi: 10.1111/anae.12076. [DOI] [PubMed] [Google Scholar]


