Abstract
Introduction:
Mandibular anterior region is an uncommon site for occurrence of intrabony pathologies. Unilocular presentation of a lesion is again less common than multilocular appearance. Demographically, most lesions occur in middle to elderly age group. The study is designed to review the pathologies manifesting a combination of these rare demographic and radiological criteria.
Materials and Methods:
A retrospective analysis of patients with anterior unilocular radiolucencies of mandible in young patients was done. Records of past 10 years were searched. There were a total of 17 patients. Their clinical history and radiographs were reviewed from the case files and correlated with histopathological examination of the lesion.
Results:
Nine different pathologies constituted the sample size of 17. A wide array of lesions was found to manifest similar signs and symptoms and radiographic findings namely ameloblastoma (three), adenomatoid odontogenic tumor (AOT, four), odontogenic keratocyst (OKC, three), ossifying fibroma (OF, two), idiopathic bone cavity (IBC, one), dentigerous cyst (DC, one), radicular cyst (RC, one), central giant cell granuloma (CGCG, one), and calcifying odontogenic cyst (COC, one).
Conclusion:
Anterior mandible is a rare site for occurrence of intrabony pathologies. Majority of patients are females. Lesions acquire large size before they are detected. Growth occurs more in length than in width. Root resorption is not uncommon and root displacement is almost a consistent feature.
Keywords: Benign tumor, cyst, impacted tooth, midline, orthopantomogram
INTRODUCTION
The basic principle behind diagnosing any lesion is to correlate the clinical and radiographic findings and establish a provisional diagnosis, followed by confirmatory histopathological examination. Radiographic interpretation for same lesion can be different and vice versa. Unilocular appearance usually represent unaggressive, slow growing, benign process. Concomitant radiographic findings are also of equal importance, viz. corticated/non-corticated borders, regular/irregular borders, root displacement, root resorption, mandibular canal displacement, and lingual cortex expansion. Aggressive benign or malignant lesions tend to favor irregular and non-corticated borders, lingual cortex expansion, resorption of adjacent tooth roots, and erosion of mandibular canal with resultant paresthesia. However, deviation from this anticipated picture is not rare. Aggressive lesions can appear unilocular at initial stage. Benign lesions in case of superimposed infection may assume aggressive characteristics.
Mandibular angle and posterior body region has been the most common site for occurrence of pathologies. As a result, less has been written about the common pathologies and their presentation in anterior mandibular region. Most of jaw pathologies occur in middle to elderly age group. However, our focus of study was to study the lesions occurring in young population. This study was designed to focus on an array of lesions presenting as anterior mandibular unilocular radiolucencies in young population, their presenting signs and symptoms, radiographic features, and prognosis.
MATERIALS AND METHODS
Records of the department in the past 10 years (2002-2011) were searched for young patients presenting with unilocular radiolucencies in anterior mandible. An orthopantomogram was used as a standard radiograph to evaluate the lesion as unilocular or multilocular. The clinical criteria documented were age, sex, extraoral swelling, expansion (both buccolingual and superoinferior), and pain. Radiographic criteria documented were impacted tooth, extent of radiolucency, shape and borders of radiolucency, root displacement, and resorption of adjacent teeth. Other steps in reaching final diagnosis viz. aspiration, incisional biopsy, surgical procedure based on primary microscopic examination and final histopathological diagnosis along with follow-up of the patient were also tabulated [Tables 1 and 2].
Table 1.
Review of cases
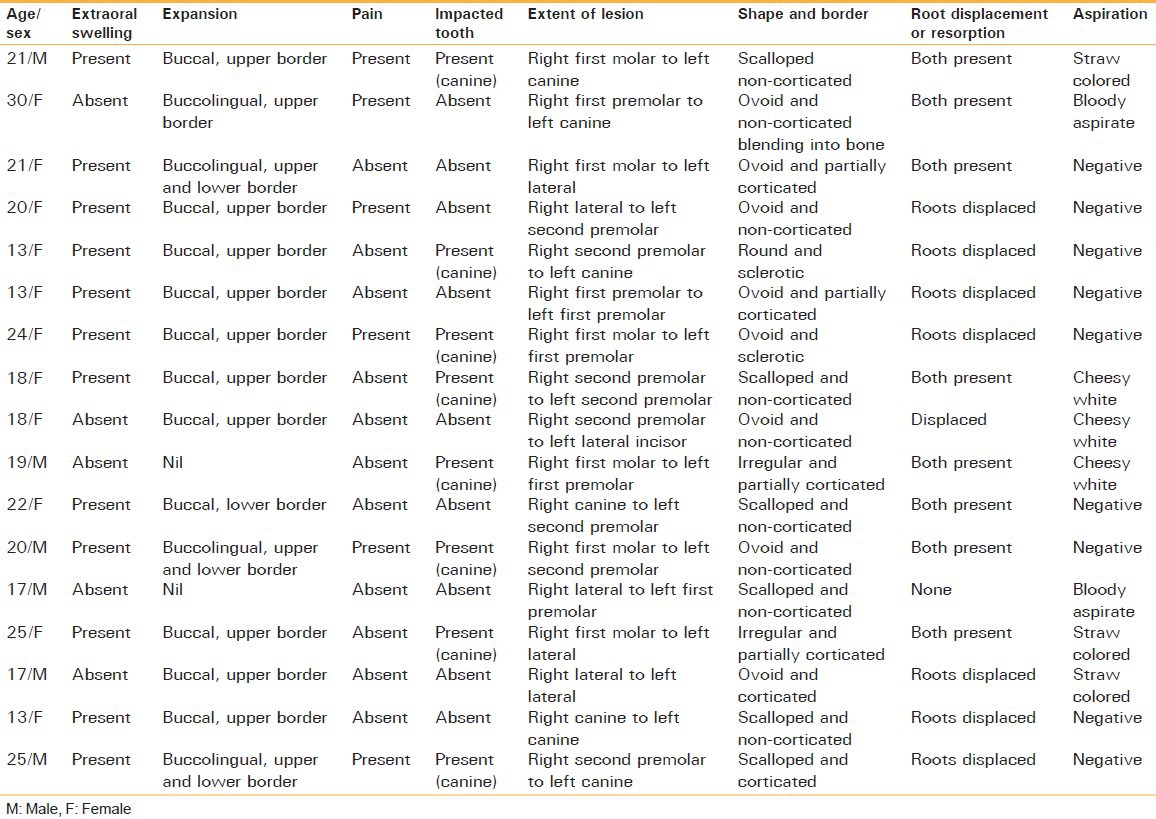
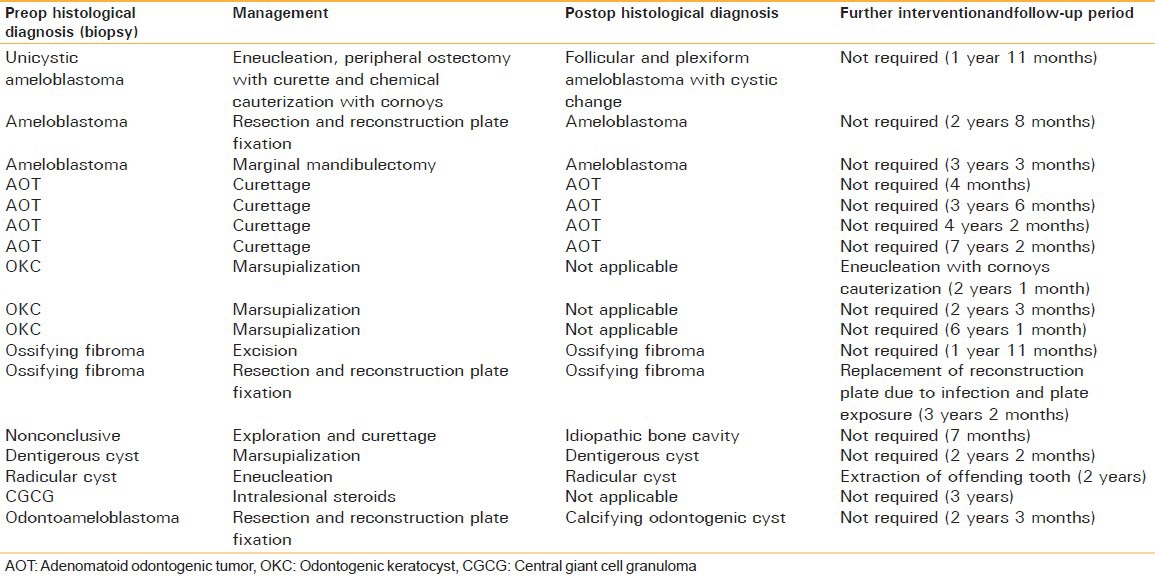
Table 2.
Diagnosis and management
RESULTS
A total of only 17 cases were found representing nine different pathologies. This was surprising compared to the number of patients treated for pathologies in our department. However, this is a subjective statement and we did not search and analyze the records of total number of patients operated for mandibular intrabony pathology. There were three cases of ameloblastoma (17.65%); four of adenomatoid odontogenic tumor (AOT) (23.53%); three of odontogenic keratocyst (OKC) (17.65%); two of ossifying fibroma (OF) (11.76%); one each of dentigerous cyst (DC) (5.88%), calcifying odontogenic cyst (COC) (5.88%), idiopathic bone cavity (IBC) (5.88%), radicular cyst (RC) (5.88%), and central giant cell granuloma (CGCG) (5.88%). The illustrations are numbered corresponding to the serial number of the cases in the tables [Figures 1-17]. Eleven out of 17 patients were females and14/17 patients presented with swelling. In 12 out of these 14 patients, swelling was perceptible extraorally and the other two presented with intraoral swelling. Out of the 12 patients, eight cases had only buccal expansion and the other four had both buccal and lingual expansion of the mandible. Two patients with intra-oral swelling exhibited only buccal expansion. Three out of four cases of buccolingual expansion involved full height of the mandible and one was restricted to upper border. Pain was present in six out of 17 cases. Only 4/17 cases had corticated borders in our series. Four cases showed partially corticated borders and the rest of nine cases had non-corticated borders. All four lesions with corticated borders had regular outline. Eight out of 13 cases of partially corticated or non-corticated borders showed irregular outline. Roots of adjacent teeth were displaced in 16 out of 17 cases and resorption of roots was seen in eight out of these 16 cases. Root resorption was seen in lesions causing significant root displacement and having non-corticated or partially corticated borders. Eight cases were associated with impacted tooth (47.06%), all of which were canines. The lesions involved minimum of four teeth and a maximum of 11 teeth with an average of 7.94 teeth per lesion.
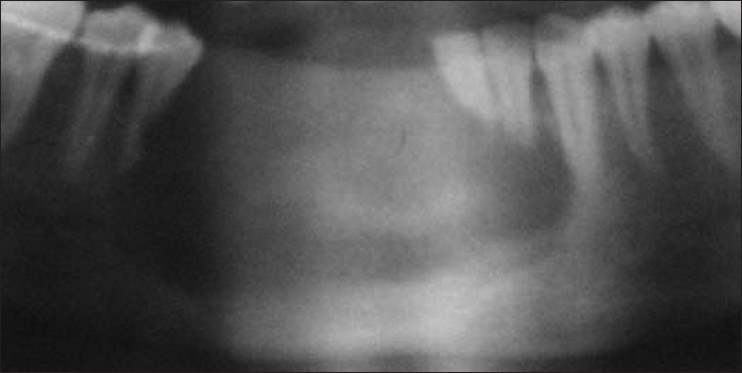
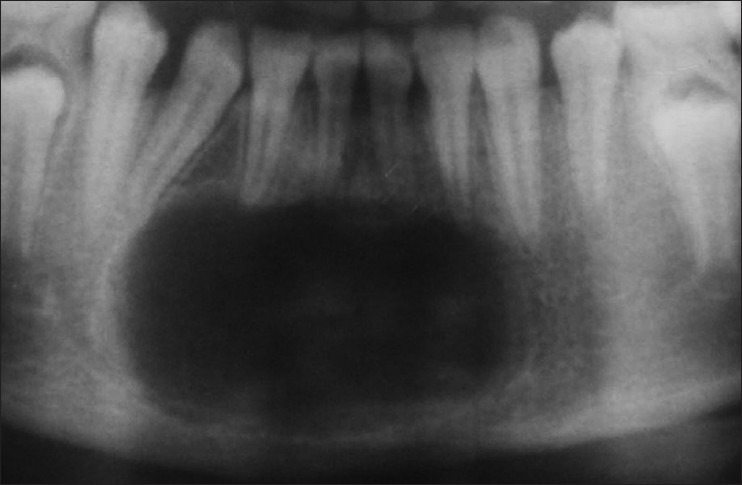
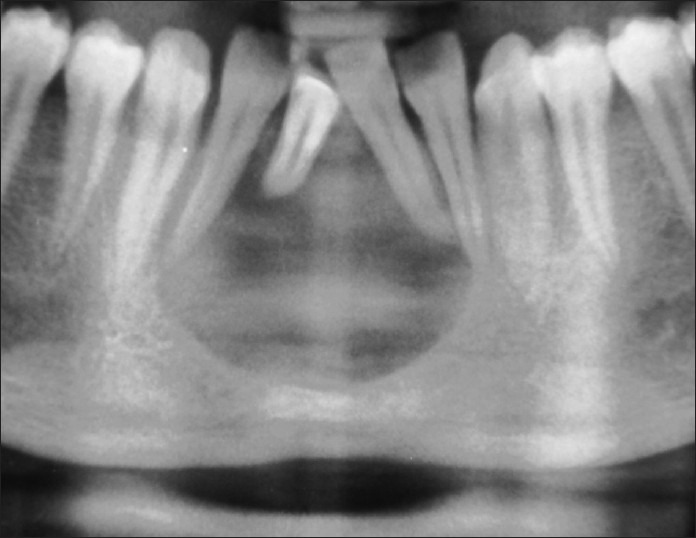
Figure 1.
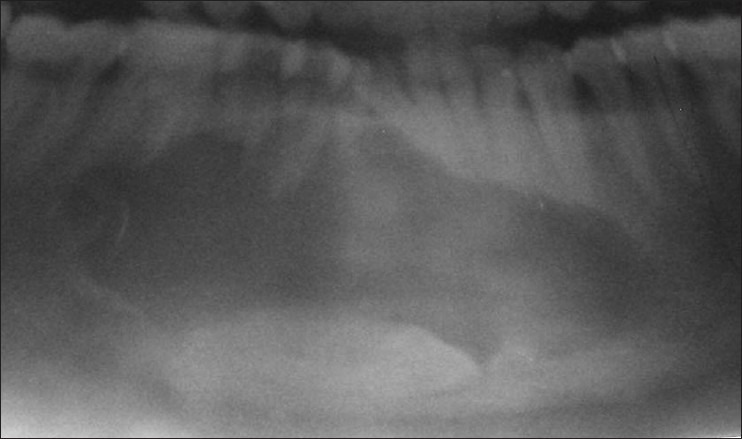
Case 1: Ameloblastoma
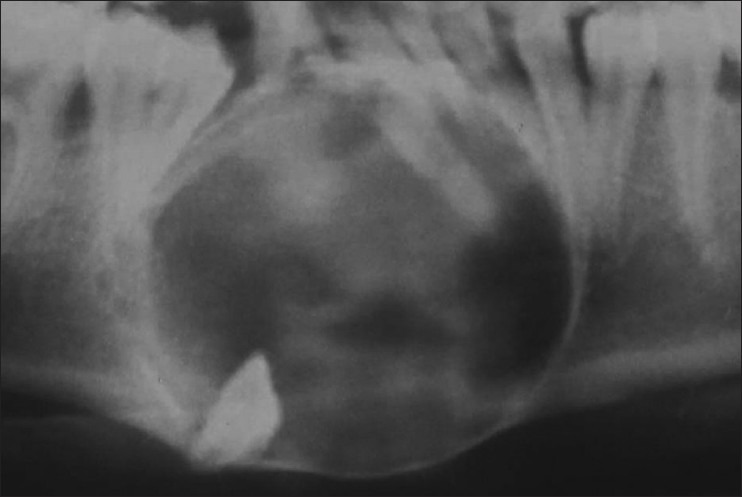
Figure 17.
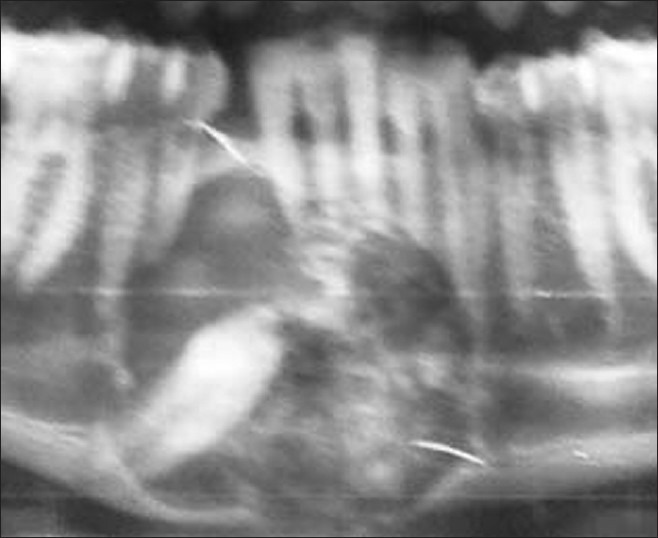
Case 17: Calcifying Odontogenic Cyst
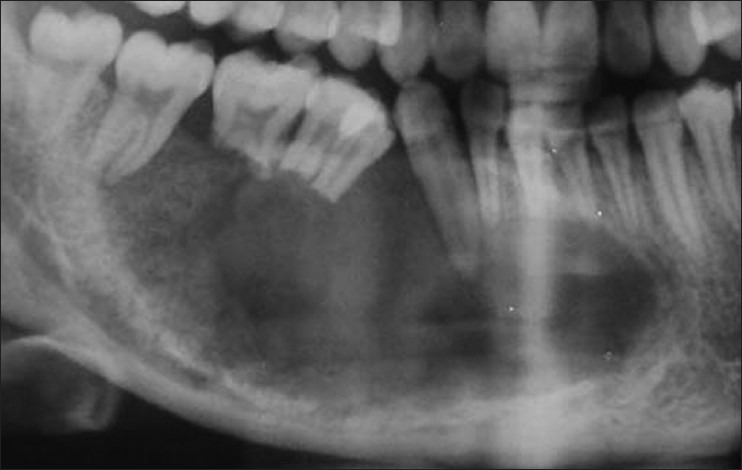
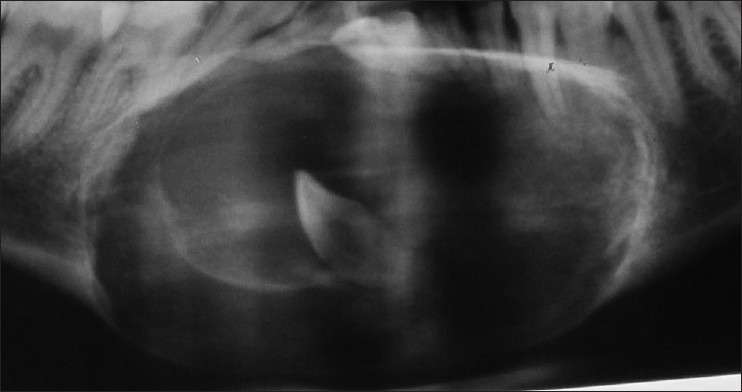
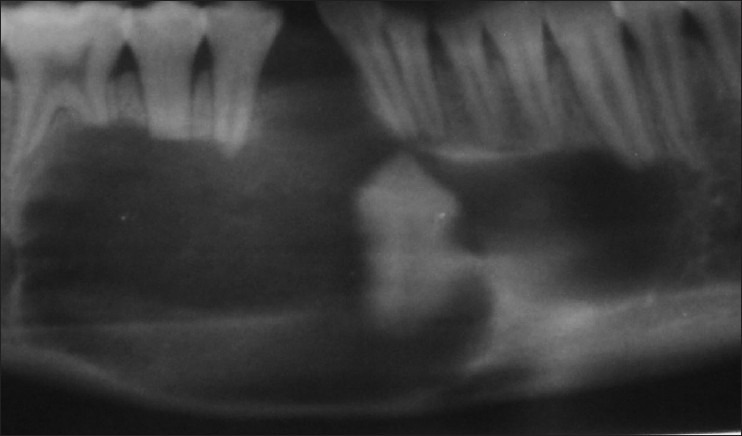
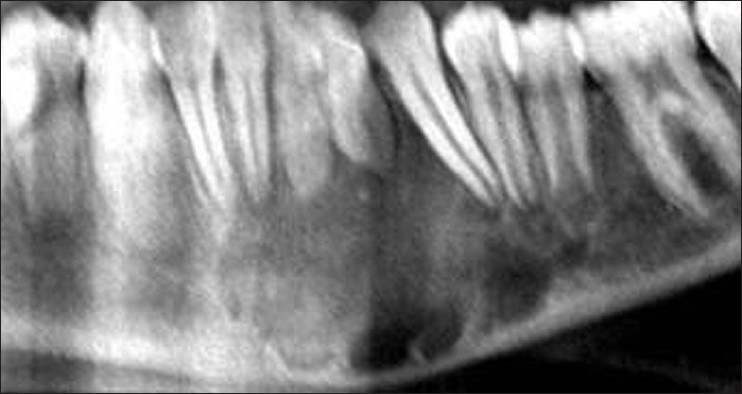
Figure 2.
Case 2: Ameloblastoma
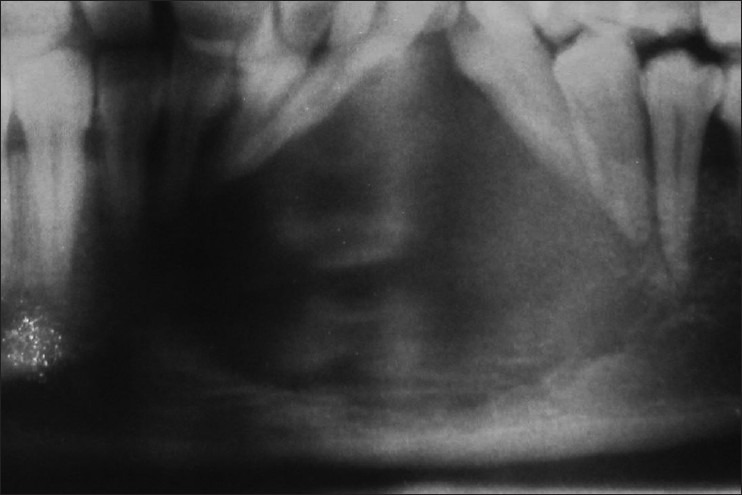
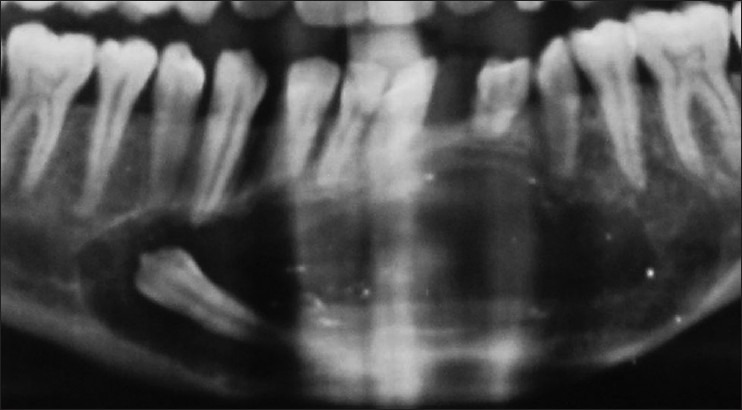
Figure 3.
Case 3: Ameloblastoma
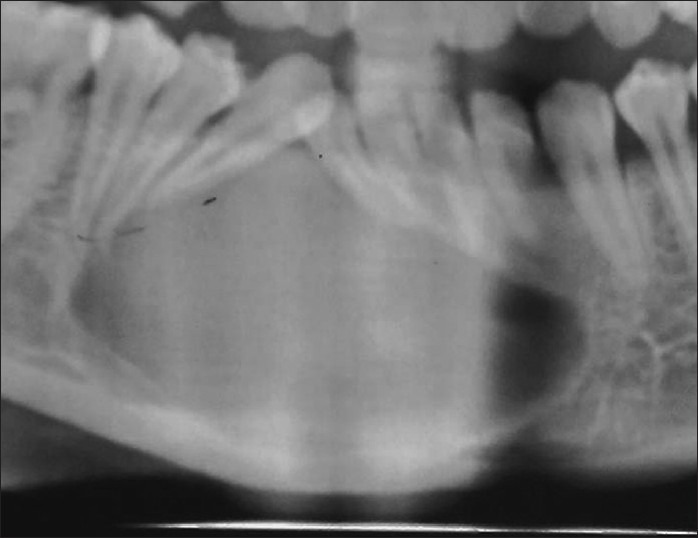
Figure 4.
Case 4: AOT
Figure 5.
Case 5: AOT
Figure 6.
Case 6: AOT
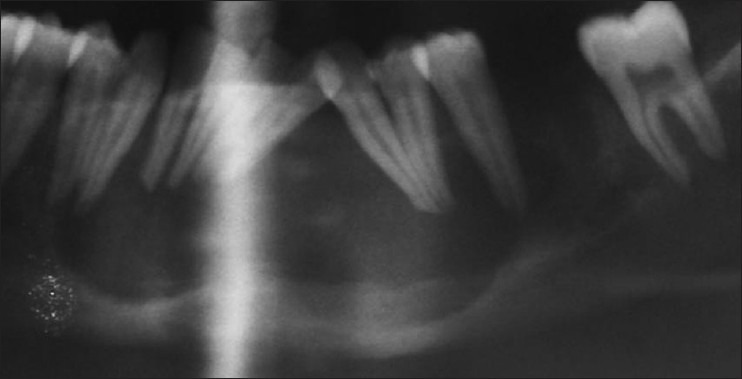
Figure 7.
Case 7: AOT
Figure 8.
Case 8: OKC
Figure 9.
Case 9: OKC
Figure 10.
Case 10: OKC
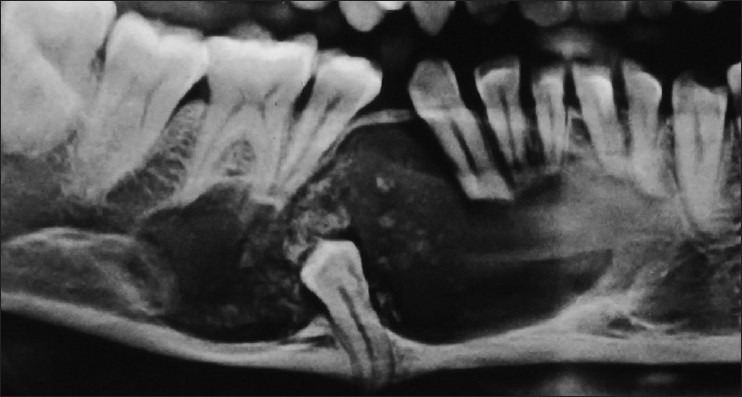
Figure 11.
Case 11: Ossifying Fibroma
Figure 12.

Case 12: Ossifying Fibroma
Figure 13.
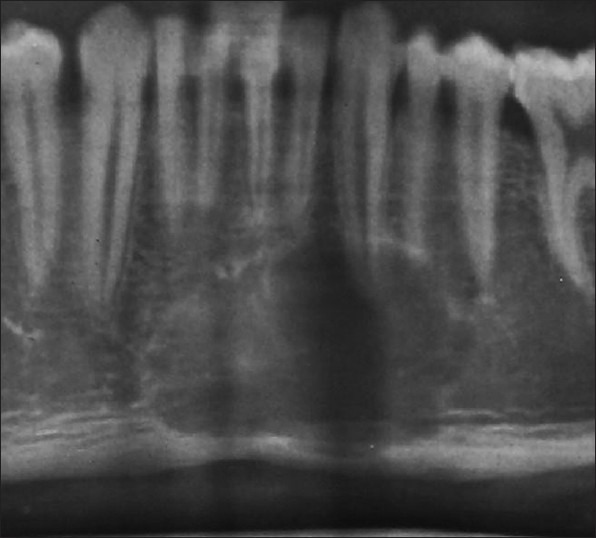
Case 13: Idiopathic Bone Cavity
Figure 14.
Case 14: Dentigerous Cyst
Figure 15.
Case 15: Radicular Cyst
Figure 16.
Case 16: CGCG
DISCUSSION
Histomorphology and histochemistry of a lesion determine the invasive potential and thus the appearance of lesion on a radiograph. A cyst has an epithelial wall that expands due to fluid collection and expression of various cytokines. However, the bone resorption follows path of least resistance making buccal plate more vulnerable to resorption. Slow expansion offers an opportunity to the overlying periosteum to form reactive bone and thus the cysts appear well-defined and exhibit corticated borders. Benign tumors that are subtle in their growth exhibit expansile resemblance to a cyst. This expansion is round/oval in three dimensions and resembles inflation of a balloon at slow pace.[1] On the contrary, OKC tends to grow along the internal aspect of jaws which ensures that cyst reaches considerable size before cortices are expanded.[2] Aggressive lesions like ameloblastomas, some CGCG, and calcifying cysts involve both cortices equally; causing buccolingual expansion rather than only buccal expansion. Chief complaint of 14 out of our 17 patients was swelling. In 12 out of these 14 cases, the swelling was perceptible extraorally which hampered aesthetics. The other two patients (case no. 2 and 9 representing ameloblastoma and OKC) presented with complaint of intraoral swelling. Ten out of these14 cases showed only buccal expansion. Four cases had both buccal and lingual expansion. All the four cases were of relatively invasive lesions; ameloblastoma (two), OF (one), and COC (one).[3,4] Lower border in anterior mandible is thick and dense, and hence less amenable to resorption. Only four out of 17 cases showed expansion extending to lower border. These included cases of ameloblastoma (case 3), OF (case 11 and 12), and COC (case 17). The second most common presenting complaint was pain which was present only in six out of 17 patients. In one case, it was the sole complaint (case 2); but in rest of the cases, it was present along with swelling. In nutshell, it can be said that most common clinical presentation of anterior mandibular unilocular lesion is of a painless swelling which is in accordance with previous studies.[3,4,5,6,7] In addition, we can say that these lesions tend to expand buccal cortex at upper border.
The word unilocular implies “single compartment”. Unilocularity can be seen in any lesion, but is rare in lesions that are more aggressive or in subtle lesions with superimposed infection. A unilocular radiolucency further exhibits different characteristics. The variations may be in the fill of radiolucency, borders, and influence on adjacent structures. Almost all lesions have variable presentations depending upon these characteristics. Benign lesions generally are round to oval and have corticated borders due to slow expansion and reactive bone formation. If the expansion outweighs the reactive bone formation, borders are non-corticated or partially corticated.[1] Borders of the same lesions may appear different at various sites in the same radiograph. In our series, approximately 50% patients had corticated or partially corticated borders. Same percentage was noted for patients with round or oval outline of lesion. The other half expressed irregular borders. This is acceptable as patients in our series comprised nine different lesions. Siar et al., reported unilocular ameloblastoma's percentage to be 20%.[8] Multicentric study by Dhanuthai et al., reported the same percentage to be 42%.[9] In another study of ameloblastomas in young patients (below 20 years) by Kahn et al., the percentage of unilocular ameloblastomas was 72%.[10] Mohamed et al., in their review concluded that most of AOT were round to oval and well demarcated.[11] Haring et al., reported the incidence of unilocular OKC to be 73.3%. They also found that the mean size of unilocular lesion was about half that of multilocular lesion.[12] Buchner reported that 156/168 cases of COCs were well defined and unilocular.[13] Cohen and Hertzanu in their series reported an incidence of 50% unilocular well-defined lesions amongst cases of CGCGs.[14]
Slow growth also ensures gradual pressure on adjacent structures; teeth or their roots, canal, and sinus floor; causing their displacement. Sixteen out of 17 lesions displaced the roots of adjacent teeth. Some of these lesions also have the propensity for resorption of roots. Eight out of 16 cases of root displacement showed concomitant root resorption. Resorption was seen only in lesions that had either non-corticated or partially corticated borders. Struthers and Shears found that 23.3% of jaw cysts and ameloblastomas caused resorption of adjacent roots. DC had much higher tendency for the same (55%) compared to other jaw cysts. Ameloblastomas had the highest tendency for the same (81%).[15]
All the lesions sparing IBC, RC, and CGCG had wide extensions. They grew more in length than width. The average number of teeth involved with any lesion was close to eight. This might be due to the fact that anterior mandible has most dense bone and expansion follows path of least resistance. IBC was discovered accidentally on OPG ordered for impacted third molars. The patient with RC complained of discolored and tilted tooth. The patient with CGCG had intraoral swelling in anterior mandible. These lesions are more infiltrative, so it could be picked at an early stage. All the remaining lesions had achieved significant size before patients presented to the institution for treatment.
We would like to stress upon some interesting illustrations demonstrating either same diagnosis with conflicting radiographic picture or with conflicting diagnosis and same radiographic picture.
Case 4 and 9 appear to be the mirror images of one another. These are two different patients with two different lesions (AOT and OKC) presenting with different signs and symptoms.
Case 10 and 14 show radiolucency of irregular shape that is partially corticated, associated with impacted tooth and causing displacement and resorption of adjacent roots and displacement of canal. These are more suggestive of an invasive tumor, but both the cases represent two different types of odontogenic cysts, that is, OKC and DC.
Case 13 and 16 also share a close resemblance although they are entirely different pathologies, the diagnosis being IBC and CGCG, respectively; with completely different line of treatment.
On the other hand, if we compare two different radiographic presentations of the same pathological type, that is, OF in case 11 and 12, we find a drastic difference. Not only radiographic pictures are contrasting but the clinical signs and symptoms also differ.
Case 6 and 7 also represent the same pathology, but an absolutely different radiographic profile. One radiograph shows a silent radiolucency with a peripheral hollow before merging into bone, not associated with any impacted tooth and not influencing the adjacent structures to a great extent. The other lesion is huge and round with sclerotic borders and including an impacted canine in its stroma, has displaced the adjoining tooth roots widely. The diagnosis in both cases was of an AOT.
CONCLUSION
Unilocular anterior mandibular radiolucencies represent an aberrant or less common site for pathologies commonly occurring in body and angle region. Anterior lesions are more common in females. Most cases report with painless intraoral or extraoral swelling. Expansion occurs more at upper border of buccal cortex. Lesions expand more in length rather than width. Root displacement is extremely common and root resorption is seen in extensive cases, especially in lesions with non-corticated or partially corticated borders. Lower border and lingual plate involvement is comparatively less common.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.White SC, Pharoah MJ. 4th ed. St. Louis: Mosby; 2000. Oral Radiology: Principles and Interpretation; pp. 355–419. [Google Scholar]
- 2.Shears M, Speight P. Cysts of the Oral and Maxillofacial Regions. 4th ed. Hoboken: Blackwell Publication Ltd; Odontogenic Keratocyst; pp. 6–58. [Google Scholar]
- 3.Reichart PA, Philipsen HP, Souner S. Ameloblastoma: Biological profile of 3677 cases. Eur J Cancer B Oral Oncol. 1995;31:86–99. doi: 10.1016/0964-1955(94)00037-5. [DOI] [PubMed] [Google Scholar]
- 4.Eversole R, Su L, ElMofty S. Benign fibro-osseous lesions of the craniofacial complex. A review. Head Neck Pathol. 2008;2:177–202. doi: 10.1007/s12105-008-0057-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Philipsen HP, Reichart PA. Adenomatoid odontogenic tumour: Facts and figures. Oral Oncol. 1998;35:125–31. doi: 10.1016/s1368-8375(98)00111-0. [DOI] [PubMed] [Google Scholar]
- 6.Mourshed F. A roentgenographic study of dentigerous cysts. 3 analysis of 180 cases. Oral Surg Oral Med Oral Pathol. 1964;18:466–73. doi: 10.1016/0030-4220(64)90392-5. [DOI] [PubMed] [Google Scholar]
- 7.Kaplan I, Buchner A, Calderon S, Kaffe I. Radiological and clinical features of calcifying epithelial odontogenic tumor. Dentomaxillofac Radiol. 2001;30:22–8. doi: 10.1038/sj/dmfr/4600566. [DOI] [PubMed] [Google Scholar]
- 8.Siar HC, Lau SH, Ng KH. Ameloblastoma of the jaws: A retrospective analysis of 340 cases in Malasian population. J Oral Maxillofac Surg. 2012;70:608–15. doi: 10.1016/j.joms.2011.02.039. [DOI] [PubMed] [Google Scholar]
- 9.Dhanuthai K, Chantarangsu S, Rojanawatsirivej S, Phattarataratip E, Darling M, Jackson-Boeters L, et al. Ameloblastoma: A multicentric study. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:782–8. doi: 10.1016/j.oooo.2012.01.011. [DOI] [PubMed] [Google Scholar]
- 10.Kahn MA. Ameloblastoma in young persons: A clinicopathologic analysis and etiologic investigation. Oral Surg Oral Med Oral Pathol. 1989;67:706–15. doi: 10.1016/0030-4220(89)90013-3. [DOI] [PubMed] [Google Scholar]
- 11.Mohamed A, Singh AS, Raubenheimer EJ, Bouckaert MM. Adenomatoidodontogenic tumour: Review of the literature and an analysis of 33 cases from South Africa. Int J Oral Maxillofac Surg. 2010;39:843–6. doi: 10.1016/j.ijom.2010.06.014. [DOI] [PubMed] [Google Scholar]
- 12.Haring JI, Van Dis ML. Odontogenic keratocyst: A clinical, radiographic, and histopathologic study. Oral Surg Oral Med Oral Pathol. 1988;66:145–53. doi: 10.1016/0030-4220(88)90082-5. [DOI] [PubMed] [Google Scholar]
- 13.Buchner A. The central (intraosseous) calcifying odontogenic cyst: An analysis of 215 cases. J Oral Maxillofac Surg. 1991;49:330–9. doi: 10.1016/0278-2391(91)90365-s. [DOI] [PubMed] [Google Scholar]
- 14.Cohen MA, Hertzanu Y. Radiologic features, including those seen with computed tomography, of central giant cell granuloma of the jaws. Oral Surg Oral Med Oral Pathol. 1988;65:255–61. doi: 10.1016/0030-4220(88)90176-4. [DOI] [PubMed] [Google Scholar]
- 15.Struthers P, Shears M. Root resorption by ameloblastomas and cysts of the jaws. Int J Oral Surg. 1976;5:128–32. doi: 10.1016/s0300-9785(76)80061-0. [DOI] [PubMed] [Google Scholar]


