Abstract
Most of the surgeons now use titanium miniplates because of its biocompatibility and corrosion resistant properties; studies have shown that these titanium particles are released in the surrounding tissues causing tissue necrosis and if these implants are placed for a long period, the adverse effect of these implants are more severe. It therefore necessitates a study to find out whether these titanium particles are released into surrounding tissues from titanium miniplates used for maxillofacial fractures so that we could use these implants, that is, bone plates and screws with more confidence.
Keywords: Fracture, scanning electron microscope, titanium implants
INTRODUCTION
The development of bone plates and other maxillofacial implants were initially an empirical process. From initial application of ivory pegs, soft iron wire, and lag screws in the fracture treatment to modern high strength alloys like stainless steel, titanium miniplates, and most recently the bioresorbable plates have scientifically evolved from concept to practice under the guidance of treating surgeons.
Since the advent of bone plates and screws in the beginning of the 20th century, failure of implants are being encountered.
Most of the studies with failed implants concentrated either on biological aspect of failure or an engineering aspect with little emphasis on comparative data from successful implants.
An additional reason to become more thorough in studying removed implants for the surgeon is due to increasing importance of the knowledge in medicolegal cases seeking redressal under the Consumer Protection Act.
Though we know that most of the surgeons now use titanium miniplates because of its biocompatibility and corrosion resistant properties, studies have shown that these titanium particles are released in the surrounding tissues causing tissue necrosis, and if these implants are placed for a long period the adverse effect of these implants are more severe.
Aims and objective
To evaluate histomorphologically the soft tissues adjacent to titanium miniplates for the presence of titanium particles.
To study soft tissue response around the titanium miniplates.
To observe for any unusual findings at the fixation site.
MATERIALS AND METHODS
Twenty patients reporting to the department of Oral and Maxillofacial Surgery, with history of open reduction and internal fixation with titanium miniplates for maxillofacial fractures were selected for the study.
Methods
Implant retrieval
Titanium bone plate and screws were removed either through intraoral/extraoral approach under local/general anesthesia and peri-implant tissue changes were observed. A small piece of soft tissue covering the plates and screws was excised and sent for scanning electron microscopic examination.
Photographic records
Photographic records of bone plates and screws in place prior to removal was made and also immediately after removal, photographic records of scanning electron microscope showing titanium particles in the soft tissue was recorded.
SOFT TISSUE RETRIEVAL AND MICROSCOPIC EXAMINATION
Soft tissues around the miniplates were retrieved after the bone plates and screws are removed.
The specimen was kept in the biopsy bottle in a dry environment. Plastic embedded 7 mm sections were used. Before examining the sections under the scanning electron microscope, the specimens were coated with a thin (about 2 nm) gold layer by a sputtering process (EMITECH, K550), for achieving a better topographic contrast. The composition of the particles was analyzed by using the integrated energy dispersive X-ray analysis (Noran Instruments, Voyager). The characteristic X-rays of an element, generated of the back scattering electrons, were analyzed.
All the soft tissue was microscopically examined with aid of scanning electron microscope (SEM-JSM 840) in the Department of Metallurgy, Indian Institute of Science Bangalore.
RESULTS
Thirty-six plates and 141 screws were retrieved from 20 patients. The duration between implant placement and retrieval ranged from 2 months to 2 years.
Bone plates and screws were retrieved for various reasons. In two patients (10%) plates were removed because of early infection within 6 months and in 4 patients (20%) plates were removed after 6 months due to late infection and these patients had extraoral draining sinus.
During the surgical procedures, in five cases loose screws and in one case fractured plates were observed.
The study conducted shows that six patient are not having titanium particles into the tissues and 14 patients are having titanium particles in the tissue.
DISCUSSION
Once the bone plates serve the purpose of rigid fixation (complete bone healing), whether the implants have to be removed or not is still a debatable matter amongst oral and maxillofacial surgeons and orthopedicians. An implant is considered to be failed when it is removed from the body due to mechanical and biological failure and there have been many researches which have supported this. In our study, we have evaluated the tissue response to titanium implants using scanning electron microscope; thus the fate of titanium bone plates.
The titanium implants in our study were retrieved for various reasons like pain, infection, and routine removal [Table 1]. Ferguson et al.,[1] and Miller et al.,[2] recommended routine removal of titanium plates and screws, while Hirai et al.,[3] and others recommended the retention of plates unless their removal is clinically indicated.
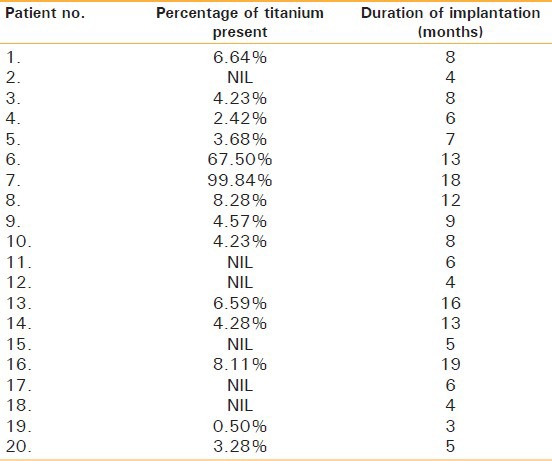
Table 1.
Results of the study
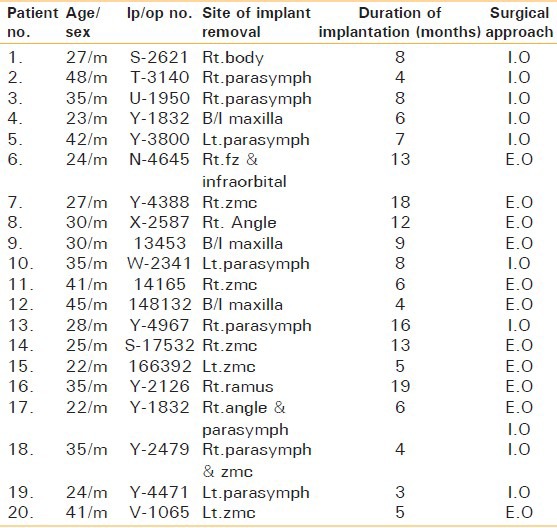
Among the group of patients studied in our unit, nine (45%) had postoperative complications, which correlated with a higher amount of peri-implant titanium particles. This could have been due to excessive molding of miniplates when they are used to fix in areas which requires contouring-like angle and parasymphysis of mandible and zygomatic buttress, fronto zygomatic, and infraorbital region. In the rest 11 patients, plates were retrieved as a routine procedure [Table 2]. The peri-implant tissues were studied under scanning electron microscope, which revealed comparatively lesser titanium particles. The complications observed in our study were higher than that reported by Katou et al.,[4] who encountered five patients with complications in his group of 27. Similarly, Katou et al.,[4] studied 15 patients out of which three had complications.
Table 2.
Reasons for implant removal
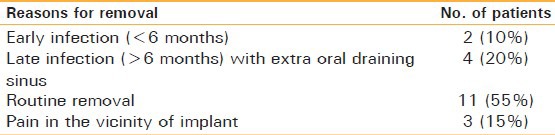
In six patients sinus formation was observed due to infection, majority of them presented with a late infection [Table 2, Figures 1-5]. Similarly, Katou et al.,[4] reported complications because of infection. Further reports on sinus formation, due to infection arising in the peri-implant tissue was supported by Hughes,[5] Brown,[6] and Black.[7] This higher rate of occurrence of infection was attributed to immunological response to the deposited metal particles released from the implants.
Figure 1.

Infection at the fractured site
Figure 5.
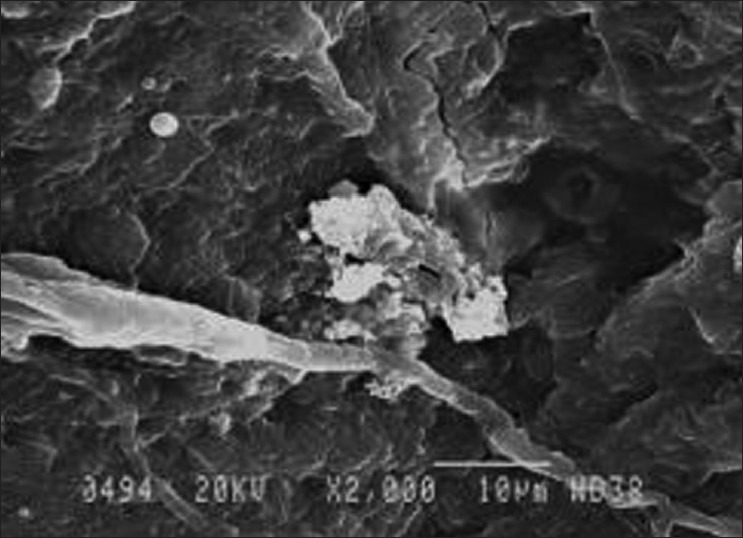
Scanning electron microscope picture showing titanium in the tissue
Figure 2.
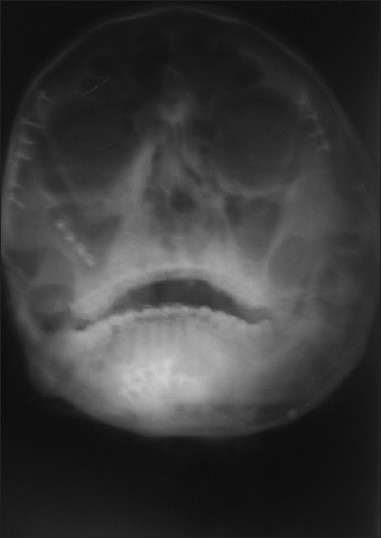
PNS view showing plates
Figure 3.

Exposure of the fractured site
Figure 4.

Tissue taken around the plates
Three patients in our study complained of pain in the vicinity of implants without any other clinical findings correlating with the pain hence we could associate the pain with the metallosis. Merritt[8] and Brown,[6] in their reported series on 10 symptomatic patients suggested that pain due to metal sensitivity should be considered when other causes of pain are ruled out [Table 2]. Tissues adjacent to implants were evaluated histologically in their series, which gave a picture of increased inflammatory cellular response in areas with metal deposits. In all patients, a complete resolution of symptoms was observed after removal of implants.
Abnormal findings like loose screws and fractured plate were observed in six of our patients on routine removal, but were asymptomatic [Table 3, Figures 6-10]. These abnormal findings as reported by Miller et al.,[2] may be due to metallosis of tissue leading to fibrosis. Mathew et al.,[9] showed similar findings and put forth the causes of screw loosening like inappropriate size of screw hole, unwanted movement of fractured fragments, and excessive molding of plates leading to distortion of hole; being some of the important causes. Though it is difficult to pinpoint on a particular cause, but removal of implant may suffice as an ultimate goal; thus precluding the possibility of unwanted effects of loose or fractured hardware.
Table 3.
Intraoperative findings

Figure 6.

Post-operative picture after implant placement
Figure 10.
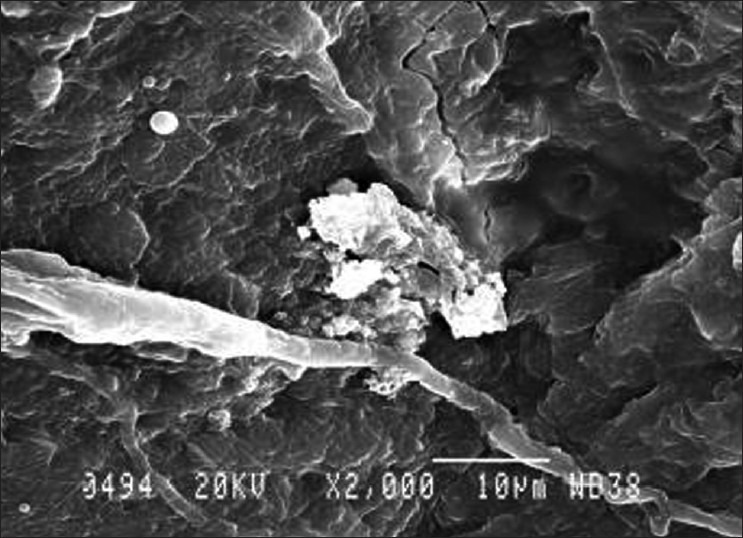
Scanning electron microscope picture showing titanium in the tissue
Figure 7.
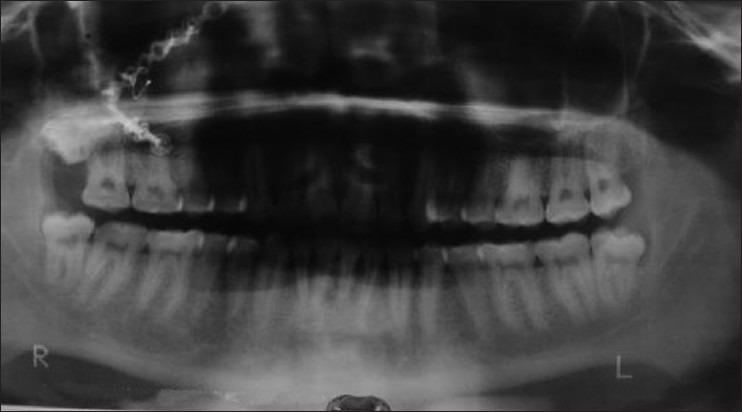
OPG showing titanium miniplates
Figure 8.

Implant exposure
Figure 9.

Fractured implants
We studied the presence of titanium in the soft tissues by using scanning electron microscope as done by Rosenberg et al.,[10] Langford and Frame,[11] and Hirai et al.[3] The amount of metal observed in each case was highly variable.
According to Tables 1 and 4, the amount of metal present in tissues did not correlate with the period of implantation.
Table 4.
Prescence of titanium in tissue around the plates
Different reasons for presence of titanium in adjacent tissues could be attributed to implant handling by the operator or manufacturer dependent:
Excessive bending of the hardware causing microfractures, thus shedding the metal particles.
Inappropriate use of drills, thus abrading the plates.
Abrasion cause between the screwdriver and screw head.
Manufacturing variations among different companies.
Irrespective of the reason of metal shedding from implants in adjoining soft tissue, there are adverse effects associated with the presence of titanium, thus favoring retrieval of bone plates after the purpose of rigid fixation (complete healing of the fracture) is served as also recommended by Rosenberg et al.,[10] Langford and Frame,[11] and Hirai et al.[3]
Our results showed presence of titanium particles in soft tissue resulting in fibrosis, necrosis, and inflammation. Hence, we recommended their removal after the purposes of rigid fixation have been fulfilled. But surely, long-term studies with more number of patients are required to affirmatively confirm the effect of titanium on living tissues.
SUMMARY AND CONCLUSION
The present study was carried out to analyze the presence and effects of titanium particles in peri-implant tissues in 20 patients operated previously in the Department of Oral and Maxillofacial Surgery.
Infection was found to be the prime reason for implant retrieval followed by pain in the vicinity of implant. Abnormal findings like loose screws, fractured plate were also noted.
Scanning electron microscopic study showed varied amount of titanium particles in the tissues surrounding the plate correlating with the patient's symptoms and clinical findings.
Following conclusions were made:
Infection and pain were predominant factors for the retrieval of bone plates.
The manufacturing composition of titanium plates and screws are not well-standardized.
Titanium released is higher in patients where excessive molding of plates, excessive movement at fracture sites is done during fixation.
“Implant failure is painful for both surgeons and patients”. Implant failure is multifactorial which mainly depends upon the quality control by the manufacturer and use of the proper technique by the surgeon.
With this small study we recommend the retrieval of titanium bone plates and screws after their purpose of rigid fixation is served. However, long-term studies need to be carried out for further supporting the results.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Ferguson AB, Jr, Laing PG, Hodge ES. The ionization of metal implants in living tissues. J Bone Joint Surg Am. 1960;42a:77–90. [PubMed] [Google Scholar]
- 2.Millar BG, Frame JW, Browne RM. A histological study of stainless steel and titanium screws in bone. Br J Oral Maxillofac Surg. 1990;28:92–5. doi: 10.1016/0266-4356(90)90129-9. [DOI] [PubMed] [Google Scholar]
- 3.Hirai H, Okumura A, Goto M, Katsuki T. Histological study of the bone adjacent to titanium bone screws used for mandibular fracture treatment. J Oral Maxillofac Surg. 2001;59:531–7. doi: 10.1053/joms.2001.22686. [DOI] [PubMed] [Google Scholar]
- 4.Katou F, Andoh N, Motegi K, Nagura H. Immuno-inflammatory responses in the tissue adjacent to titanium miniplates used in the treatment of mandibular fractures. J Craniomaxillofac Surg. 1996;24:155–62. doi: 10.1016/s1010-5182(96)80049-7. [DOI] [PubMed] [Google Scholar]
- 5.Hughes PJ, Brown SA, Payer JH, Merritt K. The effects of heat treatments and bead size on the corrosion of porous F.75 m saline and serum. J Biomed Mater Res. 1990;24:79–94. doi: 10.1002/jbm.820240108. [DOI] [PubMed] [Google Scholar]
- 6.Brown SA, Merritt K. Fretting corrosion in saline and serum. J Biomed Mater Res. 1981;15:479–88. doi: 10.1002/jbm.820150404. [DOI] [PubMed] [Google Scholar]
- 7.Black J, McDougall . New york: Churchil Livingstone; 1956. Orthopaedic biomaterials in research and practice. [Google Scholar]
- 8.Merritt K, Brown SA. Metal sensitivity to orthodontic implants. A review. Int J Dermatol. 1981;2:89–93. doi: 10.1111/j.1365-4362.1981.tb00408.x. [DOI] [PubMed] [Google Scholar]
- 9.Matthew IR, Frame JW, Browne RM, Millar BG. In vivo surface analysis of titanium and stainless steel miniplates and screws. Int J Oral Maxillofac Surg. 2000;25:463–8. doi: 10.1016/s0901-5027(96)80085-3. [DOI] [PubMed] [Google Scholar]
- 10.Rosenberg A, Grätz KW, Sailer HF. Should titanium miniplates be removed after bone healing is complete? Int J Oral Maxillofac Surg. 1993;22:185–8. doi: 10.1016/s0901-5027(05)80249-8. [DOI] [PubMed] [Google Scholar]
- 11.Langford RJ, Frame JW. Tissue changes adjacent to titanium plates in patients. J Craniomaxillofac Surg. 2002;30:103–7. doi: 10.1054/jcms.2002.0286. [DOI] [PubMed] [Google Scholar]


