Abstract
Objective:
Aloe vera is the oldest medicinal plant that has maintained its popularity over the course of time. It is widely known for its medicinal uses in wound healing, as an analgesic, and for its anti-inflammatory properties.
Aim:
The aim of this study is to evaluate the anti-inflammatory property of aloe vera mouthwash on plaque-induced gingivitis.
Materials and Methods:
Forty-five patients who were diagnosed with plaque-induced gingivitis were included in the study. They were divided into three groups with fifteen patients in each group. Group 1 was asked to rinse with 10 ml of aloe vera mouthwash twice daily for three months. Group 2 were treated with scaling only. Group 3 patients were asked to rinse with aloe vera mouthwash and scaling was done. The clinical changes were evaluated with Loe and Silness gingival index (1963) and Muhlemann and Son's Sulcus bleeding index (1971) at baseline, after one month and three months, respectively.
Results:
The data obtained was compared statistically. The paired ‘t’ test was done for intragroup comparison and one-way analysis of variance with a post hoc Tukey test was used for intergroup comparison. The data was obtained at the baseline, end of first month, and end of the third month. The result suggested reduction in gingival inflammation in all the three groups, but it was more in the aloe vera mouthwash and scaling group. Hence, it was concluded that aloe vera had a significant anti-inflammatory property. Thus, it can be used as an adjunct to mechanical therapy for treating plaque-induced gingivitis.
Keywords: Aloe vera, gingivitis, periodontal inflammation
INTRODUCTION
Aloes have been used therapeutically, certainly since the Roman times and perhaps long before.[1,2] Aloe vera (synonym: Aloe barbadensis Miller) belongs to the Liliaceae family, of which there are about 360 species. Aloe vera is a cactus-like plant that grows readily in hot, dry climates, and currently, because of demand, is cultivated in large quantities. Cosmetics and some medicinal products are made from the mucilaginous tissue in the center of the aloe vera leaf, which is called aloe vera gel. The peripheral bundle sheath cells of aloe vera produce intensely bitter, yellow latex, commonly termed as ‘aloe juice’, ‘sap’ or ‘aloes’. Aloe vera sap and aloe vera gel are often confused. Unlike aloes, aloe vera gel contains no anthraquinones, which are responsible for the strong laxative effects of aloes. However, the total leaf extracts may contain anthraquinones.
The pharmacological actions of aloe vera, as studied in vitro or in animals (in most cases the total leaf extract was used), include anti-inflammatory and anti-arthritic activity, and antibacterial and hypoglycemic effects. Aloe vera contains 75 potentially active constituents: Vitamins, enzymes, minerals, sugars, lignin, saponins, salicylic acids, and amino acids. Polysaccharides are considered to be the active ingredients of Aloe's anti-inflammation and immune-modulation effects. Inflammation is a tissue reaction by the body to injury and typically follows burns or other skin insults. It is classically characterized by swelling (tumor), pain (dolor), redness (rubor), and heat (calor), as well as loss of function.[3]
It is thus a complex process and investigations into the therapeutic properties of the gel should take account of its effects on these various symptoms. In addition, the gel may have more than one active constituent, which may be addressing different parts of the healing process. Although inflammatory processes are a natural response to injury and may hinder healing, it may also be undesirable to suppress them in an unstructured manner before their purpose is accomplished. Hence, the aim of the present study is to evaluate the anti-inflammatory property of aloe vera gel in plaque-induced gingivitis.
MATERIALS AND METHODS
The study design was a double-blind, randomized, placebo-controlled clinical study for a period of three months. It was approved by the Ethical Committee of the Institute of Dental Sciences, Bareilly. Informed consent was taken from all patients. Forty-five subjects with plaque-induced gingivitis were included, within the ages of 18 and 65 years; they were systemically healthy individuals, had not undergone prophylaxis for the last six months, and were with at least 20 teeth present. Patients on antibiotics/anti-inflammatory therapy for the last six months, pregnant females, those with a history of allergy to aloe vera, and patients unwilling to complete treatment were excluded from the study. The patients were divided into three groups.
The first group with 15 patients was given aloe vera gel mouthwash. The subjects were asked to rinse with 15 ml of solution for one minute twice daily[4] for 90 days and not to refrain from routine oral hygiene procedures. Group two subjects were treated with scaling and root planing only. Group three subjects were treated with scaling and root planing and were asked to rinse with aloe vera mouthwash twice daily for three months. Full mouth gingival index and sulcus bleeding indices were recorded at the first month as well as the third month for all subjects and were compared to baseline recordings.
Statistical analysis
The data obtained was compared statistically. The paired ‘t’ test was carried out for intragroup comparison and one-way ANOVA with post hoc Tukey test was used for intergroup comparison. A P≤ 0.05 was considered statistically significant.
RESULTS
Forty-five subjects were enrolled in the study. The result obtained was uneventful. Table 1 shows the one-way ANOVA between all the three groups at baseline, first month, and third month for Loe and Sillness gingival index and Sulcus bleeding index. There is suggestion of a reduction in gingival index and sulcus bleeding index in all groups in the first month and then in the third month. However, this reduction was not seen in the control group. This reduction was also seen when group comparisons were done at the baseline, first month, and third month within all the groups. Similar results were obtained in the Sulcus bleeding indices [Table 2].
Table 1.
One way ANOVA intergroup for Gingival index and Sulcus bleeding index
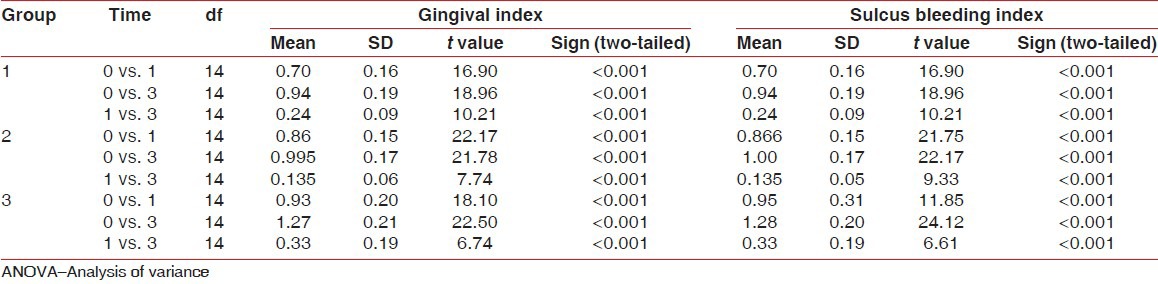
Table 2.
Paired t test for intragroup comparison between all three groups at different times
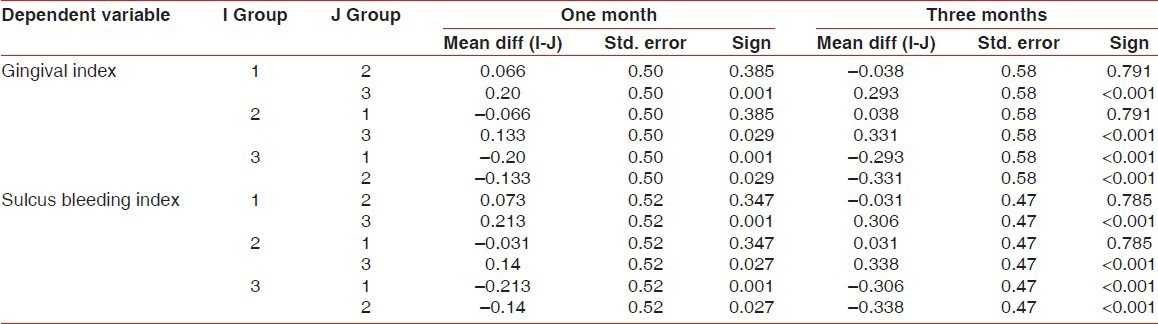
Table 3 shows post hoc tests for multiple comparisons and shows a statistically significant reduction in the gingival and sulcus bleeding indices at the end of the first month and third month, when Figure 1 was compared with Figure 2. Reduction was also statistically significant when Figure 3 was compared with Figure 2 at the end of the third month.
Table 3.
Post hoc Tukey HSD test for multiple comparisons
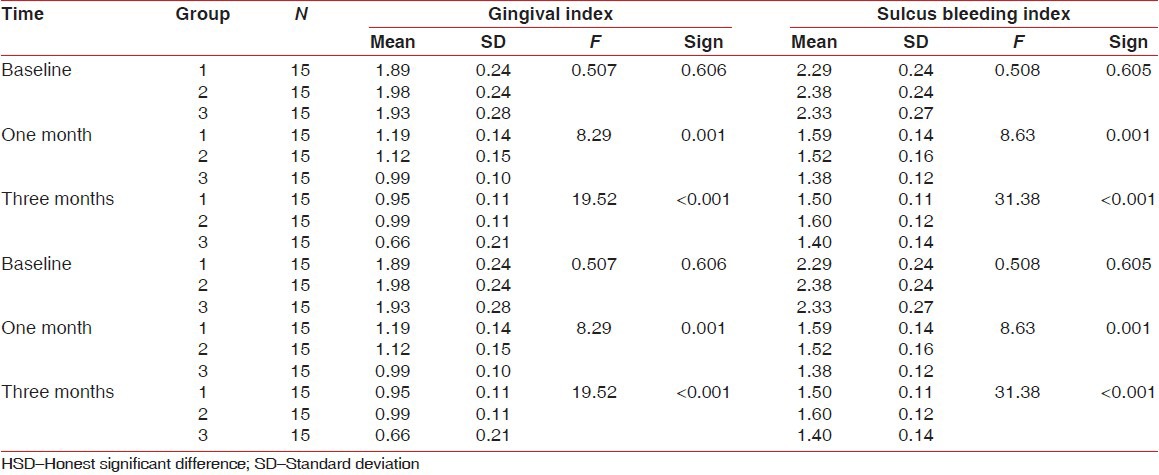
Figure 1.

Group 1 – Only aloe vera mouth wash. (a) Baseline; (b) One month; (c) Three months
Figure 2.

Group 3 – Aloe + Scaling (a) Baseline; (b) One month; (c) Three months
Figure 3.

Group 2 – Only scaling (a) Baseline; (b) One month; (c) Three months
DISCUSSION
Although inflammation is a necessary defensive mechanism it can lead to host-tissue destruction when the response is exaggerated. Thus, newer therapies must aim at moderating excessive inflammation. A similar attempt has been made in this study to treat gingivitis by aloe vera extract. The gingival index score and sulcus bleeding score are significantly reduced in all groups at the end of the first month (P < 0.01) with subsequent reduction at the end of the third month, suggestive of an anti-inflammatory effect of the ‘aloe vera mouth wash only’, ‘scaling only’, and ‘scaling and aloe vera mouthwash’ groups, with greater reduction in the gingival index and sulcus bleeding index in the ‘scaling and aloe vera mouthwash group’, as compared to both groups, at the end of one month. Reduction was more in the ‘scaling with mouthwash’ group as compared to the ‘scaling only’ and ‘aloe vera mouthwash only’ groups at the end of the third month. The results of the gingival index and sulcus bleeding index of the ‘scaling only’ and ‘aloe vera mouthwash only’ groups are suggestive of a decrease in gingival inflammation at the end of the first and third months. However, both groups had a similar degree of reduction, suggesting that the aloe vera mouthwash can be used as an adjunct to scaling, with better resolution of the inflammation.
Acceptability of the test product – reported unpalatable by few subjects. No itching, burning or other adverse effects on oral mucosa reported.
Davis et al. (1989),[5] tested the action of topical/injected aloe vera gel against inflammation produced by a variety of agents that were considered to induce different types of inflammation.
Davis et al. (1994)[6] – tested the anti-inflammatory and wound healing activity of aloe vera due to presence of growth substance mannose-6 phosphate.
Within the limitations of the study, it was found that aloe vera had a significant anti-inflammatory property. Thus, it can be used as an adjunct to mechanical therapy for treating plaque-induced gingivitis.
Hence, it can be concluded that the present study has an important impact to create an effective and inexpensive oral health intervention for low socioeconomic communities.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Crosswhite FS, Crosswhite CD. Aloe vera, plant symbolism and the threshing floor. Desert Plants. 1984;6:43–50. [Google Scholar]
- 2.Morton JF. Folk uses and commercial exploitation of Aloe leaf pulp. Econ Bot. 1961;15:311–9. [Google Scholar]
- 3.Macpherson G, editor. London: A and C Black; 1992. Inflammation, Black's Medical Dictionary; pp. 296–1. [Google Scholar]
- 4.Villalobos OJ, Salazar CR, Sánchez GR. Efecto de un enjuague bucal compuesto de aloe vera en la placa bacteriana e inflamación gingival. Acta Odontol Venez. 2001;39:16–24. [Google Scholar]
- 5.Davis RH, Rosenthal KY, Cesario LR, Rouw GA. Processed Aloe vera administered topically inhibits inflammation. J Am Podiatr Med Assoc. 1989;79:395–7. doi: 10.7547/87507315-79-8-395. [DOI] [PubMed] [Google Scholar]
- 6.Davis RH, Donato JJ, Hartman GM, Haas RC. Anti-inflammatory and wound healing activity of a growth substance in Aloe vera. J Am Podiatr Med Assoc. 1994;84:77–81. doi: 10.7547/87507315-84-2-77. [DOI] [PubMed] [Google Scholar]


