Abstract
Aim:
The aim of this study was to evaluate the clinical effectiveness of locally delivered xanthan-based Chlosite® gel as an adjunctive therapy to scaling and root planing in treatment of chronic periodontitis.
Materials and Methods:
In a randomized controlled clinical study, 30 patients were selected. Pocket depth between 5 and 7 mm was selected and each patient had two sites on the same side of the mouth. A total of 30 control sites were scaled and root planed and 30 test sites were scaled and root planed and Chlosite® gel was added. The clinical parameters, probing depth (PD), clinical attachment level (CAL), plaque index (PI) and bleeding on probing (BOP), gingival index were recorded at baseline, 6 weeks, 3 months and 6 months.
Statistical Analysis:
Paired/unpaired t-test was used, significance was placed at 5% level of significance, i.e., P < 0.05 was considered as a significant.
Results:
From baseline to a period of 6 months, significant difference was found between test and control group for PD, CAL, PI and BOP, P value being PD (P = 0.002), CAL index (P = 0.014), respectively.
Conclusion:
Subgingival injection of xanthan-based Chlosite® gel adjunct with scaling and root planing appeared to cause significant improvement compared with scaling and root planing alone in persons with chronic periodontitis.
Keywords: Chlorhexidine, local drug delivery systems, periodontitis
INTRODUCTION
Periodontitis describes a group of related inflammatory diseases resulting in the destruction of the tissues that support the tooth. Periodontitis has a multifactorial etiology with the primary etiologic agents being pathogenic bacteria that reside in the subgingival area.
Treatment of periodontal disease is routinely based on the mechanical debridement of the tooth surface and appropriate and meticulous maintenance of oral hygiene. However comprehensive mechanical debridement of sites with deep periodontal pockets is difficult to accomplish. It alone may fail to eliminate the pathogenic microflora because of their location within the gingival and dental tissues or in other areas inaccessible to periodontal instruments. As an adjunctive approach, systemic or local administration of antimicrobials is used because of the microbial etiology of periodontitis. Since the systemic antibiotics therapy has various disadvantages like hypersensitivity reaction, organ toxicity and development of resistant bacteria[1] and also requires higher dosage to attain required gingival crevicular fluid (GCF) concentration at the target site, this lead to use of local drug delivery system.
Topical administration of antibacterial agents in the form of mouthwashes, dentifrice or gels can be used effectively in controlling supragingival plaque. Irrigation systems or devices can deliver agents into deep pockets, but are not effective in halting the progression of periodontal attachment loss. As GCF within a periodontal pocket is replaced every 90 s, the effects of antiseptic pocket irrigation are only transient.[2]
Local delivery devices are system designed to deliver agents into the periodontal pocket to retain therapeutic levels for a prolonged period of time. The periodic use of local delivery systems in reducing probing depths (PD), stabilizing attachment levels and minimizing bleeding would allow better control of the disease. Controlled release local delivery systems, in which the antimicrobial is available at therapeutic levels for several days, have been evaluated in several forms and using different antimicrobials. Devices that have been developed include fibers, chips, slabs and injectable systems. Different drugs used for local drug delivery are tetracyclines including doxycycline and minocycline, metronidazole and chlorhexidine (CHX). These devices are less invasive treatment options and it requires less time compared to surgical treatment.
Hence patients with moderate periodontitis can be treated by non-surgical therapy to halt periodontal disease and limit the extent of surgical intervention needed in the future. Patients’ in whom surgery is contraindicated due to certain systemic factors in those patients local drug therapy is needful.
CHX is one of the most effective topical agents, long been used as an effective antimicrobial agent. It is an antiseptic, which adheres to organic matter and demonstrates low toxicity when applied topically. Its efficacy as a topical rinse to inhibit dental plaque and gingivitis has been well-established in study periods for up to 2 years without evidence of development of any bacterial resistance.[3] It has been found to be effective against subgingival bacteria when delivered through a sustained release device. CHX has been shown to be an effective agent in plaque inhibition because it is well-retained in the oral cavity, reacting reversibly with receptors in the mouth due to its affinity for hydroxyapetite and acidic salivary protein.[4] It has very low systemic toxic activity in humans and has not produced any appreciable resistance to oral microorganism and has not been associated with any teratogenic alterations.
Short term use of CHX causes a striking reduction in the number of oral microorganisms. In the absence of other oral hygiene measures, CHX has been shown to reduce the number of bacteria in saliva.[5]
In a developing country with a high prevalence of periodontitis, any strategy that arrests or prevents the progression of periodontitis will be definitely useful. There are very few studies available for the use of CHX in gel form as a local drug delivery system as an adjunct to scaling and root planing. In the present study, an attempt has been made to evaluate and compare the efficacy of gel containing chlorhexidine digluconate (0.5%) and chlorhexidine dichydrochloride (1.0%) as an adjunct to scaling and root planing with scaling and root planing alone. Digluconate is released immediately and dihydrochloride is released more slowly and over a longer period of time. These are bacteriostatic and bactericidal antiseptics, capable of protecting the treated pocket from recolonization of microorganism for at least 2 weeks.
MATERIALS AND METHODS
A total of 30 subjects, above 30-60 years of age comprising of both the gender were randomly selected and diagnosed as suffering from chronic localized or generalized periodontitis, from the Outpatient Department of Periodontics, K. M Shah Dental College and Hospital, Vadodara. An informed consent was taken from all the subjects before the start of the study. The ethical committee of the university was presented the synopsis and a clearance was obtained after their approval.
Inclusion criteria
Patients between 30 to 60 years of age
Good general health
Presence of two periodontal sites located on the same side PD between 5 to 7 mm
Localized or generalized chronic periodontitis patients.
Exclusion criteria
Use of systemic or subgingival antimicrobial within the 6 months prior to the study
Presence of vertical bone defect
Use of anti-inflammatory therapy within the 6 months prior to the study
Allergy to CHX
Habit of tobacco chewing and smoking
History of systemic diseases that could influence the course of periodontal disease or would require prophylactic antibiotics (not medically compromised)
Pregnancy and lactation
Aggressive periodontitis
Any teeth with furcation involvement
History of periodontal therapy 6 months back.
Clinical procedure
A special proforma was designed for the present study so as to have a systemic and methodical recording of all the observation and information. Clinical examination was done on a dental chair, under standard conditions of light, using a mouth mirror, University of North Carolina-15 (UNC-15) probe (Hu-Friedy®) and tweezers and assessment of clinical parameters were carried out. After recording of preliminary information, acrylic stent were prepared. Selected sites were randomly divided into control sites and test sites. Both of these sites should be placed on the same side of the patient mouth.
Control sites: 30 sites were treated by scaling and root planing alone.
Test sites: 30 sites were treated with scaling and root planing followed by the placement of the CHX gel in the periodontal pocket [Figure 1].
Figure 1.

Chlosite pack
The following parameters were recorded at baseline (day 0), 6 weeks, 3 months and 6 months using a UNC-15 probe (Hu-Friedy®) by a single examiner who was blinded:
Gingival index (GI)[6]
Sulcus bleeding index[7]
Plaque index (PI)[8]
Probing pocket depth - measurement to the nearest millimeter of the distance from the gingival margin to the depth of the pocket
Relative clinical attachment level (CAL).
Customized acrylic occlusal stents with vertical grooves were prepared for each subject on a study model to standardize the readings. Vertical grooves were made to guide the probe penetration vertically in the same plane. Customizes acrylic stents were stored on the prepared study casts to minimize distortion. The pocket depths were measured from the crest of marginal gingiva to the base of the pocket using UNC-15 probe [Figure 2].
Figure 2.

Measurement of relative clinical attcahment level and probing depth using a stent
Relative distance between the base of the pocket and fixed reference point (horizontal notch) on the stent was measured. This was later on used for assessment of clinical attachment gain or loss.
After recording all the parameters at the baseline, full mouth scaling and root planing was performed using ultrasonic instruments followed by hand instruments until all supra and subgingival root surfaces felt hard and smooth. No time restriction was instituted for this treatment.
Following debridement, target sites were irrigated gently with cold saline and then left for 10 min to achieve hemostasis prior to placement of CHX gel (Chlosite®) and it was applied into the deepest portion of periodontal pocket by means of a thin rounded tip needle [Figure 3].
Figure 3.

Placement of chlorhexidine gel
To ensure that the CHX gel stays long enough to be effective in the pocket, a periodontal dressing was placed without pressure over the treated sites [Figure 4].
Figure 4.

Periodontal pack in place
Post-operative home care instructions including brushing 2 times daily with a soft brush were given. Use of oral chemotherapeutic and irrigation devices was not allowed.
Recall visits
Subjects were recalled after 7 days for removal of the periodontal dressing and for oral hygiene maintenance instructions. Recall visits were again scheduled after 6 weeks, 3 months and 6 months of placement of the experimental drug for recording of clinical parameters. No subgingival instrumentation was performed at subsequent visits and patients were reinstructed on oral hygiene maintenance.
RESULTS
A total of 30 patients were included in the study. 17 were male and 13 were female. The age range taken was between 30 and 60 years.
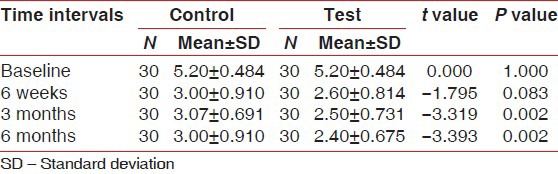
Probing pocket depth
Table 1 shows a comparison of mean PD between test and control group at baseline, 6 weeks, 3 months and 6 months with statistically significant results at 3 months and 6 months (i.e., 0.002 and P = 0.002 respectively) for the test group.
Table 1.
Comparison of mean pocket probing depth
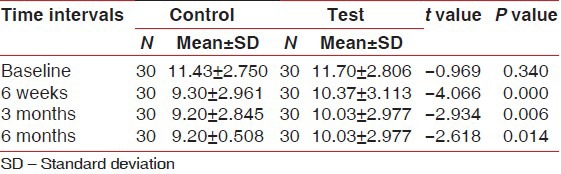
Relative CAL
Table 2 shows a comparison of mean CAL between test and control group at baseline, 6 weeks, 3 months and 6 months with statistically significant results at 6 week, 3 months and 6 months for the test group (i.e., P = 0.000, P = 0.006 and P = 0.014 respectively).
Table 2.
Comparison of mean relative clinical attachment level
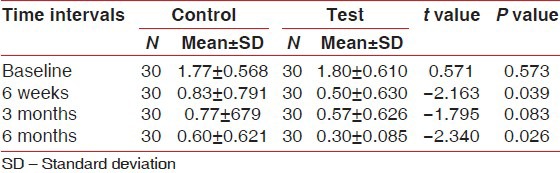
Gingival index
Table 3 shows a comparison of mean GI scores between test and control group at baseline, 6 weeks, 3 months and 6 months with statistically significant results at 6 weeks and 6 months for the test group (i.e., P = 0.039 and P = 0.026, respectively).
Table 3.
Comparison of mean Gingival index scores
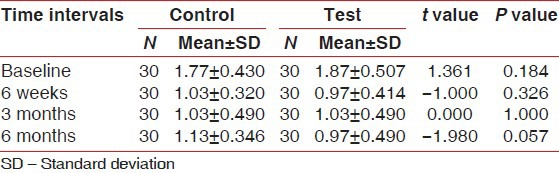
Plaque index
Table 4 shows at baseline, 6 weeks, 3 months and 6 months there was no statistically significant difference between test and control group.
Table 4.
Comparison of mean Plaque index score
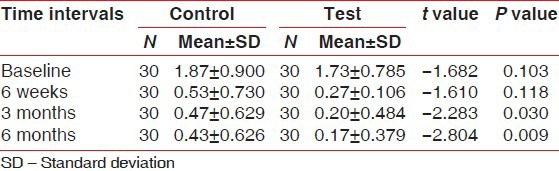
Bleeding index
Table 5 shows comparison of mean bleeding index scores between test and control group at baseline, 6 weeks, 3 months and 6 months with statistically significant results at 3 months and 6 months in the test group (i.e., P = 0.030 and P = 0.009 respectively).
Table 5.
Comparison of mean Bleeding index scores
DISCUSSION
Chlosite® (GHIMAS, Italy) is a xanthan based syringable gel system. The gel is a combination of two CHX formulations: 0.5% chlorhexidine digluconate and 1.0% chlorhexidine dihydrochloride incorporated in a saccharidic polymer, xanthan. Cross linking structure of xanthan controls the release of drugs and it exhibits a near zero order drug release. When in contact with water, it forms a three dimensional pseudoplastic reticulum capable of holding and maintaining various substances in suspension. The CHX xanthan based gel undergoes a progressive process of imbibition and is physically removed in 10-30 days. Chlorhexidine digluconate is liberated in the first day and achieves a concentration >100 μg/ml, which is maintained for an average of 6-9 days which is greater than the minimum inhibitory concentration for CHX (0.10 μg/ml). Chlorhexidine dihydrochloride is released in the following days and maintains the bacteriostatic and bactericidal concentrations for at least 2 weeks and prevents recolonization.[9]
The CHX gel is supplied with a special needle having a blunt tip and a lateral opening. This facilitates the application of the gel without traumatizing or damaging the periodontal tissues.
Periodontal probing is one of the most widely used diagnostic tools for the clinical assessment of connective tissue destruction in periodontal disease. Increased PD and loss of clinical attachment are pathognomonic for periodontitis and hence, serve as primary parameters in diagnosis of periodontal disease and evaluation the success of periodontal therapy. Results of this study are consistent with the results observed by Vinholis et al.[10] when they evaluated the effect of subgingival irrigation with a 1% CHX collagen gel in periodontal pockets as an adjunct to scaling and root planing. Mizrak et al.[11] observed similar reduction of probing pocket depth with both the group that were treated either by scaling and root planing alone or scaling and root planing with controlled release CHX chip.
Determining change in attachment level (gain or loss) is a primary measure and one of the most practical methods of determining progression of periodontal disease. The results of this study coincide with the study carried out by Perinetti et al.[12] who observed more gain of relative CALs in subjects treated with 1% CHX gel as compared to placebo gel. Cosyn and Wyn[13] observed significant additional gain of clinical attachment with sites treated by scaling and root planing with CHX varnish as compared with sites treated by scaling and root planing alone. These results are similar to those obtained in the present study.
The degree of severity of gingival inflammation can be measured by assessing GI. Furthermore, several investigators have indicated that bleeding from gingiva after light probing is indicative of gingival inflammation and disease activity. Soskolne et al.[14] observed significant reduction of GI score with scaling and root planing with CHX treated sites when compared with the control (scaling and root planing) site, which is similar to the observation of the present study. Similar results were obtained in the study by He et al.[15] where significant percentage reduction of GI was observed in the experimental group (scaling and root planing with CHX chip) compared with the control group (scaling and root planing).
Azmket et al.[16] observed that the PI decreased in both the control (scaling and root planing alone) and experimental group (scaling and root planing with CHX chip). The results of present study are similar to this study. In the present study, the reduction of plaque from baseline in the control and experimental group could be due to greater attention to oral hygiene practice by all the selected participants.
It is accepted that bleeding upon probing and PD is critical site-specific periodontal parameters evaluating the probability of periodontal disease progression. The observations of the present study are consistent with the findings of Heasman et al.[17] who observed mean reduction of bleeding index score from baseline in the experimental group (scaling and root planing with CHX chip) as well as control group (scaling and root planing alone). The result is similar to the results observed in the present study.
CONCLUSION
It can be concluded that experimental local drug delivery system containing 1.5% CHX gel can be effectively used as an adjunct to scaling and root planing and is more effective than scaling and root planing alone in the treatment of periodontal pockets. The experimental local drug delivery system is easy to use, noninvasive and requires less chair side time.
To elucidate the use of this local drug delivery system in future, a long term study, carried out on a large sample of subjects, is required.
In addition, microbiological studies can also be used to correlate with the clinical findings observed. An attempt is required to find out the efficacy of experimental material in comparison to other marketed local drug delivery system.
ACKNOWLEDGEMENTS
I am immensely thankful to Dr. Sharmila Verma and Dr. Nehal Sheth Dr. Monali Shah, whose invaluable advice and support helped extract the best in me.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Golomb G, Friedman M, Soskolne A, Stabholz A, Sela MN. Sustained release device containing metronidazole for periodontal use. J Dent Res. 1984;63:1149–53. doi: 10.1177/00220345840630091101. [DOI] [PubMed] [Google Scholar]
- 2.Heitz-Mayfield LJ, Lang NP. Surgical and nonsurgical periodontal therapy. Learned and unlearned concepts. Periodontol 2000. 2013;62:218–31. doi: 10.1111/prd.12008. [DOI] [PubMed] [Google Scholar]
- 3.Schiott CR, Briner WW, Kirkland JJ, Löe H. Two years oral use of chlorhexidine in man. III. Changes in sensitivity of the salivary flora. J Periodontal Res. 1976;11:153–7. doi: 10.1111/j.1600-0765.1976.tb00063.x. [DOI] [PubMed] [Google Scholar]
- 4.Löe H, Schiott CR. The effect of mouthrinses and topical application of chlorhexidine on the development of dental plaque and gingivitis in man. J Periodontal Res. 1970;5:79–83. doi: 10.1111/j.1600-0765.1970.tb00696.x. [DOI] [PubMed] [Google Scholar]
- 5.Davies RM, Jensen SB, Schiott CR, Löe H. The effect of topical application of chlorhexidine on the bacterial colonization of the teeth and gingiva. J Periodontal Res. 1970;5:96–101. doi: 10.1111/j.1600-0765.1970.tb00699.x. [DOI] [PubMed] [Google Scholar]
- 6.Loe H, Silness J. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand. 1963;21:533–51. doi: 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- 7.Mühlemann HR, Son S. Gingival sulcus bleeding: A leading symptom in initial gingivitis. Helv Odontol Acta. 1971;15:107–13. [PubMed] [Google Scholar]
- 8.Silness J, Loe H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condtion. Acta Odontol Scand. 1964;22:121–35. doi: 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- 9.Rusu D, Benta A, Necker A. Non-surgical periodontal therapy using a novel chlorhexidine based xanthan gel; a split mout study. Int Poster J Dent Oral Med. 2005;7:286–91. [Google Scholar]
- 10.Vinholis AH, Figueiredo LC, Marcantonio E, Júnior, Marcantonio RA, Salvador SL, Goissis G. Subgingival utilization of a 1% chlorhexidine collagen gel for the treatment of periodontal pockets. A clinical and microbiological study. Braz Dent J. 2001;12:209–13. [PubMed] [Google Scholar]
- 11.Mizrak T, Güncü GN, Caglayan F, Balci TA, Aktar GS, Ipek F. Effect of a controlled-release chlorhexidine chip on clinical and microbiological parameters and prostaglandin E2 levels in gingival crevicular fluid. J Periodontol. 2006;77:437–43. doi: 10.1902/jop.2006.050105. [DOI] [PubMed] [Google Scholar]
- 12.Perinetti G, Paolantonio M, Cordella C, D’Ercole S, Serra E, Piccolomini R. Clinical and microbiological effects of subgingival administration of two active gels on persistent pockets of chronic periodontitis patients. J Clin Periodontol. 2004;31:273–81. doi: 10.1111/j.1600-051x.2004.00481.x. [DOI] [PubMed] [Google Scholar]
- 13.Cosyn J, Wyn I. A systematic review on the effects of the chlorhexidine chip when used as an adjunct to scaling and root planing in the treatment of chronic periodontitis. J Periodontol. 2006;77:257–64. doi: 10.1902/jop.2006.050216. [DOI] [PubMed] [Google Scholar]
- 14.Soskolne WA, Heasman PA, Stabholz A, Smart GJ, Palmer M, Flashner M, et al. Sustained local delivery of chlorhexidine in the treatment of periodontitis: A multi-center study. J Periodontol. 1997;68:32–8. doi: 10.1902/jop.1997.68.1.32. [DOI] [PubMed] [Google Scholar]
- 15.He L, Geng S, Cao C. The efficacy of the chlorhexidine chip following scaling and root planing (SRP) and compared to SRP alone. Zhonghua Kou Qiang Yi Xue Za Zhi. 2001;36:443–5. [PubMed] [Google Scholar]
- 16.Azmak N, Atilla G, Luoto H, Sorsa T. The effect of subgingival controlled-release delivery of chlorhexidine chip on clinical parameters and matrix metalloproteinase-8 levels in gingival crevicular fluid. J Periodontol. 2002;73:608–15. doi: 10.1902/jop.2002.73.6.608. [DOI] [PubMed] [Google Scholar]
- 17.Heasman PA, Heasman L, Stacey F, McCracken GI. Local delivery of chlorhexidine gluconate (PerioChip) in periodontal maintenance patients. J Clin Periodontol. 2001;28:90–5. doi: 10.1034/j.1600-051x.2001.280114.x. [DOI] [PubMed] [Google Scholar]


