Abstract
Aim:
To investigate whether the use of an oxidizing mouth rinse as an adjunct to chlorhexidine is efficacious in reducing stains and plaque.
Materials and Methods:
This study had a single-blind, three-group (n = 35 each) parallel design, including a 21 days experimental period during which group I rinsed with chlorhexidine (CHX) 0.2% alone, group II used chlorhexidine (CHX) followed by hydrogen peroxide (H2O2) 1.5%. Group III rinsed with the same mouthwashes in reverse order. Patients were randomly assigned to one of the three groups. The examination for plaque, and stains was done after 1, 2, and 3 weeks of rinsing.
Results:
Group II showed significantly less stain intensity in comparison with group I after 14 and 21 days (P values 0.025 and 0.005, respectively). The proportion of stained surfaces was less in the group II than in the group I and was significant at the end of 1 week. The plaque formation was significantly less in groups II and III than group I at 7, 14, and 21 days.
Conclusion:
The adjunctive use of hydrogen peroxide to chlorhexidine proved to be superior to chlorhexidine alone with regard to the inhibition of plaque and development of stains.
Keywords: Chlorhexidine, hydrogen peroxide, plaque, stain intensity, stain area
INTRODUCTION
The role of dental plaque in the aetiology of dental diseases is well recognised. Thus, the treatment and prevention of gingivitis is a valuable goal in periodontal therapy.[1] There is evidence which demonstrates that improving oral hygiene and gingival health has been associated with a decreasing incidence of periodontal disease. On the basis that plaque-induced gingivitis always precedes the occurrence and recurrence of periodontitis, the mainstay of primary and secondary prevention of periodontal diseases is the control of supragingival plaque.[2]
Until now, mechanical cleansing is the most widely used method of supragingival plaque control and is effective in areas where access to plaque deposits is possible.[3] Evidences exist that the degree of motivation and skill required with the oral hygiene products such as toothbrushes, dental floss, toothpicks, and interdental brushes may be beyond the ability of majority of the patients. There are also groups of individuals such as temporarily disabled individuals including non-ambulatory patients and handicapped people, for whom adequate oral hygiene is a problem.[4] Therefore, an alternative method of plaque control would be desirable.
Many kinds of chemical substances have been investigated. The major problem of these substances has been the relatively short period of contact between active agent and the teeth, and existence of the side effects. Chlorhexidine (CHX) is the chemical agent which seems to be most effective in plaque control.[5] Its effect is prolonged and it has the ability to inhibit plaque formation to a large degree.[6] It is used as mouthwash, gel, sprays, varnish,[7] and in toothpastes.[8]
Though CHX is considered as the best agent for plaque control and gingivitis, many patients find its initial bitter taste unpleasant, and repeated use often produces stains and taste disturbances. Because of this, daily rinsing with CHX is not promoted. It would, however, be desirable to have the possibility to use CHX over an extended period of time. The absence of stain formation could improve patient compliance and reduce the time necessary to clean the dentition during recall.
Oxygenating agents have been employed for supragingival plaque control and in the treatment of acute ulcerative gingivitis without any harmful side effects on the tissues.[9] Hydrogen peroxide (H2O2) 1.5% has been shown to have a good stain removing capability both in vitro and in vivo. The mechanism of stain removal includes oxygen-releasing mechanical cleansing actions and oxidation or reduction reactions. Free radicals released by hydrogen peroxide break the electron-rich alkene double bonds which are responsible for discoloration, resulting in stain removal.
The use of H2O2 as an adjunct to CHX has been found to be very effective in reducing plaque scores, and in preventing the stain development.[9,10] The purpose of this study was to investigate whether the use of a hydrogen peroxide mouth rinse as an adjunct to chlorhexidine mouth rinse compared to chlorhexidine alone is efficacious in inhibiting the development of plaque and gingivitis, along with its ability to reduce the stains.
MATERIALS AND METHODS
This 21 days duration study was conducted in the department of Periodontics, of the institution. A total of 105 subjects participated in the study, out of which 55 (57.75%) were females and 50 (52.5%) were males. The subjects included BDS and dental hygienist students of the college, and the patients visiting the outpatient department of Periodontics. The patients were informed about the study and a written consent was obtained. Inclusion criteria were: (a) healthy patients of age group between 18 and 30 years, (b) no history of smoking,(c) Minimum of 24 teeth present, (d) no pockets >5 mm present, (e) no antibiotics intake for last 3 months, and (f) no systemic disease. Exclusion criteria were: (1) Presence of fixed or removable orthodontic appliance or prosthesis, (2) allergy to chlorhexidine or hydrogen peroxide, and (3) pregnant females. Scaling with ultrasonic scaler and polishing with fine grit prophylaxis paste was done for all the subjects to establish the baseline. All the subjects were given the demonstration of Bass method of tooth brushing and were asked to follow the same using Stim® soft toothbrush and Colgate® toothpaste prior to rinsing.
The selected candidates were randomly divided into one of the three treatment groups; each group comprises 35 subjects. Group I was instructed to rinse with 0.2% CHX (Hexidine®) twice daily (60 s) for 3 weeks after brushing.[11] Group II was instructed to rinse with 0.2% CHX (60 s) followed by 1.5% H2O2 (60 s) twice daily for 3 weeks after brushing. Group III was asked to rinse with 1.5% H2O2 (60 s) followed by 0.2% CHX (60 seconds) twice daily for 3 weeks after brushing. The subjects were asked to return after the end of first, second and third week for the evaluation, to check the compliance and to issue more mouthwash.
Preparation of hydrogen peroxide mouth rinse
The subjects were instructed to add 2.5 ml of Hydroxyl® mouthwash (6%) to 7.5 ml of water to make it 1.5% with the measuring cap provided with the mouthwash, just before every rinse.
Clinical examination
The name, age, gender, and address of the subjects were recorded in the performa. They were examined clinically with a mouth mirror, UNC15 periodontal probe and explorer.
The scoring procedure used to assess stain area and intensity was the Lobene index modified by Koertge and Gunsolley (GMSI)[12] with the following criteria: Stain intensity: 0 = No stain present, natural tooth coloration, 1 = faint stain 2 = clearly visible stain, orange to brown, 3 = dark stain, deep brown to black. Stain area 1 = thin line, can be continuous, 2 = thick line or band, 3 = covering the total area.
Plaque Index (PI):- The clinical scoring procedure used to assess plaque formation was the Turesky modification of the Quigley-Hein plaque index.[13] A disclosing agent (alpha plaque) was used to score plaque on a numerical scale according to the following criteria: 0 = No plaque, 1 = Separate flecks of plaque at the cervical margin of the tooth, 2 = A thin, continuous band of plaque (up to 1 mm) at the cervical margin, 3 = A band of plaque wider than 1 mm but covering less than one-third of the crown, 4 = Plaque covering at least one-third but less than two-thirds of the crown and 5 = Plaque covering two-thirds or more of the crown.
Statistical analysis
Mean of all the individual subject scores at the end of 1st, 2nd, and 3rd week was calculated for stain intensity, stain area, and plaque. For intra-group comparison, paired comparison test was applied. For inter-group comparison, general linear model, and multiple comparison test was applied. Value of ≤0.05 was considered as significant whereas ≤0.001 was highly significant.
RESULTS
For evaluation of stains and plaque scores, 105 subjects were examined. Mean scores for each group comprising of 35 subjects were calculated at the end of 1, 2, and 3 weeks. Table 1 shows the intra-group comparison of mean stain area, intensity, and plaque scores after 1, 2, and 3 weeks in all the groups. In all the groups, there was a significant increase in the mean stain area and mean stain intensity after 2 weeks in comparison to the 1st week. After the end of 3rd week, the mean stain area was significantly more than the scores at the end of 2nd week in group I and group II. Whereas there was a non-significant increase in mean stain intensity after 3 in comparison with the scores at 2 weeks in group I and group III.
Table 1.
Intra-group comparison of mean stains and plaque scores between 1st and 2nd, and 2nd and 3rd weeks
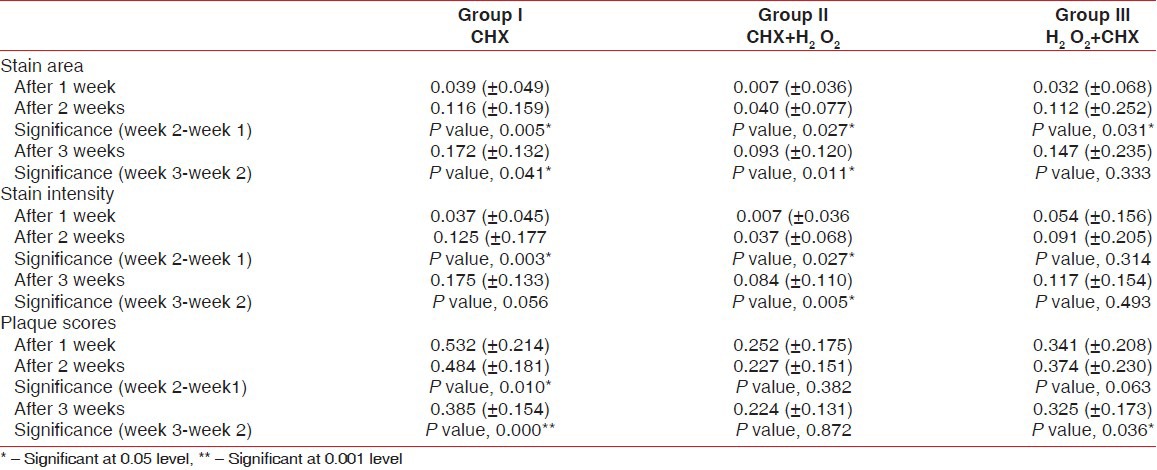
In all the three groups, there was a reduction in mean plaque score at the end of 2 weeks in comparison with scores at the end of 1 week and was significant in group I. At the end of 3 weeks also, there was further reduction in plaque scores in comparison with the scores at 2 weeks in all three groups. The reduction was significant in group I and group III.
Inter group comparison of the mean scores at the end of 1, 2, and 3 weeks was done between group I and II, I and III, and II and III as shown in Tables 2–4. After the end of 1st week [Table 2], the mean stain area was significantly more in group I and group III in comparison to group II. After 2 and 3 weeks also, the mean stain area was more in group I and group III in comparison to group II, but it was not significant.
Table 2.
Inter-group comparisons of mean stain intensity after 1, 2, and 3 weeks
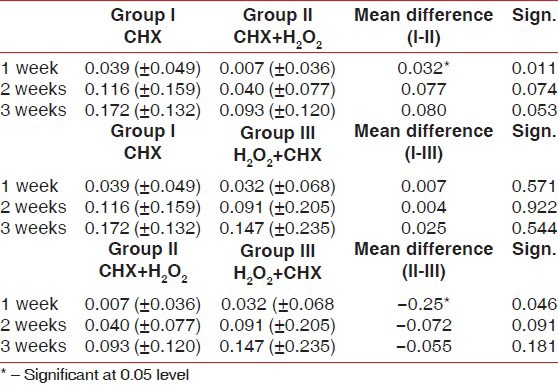
Table 4.
Inter-group comparisons of mean plaque scores after 1, 2, and 3 weeks
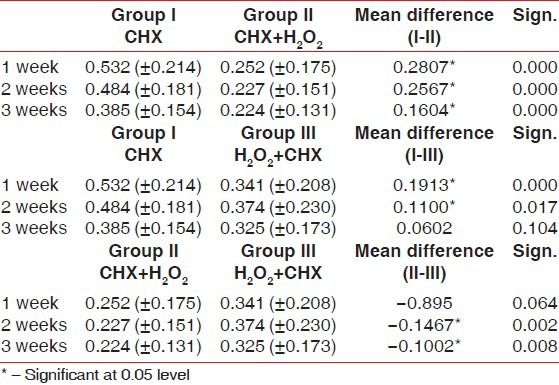
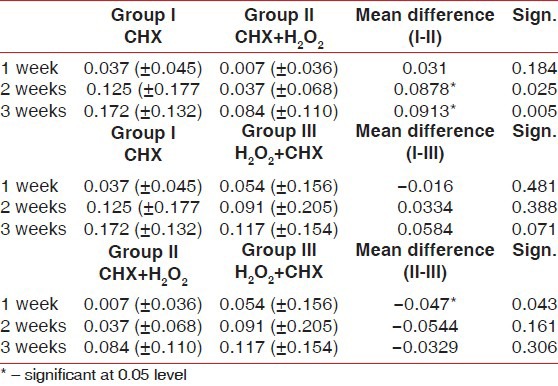
Table 3 demonstrates the comparisons of mean intensity scores between the 3 groups. At the end of 2nd and 3rd week, in comparison to group I, there was significantly less mean stain intensity in group II (P values 0.025 and 0.005, respectively). Group II also had fewer amounts of stains than group III after 2nd and 3rd week but the difference was non-significant (P values 0.061 and 0.306, respectively). The mean stain intensity was less in group III after 1, 2, and 3 weeks in comparison to group I but it was non-significant.
Table 3.
Inter-group comparisons of mean stain intensity after 1, 2, and 3 weeks
There was less amount of plaque formed in group II than group I after the end of 1st, 2nd, and 3rd week and the difference was highly significant (P values: 000, 0.000, and 0.000, respectively [Table 4]. After the end of second and third week, there was a significant reduction in plaque scores in group II in comparison with group III (P values, 0.002 and 0.008, respectively). In comparison to group I, there was significantly less amount of plaque formed in group III after the end of first (P value, 0.000) and second week (0.017). After the end of 3 weeks also, the plaque scores were less in group III than group I but it was not significant (P value, 0.104).
DISCUSSION
The association between dental plaque and gingivitis has been well established, and the importance of effective plaque control has been emphasized over the years. Till date, mechanical plaque elimination with assorted devices remains the primary and most widely accepted means of controlling plaque and maintaining good oral hygiene. As an adjunct to mechanical methods, chemical plaque control comprising of a variety of chemotherapeutic agents have been beneficial and desirable.[14] The greatest success has been with chlorhexidine, which is now considered the gold standard against which other potential antiplaque agents are measured.[15] However, the local side effects of chlorhexidine, particularly extrinsic staining and taste aberrations, have limited its long-term use in oral hygiene products.
The present study was initiated to evaluate the inhibitory properties of H2O2 on extrinsic stains induced by rinsing with CHX. The effect of H2O2 when used in combination with CHX on reducing plaque formation was also evaluated.
The results of the present study show a tendency toward less stain development when CHX is used in combination with H2O2 as compared to using it alone, as is evident from Tables 2 and 3. At the end of 2nd week, the intensity of stains was significantly less in group II in comparison with group I. At the end of 1st week, group II showed significantly less stain intensity in comparison to group III; thus indicating more efficiency of CHX + H2O2 regimen over H2O2 + CHX regimen. This finding has been supported in the study done by Eriksen et al.,[16] in a group of 50 military recruits. In a double-blind experimental design, the combination of 0.2% chlorhexidine and 1% peroxymonosulfate solution resulted in a marked reduction in extrinsic tooth discoloration along with maintained plaque preventive capacity of chlorhexidine. Similar results were obtained in the study done by Grundemann et al.,[10] who demonstrated that combination of chlorhexidine and peroxyborate (CHX + PER) resulted in less stains than CHX alone at the end of 14 days of rinsing.
There is however no doubt that chlorhexidine readily binds food dyes and chromogens to surfaces. Eriksen et al.,[16] indicated that chlorhexidine treatment alters the incorporation into plaque of a natural sulphur-containing organic component of saliva or bacteria. This natural component appears to readily interact with transition metals, particularly iron, producing stained material. Both ferric and stannic sulphides are strongly colored. These colors correlate well with clinically observed extrinsic discolorations. In a more oxidized state, these sulfide compounds transform into sulfates which generally become greyish/white and soluble. This may be an explanation of why rinsing with an oxidizing solution inhibits the staining of teeth.[17] Our study compared three different regimens: Post-brushing rinsing twice daily with chlorhexidine (CHX:CHX), chlorhexidine 0.2% followed by hydrogen peroxide 1.5% (CHX + H2O2:CHX + H2O2); and hydrogen peroxide followed by chlorhexidine (H2O2 + CHX:H2O2 + CHX). The regimens CHX + H2O2:CHX + H2O2 and H2O2 + CHX:H2O2 + CHX were more effective in inhibiting plaque than regimen CHX:CHX. The mean plaque scores in group II and group III after the end of 1and 2 weeks were significantly less than group I as shown in Table 4. After 3 weeks, there was a non-significant difference in plaque scores between group I and group III; group III being better of the two. However, in group II, the plaque scores were significantly less than the other two groups after the end of 1, 2, and 3 weeks. This is in agreement with a previous study by Dona et al.,[9] in which an adjunctive effect of sodium-perborate on the plaque-reducing effect of chlorhexidine was found.
The results of present study show that the therapeutic action of chlorhexidine 0.2% to inhibit supragingival plaque does not seem to be disturbed when it is used together with hydrogen peroxide solution. Rather rinsing with chlorhexidine with hydrogen peroxide combination even enhances plaque inhibition. This could be an additive effect since both chemicals have a different action with regards to bacterial killing. As an antiplaque mouth rinse, the mode of action of chlorhexidine is purely topical. Seymour and Heasman[18] in 1992 stated that killing of bacterial cells is initially dependant on the drug having access to the cell walls. The therapeutic action of hydrogen peroxide is obtained by the release of oxygen that instantly kills the obligate anaerobes implicated in oral infections.[19]
It has been hypothesized that sodium lauryl sulphate (SLS), the most widely used detergent in dentifrice, may counteract with chlorhexidine. A study was done by Van Strydonck et al.,[20] in 2004 and 2006[21] to compare the plaque inhibitory effect of a 0.2% chlorhexidine digluconate rinse when preceded by ordinary tooth brushing with a 1.5% SLS-containing dentifrice to the effect of the same rinse when used alone or when preceded by rinsing with an SLS-containing slurry. The study showed that the anti-plaque efficacy of a 0.2% CHX rinse was not reduced when preceded by everyday tooth brushing with a SLS-containing dentifrice.
CONCLUSION
From this study, it can be concluded that a combination of CHX + H2O2 is superior to CHX alone, when used as mouthwash as an adjunct to routine mechanical tooth cleansing. A twice daily rinsing with CHX + H2O2 combination can be safely recommended to minimize extrinsic tooth discoloration without affecting the plaque inhibiting efficacy of CHX since the removal of stains caused by using CHX alone, especially in pits and fissures, is a tedious procedure for a periodontist. The combination enhances the efficacy of chlorhexidine in reducing plaque formation.
ACKNOWLEDGMENT
I thank all the B.D.S. and Dental hygienist students, and the patients who agreed to take part in this study, and Government Dental College Shimla administration for their help and support.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Jan AM, Verkade H, Timmerman MF, Van der Weijden FA. Comparison of two commercial chlorhexidine mouthwashes. J Periodontol. 2003;74:214–8. doi: 10.1902/jop.2003.74.2.214. [DOI] [PubMed] [Google Scholar]
- 2.Lindhe J, Karring T, Lang NP. 4th ed. Oxford: Blackwell Munksgaard; 2003. Clinical Periodontology and Implant Dentistry. [Google Scholar]
- 3.Francesso AG, Sampathkumar P, Beatrice E. Microbiological and clinical effects of chlorhexidine digluconate and hydrogen peroxide mouthrinse on developing plaque and gingivitis. J Clin Periodontol. 1988;15:60–7. doi: 10.1111/j.1600-051x.1988.tb01556.x. [DOI] [PubMed] [Google Scholar]
- 4.Fischman SL. History of oral hygiene products. How far we have come in 6000 years? Periodontol 2000. 1997;15:7–14. doi: 10.1111/j.1600-0757.1997.tb00099.x. [DOI] [PubMed] [Google Scholar]
- 5.Addy M. Chlorhexidine compared with other locally delivered antimicrobials. J Clin Periodontol. 1986;13:957–64. doi: 10.1111/j.1600-051x.1986.tb01434.x. [DOI] [PubMed] [Google Scholar]
- 6.Löe H, Schiott CR. The effect of mouthrinse and topical application of chlorhexidine on development of dental plaque and gingivitis in man. J Periodontal Res. 1970;5:79–83. doi: 10.1111/j.1600-0765.1970.tb00696.x. [DOI] [PubMed] [Google Scholar]
- 7.Guiseppe P, Rosario G, imburgia M. The effect of antimicrobial sprays and mouthrinses on supragingival plaque regrowth. A comparative study. J Periodontol. 2006;77:248–56. doi: 10.1902/jop.2006.050116. [DOI] [PubMed] [Google Scholar]
- 8.Herrera D, Roldán S, Santacruz I, Santos S, Masdevall M, Sanz M. Differences in antimicrobial activity of four commercial 0.12% chlorhexidine mouthrinse formulations: An in vitro contact test and salivary bacterial counts study. J Clin Periodontol. 2003;30:307–14. doi: 10.1034/j.1600-051x.2003.00341.x. [DOI] [PubMed] [Google Scholar]
- 9.Donna BL, Grundeman LJ, Steinfort J, Timmerman MF, van der Weijden GA. The inhibitory effect of combining chlorhexidine and hydrogen peroxide on 3 day plaque accumulation. J Clin Periodontol. 1998;25:879–83. doi: 10.1111/j.1600-051x.1998.tb02385.x. [DOI] [PubMed] [Google Scholar]
- 10.Grundeman LJ, Timmerman MF. Stain and plaque reduction by combining chlorhexidine and perborate. J Clin Periodontol. 2000;27:9–15. doi: 10.1034/j.1600-051x.2000.027001009.x. [DOI] [PubMed] [Google Scholar]
- 11.Paraskevas S, Danser MM, Timmerman MF, Van der Velden U, Van der Weijden GA. Optimal rinsing time of intra-oral distribution (spread) of mouthwashes. J Clin Periodontol. 2005;32:665–9. doi: 10.1111/j.1600-051X.2005.00731.x. [DOI] [PubMed] [Google Scholar]
- 12.Macpherson LM, Stephen KW, Joiner A, Schafer F, Huntington E. Comparison of a conventional and modified tooth stain index. J Clin Periodontol. 2000;27:854–9. doi: 10.1034/j.1600-051x.2000.027011854.x. [DOI] [PubMed] [Google Scholar]
- 13.Turesky S, Gilmore N, Glickman I. Reduced plaque formation by chloromethyl analogue of Vitamin C. J Periodontol. 1970;41:41–3. doi: 10.1902/jop.1970.41.41.41. [DOI] [PubMed] [Google Scholar]
- 14.Wu CD, Savitt ED. Evaluation of the safety and efficacy of over-the-counter oral hygiene products for the reduction and control of plaque and gingivitis. Periodontol 2000. 2002;28:91–105. doi: 10.1034/j.1600-0757.2002.280105.x. [DOI] [PubMed] [Google Scholar]
- 15.Klausen B, Hougen HP, Hjort Eriksen W, Fiehn NE. The role of supragingival plaque in the prevention and treatment of periodontal disease: A review of current concepts. J Periodontal Res. 1986;21:5–22. [Google Scholar]
- 16.Eriksen HM, Solheim H, Nordbø H. Chemical plaque control and prevention of extrinsic tooth discoloration in vivo. Acta Odontol Scand. 1983;41:87–91. doi: 10.3109/00016358309162307. [DOI] [PubMed] [Google Scholar]
- 17.McKenzie WT, Forgas L, Vernino AR, Parker D, Limestall JD. Comparison of a 0.12% chlorhexidine mouthrinse and an essential oil mouthrinse on oral health in institutionalized, mentally handicapped adults: One-year results. J Periodontol. 1992;63:187–93. doi: 10.1902/jop.1992.63.3.187. [DOI] [PubMed] [Google Scholar]
- 18.Seymour RA, Heasman PA. Drugs, diseases, and the periodontium. New York: Oxford University Press; 1992. Anti-Plaque and anti-calculus agents; pp. 153–79. [Google Scholar]
- 19.Moran J, Addy M, Wade W, Milson S, McAndrew R, Newcombe RG. The effect of oxidising mouthrinses compared with chlorhexidine on salivary bacterial counts and plaque regrowth. J Clin Periodontol. 1995;22:750–5. doi: 10.1111/j.1600-051x.1995.tb00257.x. [DOI] [PubMed] [Google Scholar]
- 20.Van Strydonck DA, Timmerman MF, Van der Velden U, Van der Weijden GA. The anti-plaque efficacy of a chlorhexidine mouthrinse used in combination with toothbrushing with dentifrice. J Clin Periodontol. 2004;31:691–5. doi: 10.1111/j.1600-051X.2004.00546.x. [DOI] [PubMed] [Google Scholar]
- 21.Van Strydonck DA, Timmerman MF, Van der Velden U, Van der Weijden GA. chlorhexidine mouthrinse in combination with an SLS-containing dentifrice and dentifrice slurry. J Clin Periodontol. 2006;33:340–4. doi: 10.1111/j.1600-051X.2006.00910.x. [DOI] [PubMed] [Google Scholar]


