Abstract
Gingival enlargement related to pregnancy is sometimes seen in the oral cavity. Pregnancy is a physiological state that brings full of changes in a woman's life. The metabolism and immunology of the body are modified by progesterone and estrogen as well as other local factors, these sex hormones may modify the oral mucosa and may lead to various periodontal diseases. A case of female patient 23 yrs of age reported during 8th month of pregnancy with a localised gingival enlargement affecting the buccal aspect of left maxillary central incisor upto canine. The hormonal changes occurring during pregnancy may be associated with generalized or localised gingival enlargement and the presence of local factors may accentuate the gingival response. Rarely the enlargement becomes maasive and protrude out extraorally.
Keywords: Gingival enlargement, periodontal disease, pregnancy
INTRODUCTION
Pregnancy has far reaching systemic effects extending beyond the reproductive system involving complex physical and psychological changes that have an impact on even the healthy woman. These effects occur mainly due to hormones on almost every organ system.[1,2] Progesterone is the main sex pregnancy hormone. The level of it rises until the 8th month of pregnancy and after that it becomes stable until giving birth. The estrogen level rises slowly until the end of the pregnancy.[3] The high level of hormones in blood and saliva may cause some periodontal reaction and may increase or cause periodontal disorders. The gingival enlargement has been associated with a variety of local and systemic factors so differential diagnosis becomes an important aspect for complete management of the lesion. Most of the causative factors lead to an unusual hyperplastic tissue response to chronic inflammation associated with local irritants such as plaque, calculus or bacteria and their products.[4] Hormonal changes occurring during pregnancy and puberty, have been known to be associated with varying types of gingival enlargement. Hormonal changes can significantly potentiate the effects of local irritants on gingival connective tissue.[5]
In all forms of enlargements, good oral hygiene is necessary to minimize the effects of systemic factors, Gingivoplasty or Gingivectomy may be required after pregnancy, but should be performed in combination with prophylaxis and oral hygiene instructions.[6] Pregnancy gingival tumor is a disorder found in 0.2-0.5% of the pregnant females. It is a benign rapidly growing lesion occurring usually in 1st trimester of pregnancy and extends up to 3rd trimester. Pregnancy tumor is a smooth or lobulated exophytic lesion with a pedunculated or sessile base. This paper presents a case report of a pregnancy associated aggressive gingival enlargement of enormous size.
CASE REPORT
A 23-year-old female patient reported to the Department of Periodontics, with a localized massive gingival overgrowth on the upper left front region In relation to 21, 22 and 23 with protruding lips [Figures 1–4]. There was no history of drug intake and hereditary reasons. Patient was 8 months pregnant and revealed that her gums used to bleed on brushing since 3 months of pregnancy, but the enlargement came to the present size at this time, the patient reported that she felt difficulty in chewing, speech and closing of the lips, her esthetics was also compromised because of the enlargement. The gingival swelling was so massive that it was evident extraorally. On intraoral examination, the size of the lesion was about 3.5 cm × 2 cm in dimension and pedunculated. The tumor was bright red in color, soft that bled on slightest provocation. Subgingival calculus and plaque was present. Patient was unable to maintain oral hygiene in this area, because of gingival enlargement. Oral prophylaxis was performed after routine hematological investigation. Instructions regarding maintenance of oral hygiene were given and advised to return post-partum. She reported to the department 1 month after the delivery of the baby. The dimension of the tumor was same as before delivery. Minimum bone loss was observed on radiograph The gingival overgrowth was excised with the help of 15 no. b.p blade and electrocautery, the bleeding was controlled by the help of the ball tip of the electrocautery [Figures 5 and 6]. Periodontal dressing was Applied(coe-pack) in the involved region [Figure 7]. The excised lesion [Figure 8] was sent for histopathological examination, which revealed epithelial proliferation and underlying capillary proliferation along with marked inflammatory cell infiltration seen [Figure 9]. The healing was uneventful and no relapse was seen on follow up [Figure 10].
Figure 1.

Gingival enlargement i.r.t 21, 22 and 23 during 8th month of pregnancy
Figure 4.

Gingival enlargement during post-partum period
Figure 5.
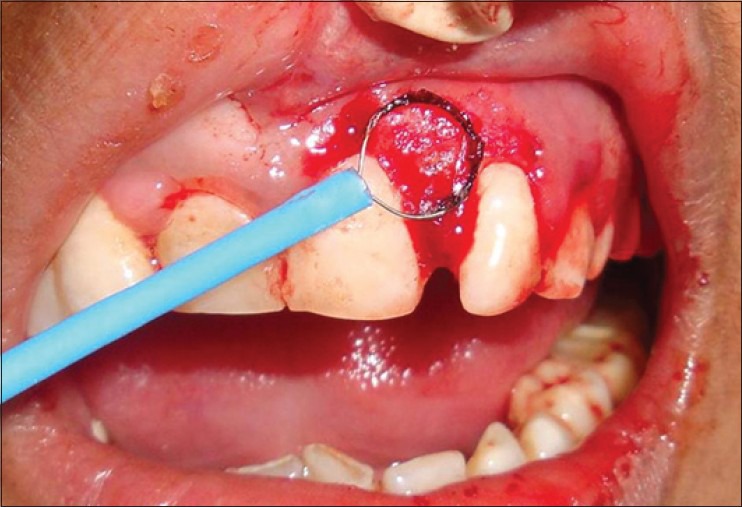
Use of electrocautery
Figure 6.

After excision of the massive gingival enlargement
Figure 7.

Periodontal dressing given
Figure 8.

Excised tissue
Figure 9.
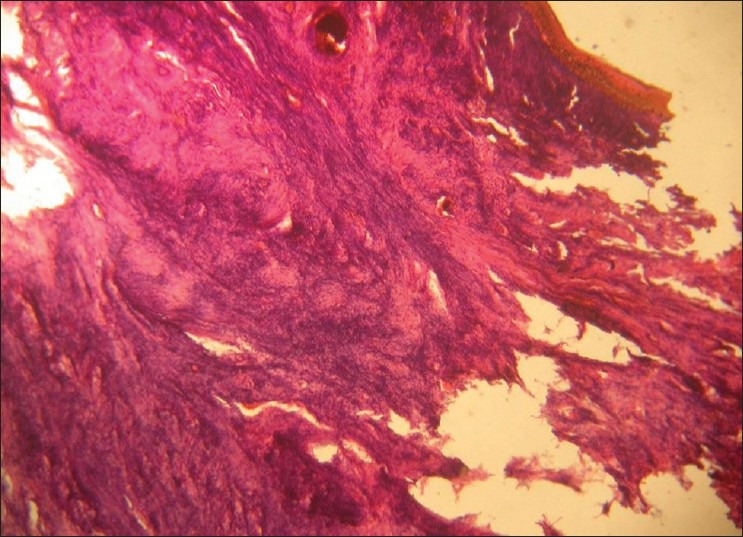
Histopathological photograph
Figure 10.

Post-operative after 1 month
Figure 2.

Gingival enlargement extraoral view
Figure 3.

Side view
DISCUSSION
Pyogenic granuloma is a non-neoplastic inflammatory hyperplasia in response to bacterial plaque and due to chronic local irritation and trauma. The lesion is common in marginal gingival. High level of sex hormones in pregnancy modifies the vascular response resulting in formation of pyogenic granuloma or in pregnancy called as pregnancy tumor. The gingival changes in pregnancy were described as early as 1898 by Pinard. Gingivitis in pregnancy is caused by bacterial plaque, like in non-pregnant individuals. Pregnancy accentuates the gingival response to plaque. The incidence of gingivitis in pregnancy varies from around 50 to 100%. Pregnancy does not alter the healthy gingiva, it effects the severity of previously inflamed area. In some cases, the inflamed gingiva forms a discrete mass referred to as pregnancy tumor.[7] Kornman and Loesch (1980) reported that the subgingival flora changes to a more anaerobic flora as pregnancy progresses Prevotella intermedia is the microorganism that increases significantly during pregnancy.[8] They also stated that the increase is due to elevations of levels of systemic estradiol and progesterone. O’Neil (1979) suggested that the altered tissue response to plaque is due to depression of the maternal T lymphocyte.[9] Formicola et al. and Associates (1970) have shown that gingiva is a target organ for female sex hormones.[10] Therefore, the maintenance of oral hygiene before and during pregnancy is very important in order to reduce the incidence and the severity of gingival inflammation. It is generally accepted that increase in gingival inflammation typically begins in the 2nd month and reaches the maximal level during the 8th month of pregnancy. These inflammatory changes may lead to gingiva that appears edematous, hyperplastic and erythematous; the changes may be localized or generalized and are usually noted on the marginal gingiva and interdental papilla.[11,12]
The size and appearance of lesion in this case is not so common, visible extraorally and of nearly 3.5 cm wide. Excisional surgery is the treatment of choice preferably after pregnancy by various methods such as scalpel, electrocautery or laser. Surgery by electrocautery and laser helps in preventing blood loss as pregnancy tumor is highly vascularized tissue. Recurrence can occur if oral hygiene maintenance is not followed. The surgical treatment should await parturition as sometimes lesional shrinkage occur but if granuloma interferes with mastication then surgery should be performed during second trimester under care.
SUMMARY AND CONCLUSION
The local factors, i.e., plaque and calculus are known to be responsible for gingival enlargement during pregnancy. The hormonal factors also play a role in aggravating the hyperplasia. Therefore, the importance of regular check-up and oral prophylaxis cannot be overlooked. In all forms of gingival enlargements, good oral hygiene is necessary to minimize the effects of systemic factors. In the present case, the massive size of the hyperplastic tissue was excised by surgical excision and the Contouring was done and bleeding was checked by electrocautery, thus relieving the patient from difficulty in speech, chewing, closing of lips and esthetics.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Gajendra S, Kumar JV. Oral health and pregnancy: A review. N Y State Dent J. 2004;70:40–4. [PubMed] [Google Scholar]
- 2.Barak S, Oettinger-Barak O, Oettinger M, Machtei EE, Peled M, Ohel G. Common oral manifestations during pregnancy: A review. Obstet Gynecol Surv. 2003;58:624–8. doi: 10.1097/01.OGX.0000083542.14439.CF. [DOI] [PubMed] [Google Scholar]
- 3.Laine MA. Effect of pregnancy on periodontal and dental health. Acta Odontol Scand. 2002;60:257–64. doi: 10.1080/00016350260248210. [DOI] [PubMed] [Google Scholar]
- 4.Regezi JA, Sciubba J, editors. 2nd ed. Philadelphia: Saunders WB; 1993. Oral Pathology, Clinical Pathological Correlations; pp. 196–202. [Google Scholar]
- 5.Daley TD, Nartey NO, Wysocki GP. Pregnancy tumor: An analysis. Oral Surg Oral Med Oral Pathol. 1991;72:196–9. doi: 10.1016/0030-4220(91)90163-7. [DOI] [PubMed] [Google Scholar]
- 6.Maier AW, Orban B. Gingivitis in pregnancy. Oral Surg Oral Med Oral Pathol. 1949;2:334–73. doi: 10.1016/0030-4220(49)90365-5. [DOI] [PubMed] [Google Scholar]
- 7.Cohen DW, Shapiro J, Friedman L, Kyle GC, Franklin S. A longitudinal investigation of the periodontal changes during pregnancy and fifteen months post-partum. II. J Periodontol. 1971;42:653–7. doi: 10.1902/jop.1971.42.10.653. [DOI] [PubMed] [Google Scholar]
- 8.Kornman KS, Loesche WJ. The subgingival microbial flora during pregnancy. J Periodontal Res. 1980;15:111–22. doi: 10.1111/j.1600-0765.1980.tb00265.x. [DOI] [PubMed] [Google Scholar]
- 9.O’Neil TC. Maternal T-lymphocyte response and gingivitis in pregnancy. J Periodontol. 1979;50:178–84. doi: 10.1902/jop.1979.50.4.178. [DOI] [PubMed] [Google Scholar]
- 10.Formicola AJ, Weatherford T, 3rd, Grupe H., Jr The uptake of H3-estradiol by the oral tissues of rats. J Periodontal Res. 1970;5:269–75. doi: 10.1111/j.1600-0765.1970.tb00728.x. [DOI] [PubMed] [Google Scholar]
- 11.Offenbacher S, Lin D, Strauss R, McKaig R, Irving J, Barros SP, et al. Effects of periodontal therapy during pregnancy on periodontal status, biologic parameters, and pregnancy outcomes: A pilot study. J Periodontol. 2006;77:2011–24. doi: 10.1902/jop.2006.060047. [DOI] [PubMed] [Google Scholar]
- 12.Clothier B, Stringer M, Jeffcoat MK. Periodontal disease and pregnancy outcomes: Exposure, risk and intervention. Best Pract Res Clin Obstet Gynaecol. 2007;21:451–66. doi: 10.1016/j.bpobgyn.2007.01.005. [DOI] [PubMed] [Google Scholar]


