Abstract
Peripheral ossifying fibroma (POF) is one of the inflammatory reactive hyperplasia of gingiva. It represents a separate clinical entity rather than a transitional form of pyogenic granuloma and shares unique clinical characteristics and diverse histopathological features. We present a case of POF in a 65-year-old male patient in the posterior maxillary gingiva, the clinical presentation of which differs from the usual presentation. Differential diagnosis and some interesting facts of POF are discussed.
Keywords: Calcifications, gingival hyperplasia, ossifying fibroma
INTRODUCTION
Peripheral ossifying fibroma (POF) is a non-neoplastic entity, which occurs on the gingiva in response to trauma or irritation. It is a reactive lesion of connective tissue and is not the soft-tissue counterpart of central ossifying fibroma. It is reported under bewildering array of terms in literature, which includes peripheral cementifying fibroma, calcifying or ossifying fibroid epulis, mineralizing ossifying pyogenic granuloma, peripheral fibroma with calcifications and calcifying fibroblastic granuloma.[1]
POF was first reported by the Shepherd in 1844 as alveolar exostosis.[1] Eversol and Robin in 1972, later coined the term peripheral ossifying fibroma.[1] It occurs in the younger age group with a female preponderance. It has a predilection for maxillary arch and most of them occur in the incisor-cuspid region. It presents as a painless mass on gingiva or alveolar mucosa measuring not exceeding 3 cm. It can be pedunculated or sessile. Earlier lesions appear irregular and red and older lesions have a smooth pink surface. Surface ulceration may be present.[2]
POF occurring in an older age group in male patient involving posterior maxilla is rare and an unusual clinical presentation. We attempt to report one such rare case with emphasis on compilation of interesting facts pertaining to POF.
CASE REPORT
A 65-year-old man visited the Department of Periodontics, Hasanambha Dental College and Hospital with a history of a swelling that had gradually increased in size during previous 2 years. He had no history of previous swelling in the oral cavity. Past medical and family history was non-contributory.
Intra oral examination revealed a solitary, pedunculated mass involving buccal interdental papilla and attached gingiva in relation to 26 and 27 [Figure 1]. Mass was pink in color with a smooth surface, measuring approximately 1.5 cm × 2 cm. No surface ulceration was noted. On palpation, it was non-tender and firm in consistency.
Figure 1.

Intra oral picture showing gingival mass with respect to 26 and 27
Intra oral periapical radiograph showed no significant bony changes. Provisional diagnosis of POF was considered.
Thorough scaling and root planning was performed to eliminate the irritating factors and after a week, complete surgical excision of the lesion was performed under local anesthesia. To prevent recurrence, complete removal of the lesion and gingival curettage is ensured followed by oral hygiene maintenance instructions to the patient.
Microscopic examination showed fibro-cellular connective tissue interspersed with plump fibroblasts in between the collagen bundles, surfaced by parakeratinzed stratified squamous epithelium [Figure 2]. Stroma showed large trabeculae of lamellar bone [Figure 3] and scattered basophilic, cementum like substances [Figure 4]. The histopathological features were diagnostic of peripheral ossifying fibroma.
Figure 2.
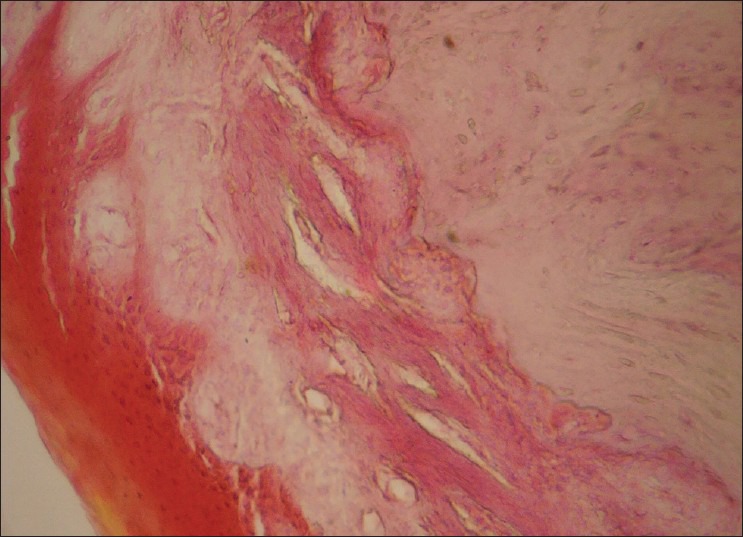
Photomicrograph showing fibro-cellular stroma with surface epithelium, (H and E, ×10)
Figure 3.
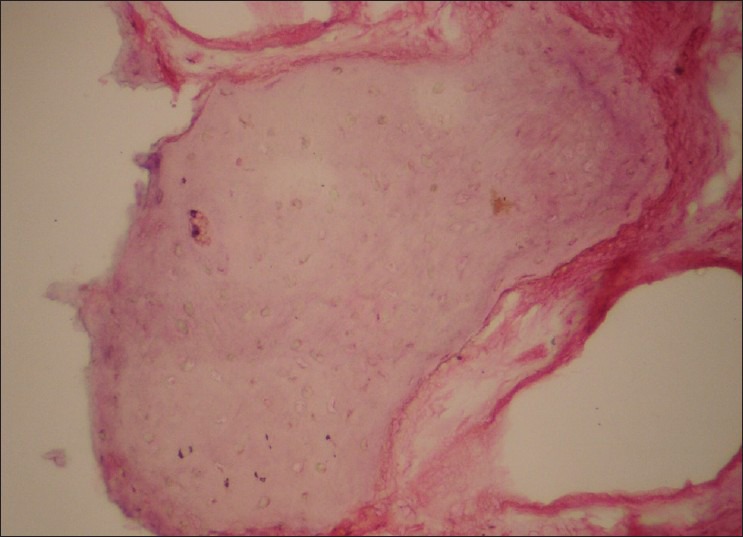
Trabeculae of lamellar bone, (H and E, ×40)
Figure 4.
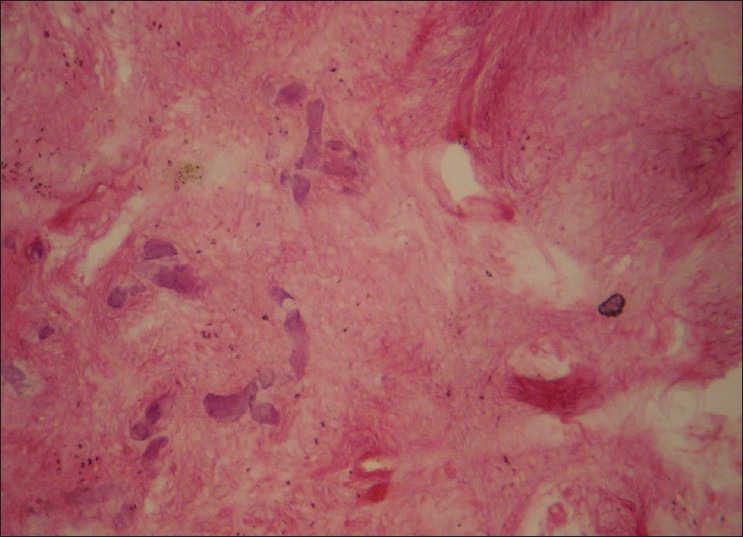
Scattered basophilic material, (H and E, ×10)
Healing was uneventful [Figure 5] and patient is followed-up for 12 months without any recurrence.
Figure 5.

Post-operative view with 10 months follow-up
DISCUSSION
Gingiva is one of those anatomical regions in the oral cavity with the broadest array of lesions occurring ranging from inflammatory to neoplastic. POF is one such reactive lesion, which occurs exclusively on gingiva. It accounts for 9.6% of gingival lesions.[3]
Histogenesis remains controversial and there are two schools of thought proposed to understand the histogenesis
of POF.
POF may initially develop as pyogenic granuloma that undergoes subsequent fibrous maturation and calcification. It represents the progressive stage of the same spectrum of pathosis.[4]
POF is due to inflammatory hyperplasia of cells of periodontal ligament/periosteum. Metaplasia of the connective tissue leads to dystrophic calcification and bone formation.[5]
Triggering factors such as subgingival plaque and calculus, dental appliances, poor quality of dental restorations, micro-organisms and food lodgement initiate the inflammatory response.[6]
Clinically POF presents as smooth lobulated pink mass on a pedunculated or sessile base. It has an increasing incidence in II decade and declining incidence after III decade.[7] Only 0.5% cases are reported in older age group.[1] There is a female predilection for the lesion due to the hormonal influences.[8] POF is usually seen anterior to molars, especially in incisor-canine region.[9] Kfir et al. reported that the size of the POF is usually smaller than 1.5 cm in diameter. A case of giant POF of 9 cm is reported in the literature.[10] Multicentric POF can also occur in oral and maxillofacial region[7] and is observed in genetic associated conditions like:
Nevoid basal cell carcinoma syndrome
Multiple endocrine neoplasia-type II
Neurofibromatosis
Gardner syndrome.[7]
POF has to be differentiated from other reactive lesions of a gingiva such as pyogenic granuloma, peripheral giant cell granuloma (PGCG) and peripheral odontogenic fibroma. Pyogenic granuloma shows red mass with surface ulceration clinically and microscopically exhibit vascular proliferation resembling granulation tissue. PGCG shows scattered giant cells in a fibrous stroma. Peripheral odontogenic fibroma contains prominent islands of odontogenic epithelium.[5] Bone involvement, though not significant in most of the cases, some alterations are noted like:
Superficial erosion of bone
Foci of calcifications
Widening of the periodontal ligament space and thickened lamina dura[5]
Migration of teeth with Interdental bone loss.[2]
The basic microscopic pattern of the POF is fibrous proliferation associated with the formation of mineralized components. Mineralized component varies from 23 to 75%.[7] Butcher and Hansen reported three types of components in POF.[9]
Dystrophic calcifications
Bone (woven/lamellar)
Cementum.
Behavior of POF
Cundiff observed 16% recurrence rate and a series studied by Eversole and Robin showed 20% recurrence rate.[7] Mesquita et al. found higher number of argyrophilic nucleolar organizer region and proliferating cell nuclear antigen positive cells in POF indicating the high proliferative activity of the lesion, which may influence the treatment modalities.[1]
What is the evidence for the origin of POF?
POF is thought to arise from the cells of the periodontal ligament.[1]
Exclusive occurrence in the gingiva
Close proximity of a gingiva to the periodontal ligament
Presence of oxytalan fibers with in mineralized matrix.
Why POF shows female preponderance?
Role of hormones has been suggested. Exposure of inflamed gingiva to progesterone and estrogen from saliva and blood stream is thought to be a contributory factor.[8]
Why POF is common in younger age group?
Loss of periodontium occurs with tooth loss as age advances. Hence marked predilection is seen in younger age group.[1]
POF versus peripheral cemento-ossifying fibroma?
Hard tissues can be elaborated in the form of bone, cementum and spheroidal calcifications, which allows for various nomenclatures. If bone predominates, the word “ossifying” is used and if cementum predominates, “cementifying” term can be used. If both, bone and cementum are observed, it can be called “cemento-ossifying fibroma.”[5]
The term cemento-ossifying is scientifically invalid as there is no histochemical or biochemical differences between bone and cementum. Besides, histopathology of ossifying fibromas occurring in areas such as skull, femur and tibia, where cementum is absent, also show similar histopathology.[5]
CONCLUSION
POF is a pathological entity whose histogenesis is yet to be delineated. It shares a varied clinic-pathological presentation. Substantial overlap exists between various focal reactive overgrowths of gingiva. Clinico-pathological characteristics may vary and on the contrary to the usual presentation, our case presented a different age, sex and site of POF. Surgical excision is considered curative and may present a high recurrence rate compared with other reactive lesions. Identification of any reactive lesions requires the formulation of differential diagnosis to enable accurate patient evaluation and management.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Reddy GV, Reddy J, Ramlal G, Ambati M. Peripheral ossifying fibroma: Report of two unusual cases. Indian J Stomatol. 2011;2:130–3. [Google Scholar]
- 2.Sharma S, Anamika S, Ramachandra SS. Peripheral ossifying fibroma: A clincal report. Compend Contin Educ Dent. 2011;32:E86–90. [PubMed] [Google Scholar]
- 3.Mishra MB, Bhishen KA, Mishra S. Peripheral ossifying fibroma. J Oral Maxillofac Pathol. 2011;15:65–8. doi: 10.4103/0973-029X.80023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Prasad S, Reddy SB, Patil SR, Kalburgi NB, Puranik RS. Peripheral ossifying fibroma and pyogenic granuloma. Are they interrelated? N Y State Dent J. 2008;74:50–2. [PubMed] [Google Scholar]
- 5.Satish BN, Kumar P. Peripheral ossifying fibroma of hard palate: A case report. Int J Dent Clin. 2010;2:30–4. [Google Scholar]
- 6.Chatterjee A, Ajmera N, Singh A. Peripheral cemento-ossifying fibroma of maxilla. J Indian Soc Periodontol. 2010;14:186–9. doi: 10.4103/0972-124X.75915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jain A, Deepa D. Recurrence of peripheral ossifying fibroma: A case report. People's J Sci Res. 2010;3:23–5. [Google Scholar]
- 8.Effiom OA, Adeyemo WL, Soyele OO. Focal reactive lesions of the Gingiva: An analysis of 314 cases at a tertiary Health Institution in Nigeria. Niger Med J. 2011;52:35–40. [PMC free article] [PubMed] [Google Scholar]
- 9.Shetty DC, Urs AB, Ahuja P, Sahu A, Manchanda A, Sirohi Y. Mineralized components and their interpretation in the histogenesis of peripheral ossifying fibroma. Indian J Dent Res. 2011;22:56–61. doi: 10.4103/0970-9290.79976. [DOI] [PubMed] [Google Scholar]
- 10.Poon CK, Kwan PC, Chao SY. Giant peripheral ossifying fibroma of the maxilla: Report of a case. J Oral Maxillofac Surg. 1995;53:695–8. doi: 10.1016/0278-2391(95)90174-4. [DOI] [PubMed] [Google Scholar]


