Abstract
Chronic inflammation has been proposed as an etiological and progression factor in prostate cancer. In this study, we used a dissociated prostate tissue recombination system to interrogate the role of interleukin 6 (IL6) and the related cytokine oncostatin M (OSM) in the initiation and progression of prostate cancer. We identified that prostatic intraepithelial neoplasia (PIN) lesions induced by PTEN loss of function (PTENLOF) progress to invasive adenocarcinoma following paracrine expression of either cytokine. Increased expression of OSM was also able to drive progression of benign human epithelium when combined with constitutively activated AKT. Malignant progression in the mouse was associated with invasion into the surrounding mesenchyme and increased activation of STAT3 in PTENLOF grafts expressing IL6 or OSM. Collectively, our work indicates that pro-inflammatory cytokines such as IL6 or OSM could activate pathways associated with prostate cancer progression and synergize with cell autonomous oncogenic events to promote aggressive malignancy.
Keywords: Prostate carcinoma, PTEN, AKT, Interleukin 6, Oncostatin M
Implications
Increased expression of IL6 or OSM synergizes with loss of PTEN to promote invasive prostate cancer.
Introduction
Chronic inflammation is observed in nearly all forms of cancer and may represent a contributing factor at initiation, progression and metastasis (1). Numerous factors have been proposed to contribute to prostatic inflammation and it has also been proposed to play a role driving in the multifocal nature of prostate cancer (2). Studies employing bacterial colonization of the prostate to elicit chronic inflammatory conditions have observed epithelial reactive hyperplasia and PIN lesions (3). Increased expression of inflammatory cytokines, including members of the IL6 family, has been observed in these models and could represent a functional mechanism (4). Immunohistochemical analysis of human prostate biopsies have shown increased expression of IL6 and the related OSM ligands and their cognate receptors with prostate cancer progression (5). Therefore, we sought to interrogate the role of inflammation by monitoring transformation of prostate epithelial cells in a pro-inflammatory environment induced by ectopic expression of IL6 or the related OSM in the stroma of tissue recombination experiments.
The interleukin-6 family of cytokines consists of several related ligands that share common protein structure and utilization of GP130 signal transducer with receptor adaptors modulating ligand specificity (6). Studies have identified increased serum levels of IL6 in prostate cancer patients correlating to increased clinical stage, hormone refractory disease and metastasis (7,8). Several prostate cancer cell lines have been shown to express IL6 while treatment with either cytokine generally confers a growth advantage (9). Ectopic expression of IL6 can promote castration-resistant conversion in castrate conditions while OSM has been shown to activate AR through an androgen-independent mechanism (9,10). Antibodies targeting IL6 inhibit xenograft growth and castration resistance, though they have shown poor clinical efficacy to date, indicating the need to more fully understand how these molecules function in the tumor microenvironment (11,12).
We sought to interrogate the functional roles of IL6 and OSM in prostate cancer in vivo using a dissociated tissue recombination system developed in our laboratory (13,14). We identified that paracrine expression of either IL6 or OSM is sufficient to promote invasive progression from intermediate PIN lesions induced by PTENLOF in mouse tissues or activation of AKT in human tissues. Increased expression of either IL6 or OSM in the context of PTEN loss resulted in increased activation of STAT3 over PTEN loss alone, indicating a potential molecular mechanism. That cytokines related to IL6 exhibit similar cancer progression behavior indicates that highly targeted therapies aimed solely at disrupting IL6 signaling could be less effective than those targeting signaling nodes common to the IL6 family.
Materials and Methods
Mouse Strains and Regeneration Assay
Housing, maintenance, surgical and experimental procedures were undertaken in compliance with the regulations of the Division of Laboratory Animal Medicine of the University of California, Los Angeles. Homozygous Ptenfl/fl, strain B6.129S4-Ptentm1Hwu/J, were purchased from Jackson Laboratory and maintained in our facility. Lentivirus preparation, titering and infection, and regeneration of dissociated cells were performed as previously described under safety regulations for lentivirus use set by Environmental Health and Safety (EH&S) at University of California, Los Angeles. Briefly, prostate tissue from 6–12 week old male mice was minced, digested and dissociated according to published protocols (13). Dissociated cells (1–2 × 105) were infected with lentivirus at an MOI of 50, recombined with UGSM (1–2 × 105), suspended in a collagen plug and engrafted under the kidney capsule for 6–10 weeks. Grafts were recovered via surgical resection of the kidney and fixed in 10% buffered formalin overnight or flash frozen. UGSM cells were prepared from pregnant C57BL/6 females on embryonic day 14 and cultured in UGSM media [DMEM, 5% FBS, 5% NuSerum (BD #355504), 1X selenium-transferrin-insulin (Gibco #51500-056), 2 mM l-glutamine].
Human prostate regenerations
For primary human cells, we used a protocol approved through the UCLA Office for the Protection of Research Subjects and all human tissue samples were de-identified to protect patient confidentiality. A total of 3 patient samples were used for this study and all specimens were processed as described previously (14). Briefly, surgical prostate specimens were removed and cancerous areas were separated from the benign tissue. Basal epithelial cells were isolated by FACS from dissociated benign tissue using PE-conjugated CD49f (eBiosciences #12-0495-83) and APC-conjugated Trop2 (FAB650A, R&D Systems) antibodies. Cells were stained in PrEGM supplemented with 2.5 μg/ml Fungizone (Gibco) and 10 μm of the p160 ROCK inhibitor Y-27632 dihydrochloride (Tocris Bioscience #1254). Sorting was performed on a BD FACS Aria II (BD Biosciences).
Cell Lines and Cytokine Treatment
PEB cells were a kind gift from Dr. Lynnette Wilson (NYU) maintained in PrEGM (Lonza, # CC-4177 and CC-3165) supplemented with 10% FBS. CaP8 cells were a kind gift from Dr. Hong Wu (UCLA) and maintained in UGSM media. Cell lines were not authenticated. Human recombinant IL6 and OSM were purchased from Cell Signaling (#8904SF and #5367SF, respectively) and were reconstituted in 1X PBS supplemented with 1% BSA. For cytokine treatment assays, cells were serum starved in DMEM supplemented with 0.2% FBS and 2 mM L-glutamine for 6–18 hours and treated with cytokines for indicated times. Results presented are representative of two replicates.
Results
Interleukin 6 and Oncostatin M expression promote progression to invasive prostate cancer in mouse and human tissues
To assess the potential role of IL6 and OSM in transformation of both mouse and human prostate epithelium, we utilized a dissociated prostate regeneration system developed in our laboratory (13,14). For mouse tissues, we used dissociated prostate cells from adult male homozygous Ptenfl/fl conditional knockout mice transduced with either GFP control or Cre-GFP lentivirus that were combined with urogenital sinus mesenchyme (UGSM) transduced with RFP control, IL6-RFP, or OSM-RFP lentivirus (Fig. 1A). Western analysis was used to confirm increased expression and activity of secreted IL6 and OSM in lysates and conditioned media of transduced UGSM (Fig. 1B).
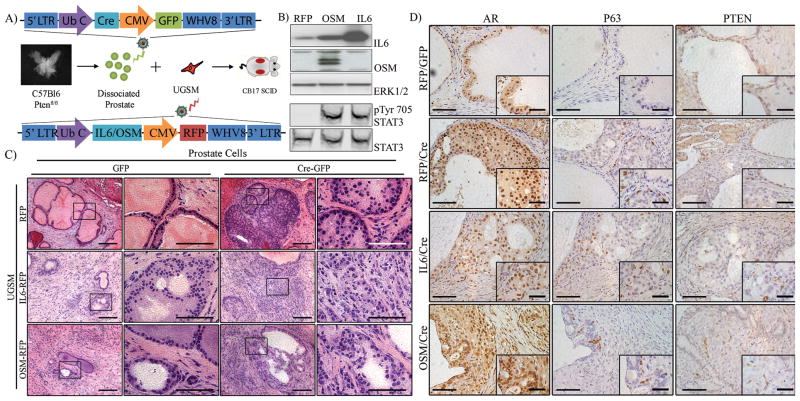
Figure 1. Paracrine expression of IL6 or OSM synergizes with epithelial loss of PTEN to promote invasive adenocarcinoma.
A) Diagram of regeneration and transformation process with lentiviral vector diagrams.
B1–3) Western analysis of UGSM cells infected with control, IL6 and OSM vectors showing heightened expression of IL6 and OSM in their respective cell lines, with a mild increase in IL6 expression in OSM-infected UGSM. Loading control is ERK1/2.
B4–5) Secretion and activity of the IL6 and OSM cytokines was confirmed by treating serum-starved 3T3 cells with conditioned media from infected UGSM. Increased phosphorylation of STAT3 in cells treated with IL6 and OSM conditioned media indicates functional activity. Imaged using Licor Odyssey CLx with Image Studio software.
C) Representative histological sections of prostate regeneration and transformation following 6–8 weeks in vivo. Control grafts exhibit normal prostate epithelial architecture with PTEN-intact grafts expressing either IL6 or OSM exhibited reduced epithelial regeneration while IL6- and OSM-expressing grafts exhibited occasional mild, focal hyperplasia. Grafts with loss of PTEN alone exhibited PIN lesions formation with characteristic neoplastic growth into the luminal interior while tumor foci from PTENLOF with IL6 or OSM exhibited invasion into the surrounding mesenchyme. Scale Bars: 10X, 200 um; 40X, 100 um.
D) IHC analysis of AR and p63 in prostate regenerations. All prostate epithelial regenerations and tumor foci retained high expression of nuclear AR. Normal regenerations exhibited P63-expressing basal cells along the basement membrane and were detached from the membrane in PIN lesions present in PTENLOF grafts and PTENLOF grafts with IL6. High grade lesions present in PTENLOF with OSM exhibited loss of P63-expressing basal cells. Scale Bars: 20X, 100μm; 63X, 50 μm
Control grafts exhibited regeneration of normal prostate cellular architecture while PTENLOF combined with control UGSM resulted in PIN lesion formation (Fig. 1C). PTENLOF combined with UGSM expressing either IL6 or OSM exhibited a heterogeneous range of transformation states, though graft wet weights were not significantly different (Supplemental Fig. S1A-C and Supplemental Table S1). IL6-expressing grafts largely exhibited high-grade PIN lesions and locally invasive growth, with a few poorly differentiated lesions present. OSM-expressing grafts often presented as locally invasive lesions with several regions of poorly differentiated adenocarcinoma with anaplastic features, indicating that OSM could promote a more aggressive disease (Supplemental Fig. S1C). Grafts displayed immunohistochemical features of human prostate cancer including nuclear AR expression and loss of P63-expressing basal cells in high grade lesions (Fig. 1D and Supplemental Fig. S1D). Phenotypically similar results were achieved using autocrine expression of OSM in donor prostate tissue with activated AKT, though grafts with IL6 were significantly inhibited and transformation was not observed (Supplemental Fig. S2). We used immunofluorescent confocal microscopy to qualitatively assess epithelial invasion, using E-cadherin to identify epithelial cells with respect to the basement membrane component collagen IV. Control and PTENLOF grafts exhibited normal e-cadherin localization to the nuclear membrane while IL6 and OSM grafts exhibited disorganized e-cadherin expression with epithelial cells invading into the surrounding mesenchyme (Supplemental Fig. S3).
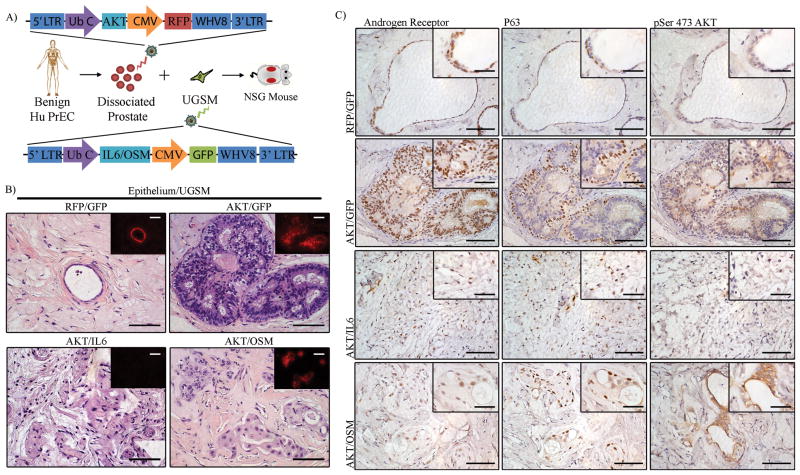
For human experiments, expression of constitutively active AKT was used as a surrogate for PTENLOF. Benign human epithelium was isolated from radical prostatectomy samples and transduced with either RFP or AKT-RFP lentivirus. Transduced cells were then combined with UGSM transduced with GFP, IL6- or OSM-GFP lentivirus, suspended in matrigel and injected subcutaneously into immune deficient hosts (Fig. 2A). Control grafts exhibited normal epithelial regeneration with nuclear AR expression in luminal epithelium and P63 expression in basal cells (Fig. 2B, C and Supplemental Fig. S4A). Expression of activated AKT resulted in PIN lesions similar to those observed in mouse PTEN knockout regenerations (Fig. 2B). Paracrine expression of either IL6 or OSM alone dramatically inhibited epithelial regeneration with only a few small nests of epithelial cells primarily composed of P63-expressing basal cells (Supplemental Fig. S4B). Similarly, paracrine expression of IL6 in grafts with AKT-infected epithelium also exhibited significant inhibition and no epithelial regeneration or transformation was observed (Fig. 2B and C). Grafts expressing OSM with AKT exhibited small nests of dysplastic epithelial cells that express AR, though they retained P63-expressing cells, indicating the lesions had not progressed to clinical adenocarcinoma (Fig. 2B and C). Activation and over-expression of AKT was confirmed by IHC analysis for phospho-serine 473 AKT levels and total protein (Fig. 2C and Supplemental Fig. S4C). The quantification of observed phenotypes is reported in Supplemental Table S2.
Figure 2. Cell autonomous expression of AKT with increased paracrine expression of OSM results in tumor progression of benign human prostate epithelium.
A) Diagram of human prostate regeneration with lentiviral constructs.
B) Representative histology of human prostate epithelial regenerations following 8–10 weeks in vivo. Benign regenerations show normal glandular epithelium while those transduced with AKT show PIN lesion formation. No regeneration or transformation was observed in grafts expressing activated AKT with IL6. Grafts with activated AKT and OSM exhibited dramatic morphological progression. Insets show expression of linked RFP marker to track viral transduction. Scale Bars: 20X, 100 μm; Inset: 20X, 100 μm.
C) IHC analysis of AR and p63 from human prostate regenerations. All grafts and tumor foci retain nuclear expression of AR. Normal regenerations exhibited P63-expressing basal cells along the basement membrane while PIN lesions induced by AKT alone exhibited P63-expressing basal cells detached from the basement membrane similar to murine PIN lesions. Tumor foci from AKT with OSM retain P63 expressing basal cells despite invasive morphological characteristics. Scale Bars: 20X, 100 μm; 63X, 50 μm.
Invasive tumor foci identified in grafts expressing IL6 or OSM with loss of PTEN exhibited increased activation of JAK/STAT pathway
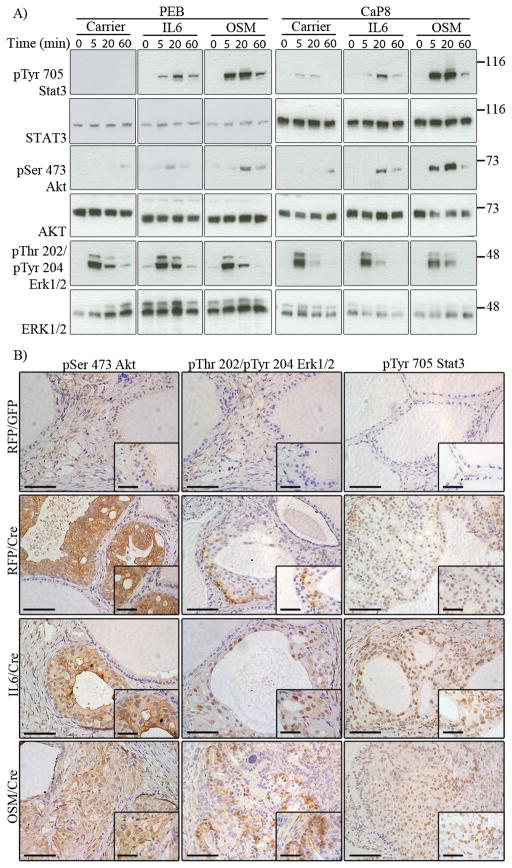
Ligand engagement of IL6-family members activates constitutively associated Janus kinases (JAK), resulting in activation of the STAT, MAPK, and AKT pathways (6). To interrogate whether IL6 and OSM exhibit differential activation of downstream pathways, we treated benign PEB and tumorigenic CaP8 cell lines with human recombinant IL6 and OSM and assessed activation of downstream pathways by western analysis (Fig. 3A). Treatment with IL6 or OSM exhibited increased STAT3 and AKT activation in both PEB and CaP8 cell lines compared to controls, with OSM exhibiting a greater increase over IL6 for both signaling pathways. Neither IL6 nor OSM exhibited a dramatic increase in ERK1/2 activation over carrier treated cells.
Figure 3. Increased expression of OSM in PTENLOF grafts results in increased phosphorylation of STAT3 and ERK1/2 downstream of IL6 and OSM.
A) Western analysis of PEB and CaP8 cells treated with carrier or 10 ng/uL of IL6 or OSM in DMEM with 0.2% FBS for indicated times. Treatment with carrier resulted in transient activation of ERK1/2 in both cell lines with a slight increase in AKT and STAT3 activation. Treatment with either IL6 or OSM exhibited activation of both AKT and STAT3 pathways with OSM consistently exhibiting increased activation over IL6. Activation of ERK1/2 above background was not consistently observed.
B) IHC analysis of AKT, ERK1/2 and STAT3 activation from normal, PTENLOF, and PTENLOF with IL6 or OSM. All grafts with PTENLOF exhibited increased activation of AKT, ERK1/2 and STAT3 above basal levels in normal regenerations. PTENLOF grafts with IL6 exhibited increased levels of STAT3 phosphorylation over PTENLOF alone with no discernible increase in ERK1/2 activation. PTENLOF with OSM exhibited consistently higher levels of STAT3 phosphorylation with a mild increase in ERK1/2 phosphorylation. Scale Bars: 20X 100 μm; 63X, 50 μm.
We used IHC analysis to interrogate activation of pathways downstream of IL6 and OSM from in vivo transformations using mouse tissues (Fig. 3B). Control regenerations exhibited little-to-no activation of AKT, ERK1/2 or STAT3. Increased AKT activation was observed in all PTENLOF lesions and were similar across PTENLOF alone and with IL6 or OSM. PTENLOF resulted in increased ERK1/2 activation over control grafts with similar levels observed in grafts from PTENLOF with IL6 while PTENLOF grafts with OSM exhibited mild, though consistently increased ERK1/2 activation. PTENLOF resulted in increased STAT3 activation compared to control grafts with further increased levels observed in grafts from both PTENLOF with IL6 or OSM. IHC analysis for total proteins confirmed basal expression levels in control grafts with all PTENLOF grafts exhibiting increased expression of total AKT, ERK1/2 and STAT3 protein (Supplemental Fig. S5). These results indicate that tumor progression via IL6 and OSM is associated with increased activation of the STAT pathway, though OSM synergy could be also be mediated in part by MAPK.
Discussion
Correlative and in vitro data strongly indicate that chronic inflammation could act as an etiological and progression factor, highlighting the need for further validation using in vivo models. Our study identified that both IL6 and OSM exhibited synergy with PTENLOF and display heterogeneous transformation phenotypes ranging from high-grade PIN and locally invasive lesions to poorly differentiated adenocarcinoma with anaplastic features. We speculate that this complexity is a result of variations in the local concentration of IL6 or OSM and could serve as a model for the heterogeneity commonly observed in human prostate cancer.
While our work focused on the interaction of IL6 and OSM in the context of PTENLOF, other studies indicate that this synergy could extend to other oncogenic insults. Exogenous expression of IL6 has been shown to transform a non-tumorigenic prostate epithelial cell line immortalized with SV40 Large T-antigen, indicating potential synergy with inhibition of the TP53 and RB pathways (15). Work by Kan and colleagues identified that while OSM suppressed the growth of normal human breast epithelium, co-expression of cMYC abrogated growth arrest and promoted transformation (16). Our results support this finding as neither cytokine was sufficient to transform mouse or human prostate epithelium on its own in our system. Oncogenic response to IL6 and related cytokines therefore seems to be dependent on the presence co-incident mutations within the prostate.
Expression of either IL6 or OSM alone strongly inhibited epithelial regeneration in both mouse and human tissues while studies using prostate cancer cell lines have shown paradoxical effects of either growth promotion or inhibition depending on the cell line. Growth inhibition by IL6-type cytokines in tumor cell lines occurs through a variety of mechanisms including activation of the P27/KIP1 checkpoint (17). A study from Duijn and Trapman indicated that the PI3K/AKT pathway modulated expression of SKP2, which mediated the down-regulation of P27/KIP1 in DU145 and PC3 but not LNCaP cells (18). Intriguingly, this corresponds with published data concerning prostate cancer cell line response to IL6 (9). Activation of the PI3K/AKT pathway by IL6 or OSM in DU145 and PC3 could inhibit the P27/KIP1 checkpoint and promote cell growth, while LNCaP cells do not exhibit this same behavior and thus respond by growth inhibition and differentiation. PTENLOF has been associated with increased levels of SKP2 and decreased levels of P27/KIP1 in human prostate cancer biopsy specimens, indicating that this checkpoint might be bypassed in the context of chronic inflammation with PTENLOF, allowing for increased tumor growth (19).
Sequencing studies indicate that prostate cancer does not exhibit dramatic mutation rates compared to many other cancers (20). Studies from our laboratory and others have shown that most single oncogenes are not sufficient to induce invasive prostate cancer, indicating that it is necessary to activate multiple signaling pathways (14). Both IL6 and OSM have been shown to activate STAT3, AKT, and MAPK in several cell types, while our in vivo studies suggest strong activation of STAT3 with a mild increase in ERK1/2 (6). These pathways have been implicated in nearly all cancers to some degree and several exhibit functional synergy when co-activated. We propose that chronic inflammation could expose tumor cells to a diverse array of cytokines that could activate multiple oncogenic pathways and serve as a surrogate for direct mutation.
Current therapeutic research strategies are increasingly using highly targeted drugs such as antibody-based therapeutics designed to inhibit the IL6 ligand or the IL6Ra subunit. The humanized antibody CNTO328 inhibits the conversion to androgen-independent disease and modulates activation of downstream pathways in prostate cancer xenografts though it has shown poor performance in clinical trials (11,12). Our studies indicate that other members of the IL6 family, and likely other cytokines, can also exhibit pro-tumorigenic functions that can even exceed those of IL6. Highly targeted therapies directed at single ligands such as IL6 could exhibit reduced efficacy due to co-expression of family members with redundant activity. Therapies targeting signaling nodes such as the JAK family could therefore exhibit greater efficacy through inhibition of both related family members and shared downstream pathways such as STAT3 and ERK1/2. Therapeutic strategies such as this would benefit greatly from an increased understanding of how cytokine expression profiles can be used as diagnostic biomarkers.
Supplementary Material
Acknowledgments
We would like to thank all of the members of the Witte laboratory for their helpful comments and insightful discussion and the technicians of the UCLA Translational Pathology Core Laboratory for their assistance in tissue processing and H&E staining. We would also like to especially thank our FACS specialist Dr. Donghui Cheng and Dr. Jioati Huang of the UCLA Pathology department. DAS is supported by UCLA Tumor Biology Program, US Department of Health and Human Services, Ruth L. Kirschstein Institutional National Research Service Award no. T32 CA009056 and is a Collegium of University Teaching Fellow with the University of California, Los Angeles. AK was a visiting Fellow on sabbatical and is a scientist with Takeda Pharmaceutical Company Limited, Kanagawa, Japan. ONW is supported by a Prostate Cancer Foundation Challenge Award (PI: Owen Witte). YZ is an Associate of and ONW is an Investigator for the Howard Hughes Medical Institute.
Footnotes
Conflict of Interest: The authors have no financial or other conflict of interests to disclose.
Author Contributions
Conception and design: D.A. Smith, A. Kiba, Y. Zong, O.N. Witte
Development of methodology: D.A. Smith, A. Kiba, Y. Zong, O.N. Witte
Acquisition of data: D.A. Smith, A. Kiba, Y. Zong
Analysis and interpretation of data: D.A. Smith, A. Kiba, Y. Zong, O.N. Witte
Writing, review and/or revision of the manuscript: D.A. Smith, A. Kiba, Y. Zong, O.N. Witte
Study supervision: O.N. Witte
References
- 1.Hanahan D, Weinberg RA. Hallmarks of Cancer: The Next Generation. Cell. 2011;144:646–74. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 2.De Marzo AM, Platz EA, Sutcliffe S, Xu J, Grönberg H, Drake CG, et al. Inflammation in prostate carcinogenesis. Nat Rev Cancer. 2007;7:256–69. doi: 10.1038/nrc2090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Elkahwaji JE, Hauke RJ, Brawner CM. Chronic bacterial inflammation induces prostatic intraepithelial neoplasia in mouse prostate. British Journal of Cancer. 2009;101:1740–8. doi: 10.1038/sj.bjc.6605370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boehm BJ, Colopy SA, Jerde TJ, Loftus CJ, Bushman W. Acute bacterial inflammation of the mouse prostate. The Prostate. 2012;72:307–17. doi: 10.1002/pros.21433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Royuela M, Ricote M, Parsons MS, García-Tuñón I, Paniagua R, De Miguel MP. Immunohistochemical analysis of the IL-6 family of cytokines and their receptors in benign, hyperplasic, and malignant human prostate. The Journal of Pathology. 2004;202:41–9. doi: 10.1002/path.1476. [DOI] [PubMed] [Google Scholar]
- 6.Heinrich PC, Behrmann I, Haan S, Hermanns HM, Müller-Newen G, Schaper F. Principles of interleukin (IL)-6-type cytokine signalling and its regulation. Biochem J. 2003;374:1–20. doi: 10.1042/BJ20030407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Drachenberg DE, Elgamal AA, Rowbotham R, Peterson M, Murphy GP. Circulating levels of interleukin-6 in patients with hormone refractory prostate cancer. The Prostate. 1999;41:127–33. doi: 10.1002/(sici)1097-0045(19991001)41:2<127::aid-pros7>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 8.Adler HL, McCurdy MA, Kattan MW, Timme TL, Scardino PT, Thompson TC. Elevated levels of circulating interleukin-6 and transforming growth factor-beta1 in patients with metastatic prostatic carcinoma. J Urol. 1999;161:182–7. [PubMed] [Google Scholar]
- 9.Culig Z, Steiner H, Bartsch G, Hobisch A. Interleukin-6 regulation of prostate cancer cell growth. J Cell Biochem. 2005;95:497–505. doi: 10.1002/jcb.20477. [DOI] [PubMed] [Google Scholar]
- 10.Godoy-Tundidor S, Hobisch A, Pfeil K, Bartsch G, Culig Z. Acquisition of Agonistic Properties of Nonsteroidal Antiandrogens after Treatment with Oncostatin M in Prostate Cancer Cells. Clinical Cancer Research. 2002;8:2356–2361. [PubMed] [Google Scholar]
- 11.Wallner L, Dai J, Escara-Wilke J, Zhang J, Yao Z, Lu Y, et al. Inhibition of Interleukin-6 with CNTO328, an Anti-Interleukin-6 Monoclonal Antibody, Inhibits Conversion of Androgen-Dependent Prostate Cancer to an Androgen-Independent Phenotype in Orchiectomized Mice. Cancer Research. 2006;66:3087–95. doi: 10.1158/0008-5472.CAN-05-3447. [DOI] [PubMed] [Google Scholar]
- 12.Fizazi K, De Bono JS, Flechon A, Heidenreich A, Voog E, Davis NB, et al. Randomised phase II study of siltuximab (CNTO 328), an anti-IL-6 monoclonal antibody, in combination with mitoxantrone/prednisone versus mitoxantrone/prednisone alone in metastatic castration-resistant prostate cancer. European Journal of Cancer. 2012;48:85–93. doi: 10.1016/j.ejca.2011.10.014. [DOI] [PubMed] [Google Scholar]
- 13.Lukacs RU, Goldstein AS, Lawson DA, Cheng D, Witte ON. Isolation, cultivation and characterization of adult murine prostate stem cells. Nat Protocols. 2010;5:702–13. doi: 10.1038/nprot.2010.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goldstein AS, Huang J, Guo C, Garraway IP, Witte ON. Identification of a cell of origin for human prostate cancer. Science. 2010;329:568–71. doi: 10.1126/science.1189992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rojas A, Liu G, Coleman I, Nelson PS, Zhang M, Dash R, et al. IL-6 promotes prostate tumorigenesis and progression through autocrine cross-activation of IGF-IR. Oncogene. 2011;30:2345–55. doi: 10.1038/onc.2010.605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kan CE, Cipriano R, Jackson MW. c-MYC Functions as a Molecular Switch to Alter the Response of Human Mammary Epithelial Cells to Oncostatin M. Cancer Res. 2011;71:6930–9. doi: 10.1158/0008-5472.CAN-10-3860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Klausen P, Pedersen L, Jurlander J, Baumann H. Oncostatin M and interleukin 6 inhibit cell cycle progression by prevention of p27kip1 degradation in HepG2 cells. Oncogene. 2000;19:3675–83. doi: 10.1038/sj.onc.1203707. [DOI] [PubMed] [Google Scholar]
- 18.Van Duijn PW, Trapman J. PI3K/Akt signaling regulates p27kip1 expression via Skp2 in PC3 and DU145 prostate cancer cells, but is not a major factor in p27kip1 regulation in LNCaP and PC346 cells. The Prostate. 2006;66:749–60. doi: 10.1002/pros.20398. [DOI] [PubMed] [Google Scholar]
- 19.Yang G, Ayala G, Marzo AD, Tian W, Frolov A, Wheeler TM, et al. Elevated Skp2 Protein Expression in Human Prostate Cancer Association with Loss of the Cyclin-dependent Kinase Inhibitor p27 and PTEN and with Reduced Recurrence-free Survival. Clin Cancer Res. 2002;8:3419–26. [PubMed] [Google Scholar]
- 20.Barbieri CE, Demichelis F, Rubin MA. Molecular genetics of prostate cancer: emerging appreciation of genetic complexity. Histopathology. 2012;60:187–98. doi: 10.1111/j.1365-2559.2011.04041.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.