Abstract
The emergency department (ED) is often where atrial fibrillation (AF) is first detected, acutely treated and affected patients dispositioned. We used the Nationwide Emergency Department Sample (NEDS) to estimate the percentage of visits resulting in hospitalization and investigate associations between patient and hospital characteristics with hospitalization at the national and regional levels. We conducted a cross-sectional study of adults with AF listed as the primary ED diagnosis in the 2007–2009 NEDS. We performed multivariable logistic regression analyses investigating the associations between pre-specified patient and hospital characteristics with hospitalization. From 2007–2009, there were 1,320,123 weighted AF ED visits, with 69% hospitalized nationally. Mean regional hospitalization proportions were: Northeast (74%), Midwest (68%), South (74%) and West (57%). The highest odds ratios for predicting hospitalization were heart failure (3.85, 95% CI 3.66 to 4.04), chronic obstructive pulmonary disease (2.47, 95% CI 2.34 to 2.61), and coronary artery disease (1.65, 95% CI 1.58 to 1.73). After adjusting for age, privately insured (0.77, 95% CI 0.73 to 0.81) and self-pay (0.77 95% CI 0.66 to 0.90) patients had lower odds when compared to Medicare recipients, whereas Medicaid (1.21, 95% CI 1.11 to 1.32) patients tended to have higher odds. Patients living in low-income zip codes (1.18, 95% CI 1.12 to 1.25) and individuals treated at large metropolitan hospitals (1.75, 95% CI 1.59, 1.93) had higher odds. In conclusion, our analysis showed considerable regional variation in the management of ED AF patients and in associations between patient socioeconomic and hospital characteristics with ED disposition; adapting best practices from among this variation in management could reduce hospitalizations and healthcare expenses.
Atrial fibrillation (AF) affects between 3 and 6 million Americans with estimated national incremental healthcare costs ranging from $6 to $26 billion per year.1–3 The emergency department (ED) is often where AF is first detected, acutely treated and affected patients dispositioned.4,5 ED visits for AF increased by 88% between 1993 and 2004, with 64% of these visits resulting in hospitalization.5 Understanding factors that influence hospitalization may result in more informed acute AF management. Specifically, our healthcare system may benefit from a greater knowledge of how healthcare disparities impact the significant United States (US) regional variation in hospitalizations for AF. The frequency of ED AF visits, national and regional AF hospitalizations, and ED cardioversions have not been studied following the publication of the 2006 ACC/AHA/ESC guidelines.6 We used the Nationwide Emergency Department Sample (NEDS) to investigate age-specific ED visit rates for AF, percentage of ED visits resulting in hospitalization, as well as associations between specific patient and hospital characteristics with hospitalization at the national and regional levels.7
Methods
NEDS is a US administrative database maintained by the Agency for Healthcare Research and Quality as a component of the Healthcare Cost and Utilization Project. NEDS contains data from 25 – 30 million unweighted hospital-based ED visits annually representing about 20% of all US visits.7 NEDS includes data from approximately 29 states and stratifies the data by geographic region (Northeast, Midwest, South and West), trauma center designation, urban-rural status, teaching hospital status, and ownership. The NEDS database includes weights for calculating national estimates from the 20% sample of measured ED visits. NEDS consists of 4 files: 1) a core file including demographic, diagnostic, ED charges, and disposition data; 2) a supplemental ED file with ED procedures; 3) an inpatient file with hospital procedures for those admitted; and 4) a hospital file describing the characteristics of the hospital-based ED. For each ED encounter, NEDS reports up to 15 diagnoses coded according to their respective ICD-9 codes. NEDS also classifies each ICD-9 diagnosis as a non-chronic or chronic condition based on a validated algorithm.7,8
We conducted a cross-sectional study of adults with AF, identified by the ICD-9 code 427.31 listed as the primary ED diagnosis from 2007–2009. We limited our analysis to the 3 years following publication of the 2006 ACC/AHA/ESC Guidelines for the Management of Patients with AF.6 All outcomes referring to hospitalizations included visits in which the patient was admitted to the same hospital or transferred to a short-term acute care hospital. We calculated annual incidences of AFED visits from 2007–2009, percentages of AFED visits resulting in hospitalization, and the percentage of visits associated with ED or inpatient electrical cardioversions. We further stratified these incidences by US geographic region and age groups defined by the US Census.9 We documented ED cardioversion frequencies to determine whether regional variation in hospitalization may be explained by increased frequency of ED cardioversion in the regions with lower hospitalization percentages. Electrical cardioversions performed in the ED and inpatient settings were measured using specific CPT codes 92960 and 92961 in the ED procedures section and Clinical Classifications Software code 225 in the Inpatient procedures section.
National and regional estimates of frequencies and percentages, as well as all regression analyses, accounted for the NEDS sampling design. Age-specific annual incidences of AFED visits were calculated by dividing the weighted annual number of AFED visits by July population estimates from the US Census Bureau, then expressing this quantity as ED visits per 1,000 persons. Two multivariable logistic regression analyses were used to investigate the association between a priori selected patient and hospital characteristics with hospitalization. The models evaluated associations between these independent variables, including US geographic region as an independent variable, and hospitalization from the ED at the national level stratified by region. The Appendix Table 1 provides a detailed description of the independent variables. We chose these patient and hospital characteristics based on our prior investigations, an extensive review of the medical literature, and our clinical experience.4,5,10–17 This study was conducted with de-identified data and was approved by the local institutional review board as non-human research. All analyses were done using the statistical programming language SAS software, Version 9.2 of the SAS System for Linux (Cary, NC).
Results
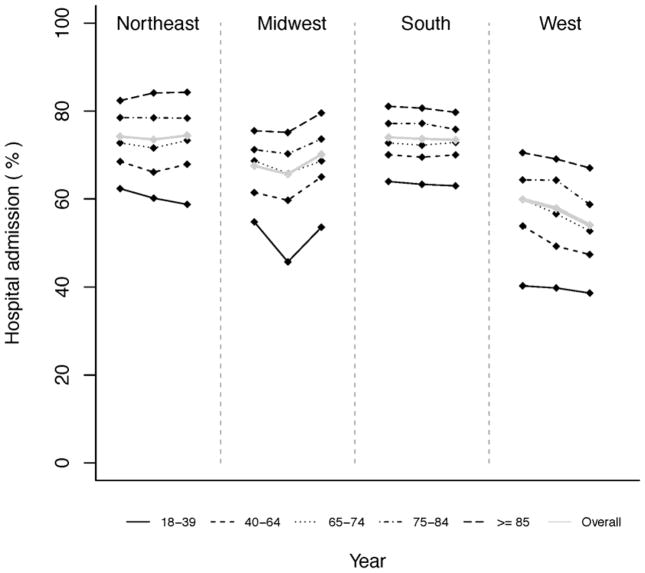
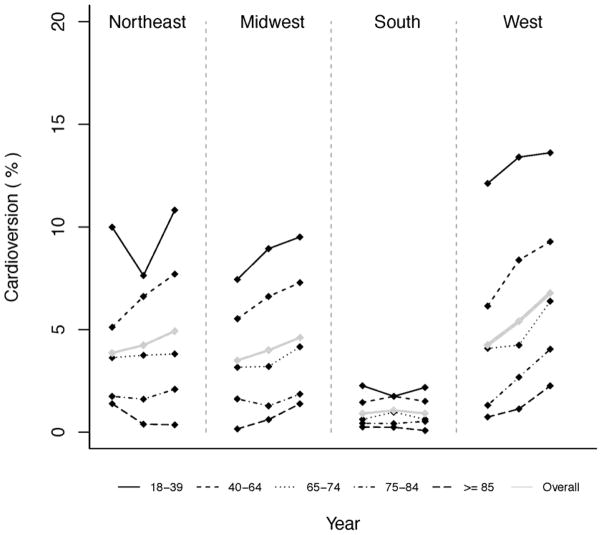
From 2007–2009, there were 376,162,043 (95% CI: 362,625,877; 389,698,208) total weighted ED visits including 1,320,123 (95% CI: 1,258776; 1,381471) weighted AFED visits. Table 1 reports the characteristics for the AFED visits overall including regional hospitalization frequencies. Characteristics stratified by census age groups are presented in Table 2. Figure 1 shows what appears to be a consistent trend in all 4 US geographic regions, with higher hospitalization percentages associated with increasing patient age. The percentage of AF patients who underwent ED electrical cardioversion nationwide during 2007–2009 was 3.5% (95% CI: 2.9, 4.1). Regional percentages of ED cardioversion were as follows: Northeast 4.3% (95% CI: 3.2, 5.5); Midwest 4.0% (95% CI: 2.5, 5.5); South 1.0% (0.7, 1.2); and West 5.6% (95% CI: 4.1, 7.1). Electrical cardioversions were most frequently performed in the youngest adults (Figure 2) and in the inpatient setting, with reported frequencies of 9.4% (95% CI: 8.8, 10) in 2007, 9.5% (95% CI: 8.8, 10.2) in 2008, and 10.1% (95% CI: 9.4, 10.8) in 2009. There was less regional variation in the performance of inpatient cardioversions (Appendix Table 2- online only).
Table 1.
Characteristics For Atrial Fibrillation Emergency Department Visits
| Characteristic | 2007 (Non-weighted AF ED Visits n=89056) | 2008 (Non-weighted AF ED Visits n=101211) | 2009 (Non-weighted AF ED Visits n=102979) |
|---|---|---|---|
| Overall Weighted AF ED Visits (95% CI) | 411406 (381029, 441783) | 445924 (412503, 479345) | 462794 (429160, 496427) |
| AF ED visits per 1000 person-years * | 1.8% (1.6, 2.0) | 1.9% (1.7, 2.2) | 2.0% (1.8, 2.2) |
| Northeast | 85834 (20.9%) | 88987 (20.0%) | 90547 (19.6%) |
| Midwest | 100160 (24.4%) | 103923 (23.3%) | 111942 (24.2%) |
| South | 154313 (37.5%) | 166748 (37.4%) | 172070 (37.2%) |
| West | 71098 (17.3%) | 86267 (19.4%) | 88235 (19.1%) |
| Age (years)* | 69.2 (68.9, 69.4) | 69.4 (69.2, 69.7) | 69.5 (69.3, 69.8) |
| Female | 215406 (52.4%) | 233940 (52.5%) | 243443 (52.6%) |
| ED Disposition | |||
| Treated and Released | 119836 (29.1%) | 138045 (31.0%)) | 141679 (30.6%) |
| Admitted to Same hospital | 275663 (67.0%) | 291822 (65.4%) | 306495 (66.2%) |
| Transferred to Short Term hospital | 12563 (3.1%) | 14731 (3.3%) | 13636 (3.0%) |
| Died in ED | 152.48 (0.04%) | 243.91 (0.05%) | 292.95 (0.06%) |
| Died in Hospital | 2981 (0.7%) | 3092 (0.7%) | 3166 (0.7%) |
| Regional Hospitalization % (95% CI) | |||
| Northeast | 74.2% (71.3, 77.2) | 73.6% (70.4, 76.8) | 74.5% (71.4, 77.6) |
| Midwest | 67.5% (65.2, 70.0) | 65.7% (63.3, 68.0) | 70.2% (67.9, 72.4) |
| South | 74.1% (72.1, 76.0) | 73.7% (71.8, 75.7) | 73.5% (71.7, 75.2) |
| West | 59.9% (56.5, 63.2) | 57.9% (54.4, 61.4) | 54.1% (49.7, 58.5) |
| Length of Stay (days)* | 3.7 (3.6, 3.7) | 3.7 (3.7, 3.8) | 3.7 (3.6, 3.7) |
| ED Cardioversion | 3929 (2.9%) | 5374 (3.5%) | 6368 (4.1%) |
| Inpatient Cardioversion | 25855 (9.4%) | 27838 (9.5%) | 30852 (10.1%) |
| Total ED Charge (USD)* | $1892(1803,1980) | $2169 (2061, 2276) | $2437 (2334, 2540) |
| Total Combined ED and Inpatient Charge (USD)* | $21771 (20712, 22828) | $23667 (22406, 24927) | $24752 (23635, 25869) |
| Weekend ED visit | 103331 (25.2%) | 112360 (25.2%) | 115567 (25.0%) |
| HypertensionŤ | 145815 (35.4%) | 160797 (36.1%) | 167623 (36.2%) |
| DiabetesŤ | 44476 (10.8%) | 50835 (11.4%) | 52930 (11.4%) |
| Coronary Artery DiseaseŤ | 60409 (14.7%) | 68173 (15.3%) | 68426 (14.8%) |
| Chronic Obstructive Pulmonary DiseaseŤ | 40501 (9.8%) | 33220 (7.5%) | 34344 (7.4%) |
| Heart FailureŤ | 70589 (17.2%) | 72452 (16.3%) | 82929 (17.9%) |
| Insurance Type % (95% CI) | |||
| Medicare | 66.2% (65.2, 37.1) | 66.7% (65.8, 67.7) | 66.7% (65.7, 67.7) |
| Medicaid | 4.0% (3.6, 4.3) | 4.3% (3.9, 4.7) | 4.7% (4.3, 5.2) |
| Private, including HMO | 24.0% (23.2, 24.8) | 23.3% (22.5, 24.2) | 22.8% (22.1, 23.6) |
| Self-pay | 3.7% (3.3, 4.0) | 3.3% (3.0, 3.6) | 3.5% (3.2, 3.8) |
| No charge | 0.4% (0.2, 0.6) | 0.4% (0.2, 0.5) | 0.4% (0.2, 0.6) |
| Other | 1.9% (1.6, 2.2) | 2.0% (1.7, 2.3) | 1.9% (1.6, 2.1)3 |
| Low-income | 98359 (24.4%) | 102227 (23.5%) | 105674 (23.4%) |
| Large Metropolitan | 179112 (48.9%) | 189144 (47.7%) | 197803 (48.0%) |
| Teaching Hospital | 145749 (35.4%) | 149259 (33.5%) | 158999 (34.4%) |
| Safety Net Hospital | 185127 (45.0%) | 213410 (47.9%) | 241649 (52.2%) |
Data presented as National Weighted Frequencies (Percentages of Total Annual ED AF visits) unless otherwise specified.
Data reported as Mean with (95% CI)
Frequencies of documented chronic disease reported as weighted frequency (%)
Table 2.
Characteristics For Atrial Fibrillation Emergency Department Visits Stratified By Age Group
| Age (Years) | ||||||
|---|---|---|---|---|---|---|
| Characteristic | 18–39 | 40–64 | 65–74 | 75–84 | > 85 | Overall |
| Overall Weighted ED AF Visits | 0.04% (0.04, 0.04) | 0.4% (0.4, 0.4) | 1.2% (1.2, 1.3) | 1.5% (1.5, 1.5) | 1.4% (1.4, 1.4) | 0.4% (0.3, 0.4) |
| Female (%) | 20.5% (19.6, 21.5) | 36.0% (35.5, 36.5) | 52.5% (51.9, 53.1) | 63.6% (63.1, 64.1) | 73.4% (72.8, 74.0) | 52.5%(52.2, 52.8) |
| ED Disposition | ||||||
| Discharged | 44.2% (42.4, 45.9) | 35.8% (34.6, 37.0) | 31.2% (30.1, 32.3) | 26.4% (25.4, 27.4) | 21.3% (20.4, 22.2) | 30.3% (29.3, 31.3) |
| Admitted to Same Hospital | 52.3% (50.5, 54.0) | 60.9% (59.7, 62.2) | 64.9% (63.7, 66.2) | 70.0% (68.8, 71.2) | 75.4% (74.3, 76.4) | 66.2% (65.1, 67.3) |
| Transferred to Short Term Hospital | 3.0% (2.6, 3.4) | 27.8% (2.5, 3.1) | 3.5% (3.0, 4.0) | 3.2% (2.8, 3.7) | 2.9% (2.5, 3.4) | 3.1% (2.7, 3.5) |
| Died in ED | 0.02% (0, 0.04) | 0.03% (0.02, 0.05) | 0.04% (.02, 0.06) | 0.06% (0.04, 0.07) | 0.1% (0.1, 0.1) | 0.05% (0.04, 0.06) |
| Medicare | 3.7% (3.2, 4.2) | 12.8% (12.4, 13.2) | 83.0% (82.3, 83.8) | 91.5% (90.9, 92.1) | 93.6% (93.0, 94.2) | 62.8% (62.1, 63.5) |
| Medicaid | 11.6% (10.7, 12.5) | 9.4% (8.9, 9.9) | 1.6% (1.3, 1.8) | 1.0% (0.8, 1.2) | 0.6% (0.5, 0.7) | 4.0% (3.8, 4.3) |
| Private, including HMO | 62.1% (60.6, 63.6) | 63.5% (62.4, 64.6) | 13.6% (12.9, 14.3) | 6.2% (5.7, 6.8) | 4.7% (4.2, 5.2) | 27.1% (26.4, 27.7) |
| Self-pay | 17.5% (16.3, 18.6) | 8.9% (8.4, 9.4) | 0.9% (0.8, 1.1) | 0.6% (0.5, 0.7) | 0.5% (0.3, 0.6) | 3.8% (3.6, 4.1) |
| No charge | 0.9% (0.6, 1.3) | 0.9% (0.6, 1.2) | 0.1% (0.03, 0.1) | 0.04 (0.01, 0.06) | 0.03% (0.01, 0.04) | 0.3% (0.2, 0.5) |
| Other | 4.3% (3.7, 4.9) | 4.5% (4.0, 4.9) | 0.8% (0.7, 1.0) | 0.7% (0.5, 0.8) | 0.6% (0.5, 0.8) | 2.0% (1.8, 2.2) |
| Low-income | 25.1% (23.3, 26.9) | 24.0% (22.5, 25.4) | 24.6% (23.1, 26.2) | 23.3% (21.8, 24.8) | 22.5% (20.9, 24.1) | 23.8% (22.3, 25.2) |
| Weekend ED Visit | 28.1% (27.2, 28.9) | 25.2% (24.9, 25.6) | 25.0% (24.7, 25.5) | 24.5% (24.2, 24.9) | 25.1% (24.6, 25.5) | 25.1% (24.9, 25.3) |
| Hypertension | 17.2% (16.2, 18.1) | 34.9% (34.3, 35.5) | 40.2% (39.6, 40.9) | 37.6% (36.9, 38.2) | 33.5% (32.8, 34.2) | 35.9% (35.4, 36.4) |
| Diabetes | 3.6% (3.1, 4.1) | 12.1% (11.7, 12.4) | 13.9% (13.5, 14.3) | 11.2% (10.9, 11.5) | 7.5% (7.2, 7.8) | 11.2% (11.0, 11.5) |
| Coronary Artery Disease | 1.5% (1.3, 1.8) | 11.0% (10.6, 11.3) | 17.4% (17.0, 17.9) | 18.6% (18.2, 19.0) | 15.8% (15.3, 16.3) | 14.9%(14.6, 15.2) |
| Chronic Obstructive Pulmonary Disease | 0.4% (0.3, 0.5) | 5.7% (5.5, 6.0) | 10.0% (9.7, 10.4) | 10.4% (10.1, 10.7) | 8.4% (8.0, 8.7) | 8.2% (8.0, 8.4) |
| Heart Failure | 3.6% (3.2, 4.0) | 12.0% (11.6, 12.4) | 15.0% (14.6, 15.5) | 20.3% (19.7, 20.8) | 28.2% (27.5, 29.0) | 17.1% (16.7, 17.5) |
| Large Metropolitan | 53.3% (50.6, 56.1) | 49.3% (46.9, 51.8) | 45.5% (43.1, 47.9) | 47.5% (45.1, 50.0) | 49.8%(47.2, 52.3) | 48.2% (45.8, 50.5) |
| Teaching Hospital | 40.3% (37.5, 43.1) | 37.8% (35.3, 40.2) | 32.5% (30.0, 34.9) | 32.6% (30.1, 35.1) | 32.5% (29.9, 35.1) | 34.4% (32.0, 36.8) |
| Safety Net Hospital | 52.0% (48.5, 55.5) | 50.5% (47.3, 53.7) | 49.7% (46.5, 52.9) | 46.7% (43.4, 50.0) | 45.0% (41.7, 48.4) | 48.5% (45.3, 51.7) |
| ED Electrical Cardioversion Performed | 8.0% (6.5, 9.4) | 5.4% (4.4, 6.4) | 3.0% (2.4, 3.6) | 1.6% (1.2, 1.9) | 0.7% (0.4, 1.0) | 3.5% (2.9, 4.1) |
| Inpatient Electrical Cardioversion Performed | 14.2% (13.1, 15.3) | 13.1% (12.5, 13.8) | 10.7% (10.1, 11.3) | 8.2% (7.7, 8.7) | 4.6% (4.2, 4.9) | 9.7% (9.2, 10.1) |
Data is presented as frequencies per age group and overall with % (95% confidence intervals)
Figure 1.
Hospitalizations by region and adult census age categories
Figures are stratified by region with each dot representing a year and each line type an age group. Overall estimates for each region are also included.
Figure 2.
ED cardioversions by adult census age category and region
Figures are stratified by region and illustrate percentages calculated from weighted frequencies. Each dot represents a year and each line type an age group, including the overall estimate for each region ignoring age.
Multivariable analyses found that the Midwest and West regions had lower odds of admission compared to the Northeast (Table 3). The strongest predictors of hospitalization were a history of heart failure, chronic obstructive pulmonary disease and coronary artery disease. After adjusting for age, privately insured and self-pay patients had lower odds of hospitalization when compared to Medicare patients, whereas Medicaid patients tended to have higher odds. Patients living in a low-income zip code and individuals treated at large metropolitan, safety net, and private investor-owned hospitals had higher odds of hospitalization. We investigated insurance status in individuals identified as low-income and found that 65% had Medicare, 6% Medicaid, 20% private insurance, 5% self-pay, and 2.5% with no charge/other insurance.
Table 3.
Multivariable Analysis Investigating Association between Covariates and Hospitalization for Emergency Department Patients with Atrial Fibrillation at the National and Regional Levels
| Characteristic | Region | Adjusted OR (95% CI) | P |
|---|---|---|---|
| Age | National | 1.008 (1.007, 1.010) | <.0001 |
| Northeast | 1.003 (1.00, 1.007) | 0.0517 | |
| Midwest | 1.011 (1.009, 1.014) | <.0001 | |
| South | 1.006 (1.003, 1.008) | <.0001 | |
| West | 1.013 (1.010, 1.016) | <.0001 | |
| Female | National | 1.064 (1.040, 1.088) | <.0001 |
| Northeast | 1.101 (1.045, 1.160) | 0.0003 | |
| Midwest | 1.035 (0.989, 1.083) | 0.1419 | |
| South | 1.057 (1.022, 1.093) | 0.0014 | |
| West | 1.072 (1.013, 1.133) | 0.0152 | |
| United States Region | Northeast (ref) | 1.00 | |
| Midwest | 0.762 (0.655, 0.886) | 0.0004 | |
| South | 0.846 (0.690, 1.036) | 0.1058 | |
| West | 0.44 (0.357, 0.543) | <.0001 | |
| Heart Failure | National | 3.845 (3.655, 4.017) | <.0001 |
| Northeast | 6.154 (5.419, 6.989) | <.0001 | |
| Midwest | 3.577 (3.302, 3.874) | <.0001 | |
| South | 3.229 (2.966, 3.515) | <.0001 | |
| West | 3.882 (3.445, 4.374) | <.0001 | |
| Chronic Obstructive Pulmonary Disease | National | 2.469 (2.340, 2.605) | <.0001 |
| Northeast | 3.346 (2.916, 3.840) | <.0001 | |
| Midwest | 2.343 (2.118, 2.605) | <.0001 | |
| South | 2.285 (2.108, 2.477) | <.0001 | |
| West | 2.242 (1.959, 2.566) | <.0001 | |
| Coronary Artery Disease | National | 1.651 (1.576, 1.729) | <.0001 |
| Northeast | 2.105 (1.850, 2.396) | <.0001 | |
| Midwest | 1.492 (1.374, 1.619) | <.0001 | |
| South | 1.535 (1.420, 1.632) | <.0001 | |
| West | 1.797 (1.581, 2.043) | <.0001 | |
| Hypertension | National | 1.131 (1.094, 1.205) | <.0001 |
| Northeast | 1.437 (1.266, 1.630) | <.0001 | |
| Midwest | 1.105 (1.017, 1.200) | 0.0177 | |
| South | 0.943 (0.889, 1.001) | 0.0523 | |
| West | 1.263 (1.105, 1.443) | .00006 | |
| Diabetes | National | 1.147 (1.104, 1.193) | <.0001 |
| Northeast | 1.22 (1.112, 1.340) | <.0001 | |
| Midwest | 1.147 (1.061, 1.240) | 0.0006 | |
| South | 1.093 (1.030, 1.160) | 0.0033 | |
| West | 1.154 (1.057, 1.261) | 0.0014 | |
| Payer Status | |||
| Medicare (ref) | 1.00 | ||
| Medicaid | National | 1.21 (1.110, 1.319) | <.0001 |
| Northeast | 0.982 (0.797, 1.211) | 0.8677 | |
| Midwest | 1.179 (0.986, 1.410) | 0.0718 | |
| South | 1.138 (0.996, 1.281) | 0.0580 | |
| West | 1.516 (1.284, 1.790) | <.0001 | |
| Private Insurance | National | 0.77 (0.729, 0.812) | <.0001 |
| Northeast | 0.599 (0.498, 0.720) | <.0001 | |
| Midwest | 0.852 (0.794, 0.914) | <.0001 | |
| South | 0.792 (0.739, 0.849) | <.0001 | |
| West | 0.849 (0.767, 0.940) | 0.0016 | |
| Self pay | National | 0.772 (0.659, 0.903) | 0.0013 |
| Northeast | 0.753 (0.612, 0.925) | 0.0071 | |
| Midwest | 1.082 (0.937, 1.249) | 0.2852 | |
| South | 0.628 (0.471, 0.839) | 0.0017 | |
| West | 0.923 (0.731, 1.166) | 0.5002 | |
| Low-income | National | 1.182 (1.117, 1.252) | <.0001 |
| Northeast | 1.14 (0.981, 1.325) | 0.0883 | |
| Midwest | 1.201 (1.098, 1.313) | <.0001 | |
| South | 1.142 (1.056, 1.234) | 0.0008 | |
| West | 1.379 (1.140, 1.666) | 0.0009 | |
| Large Metropolitan | National | 1.75 (1.589, 1.928) | <.0001 |
| Hospital | Northeast | 1.99 (1.570, 2.522) | <.0001 |
| Midwest | 1.554 (1.299, 1.859) | <.0001 | |
| South | 1.785 (1.521, 2.094) | <.0001 | |
| West | 1.689 (1.352, 2.111) | <.0001 | |
| Teaching Hospital | National | 1.161 (1.011, 1.333) | 0.0342 |
| Northeast | 1.236 (0.979, 1.561) | 0.0752 | |
| Midwest | 1.222 (1.018, 1.466) | 0.0313 | |
| South | 0.79 (0.470, 1.328) | 0.3730 | |
| West | 1.047 (0.569, 1.927) | 0.8835 | |
| Safety Net Hospital | National | 1.219 (1.105, 1.344) | <.0001 |
| Northeast | 0.882 (0.685, 1.137) | 0.3323 | |
| Midwest | 1.107 (0.954, 1.284) | 0.1808 | |
| South | 1.234 (1.047, 1.455) | 0.0123 | |
| West | 1.667 (1.410, 2.191) | <.0001 | |
| Hospital Ownership Government or Private, collapsed (ref) | 1.00 | ||
| Government, non-federal, public | National | 0.964 (0.807, 1.150) | 0.6821 |
| Northeast | 0.107 (0.086, 0.134) | <.0001 | |
| Midwest | 0.876 (0.684, 1.121) | 0.2929 | |
| South | 0.618 (0.371, 1.030) | 0.0646 | |
| West | 1.15 (0.651, 2.033) | 0.6297 | |
| Private, non-profit | National | 1.089 (0.898, 1.322) | 0.3849 |
| Northeast | 0.105 (0.087, 0.127) | <.0001 | |
| Midwest | 0.129 (0.112, 0.149) | <.0001 | |
| South | 0.675 (0.408, 1.116) | 0.1254 | |
| West | 1.532 (0.866, 2.711) | 0.1430 | |
| Private, investor-owned | National | 1.514 (1.250, 1.833) | <.0001 |
| Northeast | 0.124 (0.100, 0.153) | <.0001 | |
| Midwest | 0.15 (0.128, 0.176) | <.0001 | |
| South | 0.999 (0.601, 1.659) | 0.9955 | |
| West | 1.836 (1.055, 3.195) | 0.0315 | |
| Weekend ED Visit | National | 0.995 (0.971, 1.019) | 0.6914 |
| Northeast | 0.971 (0.922, 1.022) | 0.2602 | |
| Midwest | 1.008 (1.351, 1.839) | 0.7076 | |
| South | 1.016 (1.541, 2.108) | 0.3789 | |
| West | 0.97 (0.901, 1.406) | 0.4306 | |
Discussion
We found that the percentage of ED AF patients hospitalized nationally remained stable between 2007–2009; however, there continues to be regional differences in AF hospitalizations. ED electrical cardioversions are infrequently performed in the US despite being an approved and routinely practiced treatment in Canada and Europe.6,18–21 In addition to the expected differences in hospitalization due to underlying comorbidities, there were striking differences in EDAF management based on region, insurance, hospital type, and socioeconomics. These covariates may be surrogates for a patient’s access to specialized healthcare resources, including whether the patient has a primary care provider or cardiologist who can monitor their AF after ED discharge. Our results provide evidence to suggest that healthcare disparities are associated with AF treatment in the US, specifically resulting in more frequent hospitalizations among patients seen at hospitals that primarily serve uninsured and underinsured patients. Better understanding of the source of these differences could generate opportunities for the delivery of more standardized treatment regimens that may provide a platform for improved care and more efficient resource utilization. Given the increasing AF prevalence and the rising number of AFED visits, identifying strategies that will reduce the number of hospitalizations, while maintaining or improving quality of care, should be a priority.
The epidemiology and natural course for most individuals with AF is that it becomes a chronic condition requiring long-term surveillance and is not likely to be successfully treated during a 3-day hospitalization.6,22,23 Khairallah et al reviewed US hospitalizations for primary AF between 1996 and 2001 and found a 34% increase in admissions but no significant trend toward increased or decreased inpatient mortality.24 However, recent studies have emphasized the significance of close outpatient follow-up for patients with AF discharged from the ED citing that a lack of timely follow-up care is associated with increased 90-day mortality and repeat ED visits.25,26 Yet, our results are consistent with the notion that the US healthcare system frequently uses expensive hospitalizations to manage AF instead of less costly outpatient care. AF management often requires a patient to take one or a combination of the following: an atrioventricular nodal blocking agent, an antiarrhythmic medication, and an oral anticoagulant. Prescribing these medications from the ED to patients lacking primary care physicians and insurance presents a number of impediments to discharge. Patients with AF need a “medical home” to monitor their AF and medication response, reevaluate their risks for stroke and bleeding, and also treat associated diseases.6,27,28 Our analysis found that patients with private insurance, whom hospitals might have a financial interest to admit, were less likely to be hospitalized for their AF than patients with Medicare, even after adjusting for age. One plausible explanation is that patients with private insurance may have greater access to internists and cardiologists. If the ED physician can arrange a specific follow-up plan for the patient and have confidence that the patient can afford the medications and be reevaluated in a timely manner, he or she may be more likely to discharge the patient.29
The healthcare expenditures associated with AF hospitalization from the ED are substantial. In the 2009 NEDS data, there were an estimated 320,000 patients admitted from the ED, and the median ED and inpatient charges were nearly $20,000 more than the charges for patients discharged from the ED. These charges are likely underestimated; they do not include the charges associated with nosocomial complications that might occur from potentially preventable hospitalizations. A 15% reduction in hospitalizations would reduce inpatient charges by an estimated $1 billion dollars annually, and US hospitalizations would still be 3-fold higher than reported in Canada (16%) and Europe (29%).7,20,21 Our results support the need for patients with AF to have a medical home to coordinate their rate or rhythm control treatments, regularly reevaluate their stroke risk, and provide urgent follow-up when they experience acute AF-related events requiring ED evaluation. Medical homes have reduced ED visits by 29%, hospitalizations by 6%, and were associated with enhanced prevention and improved chronic disease care.28–30
This investigation used a large national database based on administrative and charge data, and it is subject to several limitations inherent to these databases. There is the potential that our investigation underestimates the true AFED burden because patients with AF-related ED visits might have an alternative diagnosis (e.g., chest pain) listed as the primary ED diagnosis and AF listed as a supporting diagnosis. We chose to analyze only those patients with AF ICD-9 code listed as the primary diagnosis. The inclusion of patients with AF listed as a supporting diagnosis may have led to inclusion of patients with permanent AF but without an emergent AF-related condition. Charges are only a surrogate and often inflated estimate for costs and do not reflect the true “cost” of the ED visit and hospitalization. NEDS data are discharge-level records not patient-level records; thus it is impossible to account for the effect of repeat ED visits or readmissions. The prevalence of comorbidities was likely under reported given the focus of ED documentation on acute conditions. NEDS is also limited by the potential presence of residual confounders (e.g., access to primary care, symptoms duration, anticoagulant use, and vital signs) as the administrative data lack clinical information not captured in ICD-9 codes. A large prospective cohort study would be needed to more fully investigate the effect of hospitalization on outcomes for ED patients with AF.11
Supplementary Material
Acknowledgments
FUNDING
No industry financial support or compensation has been or will be received for conducting this study. Dr. Barrett and this study are funded by NIH grant K23 HL102069 from the National Heart, Lung and Blood Institute, Bethesda, MD. Dr. Self is supported in part by an NIH KL2TR000446 from the National Center for Advancing Translational Sciences. Dr. McNaughton is supported by NIH grant HL1K12HL109019. Dr. Collins is supported by NIH grant K23HL085387. Dr. Storrow is supported by NIH K12HL1090 and UL1TR000445. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
There are no conflicts of interest in connection with this submission or are there any copyright constraints.
CONFLICTS OF INTEREST
None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, Singer DE. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001;285:2370–2375. doi: 10.1001/jama.285.18.2370. [DOI] [PubMed] [Google Scholar]
- 2.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Magid D, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, Moy CS, Mussolino ME, Nichol G, Paynter NP, Schreiner PJ, Sorlie PD, Stein J, Turan TN, Virani SS, Wong ND, Woo D, Turner MB. Heart Disease and Stroke Statistics--2013 Update: A Report From the American Heart Association. Circulation. 2013;127:e6–e245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim MH, Johnston SS, Chu BC, Dalal MR, Schulman KL. Estimation of total incremental health care costs in patients with atrial fibrillation in the United States. Circ Cardiovasc Qual Outcomes. 2011;4:313–320. doi: 10.1161/CIRCOUTCOMES.110.958165. [DOI] [PubMed] [Google Scholar]
- 4.Barrett TW, Martin AR, Storrow AB, Jenkins CA, Harrell FE, Jr, Russ S, Roden DM, Darbar D. A clinical prediction model to estimate risk for 30-day adverse events in emergency department patients with symptomatic atrial fibrillation. Ann Emerg Med. 2011;57:1–12. doi: 10.1016/j.annemergmed.2010.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McDonald AJ, Pelletier AJ, Ellinor PT, Camargo CA., Jr Increasing US emergency department visit rates and subsequent hospital admissions for atrial fibrillation from 1993 to 2004. Ann Emerg Med. 2008;51:58–65. doi: 10.1016/j.annemergmed.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 6.Fuster V, Ryden LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA, Halperin JL, Le Heuzey JY, Kay GN, Lowe JE, Olsson SB, Prystowsky EN, Tamargo JL, Wann S, Smith SC, Jr, Jacobs AK, Adams CD, Anderson JL, Antman EM, Halperin JL, Hunt SA, Nishimura R, Ornato JP, Page RL, Riegel B, Priori SG, Blanc JJ, Budaj A, Camm AJ, Dean V, Deckers JW, Despres C, Dickstein K, Lekakis J, McGregor K, Metra M, Morais J, Osterspey A, Tamargo JL, Zamorano JL. ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Circulation. 2006;114:e257–354. doi: 10.1161/CIRCULATIONAHA.106.177292. [DOI] [PubMed] [Google Scholar]
- 7.Agency for Healthcare Research and Quality. HCUP Nationwide Emergency Department Sample (NEDS) Rockville, MD: 2007, 2008, 2009. Healthcare Cost and Utilization Project (HCUP) [Google Scholar]
- 8.Hwang W, Weller W, Ireys H, Anderson G. Out-of-pocket medical spending for care of chronic conditions. Health Aff (Millwood) 2001;20:267–278. doi: 10.1377/hlthaff.20.6.267. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. [Accessed September 3, 2012];National Vital Statistics System: US census population with bridged race categories. http://www.cdc.gov/nchs/nvss/bridged_race.htm.
- 10.Barrett TW, Abraham RL, Jenkins CA, Russ S, Storrow AB, Darbar D. Risk Factors for Bradycardia Requiring Pacemaker Implantation in Patients With Atrial Fibrillation. Am J Cardiol. 2012;110:1315–1321. doi: 10.1016/j.amjcard.2012.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barrett TW, Storrow AB, Jenkins CA, Harrell FE, Jr, Miller KF, Moser KM, Russ S, Roden DM, Darbar D. Atrial fibrillation and flutter outcomes and risk determination (AFFORD): design and rationale. J Cardiol. 2011;58:124–130. doi: 10.1016/j.jjcc.2011.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA. 2001;285:2864–2870. doi: 10.1001/jama.285.22.2864. [DOI] [PubMed] [Google Scholar]
- 13.Miyasaka Y, Barnes ME, Gersh BJ, Cha SS, Bailey KR, Seward JB, Tsang TS. Changing trends of hospital utilization in patients after their first episode of atrial fibrillation. Am J Cardiol. 2008;102:568–572. doi: 10.1016/j.amjcard.2008.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Perrea DN, Ekmektzoglou KA, Vlachos IS, Tsitsilonis S, Koudouna E, Stroumpoulis K, Xanthos T. A formula for the stratified selection of patients with paroxysmal atrial fibrillation in the emergency setting: a retrospective pilot study. J Emerg Med. 2011;40:374–379. doi: 10.1016/j.jemermed.2008.02.062. [DOI] [PubMed] [Google Scholar]
- 15.Wang TJ, Massaro JM, Levy D, Vasan RS, Wolf PA, D’Agostino RB, Larson MG, Kannel WB, Benjamin EJ. A risk score for predicting stroke or death in individuals with new-onset atrial fibrillation in the community: the Framingham Heart Study. JAMA. 2003;290:1049–1056. doi: 10.1001/jama.290.8.1049. [DOI] [PubMed] [Google Scholar]
- 16.Zimetbaum P, Reynolds MR, Ho KK, Gaziano T, McDonald MJ, McClennen S, Berezin R, Josephson ME, Cohen DJ. Impact of a practice guideline for patients with atrial fibrillation on medical resource utilization and costs. Am J Cardiol. 2003;92:677–681. doi: 10.1016/s0002-9149(03)00821-x. [DOI] [PubMed] [Google Scholar]
- 17.Burt CW, Arispe IE. Characteristics of emergency departments serving high volumes of safety-net patients: United States, 2000. Vital Health Stat. 2004;13:1–16. [PubMed] [Google Scholar]
- 18.Bellone A, Etteri M, Vettorello M, Bonetti C, Clerici D, Gini G, Maino C, Mariani M, Natalizi A, Nessi I, Rampoldi A, Colombo L. Cardioversion of acute atrial fibrillation in the emergency department: a prospective randomised trial. Emerg Med J. 2012;29:188–191. doi: 10.1136/emj.2010.109702. [DOI] [PubMed] [Google Scholar]
- 19.del Arco C, Martin A, Laguna P, Gargantilla P. Analysis of current management of atrial fibrillation in the acute setting: GEFAUR-1 study. Ann Emerg Med. 2005;46:424–430. doi: 10.1016/j.annemergmed.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 20.Scheuermeyer FX, Grafstein E, Stenstrom R, Innes G, Heslop C, Macphee J, Pourvali R, Heilbron B, McGrath L, Christenson J. Thirty-Day and 1-Year Outcomes of Emergency Department Patients With Atrial Fibrillation and No Acute Underlying Medical Cause. Ann Emerg Med. 2012;60:755–765. doi: 10.1016/j.annemergmed.2012.05.007. [DOI] [PubMed] [Google Scholar]
- 21.Stiell IG, Clement CM, Brison RJ, Rowe BH, Borgundvaag B, Langhan T, Lang E, Magee K, Stenstrom R, Perry JJ, Birnie D, Wells GA. Variation in management of recent-onset atrial fibrillation and flutter among academic hospital emergency departments. Ann Emerg Med. 2011;57:13–21. doi: 10.1016/j.annemergmed.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 22.Magnani JW, Rienstra M, Lin H, Sinner MF, Lubitz SA, McManus DD, Dupuis J, Ellinor PT, Benjamin EJ. Atrial fibrillation: current knowledge and future directions in epidemiology and genomics. Circulation. 2011;124:1982–1993. doi: 10.1161/CIRCULATIONAHA.111.039677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Soliman EZ, Sorlie PD, Sotoodehnia N, Turan TN, Virani SS, Wong ND, Woo D, Turner MB. Heart disease and stroke statistics--2012 update: a report from the American Heart Association. Circulation. 2012;125:e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Khairallah F, Ezzedine R, Ganz LI, London B, Saba S. Epidemiology and determinants of outcome of admissions for atrial fibrillation in the United States from 1996 to 2001. Am J Cardiol. 2004;94:500–504. doi: 10.1016/j.amjcard.2004.04.068. [DOI] [PubMed] [Google Scholar]
- 25.Atzema CL, Austin PC, Chong AS, Dorian P. Factors associated with 90-day death after emergency department discharge for atrial fibrillation. Ann Emerg Med. 2013;61:539–548. doi: 10.1016/j.annemergmed.2012.12.022. [DOI] [PubMed] [Google Scholar]
- 26.Atzema CL, Dorian P, Ivers NM, Chong AS, Austin PC. Evaluating early repeat emergency department use in patients with atrial fibrillation: A population-based analysis. Am Heart J. 2013;165:939–948. doi: 10.1016/j.ahj.2013.02.026. [DOI] [PubMed] [Google Scholar]
- 27.Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, Hindricks G, Kirchhof P, Bax JJ, Baumgartner H, Ceconi C, Dean V, Deaton C, Fagard R, Funck-Brentano C, Hasdai D, Hoes A, Kirchhof P, Knuuti J, Kolh P, McDonagh T, Moulin C, Popescu BA, Reiner Z, Sechtem U, Sirnes PA, Tendera M, Torbicki A, Vahanian A, Windecker S, Vardas P, Al-Attar N, Alfieri O, Angelini A, Blomstrom-Lundqvist C, Colonna P, De Sutter J, Ernst S, Goette A, Gorenek B, Hatala R, Heidbuchel H, Heldal M, Kristensen SD, Kolh P, Le Heuzey JY, Mavrakis H, Mont L, Filardi PP, Ponikowski P, Prendergast B, Rutten FH, Schotten U, Van Gelder IC, Verheugt FW. 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012;33:2719–2747. doi: 10.1093/eurheartj/ehs253. [DOI] [PubMed] [Google Scholar]
- 28.Jackson GL, Powers BJ, Chatterjee R, Bettger JP, Kemper AR, Hasselblad V, Dolor RJ, Irvine J, Heidenfelder BL, Kendrick AS, Gray R, Williams JW. Patient-Centered Medical Home A Systematic Review. Ann Intern Med. 2013;158:169–178. doi: 10.7326/0003-4819-158-3-201302050-00579. [DOI] [PubMed] [Google Scholar]
- 29.Katz EB, Carrier ER, Umscheid CA, Pines JM. Comparative effectiveness of care coordination interventions in the emergency department: a systematic review. Ann Emerg Med. 2012;60:12–23. doi: 10.1016/j.annemergmed.2012.02.025. [DOI] [PubMed] [Google Scholar]
- 30.Hoff T, Weller W, DePuccio M. The patient-centered medical home: a review of recent research. Med Care Res Rev. 2012;69:619–644. doi: 10.1177/1077558712447688. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.