Abstract
Black men have less physician contact than other groups and thus lower rates of hypertension treatment and control. In the BARBER-1 trial, hypertension control in 8 active-intervention barbershops where barbers offered blood pressure (BP) checks with haircuts and motivated black male patrons with high BP to seek provider follow-up showed a small improvement over that in 7 comparison shops where patrons received hypertension pamphlets but not barber-BP checks. Under-treatment of hypertension, which is common in primary care, may have impacted the outcomes. Thus, in patrons with baseline systolic BP ≥140 mmHg and 10-month follow-up including BP and medication data, we performed post-hoc comparison of systolic BP reduction between comparison-arm patrons (n=68) treated by primary care providers (PCPs) with a) intervention-arm patrons (n=37) treated by PCPs, or b) intervention-arm patrons (n=33) who lacked access to PCPs and were treated by hypertension specialist physicians serving as safety-net providers. The latter group had higher baseline systolic BP than the others (162±3 vs. 155±2 and 154±2 mmHg, respectively, p<0.01). After adjustment for baseline systolic BP and other covariates, systolic BP reduction was 21±4 mmHg greater than in the comparison group (p<.0001) when barbers referred patrons to hypertension specialists but no different when they referred to PCPs (4±4 mmHg, p=0.31). Specialist-treated patrons received more BP medication and different classes of medication than PCP-treated patrons. In conclusion, the barber-based intervention—if connected directly to specialty-level medical care—could have a large public health impact on hypertensive disease in black men.
Keywords: Hypertension, African-Americans, Gender, Antihypertensive Medication
Hypertension is particularly devastating to non-Hispanic black men, who have a higher prevalence of hypertension than most other groups but less physician contact, leading to low rates of hypertension awareness, treatment, and control.1–6 As a result, black men have the highest hypertension death rate of any U.S. race, ethnic, or gender group.4, 7 We conducted a cluster-randomized trial of a hypertension control program implemented through black-owned barbershops, enlisting barbers to monitor blood pressure (BP) and promote provider follow-up for uncontrolled hypertension. In this trial (Barber-Assisted Reduction in Blood Pressure among Ethnic Residents [BARBER-1]),8 we observed a small intervention effect on systolic BP, indicating that further research is needed to develop a more potent intervention model.8, 9 We previously reported a high level of adherence to the study protocol by the barbers and their patrons,8 but had not examined the quality of medical care delivered by the patrons’ healthcare providers.
Under-treatment of hypertension by office-based primary care providers (PCPs) is increasingly recognized as a key barrier to hypertension control,10–12 both in provider networks and national databases,13 and thus constitutes one hypothesis to explain the smaller than desired effect size in the BARBER-1 trial. To test this hypothesis, we conducted a post-hoc subgroup analysis of BARBER-1 participants with unequivocally elevated baseline systolic BP and a completed exit interview. We compared systolic BP reductions and antihypertensive treatment regimens prescribed for hypertensive barbershop patrons in the comparison group–who received hypertension pamphlets and usual medical care by PCPs—with hypertensive patrons in the intervention group who followed their barbers’ advice to seek medical follow up for high BP and had documented office visits with either: a) PCPs, or b) American Society of Hypertension-certified hypertension specialists. Using hypertension specialty care as a benchmark, we examined whether under-treatment of hypertension in primary care limited the ability of the barber-based intervention to lower systolic BP.
Methods
In the BARBER-1 trial, patron consent was obtained and data were collected and stored in accordance with the guidelines of the Health Insurance Portability and Accountability Act. The study and analyses were approved by the Institutional Review Boards at the University of Texas Southwestern Medical Center, Temple University Institute for Survey Research, and Cedars-Sinai Medical Center.
The design and major outcomes of the BARBER-1 trial have been published.8, 14 Briefly, black male patrons of 17 black-owned barbershops in Dallas, Texas underwent baseline BP screening to identify those with hypertension and calculate an initial hypertension control rate for each shop (% with BP <135/85 or <130/80 if diabetic). All participants received written results of baseline BPs and detailed instructions for appropriate medical follow up. Then, shops were randomized to a comparison group that received hypertension pamphlets written for black patients by the American Heart Association or an intervention group in which barbers continually offered BP checks with haircuts and promoted physician follow-up with peer health messaging. We previously reported that, after 10 months, hypertension control improved, but systolic BP fell by only 2.5 mmHg more in the intervention group than in the comparison group (P=0.08), despite high levels of intervention fidelity by the barbers and acceptance by patrons.8
In this subsequent post-hoc analysis, we evaluated the potential impact of the quality of medical care received on systolic BP reduction in the BARBER-1 trial. We analyzed data from participants who completed the study and had a baseline systolic BP ≥140 mmHg; participants with baseline systolic BP <140 mmHg were excluded from this analysis, because of unresolved controversy as to whether lower BP treatment thresholds lead to improved cardiovascular outcomes among black individuals or those with diabetes mellitus.15–17 Data were analyzed in three subgroups of completers: (1) comparison-arm patrons all of whom were treated by PCPs, (2) intervention-arm patrons who followed their barbers’ advice and had documented office visits with PCPs, and (3) intervention-arm patrons who followed their barbers’ advice and had documented office visits with physicians who were certified as hypertension specialists by the American Society of Hypertension and were part of the study. The last subgroup of barbershop patrons had limited or no access to PCPs (either in private practice or in county or federally-funded safety net clinics) and were therefore referred to the academic medical center hypertension clinic, which agreed to provide discounted care (at a federally qualified health center rate) for uninsured study participants who were charged a co-pay of $50 dollars for an initial office visit and $25 for each follow-up visit.
The primary outcome was systolic BP reduction after 10 months. BP was measured in the barbershops by professional field interviewers using a validated oscillometric monitor (Welch Allyn, Arden, North Carolina).18 They took 6 consecutive BP readings on each hypertensive subject on each of 2 days both at baseline and at the exit interview. The final four readings on the second day of each set were averaged to obtain stable mean values.1, 3 Secondary outcomes, also assessed at the 10-month exit interview, included diastolic BP reduction, number and classes of BP medications in each participant’s final antihypertensive regimen, and medication adherence, using the four-item Morisky questionnaire (with higher scores indicating high medication-taking adherence behaviors).19 In the intervention group, interaction with a medical provider was documented by wallet-size provider referral cards the barbers gave to patrons with high BP readings; patrons received a free haircut for each card signed by their provider and returned to their barber. There was no objective means of documenting provider interaction in the comparison group.
Descriptive statistics are presented as simple means and standard errors. Unadjusted mean change in systolic BP and Kernel distributions were plotted for each of the three groups. Using ANOVA and standard linear and logistic multivariate regression models, statistical comparisons were made between a) intervention-arm patrons treated by hypertension specialists vs. comparison-arm patrons; b) intervention-arm patrons treated by community providers vs. comparison-arm patrons; and c) intervention-arm patrons treated by hypertension specialists vs. intervention-arm patrons treated by community providers. To model the primary outcome of systolic BP reduction, we assumed that missing final BP values were missing at random. Independent predictors of change in systolic BP were identified in linear regression models that adjusted for baseline systolic BP and other covariates (including age, education, marital status, smoking status and number of doctor visits; the latter was available only in the intervention group). The same approach was used to model secondary outcomes. Statistical significance was determined using the likelihood ratio test with a 2-sided alpha level of <.05. SAS, version 9.1.3 (© SAS Institute Inc., Cary, North Carolina and R, version 2.15.1 (© The R Foundation of Statistical Computing, www.r-project.org) were used for statistical analyses.
Results
A total of 258 patrons in the intervention group and 227 patrons in the comparison group completed both the baseline and exit interviews. Of these, baseline systolic BP was ≥140 mmHg in 70 patrons in the intervention group (33 patrons treated by hypertension specialists and 37 patrons treated by PCPs) and 68 patrons in the comparison group all treated by PCPs.
Table 1 shows the baseline characteristics of these three groups. Intervention-arm participants who were treated by hypertension specialists were younger than comparison-arm participants and, though more were employed, fewer had health insurance or pre-existing PCPs and thus required a safety-net provider; they also had higher baseline systolic and diastolic BP. Intervention-arm participants who were treated by community PCPs were well matched with the comparison group except for a shorter duration of barbershop patronage.
Table 1.
Baseline characteristics
| Group Assignment | Barber-based Intervention | Comparison | |
|---|---|---|---|
|
| |||
| Treating Physicians | Hypertension-specialists | PCPs | PCPs |
|
| |||
| (n=33 patrons) | (n=37 patrons) | (n=68 patrons) | |
| Mean ± SE | Mean ± SE or | Mean ± SE or | |
| Age (years) | 52 ± 2* | 57 ± 2 | 60 ± 2 |
| Body mass index (kg•m−2) | 33 ± 1 | 31 ± 1 | 32 ± 1 |
| Married or living with partner | 21 (64%) | 26 (70%) | 54 (80%) |
| Level of education | |||
| ≤High school | 15 (46%) | 20 (54%) | 23 (34%) |
| College | 16 (49%) | 16 (43%) | 31 (46%) |
| Postgraduate | 2 (6%) | 1 (3%)* | 13 (19%) |
| Full-time employment | 26 (79%)* | 18 (49%) | 33 (49%) |
| Any health insurance | 19 (58%)* | 34 (92%) | 64 (94%) |
| Established PCP | 17 (51%)* | 33 (90%) | 63 (93%) |
| Income (% of Poverty Level)a | 330 ± 37 | 330 ± 31 | 380 ± 22 |
| Barbershop patronage | |||
| Duration (years) | 8 ± 1* | 7 ± 1* | 13 ± 9 |
| Time between haircuts (weeks) | 3 ± 0.5 | 3 ± 0.5 | 3 ± 2 |
| Baseline systolic BP (mmHg) | 162 ± 3* | 154 ± 2 | 155 ± 2 |
| Baseline diastolic BP (mmHg) | 96 ± 2* | 88 ± 2 | 86 ± 1 |
| Current smoker | 8 (24%) | 8 (22%) | 15 (22%) |
| Diabetes mellitus | 7 (21%) | 13 (35%) | 21 (37%) |
| Hyperlipidemia | 18 (56%)* | 20 (54%) | 33 (49%) |
| History of stroke, myocardial infarction or heart failure | 4 (12%) | 13 (35%)* | 7 (10%) |
Likelihood ratio test p value ≤ .05 vs. comparison group
Calculated as income/2007 United States poverty level: $10210 for a single person and $20650 for a 4-person household x100.
Abbreviations: BP, blood pressure; HTN, hypertension; PCP, primary care providers, SE, standard error
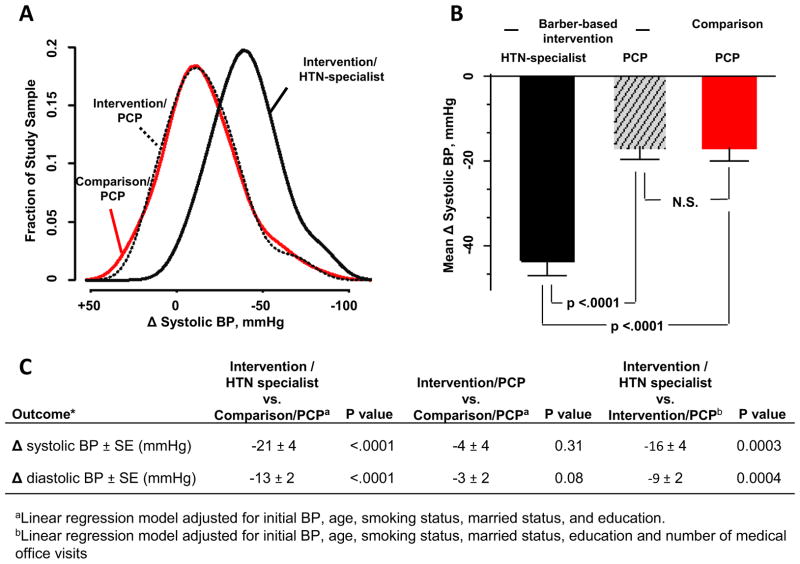
The mean reduction in systolic BP was 2.6 times greater in intervention-group patrons treated by hypertension specialists than in the comparison group or in the intervention-group patrons treated by PCPs, whereas, the systolic BP reduction in intervention-group patrons treated by community PCPs was indistinguishable from that in the comparison group (Table 2 and Figure 1). After adjustment for baseline systolic BP and other covariates, systolic BP reduction was greater compared with the comparison group when barbers referred patrons to hypertension specialists but no different when they referred to PCPs (Figure 1). Other multivariate-adjusted independent predictors of greater systolic BP reduction were: (1) higher baseline systolic BP (Δ systolic BP= −8±1 mmHg per 10 mmHg elevation in baseline BP >140 mmHg, p=0.003 [β-coefficient ± SE]); and (2) treatment with 3 or more BP medications (Δ systolic BP= −9±3 mmHg, p=0.003). In contrast, neither medication adherence nor office visit frequency predicted systolic BP reduction. An intervention effect on diastolic BP reduction was also only seen in patrons treated by hypertension specialists (Table 2 and Figure 1).
Table 2.
Outcomes
| Group Assignment | Barber-based Intervention | Comparison | |
|---|---|---|---|
|
| |||
| Treating Physicians | Hypertension-specialists | PCPs | PCPs |
|
| |||
| Variable | (n=33 patrons) | (n=37 patrons) | (n=68 patrons) |
| Mean ± SE | Mean ± SE | Mean ± SE | |
| Final Blood Pressure | |||
| Systolic BP [mmHg] | 122 ± 2* | 138 ± 3 | 139 ± 2 |
| Diastolic BP [mmHg] | 75 ± 1* | 81 ± 2 | 80 ± 1 |
| Change of systolic BP (final-initial) [mmHg] | −41 ± 4* | −16 ± 3 | −16 ± 3 |
| Change of diastolic BP (final-initial) [mmHg] | −21 ± 3* | −7.4 ± 1 | −6.2 ± 1 |
| Hypertension control rate (%with final BP<135/85 mmHg)a | 29 (88%)* | 18 (49%) | 29 (43%) |
| Final BP regimen | |||
| Number of medications | |||
| None | 0* | 4 (11%) | 15 (22%) |
| 1 | 3 (9%) | 5 (14%) | 9 (13%) |
| 2 | 6 (18%) | 12 (32%) | 19 (28%) |
| 3 or more | 24 (73%)* | 16 (43%) | 25 (37%) |
| Mean | 3.4 ± 0.3* | 2.3 ± 0.2 | 2.1 ± 0.2 |
| Medications | |||
| ACE-inhibitor or ARBs | 31 (94%)* | 17 (51%) | 24 (45%) |
| Calcium channel blocker | 30 (91%)* | 24 (65%) | 24 (45%) |
| Diuretic | 22 (67%) | 25 (76%) | 25 (47%) |
| Alpha/Beta blocker | 11 (33%)* | 2 (6%) | 2 (4%) |
| Aldosterone antagonist | 5 (20%)* | 0 | 0 |
| Central sympatholytic | 4 (15%) | 0 | 0 |
| Direct vasodilator | 1 (3%) | 1 (3%) | 1 (2%) |
| Beta blocker | 0* | 10 (30%) | 10 (19%) |
| Alpha blocker | 0 | 3 (9%) | 3 (6%) |
| Medication adherenceb | 3.0 ± 0.2 | 3.1 ± 0.2 | 3.4 ± 0.2 |
Abbreviations: ACE indicates angiotensin converting enzyme; ARBs, angiotensin receptor blockers; BP, blood pressure; PCP, primary care providers; SE, standard error.
Likelihood ratio test p value <.05 vs. comparison group.
Cut-off for out-of-office BP
Morisky scale: scores ranging from 0 to 4, with 4 representing perfect adherence.
Figure 1. Post-hoc Analyses of BP Outcomes.
A) Distribution of systolic BP change in 3 subgroups: 1) comparison group patrons treated by PCPs (red solid line); 2) intervention group patrons treated by PCPs (black dotted line); 3) intervention group patrons treated by hypertension specialists (black solid line). B) Mean change in systolic BP in the three subgroups. C) Results of the multivariate linear regression model showing adjusted estimates of the mean group differences in the change of systolic and diastolic BP. The change scores in each intervention subgroup are compared to those of the comparison group and finally within the intervention group with each other.
Abbreviations: BP indicates blood pressure; HTN, hypertension; PCP, primary care provider; SE, standard error.
Intervention-arm patrons who were referred to hypertension specialists received more BP medication than PCP-treated patrons in the comparison group; after adjustment for the higher baseline BP in the specialist-treated group, hypertension specialists prescribed one additional class of BP medication per antihypertensive regimen (p<0.002). In contrast, PCPs prescribed the same amount of medication for patrons in intervention and comparison groups. A higher percentage of patrons referred to hypertension specialists received treatment with angiotensin converting enzyme (ACE)-inhibitors or angiotensin II receptor blockers (ARBs) and calcium channel blockers (CCBs) but a smaller percentage received standard beta-blockers (Table 2).
Discussion
The major new finding in this post-hoc analysis is that under-treatment of hypertension in primary care markedly limited the ability of the barber-based BP monitoring and medical referral program to lower systolic BP. The findings indicate that intervention potency could be improved by an order of magnitude if new care delivery and payment models would enable barbers to refer all their hypertensive patrons to specialty-trained providers.
The intervention model emphasized the barber-patron relationship, with the only direct link between the referring barbers and medical providers being referral cards, which showed that systolic BP in the barbershop was on average ~20 mmHg above recommended treatment targets. However, we found that the cards alone are not sufficient to influence provider prescribing behavior, because BP reduction—as well as the numbers and classes of BP medications prescribed—in intervention-arm patrons treated by PCPs were indistinguishable from those in comparison-arm patrons treated by PCPs. These findings are consistent with recent analysis of the National Ambulatory Medical Care Survey showing that office-based PCPs prescribe new BP medication for patients with an established diagnosis of hypertension during only one in five office visits where the recorded systolic BP is >140 mmHg.13
The involvement of hypertension specialists in the intervention was not pre-specified but rather evolved as the only viable means to offer affordable hypertension treatment to a subset of participants who were too young to qualify for Medicare and were employed with income levels that both were too high to qualify for Medicaid or standard safety-net care but too low to afford private health insurance, high deductibles, and copayments. The 21 mmHg larger reduction in systolic BP (and 13 mmHg larger reduction in diastolic BP) in this intervention subgroup (vs. the comparison group) represents the optimal situation of the barber-based BP monitoring and medical referral program being linked directly to affordable specialty-level healthcare.
The effect size is impressive for two reasons. First, this intervention subgroup had less favorable baseline demographics—a decade younger in age, half the duration of barbershop patronage, much less previous engagement with the healthcare system and a 7 mmHg higher baseline systolic BP— than the comparison group. Second, the comparison group itself had a sizeable BP reduction which was expected from regression to the mean,20 the Hawthorne effect,21 and a positive influence on treatment-seeking behavior from pamphlets on hypertension in blacks, written results of baseline BPs, and detailed instructions for appropriate medical follow.
The greater BP reduction and lower achieved BP levels in the specialist-treated patrons are explained in part by a greater percentage receiving combination drug therapy with three or more BP medications of different classes, as endorsed by recent hypertension guidelines.22–24 Despite the greater number of medications prescribed by the specialists, there was no group difference in medication adherence. Specialists prescribed more ACE-inhibitors, ARBs, and CCBs, which are generally well tolerated, and avoided standard beta blockers which are less well tolerated.25 Also, vasodilating beta blockers and aldosterone antagonists, which are recommended for difficult hypertension,26 were prescribed only by the specialists. Their achieved average BP of 122/75 mmHg may or may not seem lower than necessary in light of recent controversy as to whether or not higher cardiovascular risk of black hypertensives justifies lower-than-usual BP treatment targets (e.g., <130/80 mmHg).15, 16 Nonetheless, the final average systolic BP achieved in the comparison group fails to meet the universally accepted target for out-of-office BP <135 mmHg.23, 24 Their final hypertension control rate closely approximates the currently estimated hypertension control rate for U.S. black men of 36%, which is far below that of the general population and thus considered unacceptable.2
This study has several limitations. Only a small subset of barbershop patrons completed both the baseline and exit interviews in the BARBER-1 trial, which was designed as a cohort of barbershops rather than of individuals.14 Without knowing reasons why subjects did not participate in either the baseline interview or the exit interview (e.g., natural turnover of the barbershops’ clientele), the analysis makes the assumption that data are missing at random. Moreover, because patrons with systolic BP <140 mmHg were excluded from this post-hoc analysis, the remaining sample size per shop was too small to retain clustered statistics. Thus, our analyses ignore intra-class correlation (ICC), which might lead us to over-estimate treatment effects;27 however, the main conclusion of our study should not be affected given the robust effect size and the near-zero ICC values previously reported.8 Because assignment to hypertension specialist- or PCP- treatment within the intervention group was neither random nor pre-specified, the results are hypothesis generating.
Acknowledgments
Funding sources: This work was funded by grants to Dr. Victor from the National Heart, Lung and Blood Institute (R01HL080582; Bethesda, Maryland) and the Lincy Foundation (Los Angeles, California); and the UCLA Clinical Translational Science Institute grant from the National Center for Research Resources (UL1RR033176, Bethesda, Maryland), which is now at the National Center for Advancing Translational Sciences (UL1TR000124, Bethesda, Maryland).
Footnotes
Conflicts of Interest: none
Trial registration: clinicaltrials.gov identifier: NCT00325533
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Magid D, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, Moy CS, Mussolino ME, Nichol G, Paynter NP, Schreiner PJ, Sorlie PD, Stein J, Turan TN, Virani SS, Wong ND, Woo D, Turner MB American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Executive summary: heart disease and stroke statistics--2013 update: a report from the American Heart Association. Circulation. 2013;127:143–152. doi: 10.1161/CIR.0b013e318282ab8f. [DOI] [PubMed] [Google Scholar]
- 2.Guo F, He D, Zhang W, Walton RG. Trends in prevalence, awareness, management, and control of hypertension among United States adults, 1999 to 2010. J Am Coll Cardiol. 2012;60:599–606. doi: 10.1016/j.jacc.2012.04.026. [DOI] [PubMed] [Google Scholar]
- 3.Wright JT, Jr, Dunn JK, Cutler JA, Davis BR, Cushman WC, Ford CE, Haywood LJ, Leenen FH, Margolis KL, Papademetriou V, Probstfield JL, Whelton PK, Habib GB ALLHAT Collaborative Research Group. Outcomes in hypertensive black and nonblack patients treated with chlorthalidone, amlodipine, and lisinopril. JAMA. 2005;293:1595–1608. doi: 10.1001/jama.293.13.1595. [DOI] [PubMed] [Google Scholar]
- 4.Victor RG, Leonard D, Hess P, Bhat DG, Jones J, Vaeth PA, Ravenell J, Freeman A, Wilson RP, Haley RW. Factors associated with hypertension awareness, treatment, and control in Dallas County, Texas. Arch Intern Med. 2008;168:1285–1293. doi: 10.1001/archinte.168.12.1285. [DOI] [PubMed] [Google Scholar]
- 5.Hyman DJ, Pavlik VN. Characteristics of patients with uncontrolled hypertension in the United States. N Engl J Med. 2001;345:479–486. doi: 10.1056/NEJMoa010273. [DOI] [PubMed] [Google Scholar]
- 6.Williams DR. The health of men: structured inequalities and opportunities. Am J Public Health. 2003;93:724–731. doi: 10.2105/ajph.93.5.724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cutler JA, Sorlie PD, Wolz M, Thom T, Fields LE, Roccella EJ. Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988–1994 and 1999–2004. Hypertension. 2008;52:818–827. doi: 10.1161/HYPERTENSIONAHA.108.113357. [DOI] [PubMed] [Google Scholar]
- 8.Victor RG, Ravenell JE, Freeman A, Leonard D, Bhat DG, Shafiq M, Knowles P, Storm JS, Adhikari E, Bibbins-Domingo K, Coxson PG, Pletcher MJ, Hannan P, Haley RW. Effectiveness of a barber-based intervention for improving hypertension control in black men: the BARBER-1 study: a cluster randomized trial. Arch Intern Med. 2011;171:342–350. doi: 10.1001/archinternmed.2010.390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yancy CW. A bald fade and a BP check: Comment on “Effectiveness of a barbershop-based intervention for improving hypertension control in black men”. Arch Intern Med. 2011;171:350–352. doi: 10.1001/archinternmed.2010.404. [DOI] [PubMed] [Google Scholar]
- 10.Okonofua EC, Simpson KN, Jesri A, Rehman SU, Durkalski VL, Egan BM. Therapeutic inertia is an impediment to achieving the Healthy People 2010 blood pressure control goals. Hypertension. 2006;47:345–351. doi: 10.1161/01.HYP.0000200702.76436.4b. [DOI] [PubMed] [Google Scholar]
- 11.Oliveria SA, Lapuerta P, McCarthy BD, L’Italien GJ, Berlowitz DR, Asch SM. Physician-related barriers to the effective management of uncontrolled hypertension. Arch Intern Med. 2002;162:413–420. doi: 10.1001/archinte.162.4.413. [DOI] [PubMed] [Google Scholar]
- 12.O’Connor PJ. Overcome clinical inertia to control systolic blood pressure. Arch Intern Med. 2003;163:2677–2678. doi: 10.1001/archinte.163.22.2677. [DOI] [PubMed] [Google Scholar]
- 13.Khanna RR, Victor RG, Bibbins-Domingo K, Shapiro MF, Pletcher MJ. Missed Opportunities for Treatment of Uncontrolled Hypertension at Physician Office Visits in the United States, 2005 Through 2009. Arch Intern Med. 2012;172:1344–1345. doi: 10.1001/archinternmed.2012.2749. [DOI] [PubMed] [Google Scholar]
- 14.Victor RG, Ravenell JE, Freeman A, Bhat DG, Storm JS, Shafiq M, Knowles P, Hannan PJ, Haley R, Leonard D. A barber-based intervention for hypertension in African American men: design of a group randomized trial. Am Heart J. 2009;157:30–36. doi: 10.1016/j.ahj.2008.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Flack JM, Sica DA, Bakris G, Brown AL, Ferdinand KC, Grimm RH, Jr, Hall WD, Jones WE, Kountz DS, Lea JP, Nasser S, Nesbitt SD, Saunders E, Scisney-Matlock M, Jamerson KA International Society on Hypertension in Blacks. Management of high blood pressure in Blacks: an update of the International Society on Hypertension in Blacks consensus statement. Hypertension. 2010;56:780–800. doi: 10.1161/HYPERTENSIONAHA.110.152892. [DOI] [PubMed] [Google Scholar]
- 16.Wright JT, Jr, Agodoa LY, Appel L, Cushman WC, Taylor AL, Obegdegbe GG, Osei K, Reed J. New recommendations for treating hypertension in black patients: evidence and/or consensus? Hypertension. 2010;56:801–803. doi: 10.1161/HYPERTENSIONAHA.110.159566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ Joint National Committee on Prevention, Detection Evaluation, and Treatment of High Blood Pressure, National Heart, Lung, and Blood Institute, National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 18.Jones CR, Taylor K, Poston L, Shennan AH. Validation of the Welch Allyn ‘Vital Signs’ oscillometric blood pressure monitor. J Hum Hypertens. 2001;15:191–195. doi: 10.1038/sj.jhh.1001141. [DOI] [PubMed] [Google Scholar]
- 19.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Blomqvist N. On the bias caused by regression toward the mean in studying the relation between change and initial value. J Clin Periodontol. 1987;14:34–37. doi: 10.1111/j.1600-051x.1987.tb01510.x. [DOI] [PubMed] [Google Scholar]
- 21.Wickstrom G, Bendix T. The “Hawthorne effect”--what did the original Hawthorne studies actually show? Scand J Work Environ Health. 2000;26:363–367. [PubMed] [Google Scholar]
- 22.Gradman AH. Rationale for triple-combination therapy for management of high blood pressure. J Clin Hypertens (Greenwich) 2010;12:869–878. doi: 10.1111/j.1751-7176.2010.00360.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, Grassi G, Heagerty AM, Kjeldsen SE, Laurent S, Narkiewicz K, Ruilope L, Rynkiewicz A, Schmieder RE, Struijker Boudier HA, Zanchetti A, Vahanian A, Camm J, De Caterina R, Dean V, Dickstein K, Filippatos G, Funck-Brentano C, Hellemans I, Kristensen SD, McGregor K, Sechtem U, Silber S, Tendera M, Widimsky P, Zamorano JL, Kjeldsen SE, Erdine S, Narkiewicz K, Kiowski W, Agabiti-Rosei E, Ambrosioni E, Cifkova R, Dominiczak A, Fagard R, Heagerty AM, Laurent S, Lindholm LH, Mancia G, Manolis A, Nilsson PM, Redon J, Schmieder RE, Struijker-Boudier HA, Viigimaa M, Filippatos G, Adamopoulos S, Agabiti-Rosei E, Ambrosioni E, Bertomeu V, Clement D, Erdine S, Farsang C, Gaita D, Kiowski W, Lip G, Mallion JM, Manolis AJ, Nilsson PM, O’Brien E, Ponikowski P, Redon J, Ruschitzka F, Tamargo J, van Zwieten P, Viigimaa M, Waeber B, Williams B, Zamorano JL The task force for the management of arterial hypertension of the European Society of, Hypertension The task force for the management of arterial hypertension of the European Society of, Cardiology. 2007 Guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Eur Heart J. 2007;28:1462–1536. doi: 10.1093/eurheartj/ehm236. [DOI] [PubMed] [Google Scholar]
- 24.Krause T, Lovibond K, Caulfield M, McCormack T, Williams B Guideline Development Group. Management of hypertension: summary of NICE guidance. BMJ. 2011;343:d4891. doi: 10.1136/bmj.d4891. [DOI] [PubMed] [Google Scholar]
- 25.Elliott WJ. Improving outcomes in hypertensive patients: focus on adherence and persistence with antihypertensive therapy. J Clin Hypertens (Greenwich) 2009;11:376–382. doi: 10.1111/j.1751-7176.2009.00138.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, White A, Cushman WC, White W, Sica D, Ferdinand K, Giles TD, Falkner B, Carey RM American Heart Association Professional Education Committee. Resistant hypertension: diagnosis, evaluation, and treatment: a scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension. 2008;51:1403–19. doi: 10.1161/HYPERTENSIONAHA.108.189141. [DOI] [PubMed] [Google Scholar]
- 27.Preisser JS, Reboussin BA, Song EY, Wolfson M. The importance and role of intracluster correlations in planning cluster trials. Epidemiology. 2007;18:552–560. doi: 10.1097/ede.0b013e3181200199. [DOI] [PMC free article] [PubMed] [Google Scholar]