Abstract
Asian Americans experience disproportionate incidence and mortality rates of certain cancers, compared to other racial/ethnic groups. Primary care physicians are a critical source for cancer screening recommendations and play a significant role in increasing cancer screening of their patients. This study assessed primary care physicians’ perceptions of cancer risk in Asians and screening recommendation practices. Primary care physicians practicing in New Jersey and New York City (n=100) completed a 30-question survey on medical practice characteristics, Asian patient communication, cancer screening guidelines, and Asian cancer risk. Liver cancer and stomach cancer were perceived as higher cancer risks among Asian Americans than among the general population, and breast and prostate cancer were perceived as lower risks. Physicians are integral public health liaisons who can be both influential and resourceful toward educating Asian Americans about specific cancer awareness and screening information.
Keywords: Asian Americans, cancer, primary care physician, health disparities
Introduction
Cancer incidence and mortality rates continue to decline, however, Asian Americans experience a disproportionate burden of certain types of cancers among all racial and ethnic groups. According to the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) Cancer Statistics Review, during 2005–2009, the top five highest age adjusted incidence rates for Asians and Pacific Islanders by cancer site were breast, colon, prostate, lung, and liver and the top five highest mortality rates by cancer site were lung, colon, liver, stomach, and pancreas (Howlader et al., 2012). Asian and Pacific Islanders also have the highest incidence rates of liver and stomach cancer among all racial/ethnic groups (American Cancer Society, 2012). Further, Asian and Pacific Islanders had the highest mortality rate from liver cancer reported during 2005–2009 (Howlader et al., 2012).
Primary care providers are a critical source for communication of the importance of cancer prevention services. Physician recommendations are associated with cancer screenings among Asian Americans and other minority groups (Tu et al., 2003; Taylor et al., 2004; Lubetkin et al., 2008; Tsui and Tanjasiri, 2008). Physician recommendations have also impacted hepatitis B screening and vaccination among Asian Americans (Nguyen et al., 2010; Strong et al., 2012) as hepatitis B is an important risk factor for liver cancer. Physicians also serve as a top source of cancer information (O’Malley et al., 2002). In a study of smoking cessation among Chinese Americans in New York City, almost half of the respondents stated that they received most of their health-related information from their physicians (Ferketich et al., 2004). In examining barriers and facilitators of breast cancer screening among Chinese women in the Philadelphia area, physicians who served as the information source of mammograms was the only significant predictor in reporting having had a mammogram (Su et al., 2006). Physicians are integral public health liaisons that can educate Asian Americans about specific cancers and provide screening information and recommendations. However, some physicians may not be aware of or understand the cancer disparities in this population. The purpose of this study was to assess primary care physicians’ perceptions of cancer risk among Asian Americans and examine their screening recommendation practices.
Materials and Methods
Sample
The study sample comprised of primary care physicians who practiced in internal medicine, family practice, or OB/GYN within specified Asian–concentrated ZIP Codes in New Jersey or New York City. This approach was used with the key assumption that Asians residing within highly concentrated ZIP Codes will see primary care physicians within their ZIP Code (Chakrabarti, 2005). Large proportions of Asian residents by ZIP Code were identified using the American Fact Finder tool of the U.S. Census. For the purpose of this study, a “large proportion” was operationally defined as a proportion of Asians composing more than 25 percent of the population residing within a specified ZIP Code. Physicians were randomly selected using the Statistical Package for the Social Sciences (SPSS) uniform random numbers selection procedure from a provider directory in the New York City and New Jersey area.
Survey instrument
Randomly selected physicians were mailed a 30 question, cross-sectional survey. The survey assessed four areas: (1) Physician’s general practice information, which included questions on: the physician’s Asian patient load; services provided; location of services; interpreter and bilingual staff access; and time spent with each patient. In addition, questions on charting smoking status, cancer screening reminders, and occurrence of cancer prevention screening recommendations were asked; (2) Asian patient communication, which included questions on: barriers to communicating with Asian patients; physician perceptions of screening barriers experienced by Asian patients; and a self-assessment of the physician’s cultural competency; (3) Perceptions of cancer risk, which included questions on: which organizational cancer screenings guidelines were followed and how often they were used; and physician perception of cancer risk among Asians compared to the general population. Cancer risk perceptions were operationalized as an assessment of cancer risks by cancer type for Asians compared to the general population. The cancer types assessed were breast, cervical, colorectal, liver, lung, prostate, stomach, and all cancers (in general); and (4) Demographics including age, gender, race/ethnicity, language, medical specialization, length of clinical practice, and medical education information.
Data analysis
Nonparametric and inferential statistical analyses were computed and served a particular purpose in summarizing the data through numerical means. Data recoding and transformation was conducted to meet the data variable requirements of specific statistics. Missing values were coded appropriately when data were entered into the system. Patterns of missing data were examined to determine whether the patterns are random or systematic. Remedies to account for missing data during analysis included case wise deletion (if necessary) or to use scale score averages as a substitute for missing data. All data were entered in SPSS, version 18.0, and this program was used to compute statistics.
Results
Surveys were mailed to 852 internal medicine, family practice, and OB/GYN physicians in New Jersey and New York City during the summer of 2006. A total of 103 surveys were returned, of which 100 were deemed complete and entered into a database. Table 1 displays the demographic characteristics of the sample. The respondents’ ages ranged from 31–77 years old, with a mean age of 47.0 years (SD=10.40). The sample was mostly male and Asian, practiced internal medicine, and primarily spoke English. Almost half (47.0%) had 10 or fewer years of clinical experience, and over half (53.0%) received their medical education in the United States. Some of the physicians reported receiving their medical education abroad (e.g., Asia and Europe).
Table 1.
Demographic Characteristics of Respondents
| Demographic characteristic | Frequency | % |
|---|---|---|
| Gender* | ||
| Male | 61 | 61.6 |
| Female | 38 | 38.4 |
| Agea | ||
| 30–39 | 22 | 23.2 |
| 40–49 | 38 | 40.0 |
| 50–59 | 21 | 22.1 |
| 60–69 | 12 | 12.6 |
| ≥70 | 2 | 2.1 |
| Race/ethnicity* | ||
| African American | 3 | 3.0 |
| Asian | 63 | 63.6 |
| Hispanic/Latino | 4 | 4.0 |
| White | 29 | 29.3 |
| Primary language | ||
| English | 61 | 61.0 |
| Other | 24 | 24.0 |
| Both | 15 | 15.0 |
| Specialization | ||
| OB/GYN | 27 | 27.0 |
| Family practice | 21 | 21.0 |
| Internal medicine | 42 | 42.0 |
| Other | 2 | 2.0 |
| OB/GYN and family practice | 1 | 1.0 |
| OB/GYN and other | 1 | 1.0 |
| Internal medicine and other | 6 | 6.0 |
| Years of practice in United States | ||
| ≤5 | 20 | 20.0 |
| 6–10 | 27 | 27.0 |
| 11–20 | 27 | 27.0 |
| 21–30 | 21 | 21.0 |
| ≥31 | 5 | 5.0 |
| Medical education origin | ||
| United States | 53 | 53.0 |
| Asia | 32 | 32.0 |
| Other country | 9 | 9.0 |
| Multiple countries | 6 | 6.0 |
N<100 because of missing values
Medical practice characteristics
The physicians reported that they saw an average of 99.3 patients (SD=51.45) per week and that 49.3 percent (SD=35.08) of their patients were Asian. Physicians indicated that they spent an average of 12.3 minutes (SD=8.27) on patient education for their Asian patients during a regular checkup. Most of the respondents (69 physicians) reported that most (69.4%) of their Asian patients were self-referrals. Table 2 presents additional medical practice characteristics that were reported. A large proportion (59.0%) of the physicians reported that 76–100 percent of their Asian patients had health insurance. Over half (56.0%) of the physicians were in private practice, followed by community or local health clinic (17.0%), a combination of practice settings (11.0%), and hospital (10.0%). Almost all physicians (96.0%) charted their Asian patients’ smoking status. In addition, smoking cessation counseling was the most selected free preventive service offered. Nearly a third of the physicians (30.0%) did not provide reminders for cancer screening tests. Further, none of the physicians provided e-mail reminders, and most reported using “other” reminder methods (e.g., reminding patients during a patient visit or annual physical, providing a verbal reminder). A large proportion of the physicians (65.3%) reported that less than 10 percent of their Asian patients needed an interpreter to speak with them. For those patients needing an interpreter, physicians selected family members and friends most frequently as the one who provided interpretation or translation at their practice followed by physicians and administrative staff.
Table 2.
Summary of Additional Medical Practice Characteristics
| Characteristic | Frequency | % |
|---|---|---|
| Asian patient with health insurance | ||
| Less than 10% of patients | 1 | 1.0 |
| 10–25% of patients | 4 | 4.0 |
| 26–50% of patients | 6 | 6.0 |
| 51–75% of patients | 28 | 28.0 |
| 76–100% of patients | 59 | 59.0 |
| Don’t know | 2 | 2.0 |
| Free preventive services* | ||
| Smoking cessation counseling | 52 | — |
| Mammograms | 29 | — |
| Pap tests | 27 | — |
| Colon cancer screenings | 23 | — |
| Hepatitis B screening or vaccination | 31 | — |
| Prostate cancer screening | 23 | — |
| Other preventive services | 11 | — |
| Practice settings | ||
| Hospital | 10 | 10.0 |
| Community or local health clinic | 17 | 17.0 |
| Private practice | 56 | 56.0 |
| Health maintenance organization | 3 | 3.0 |
| Other | 3 | 3.0 |
| More than one | 11 | 11.0 |
| Chart Asian patient smoking status | ||
| Yes | 96 | 96.0 |
| No | 4 | 4.0 |
| Cancer screening reminder method | ||
| No reminder | 30 | 30.0 |
| 20 | 20.0 | |
| Phone | 11 | 11.0 |
| 0 | 0.0 | |
| Other | 27 | 27.0 |
| More Than One | 12 | 12.0 |
| Need interpreter to speak with Asian patient | ||
| Less than 10% of patients | 64 | 65.3 |
| 10–25% of patients | 9 | 9.2 |
| 26–50% of patients | 8 | 8.2 |
| 51–75% of patients | 8 | 8.2 |
| 76–100% of patients | 9 | 9.2 |
| Who provides translation or interpretation services* | ||
| Yourself | 42 | — |
| Another health care provider | 35 | — |
| Administrative staff | 37 | — |
| Volunteer | 11 | — |
| Family member or friend | 56 | — |
| Not needed | 5 | — |
Totals exceed sample size because of multiple selections
Organizational cancer screening guidelines
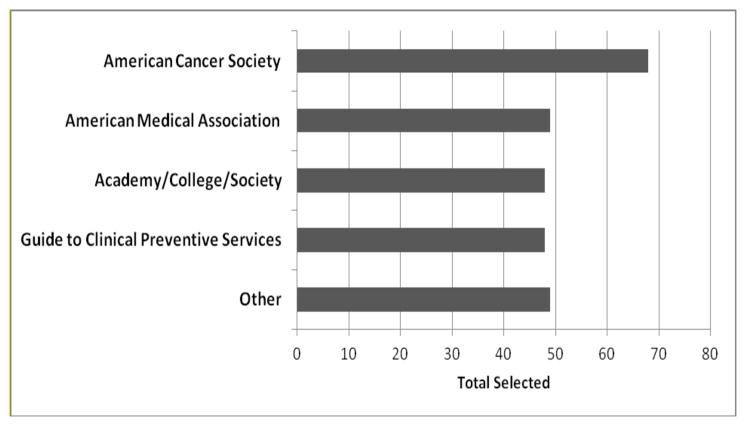
Physicians were provided with a list of several health organizations and were asked to select which organization’s cancer screening guidelines they followed. As shown in Figure 1, the American Cancer Society received the most selections with 68. A total of 49 physicians selected the American Medical Association followed closely with 48 physicians selecting guidelines set forth by an academy, college, or [professional] society. A total of 48 selected the Guide to Clinical Preventive Services, and 49 physicians selected other organizations.
Figure 1. Frequency (Total Selected) of Organizational Cancer Screening Guidelines Followed.<.
br>Note: Total exceeds sample size because of multiple selections
Frequency of prevention screening recommendations
Physicians were asked how often—on a scale from 1 to 5, with 1 being never and 5 being always—they recommended prevention screenings to their Asian patients during a checkup. As shown in Table 3, frequency of cervical cancer screening recommendations and breast cancer screening recommendations had the largest mean score (4.9) and the lowest variability. Frequency of stomach cancer screening recommendations received the lowest mean score (2.7); however, it had the largest variability. A total of 14 physicians selected “not applicable” for prostate cancer, which may indicate possible responses from OB/GYN physicians, and 9 physicians selected more than one “not applicable” answer choice for this question.
Table 3.
Frequency of Prevention Screening Recommendations Made to Asian Patients
| Prevention screening | N | Range* | Mean | SD |
|---|---|---|---|---|
| Breast cancer | 97 | 3–5 | 4.9 | 0.31 |
| Cervical cancer | 95 | 2–5 | 4.9 | 0.43 |
| Colorectal cancer | 97 | 1–5 | 4.5 | 0.88 |
| Hepatitis B | 96 | 1–5 | 4.1 | 1.07 |
| Prostate cancer** | 77 | 1–5 | 4.1 | 1.35 |
| Smoking cessation | 98 | 1–5 | 4.6 | 0.80 |
| Stomach cancer | 87 | 1–5 | 2.7 | 1.46 |
The scale ranged from 1 (never) to 5 (always).
Fourteen physicians selected “not applicable
Perception of cancer risk in asians
Physicians were asked to rate their perceptions of relative cancer risks for Asians in comparison to risks for the general population. As shown in Table 4, perceived cancer risk among Asians for all cancers had a mean score of 3.2. Liver cancer (4.4) and stomach cancer (4.3) had the highest perceived cancer risk among Asians by physicians, and breast cancer (2.8) and prostate cancer (2.9) were reported as having the lowest perceived cancer risk for Asians. Cervical cancer had the largest degree of variability (SD=0.95), and the category of all cancer had the smallest variability (SD=0.65). Figure 2 displays the range of responses by percent of physician perceptions of Asian cancer risk [by cancer type] as compared to the risk of the general population.
Table 4.
Summary of Physician Perceptions of Asian Cancer Risk as Compared to the General Population
| Cancer type | N | Range* | Mean | SD |
|---|---|---|---|---|
| All cancer | 92 | 1–5 | 3.2 | 0.65 |
| Breast cancer | 98 | 1–5 | 2.8 | 0.89 |
| Cervical cancer | 98 | 1–5 | 3.2 | 0.95 |
| Colorectal cancer | 98 | 1–5 | 3.3 | 0.90 |
| Liver cancer | 99 | 1–5 | 4.4 | 0.82 |
| Lung cancer | 97 | 1–5 | 3.6 | 0.92 |
| Prostate cancer | 96 | 1–5 | 2.9 | 0.75 |
| Stomach cancer | 98 | 1–5 | 4.3 | 0.81 |
The scale ranged from 1 to 5, where 1 is lower risk, 3 is same risk, and 5 is higher risk
Figure 2. Percent of Physician Perceptions of Asian Cancer Risk Compared to the General Population, by Cancer Type.
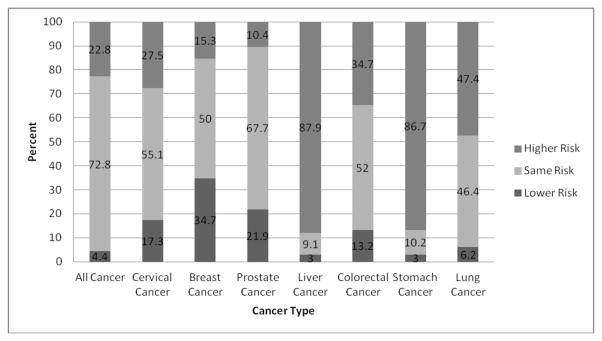
note: total percentages may not equal to 100% due to rounding
Discussion
The results from the survey indicate that this group of physicians follow a variety of screening guidelines, engage in a high frequency of recommending specific prevention screenings, and have varied perceptions of cancer risk among Asians. Physicians reported following the American Cancer Society cancer screening guidelines the most. This finding is consistent with results from a nationally representative survey of primary care physicians on cancer screening recommendations and practices, in which physicians reported the American Cancer Society guidelines as very influential for breast cancer screening (Meissner et al., 2011) and the second most influential (organization specific) for Pap testing for cervical cancer (Yabroff et al., 2009). In a study of the impact of physicians’ health beliefs on colorectal cancer screening practices, over 79 percent of the physicians in the St. Louis area also agreed with the American Cancer Society guidelines, and 91.3 percent followed the American Cancer Society guidelines for recommending colorectal cancer screening to their patients (Shieh et al., 2005). In a study examining the cancer screening practices of physicians serving Chinese Americans in San Francisco, physicians reported using the American Cancer Society guidelines the most for breast, cervical, and colorectal cancer screening practices (Lee et al., 1999).
Almost half of the physicians selected multiple organizational screening guidelines indicating a variation in cancer screening recommendations followed. In a study examining physician perception of clinical practice guidelines on breast and cervical cancer screening, most physicians preferred multiple guidelines and perceived guidelines that were more aggressive as influential (Han et al., 2011). Many physicians may also be confused or unaware of the current guidelines or how they may differ from other guidelines (Holland-Barkis et al., 2006). In their study on physicians’ awareness and adherence to cervical cancer screening guidelines in Texas, which involved a cross-sectional, mail survey of physicians in a large, university-based health organization, the most commonly identified guideline for cervical cancer screening was the American College of Obstetrics and Gynecology, followed by the American Academy of Family Practice, the American Cancer Society, and the U.S. Preventive Services Task Force.
Preventive screenings were almost always recommended to Asian patients during a visit, with the exception of stomach cancer screening—understandable because no known official stomach cancer screening guideline is available in the U.S. Moreover, the American Cancer Society (2011) indicates that because this disease is less common in the U.S., studies have shown that mass screening may not be useful. No standard or routine screening test is available for stomach cancer; however, several screening tests are being studied to find stomach cancer at an early stage (National Cancer Institute, 2012). The high frequency of breast, cervical, and colorectal cancer screening recommendations along with hepatitis B screening made to Asian patients was consistent with the findings of breast, cervical, colorectal, and hepatic cancer screening recommendation practices among Asian physicians serving Asian patients in New York City (Bodle et al., 2008).
Physicians perceived Asian cancer risk for all cancers to be slightly above “same risk,” as compared to the general population. The highest perceived cancer risk for Asians was liver and stomach cancers which was consistent with the high age adjusted incidence rates from the National Cancer Institute’s Cancer Statistics Review. The risk of breast and prostate cancer among Asians was perceived as being slightly lower in comparison to those cancers in the general population. Despite these beliefs, breast and prostate cancer are some of the more common cancer affecting Asian-Americans. Although Asians (and Pacific Islanders) have lower incidence rates (79.7 per 100,000) and mortality rates (10.5 per 100,000) of prostate cancer as compared to all racial and ethnic groups (American Cancer Society, 2012), when examined at the Asian subgroup level, prostate cancer incidence was highest among Asian Indian or Pakistani, Chinese, Filipino, and Japanese males (Miller et al., 2008). During 2005–2009, breast cancer had the highest incidence and second highest mortality rate among Asian and Pacific Islander females (Howlader et al., 2012). Further, breast cancer incidence among specific Asian subgroups was highest for Asian Indian or Pakistani, Chinese, Filipina, Japanese, Kampuchean, Korean, and Vietnamese females (Miller et al., 2008). Cancer registry data from northern California also suggested increased rates of invasive breast cancer incidence for Chinese, Korean, Vietnamese, and South Asian women from 1990–2002 (Keegan et al., 2007).
There were several limitations in this study. First, a low response rate may lead to concerns of non-response bias. However, low response rates are common in mailed physician surveys. In an analysis of physician-mailed survey studies published from 1986–1995 involving studies with more than 1,000 physicians, Cummings et al. (2001) found the response rates ranged from 11 percent to 39 percent. In a study of 178 articles on factors associated with response rates, physicians were found to have the lowest response rates among all types of respondent groups including dentists, nurses, other health care workers, administrators, patients, students, and other respondents (Asch et al., 1997). A second limitation is that this study did not focus on specific Asian subgroups and only examined Asians in aggregate form. Though this method establishes useful means of examining an issue with a larger group, the effects for specific Asian subgroups were not analyzed. Further, some data sources relied upon for comparisons contained Pacific Islander data. There are many different Asian subgroups, and most of these groups experience different cancer burdens. In addition, although the results may be weighted more towards male and Asian physicians practicing in New Jersey and New York City, another limitation is the fact that this sample’s Asian patients were reported to be highly insured, and a majority of the physicians reported that less than 10 percent of their patients needed a translator/interpreter. The underserved and uninsured cohort is of most concern because it is most vulnerable to not receiving secondary prevention (screening and early detection) services because they are not accustomed to the preventive health care as Asians with health insurance and do not have access to the guidance of a primary care provider.
In conclusion, the results of this study suggest an opportunity to raise awareness of the varied physician perceptions of cancer risk among Asians and to provide a platform for physicians to understand the importance of making cancer screening recommendations. Physician interactions with patients serve as a proxy to educate about cancer and recommending appropriate screenings. Physicians should be educated on all of the cancer health disparities experienced among Asian Americans using the most current data available, especially data at the subgroup level. This will raise awareness of the cancer burden possibly unknown to physicians and may prompt them to make appropriate cancer screening recommendations.
References
- American Cancer Society. Cancer Facts and Figures 2012. Atlanta, GA: Author; 2012. [Google Scholar]
- American Cancer Society. Stomach Cancer. 2011 Retrieved July 24, 2012. Available at: http://www.cancer.org/acs/groups/cid/documents/webcontent/003141-pdf.pdf.
- Asch DA, Jedrziewski MK, Christakis NA, et al. Conducting physician mail surveys on a limited budget: A randomized trial comparing $2 bill versus $5 bill incentives. J Clin Epidemiol. 1997;50:1129–36. [Google Scholar]
- Bodle EE, Islam N, Kwon SC, et al. Cancer screening practices of Asian American physicians in New York City. J Immigr Minor Health. 2008;10:239–46. doi: 10.1007/s10903-007-9077-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakrabarti S. Unpublished Master’s Thesis. Temple University; Philadelphia, PA: 2005. Philadelphia physicians’ perceived cultural barriers to cancer screening of their Asian American patients. [Google Scholar]
- Cummings SM, Savitz LA, Konrad TR. Reported response rates to mailed physician questionnaires. Health Serv Res. 2001;35:1347–55. [PMC free article] [PubMed] [Google Scholar]
- Ferketich A, Wewers ME, Kwong K. Smoking cessation interventions among Chinese Americans: the role of families, physicians, and the media. Nicotine Tob Res. 2004;6:241–8. doi: 10.1080/14622200410001676350. [DOI] [PubMed] [Google Scholar]
- Han P, Klabunde CN, Breen N, et al. Multiple clinical practice guidelines for breast and cervical cancer screening: Perceptions of US primary care physicians. Med Care. 2011;49:139–48. doi: 10.1097/MLR.0b013e318202858e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holland-Barkis P, Forjuoh SN, Couchman GR, et al. Primary care physicians’ awareness and adherence to cervical cancer screening guidelines in Texas. Prev Med. 2006;42:140–5. doi: 10.1016/j.ypmed.2005.09.010. [DOI] [PubMed] [Google Scholar]
- Howlader N, Noone AM, Krapcho M, et al. SEER Cancer Statistics Review, 1975–2009 (Vintage 2009 Populations) National Cancer Institute; Bethesda, MD: 2012. Retrieved July 24, 2012, Available at: http://seer.cancer.gov/csr/1975_2009_pops09/ [Google Scholar]
- Keegan THM, Gomez SL, Clarke CA, et al. Recent trends in breast cancer incidence among 6 Asian groups in the greater bay area of northern California. Int J Cancer. 2007;120:1324–9. doi: 10.1002/ijc.22432. [DOI] [PubMed] [Google Scholar]
- Lee MM, Lee F, Stewart S, McPhee S. Cancer screening practices among primary care physicians serving Chinese Americans in San Francisco. West J Med. 1999;170:148–55. [PMC free article] [PubMed] [Google Scholar]
- Lubetkin EI, Santana A, Tso A, Jia H. Predictors of cancer screening among low-income primary care patients. J Health Care Poor Underserved. 2008;19:135–48. doi: 10.1353/hpu.2008.0001. [DOI] [PubMed] [Google Scholar]
- Meissner HI, Klabunde CN, Han PK, et al. Breast cancer screening beliefs, recommendations, and practices. Cancer. 2011;117:3101–11. doi: 10.1002/cncr.25873. [DOI] [PubMed] [Google Scholar]
- Miller BA, Chu KC, Hankey BF, Ries LAG. Cancer incidence and mortality patterns among specific Asian and Pacific Islander populations in the U.S. Cancer Causes Control. 2008;19:227–56. doi: 10.1007/s10552-007-9088-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Cancer Institute. Stomach (Gastric cancer) Screening (PDQ): Patient version. 2012 Retrieved July 25, 2012. Available at: http://cancer.gov/cancertopics/pdq/screening/gastric/Patient/
- Nguyen TT, McPhee SJ, Stewart S, et al. Factors associated with hepatitis B testing among Vietnamese Americans. J Gen Intern Med. 2010;25:694–700. doi: 10.1007/s11606-010-1285-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Malley AS, Renteria-Weitzman R, Huerta EE, et al. Patient and provider priorities for cancer prevention and control: a qualitative study in mid-Atlantic Latinos. Ethn Dis. 2002;12:383–91. [PubMed] [Google Scholar]
- Shieh K, Gao F, Ristvedt S, et al. The impact of physicians’ health beliefs on colorectal cancer screening practices. Dig Dis Sci. 2005;50:809–14. doi: 10.1007/s10620-005-2644-3. [DOI] [PubMed] [Google Scholar]
- Strong C, Lee S, Tanaka M, Juon HS. Ethnic differences in prevalence and barriers of HBV screening and vaccination among Asian Americans. J Community Health. 2012;37:1071–80. doi: 10.1007/s10900-012-9541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su X, Ma GX, Seals B, et al. Breast cancer early detection Harry T Kwon et al among Chinese women in the Philadelphia area. J Womens Health. 2006;15:507–19. doi: 10.1089/jwh.2006.15.507. [DOI] [PubMed] [Google Scholar]
- Taylor VM, Yasui Y, Burke N, et al. Pap testing adherence among Vietnamese American women. Cancer Epidemiol Biomarkers Prev. 2004;13:613–19. [PubMed] [Google Scholar]
- Tsui T, Tanjasiri SP. Cervical cancer screening among Thai women in Northern California. J Womens Health. 2008;17:393–401. doi: 10.1089/jwh.2007.0427. [DOI] [PubMed] [Google Scholar]
- Tu SP, Yasui Y, Kuniyuki AA, et al. Mammography screening among Chinese-American women. Cancer. 2003;97:1293–302. doi: 10.1002/cncr.11169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yabroff KR, Saraiya M, Meissner HI, et al. Specialty differences in primary care physician reports of Papanicolaou test screening practices: A national survey, 2006 to 2007. Ann Intern Med. 2009;151:1602–11. doi: 10.7326/0003-4819-151-9-200911030-00005. [DOI] [PubMed] [Google Scholar]