Abstract
Background
Incisional pain is particularly troublesome after hysterectomy. A method called transversus abdominis plane block (TAPB) has shown promise in managing postoperative pain. In this study, we evaluated the analgesic efficacy of ultrasound-guided TAPB after hysterectomy at different time points and at each time point separately for 48 hours.
Methods
Forty-two patients (ASA I, II) who were electively chosen to undergo total abdominal hysterectomy were divided into 2 groups, control (group C) and intervention (group I). Twenty-one patients underwent TAPB (group I) and 21 patients received only the standard treatment with a fentanyl pump (group C). Both groups received standard general anesthesia. For patients in group I, following the surgery and before emergence from anesthesia, 0.5 mg/kg of ropivacaine 0.2% (about 20 cc) was injected bilaterally between the internal oblique and transverse abdominis muscles using sonography. Pain scores using the Visual Analogue Scale (VAS) and drug consumption were measured at 2, 6, 12, 24, and 48 hours after TAPB.
Results
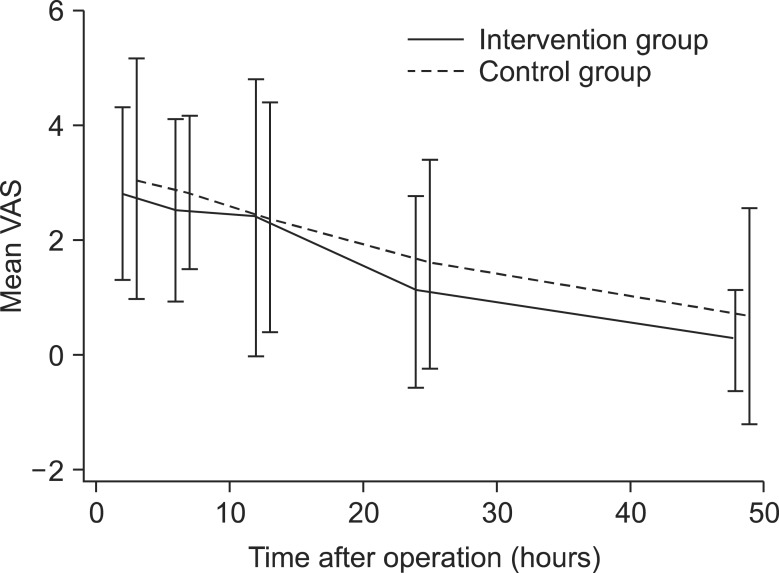
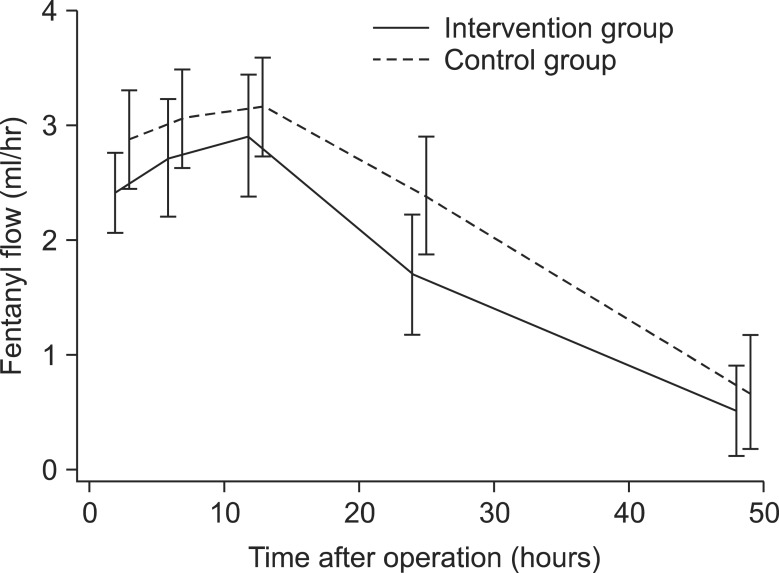
There were no significant differences in demographics between the two groups. VAS scores appeared to be lower in group I, although there was no interaction with time when we compared mean VAS measurements at different time points between group I and group C (P > 0.05). The amount of fentanyl flow was consistently higher in group C, but when we compared the two groups at each time point separately, the observed difference was not statistically significant (P < 0.053). The incidence of vomiting was 10% in group I and 28% in group C. There were no complaints of itching, and sedation score was 0 to 3. There were no complications.
Conclusions
This study showed that TAPB did not result in a statistically significant decrease in VAS scores at different time points. TAPB did lead to decreased fentanyl flow, but when we compared the two groups at each time point separately, the observed difference was not statistically significant.
Keywords: fentanyl, hysterectomy, transversus abdominis plane block
INTRODUCTION
Total abdominal hysterectomy is a major surgery that results in severe postoperative pain. Patients undergoing hysterectomy require a high-quality multimodal pain management program with a low rate of complications. The treatment of choice is generally opioids, which cause sedation, nausea, and vomiting [1-3]; therefore a method is needed to decrease opioid consumption and its complications. Incisional pain is particularly troublesome after hysterectomy. Because the sensory afferent nerves run between the abdominal muscles [4], by a method called transversus abdominis plane block (TAPB), these nerves could be blocked and postoperative pain could be managed. This has been found to be an effective method in colonectomy [5], cesarean section with midline incision [6], and prostatectomy [7], and it is also effective in managing pain following abdominal hysterectomy [8]. Use of sonography for placement of the needle and drug distribution can lower the risks associated with TAPB, particularly in overweight people, and increases the safety and effectiveness of the block [9]. Until now there have been no clinical trials conducted to determine the value of ultrasound-guided TAPB at different time points after total abdominal hysterectomy. In this study, we examined the effect of TAPB in managing post-hysterectomy pain at different post-surgical time points and we analyzed the procedure's complications.
The purpose of this study was to determine the analgesic efficacy of ultrasound-guided TAPB after hysterectomy at different time points and at each time point separately. Our hypothesis was that ultrasound-guided TAPB could manage the pain and reduce the amount of fentanyl consumed via analgesic pump for 48 hours during the times.
MATERIALS AND METHODS
After receiving approval from our institution's ethics committee and individual consent from the study volunteers, 42 patients (ASA I, II) were electively chosen to undergo total abdominal hysterectomy. Exclusion criteria included patients' dissatisfaction, allergies to local anesthetics, infection in the injection site, coagulation disorders, any internal, brain, mental or physical illnesses which could interfere with the evaluation of VAS scores, addiction to drugs or alcohol, liver or kidney failure, or severe obesity.
In this clinical trial study, patients were selected by random number table. They were divided into 2 groups, control (group C) and intervention (group I). Twenty-one patients underwent TAPB (group I). The patients, gynecologist, and pain management group were blinded to the group selection. Both groups received general anesthesia. All patients received the standard treatment of 1.2 µ/kg fentanyl by infusion pump (2 ml/hr speed of infusion). VAS scores and the amount of fentanyl flow were measured at 2, 6, 12, 24, and 48 hours after TAPB. In cases in which the VAS score was over 3, a flow of 2 ml/h was added to the speed of infusion; if the VAS score was 1-3, the old speed would be used; and if the patient reported no pain, the infusion would be cut off. Complications due to injection, nausea (0 = none, 1 = low, 2 = medium, 3 = severe), Ramsay sedation score according to Ramsay sedation scale (0 = awake, 1 = wakes up quickly, 2 = asleep but wakes up easily, 3 = deep sleep), and itchiness (0 = none, 1 = medium, 2 = medium need of treatment, 4 = severe) were recorded (score more than 0 for nausea, vomiting, and itching considered). In patients with nausea, 4 mg IV ondansetron was administered. In cases in which the sedation score was 3, the fentanyl infusion would be cut off, and in cases of itching, intravenous diphenhydramine was injected. The overall amount of fentanyl received was recorded.
Patients were placed in the supine position. They were anesthetized with 1.5 µ/kg fentanyl, 3 mg/kg propofol, 1.5 µ/kg midazolam, and 0.5 mg/kg atracurium. Anesthesia was maintained with 150 µ/kg/min propofol and 1.5 µ/kg fentanyl. After the procedure and before patients awakened, TAPB was performed in group I. The injection site was located between the iliac crest and the lower costal margin. Through in-plane technique under the guidance of sonography, the SonoTAP cannula (21 G, 110 mm) needle was inserted between the internal oblique and transverse abdominis muscles, deep to the fascia. After aspiration, 0.5 mg/kg of 0.2% ropivacaine was injected and correct distribution of the drug was confirmed by sonography (Fig. 1).
Fig. 1.
Needle pass through muscle layers. Needle tip between internal oblique and transverse abdominis muscles.
Statistical analysis was performed using Sata 11 and SPSS 11. Values for volunteers' demographic information were shown as medium. Fentanyl infusion speed (flow) and VAS scores in different time periods were measured as mean (SD); these were compared between both groups by t-test. P values less than 0.05 were considered statistically significant. Prevalence of nausea was measured by the Chi-square test (the minimum expected count is 3.90).
RESULTS
There were no significant differences in demographics between the two groups (median age in group I was 64 years versus 65 years in group C, and mean weight was 71.2 kg in group I versus 72 kg in group C). In this study, we compared VAS scores and fentanyl consumption at different time points and at each time point separately. VAS scores appeared to be lower in group I, although there was no interaction with time when we compared mean VAS measurements at different time points between groups I and C (P > 0.05) (Fig. 2). The amount of fentanyl flow was consistently higher in group C, but when we compared the two groups at each time point separately, the observed difference was not statistically significant (Fig. 3). Total fentanyl consumption was also not statistically significantly different (P < 0.053) when analyzed at each time point separately. The incidence of vomiting was 10% in group I and 28% in group C. Although the incidence of vomiting was higher in group C, the difference was not statistically significant (value = 2.250). No patients complained of itching, and sedation score was 0 to 3. There were no complications from TAPB.
Fig. 2.
Comparison of VAS scores over time following the TAH.
Fig. 3.
Comparing mean of flow for fentanyl.
DISCUSSION
TAPB is a compartment block in which the local anesthesia is distributed deep to the fascia between the internal oblique muscles and the transverse abdominis muscles. It blocks almost all of the visceral nerves that pass through the abdominal structures that are cut during abdominal incision and are a cause of pain generation after surgery [7,10,11]. TAPB was first described by Rafi [12], Hebbard was the first to use sonography for this type of block [13], and the procedure was named by McDonnell [7,11]. This method is a suitable substitute for epidural analgesia in abdominal surgeries. TAPB reduces opioid consumption and its complications (nausea, vomiting, urinary retention, decrease in blood pressure), and does not have the complications of neuroaxial block (decrease in blood pressure, motor block). The procedure is simple and easily available, without any encroachment on the epidural space with effective analgesia, and it is very suitable in patients who are not candidates for epidural analgesia [14,15]. In a double-blind study examining TAPB after abdominal hysterectomy [8], most of the patients' pains were scored but not all of them decreased, although they used more analgesic than we did in our study, as well as a higher concentration of ropivacaine postoperatively. Categorical pain scores were decreased only at 12, 36, and 48 hours postoperatively, the patients had lower incidence of sedation (37 vs 63%), and no nausea was observed. As in our study, there were no reports of complications due to TAPB. A study by Kanazi et al. [16] found that ultrasound-guided TAPB with bupivacaine is not as effective as subarachnoid morphine along with bupivacaine for cesarean section. Painkillers were demanded more in the TAPB group at 0 and 12 hours postoperatively, similarly to our study, in which VAS scores seemed higher at 12 hours postoperatively in group I. In another study, the effectiveness of blind TAPB in comparison with a standard method of analgesia (morphine pump along with acetaminophen and diclofenac sodium suppository) was proved in the first 24 hours following large bowel surgery [5]. Another study, conducted by McDonnell et al. [6], found that blind TAPB along with a multimodal pain management regimen after cesarean section had good analgesic effects. In this study, 1.5 mg/kg ropivacaine was used bilaterally, and both groups received standard analgesia as in the previous study, which is higher than the dosages used in our study. Pain scores were decreased at only some of the time points in the TAPB group. The incidence of sedation was 36% in control group in comparison with 0 in the TAPB group. According to another study [17], morphine consumption decreases after ultrasound-guided TAPB in cesarean section. Although satisfaction rates were higher in the TAPB group, there were no differences in VAS scores between groups. There were also no complications reported in this study due to TAPB. Only one person experienced ecchymosis, less than 1 cm in diameter, in the injection area. Itching and sedation were seen in both groups. Blind TAPB after outpatient cholecystectomy showed that TAPB is ineffective for the duration of surgery but had more analgesic effect in the recovery room (P = 0.003). Another study found that TAPB resulted in the same amount of analgesia in comparison with trocar incision infiltration in laparoscopic cholecystectomy [18].
Our first outcome was to determine VAS scores at 2, 6, 12, 24, and 48 hours after TAPB, and our second outcome was to determine the amount of opioid consumption after the block to compare VAS scores and fentanyl consumption at different time points and at each time point separately. Limitations of this study include the performance of the block by many different pain fellows. Although the same technique, with sonography guidance, was performed in all the patients, there were technical differences. In addition, although most of the surgeries were performed by one gynecologist, the duration of the surgeries differed, which can affect postoperative stress and the amount of opioid consumption. We also used lower concentrations of local anesthetics in comparison with other studies. Perhaps a higher concentration of ropivacaine could be more effective in analgesic difference between the two groups. Overall, this study showed that TAPB could not cause a statistically significant decrease in patients' pain scores at different time points. TAPB decreases postoperative opioid consumption, but if the two groups are compared at each time point separately, the observed difference is not statistically significant. The usage of fentanyl instead of morphine, which was used in previous studies, resulted in fewer complications. We experienced no complications due to TAPB.
References
- 1.Stanley G, Appadu B, Mead M, Rowbotham DJ. Dose requirements, efficacy and side effects of morphine and pethidine delivered by patient-controlled analgesia after gynaecological surgery. Br J Anaesth. 1996;76:484–486. doi: 10.1093/bja/76.4.484. [DOI] [PubMed] [Google Scholar]
- 2.Woodhouse A, Mather LE. The effect of duration of dose delivery with patient-controlled analgesia on the incidence of nausea and vomiting after hysterectomy. Br J Clin Pharmacol. 1998;45:57–62. doi: 10.1046/j.1365-2125.1998.00635.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ng A, Swami A, Smith G, Davidson AC, Emembolu J. The analgesic effects of intraperitoneal and incisional bupivacaine with epinephrine after total abdominal hysterectomy. Anesth Analg. 2002;95:158–162. doi: 10.1097/00000539-200207000-00028. [DOI] [PubMed] [Google Scholar]
- 4.Netter FH. Back and spinal cord. In: Netter FH, editor. Atlas of human anatomy. (NJ): Ciba-Geigy Corporation; 1989. pp. 145–155. [Google Scholar]
- 5.McDonnell JG, O'Donnell B, Curley G, Heffernan A, Power C, Laffey JG. The analgesic efficacy of transversus abdominis plane block after abdominal surgery: a prospective randomized controlled trial. Anesth Analg. 2007;104:193–197. doi: 10.1213/01.ane.0000250223.49963.0f. [DOI] [PubMed] [Google Scholar]
- 6.McDonnell JG, Curley G, Carney J, Benton A, Costello J, Maharaj CH, et al. The analgesic efficacy of transversus abdominis plane block after cesarean delivery: a randomized controlled trial. Anesth Analg. 2008;106:186–191. doi: 10.1213/01.ane.0000290294.64090.f3. [DOI] [PubMed] [Google Scholar]
- 7.O'Donnell BD, McDonnell JG, McShane AJ. The transversus abdominis plane (TAP) block in open retropubic prostatectomy. Reg Anesth Pain Med. 2006;31:91. doi: 10.1016/j.rapm.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 8.Carney J, McDonnell JG, Ochana A, Bhinder R, Laffey JG. The transversus abdominis plane block provides effective postoperative analgesia in patients undergoing total abdominal hysterectomy. Anesth Analg. 2008;107:2056–2060. doi: 10.1213/ane.0b013e3181871313. [DOI] [PubMed] [Google Scholar]
- 9.Shibata Y, Sato Y, Fujiwara Y, Komatsu T. Transversus abdominis plane block. Anesth Analg. 2007;105:883. doi: 10.1213/01.ane.0000268541.83265.7d. [DOI] [PubMed] [Google Scholar]
- 10.McDonnell JG, O'Donnell BD, Farrell T, Gough N, Tuite D, Power C, et al. Transversus abdominis plane block: a cadaveric and radiological evaluation. Reg Anesth Pain Med. 2007;32:399–404. doi: 10.1016/j.rapm.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 11.Russon K, Blanco R. Ultrasound-guided transversus abdominal plane block. In: Bigeleisen PE, editor. Ultrasound guided regional anesthesia and pain medicine. Philadelphia (PA): Lippincott Williams & Wilkins Health; 2010. pp. 93–96. [Google Scholar]
- 12.Rafi AN. Abdominal field block: a new approach via the lumbar triangle. Anaesthesia. 2001;56:1024–1026. doi: 10.1046/j.1365-2044.2001.02279-40.x. [DOI] [PubMed] [Google Scholar]
- 13.Hebbard P. Subcostal transversus abdominis plane block under ultrasound guidance. Anesth Analg. 2008;106:674–675. doi: 10.1213/ane.0b013e318161a88f. [DOI] [PubMed] [Google Scholar]
- 14.Niraj G, Kelkar A, Jeyapalan I, Graff-Baker P, Williams O, Darbar A, et al. Comparison of analgesic efficacy of subcostal transversus abdominis plane blocks with epidural analgesia following upper abdominal surgery. Anaesthesia. 2011;66:465–471. doi: 10.1111/j.1365-2044.2011.06700.x. [DOI] [PubMed] [Google Scholar]
- 15.Mokini Z. Transverse abdominal plexus block. In: Mokini Z, Vitale G, Costantini A, Fumagalli R, editors. The flying publisher guide to ultrasound blocks for the anterior abdominal wall: principles and implementation for adult and pediatric surgery. Wuppertal: Flying Publisher; 2011. p. 35. [Google Scholar]
- 16.Kanazi GE, Aouad MT, Abdallah FW, Khatib MI, Adham AM, Harfoush DW, et al. The analgesic efficacy of subarachnoid morphine in comparison with ultrasound-guided transversus abdominis plane block after cesarean delivery: a randomized controlled trial. Anesth Analg. 2010;111:475–481. doi: 10.1213/ANE.0b013e3181e30b9f. [DOI] [PubMed] [Google Scholar]
- 17.Belavy D, Cowlishaw PJ, Howes M, Phillips F. Ultrasound-guided transversus abdominis plane block for analgesia after caesarean delivery. Br J Anaesth. 2009;103:726–730. doi: 10.1093/bja/aep235. [DOI] [PubMed] [Google Scholar]
- 18.El Bayoumy R, Khan O, King E, Wainwright D, Sadek S. Trans-abdominal plane (TAP) block analgesia in day case laparoscopic cholecystectomy - a prospective study: 14AP12-6. Eur J Anaesth. 2010;27:222. [Google Scholar]