Abstract
Most studies related to BRCA mutations have been performed in Western populations, and only a few small studies have been conducted in Korean populations. In 2007, the Korean Hereditary Breast Cancer (KOHBRA) Study was established to obtain evidence for the accurate risk assessment and management of hereditary breast and ovarian cancer (HBOC) in Korea. Between May 2007 and May 2010, the first phase of the KOHBRA Study was performed to estimate the prevalence of BRCA1/2 mutations among patients and their families at risk for HBOC. Between June 2010 and May 2013, the second phase of the KOHBRA Study was performed to identify the clinical characteristics and prognostic indicators of BRCA-related breast cancer and environmental and genetic modifiers of BRCA mutations and to develop a Korean BRCA risk calculator and nationwide genetic counseling network for HBOC. Herein, we review the results of the KOHBRA Study and describe the future perspectives of the study.
Keywords: BRCA1 genes, BRCA2 genes, Breast neoplasms, Hereditary neoplastic syndromes
INTRODUCTION
Breast cancer is the most common cancer among women worldwide [1] and the second most common cancer in Korean women [2]. Genetic predisposition is an important risk factor for breast cancer, accounting for 5% to 10% of all breast cancer cases [3]. To date, 5 high-penetrance genes (BRCA1, BRCA2, TP53, PTEN, and LKB1), 4 intermediate-penetrance genes (ATM, BRIP1, CHEK2, and PALB2), and various low-penetrance loci (rs3803662, rs889312, rs3817198, and rs13281615) have been discovered [4]. BRCA1 and BRCA2 mutations are responsible for most hereditary breast cancers (HBCs).
BRCA1 and BRCA2 were identified in 1994 and 1995, respectively [5,6]. Since then, numerous epidemiologic and clinical studies have been performed; however, most of these studies were based on Western populations. Previous studies revealed that the prevalence of BRCA1 and BRCA2 mutations differs among diverse ethnic groups [7]. The penetrance of BRCA mutations also differs between ethnicities, and this may be associated with the potential modifying effects of individual environmental and genetic backgrounds. In Korea, BRCA1 mutation was first reported in 1995 [8]; however, few studies of BRCA1/2 were performed until the early 2000s. The opportunity for BRCA1/2 genetic testing and cancer prevention has been overlooked in the Korean population.
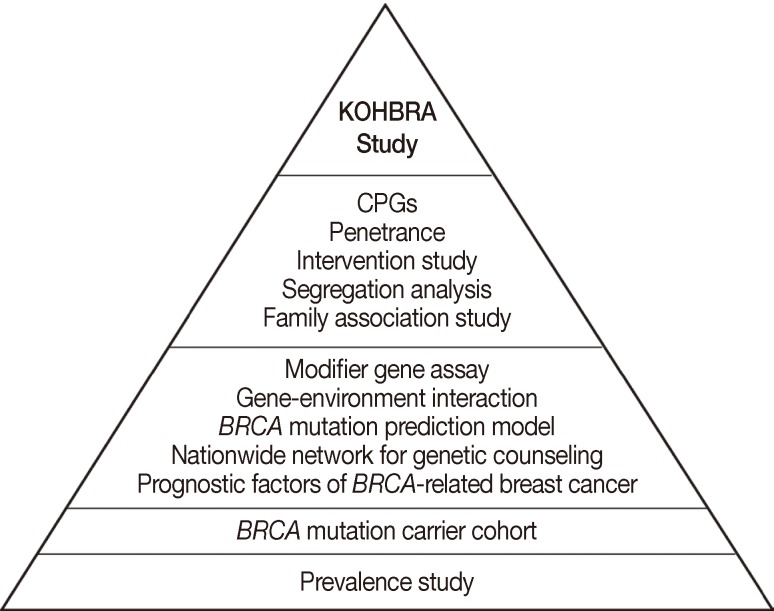
In May 2007, the Korean Hereditary Breast Cancer (KOHBRA) Study, a large, prospective, nationwide study, was established to acquire evidence for the accurate risk assessment and management of hereditary breast and ovarian cancer (HBOC) in the Korean population. The KOHBRA Study was planned as a 10-year project to develop Korean clinical practice guidelines (CPGs) for HBC (Figure 1). Between May 2007 and May 2010, the first phase of the KOHBRA Study was conducted to estimate the prevalence of BRCA1/2 mutations among patients and their families at risk of HBOC, to identify Korean founder mutations, and to establish a BRCA1/2 mutation carrier cohort. Between June 2010 and May 2013, the second phase of the KOHBRA Study was conducted to identify the clinicopathological characteristics and prognostic factors of BRCA-related breast cancer and environmental and genetic modifiers of BRCA mutations and to develop a Korean BRCA risk prediction model and nationwide genetic counseling network for HBC in Korea. In this article, we review the studies conducted through the KOHBRA Study over the past 6 years and describe the future perspectives of the study.
Figure 1.
The Korean Hereditary Breast Cancer (KOHBRA) Study. The KOHBRA Study was planned as a 10-year project to develop Korean clinical practice guidelines (CPGs).
PREVALENCE OF BRCA MUTATIONS AND FOUNDER MUTATION
Between May 2007 and May 2010, 1967 subjects from 36 institutions were enrolled in the KOHBRA Study, and all subjects received genetic counseling and BRCA genetic testing [9]. The following individuals were eligible for inclusion in the KOHBRA Study: 1) patients with breast cancer and a family history of breast or ovarian cancer; 2) patients with breast cancer without a family history of breast or ovarian cancer who were ≤40 years of age at diagnosis, diagnosed with bilateral breast cancer or another primary malignancy related to BRCA mutations, or male; and 3) family members of BRCA1/2 mutation carriers [10]. Recently, we reported 2 BRCA mutation prevalence studies for patients with familial [11] and nonfamilial breast cancers who were at risk for HBOC [9]. A summary of BRCA1/2 mutation prevalence according to risk factors is shown in Table 1. Of the 775 breast cancer patients with family histories of breast or ovarian cancer, 168 patients (21.7%) were determined to have deleterious BRCA1/2 mutations (BRCA1, 9.3%; BRCA2, 12.4%). From this study, we were able to identify subsets of the population with a BRCA mutation prevalence exceeding the 10% threshold commonly used to select families for BRCA genetic testing. These subsets included breast cancer patients with 1 or more relatives who had ovarian cancer at any age and breast cancer patients with a family history of breast cancer and 1 or more of the following: 2 or more family members with breast cancer; 1 family member diagnosed with breast cancer (age at diagnosis <50 years for at least 1 case); and other risk factors including bilateral breast cancer and a personal history of ovarian cancer. Among the 758 patients without family histories of breast or ovarian cancer who were at risk for HBOC, the overall BRCA mutation prevalence was 8.6% (BRCA1, 3.3%; BRCA2, 5.3%). According to the risk classification, the prevalence of BRCA1/2 mutations was 10.0% among 270 patients with early-onset disease (diagnosed at age <35 years), 17.7% among 124 patients with bilateral breast cancer, 50.0% among 6 patients with breast and ovarian cancer, 5.9% among 17 male patients with breast cancer, and 7.6% among 17 patients with multiple organ cancer [9]. Based on these results, genetic counseling for HBOC should be offered for patients with early-onset nonfamilial breast cancer, bilateral breast cancer, and breast and ovarian cancer, as these patients had a BRCA1/2 mutation prevalence exceeding 10%. These findings are largely consistent with the National Comprehensive Cancer Network (NCCN) guidelines for BRCA testing [12]. However, we could not obtain accurate prevalence data for several subsets due to small sample sizes, especially for male patients with breast cancer and patients with both breast and ovarian cancer. Continuous recruitment has been performed to obtain more accurate prevalence data. The KOHBRA Study recruited 3,144 patients and family members at high risk for HBOC from 40 centers between May 2007 and April 2013 and plans to report the comprehensive prevalence table for BRCA mutations using this larger sample size.
Table 1.
Prevalence of BRCA1/2 mutation among breast cancer patients according to risk factors
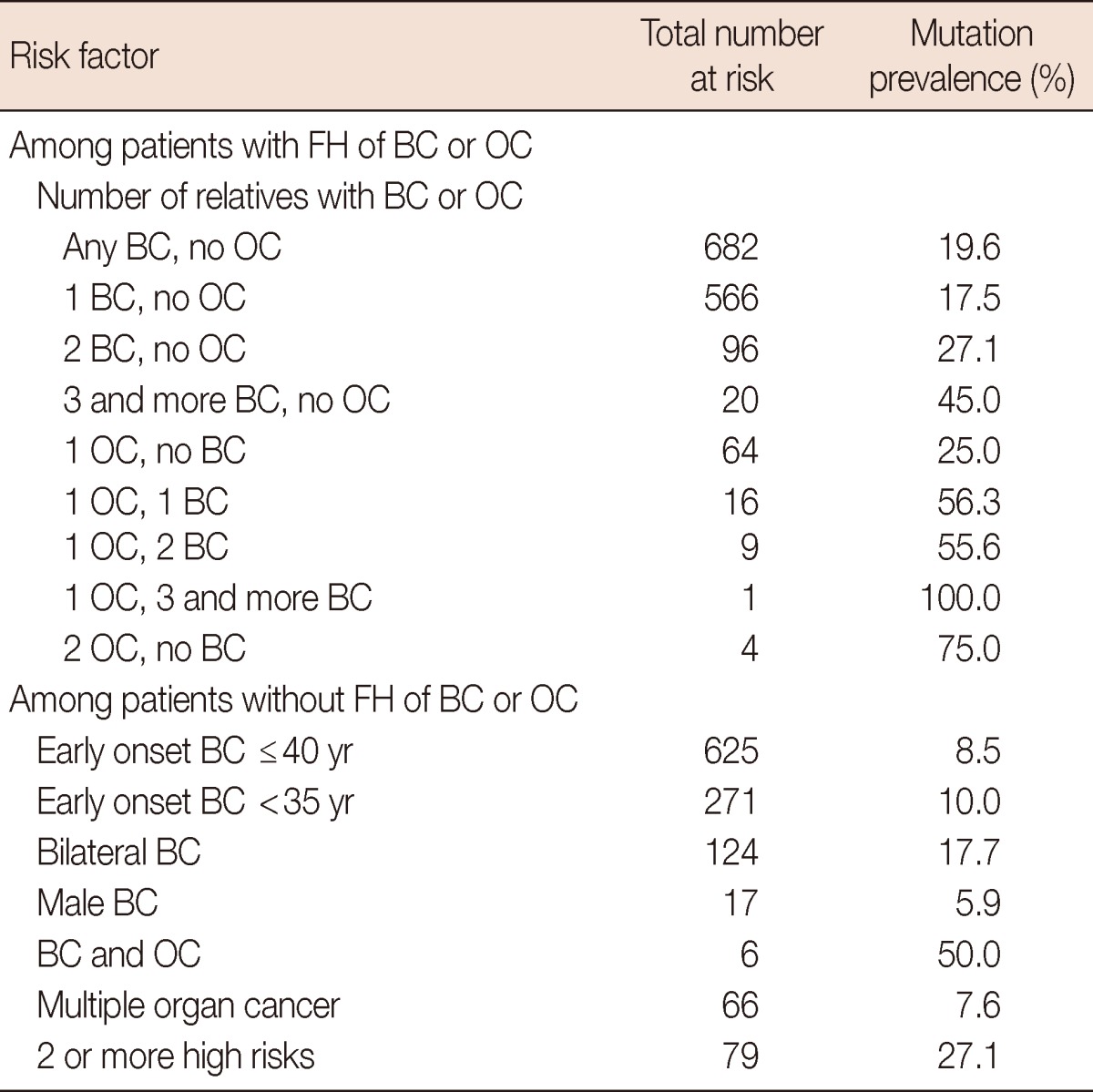
FH=family history; BC=breast cancer; OC=ovary cancer.
Thirty-three and 35 distinct BRCA1 and BRCA2 mutations were identified in the interim analysis of 831 patients with familial or nonfamilial breast cancer in the KOHBRA Study cohort, respectively [10]. Among these 68 mutations, the 7708C>T (p.Arg2494X) BRCA2 mutation (12%) was the most common (Table 2). This mutation was identified as a Korean founder mutation in the haplotype analysis by Seong et al. [13]. The 7708C>T (p.Arg2494X) BRCA2 mutation was the most frequently detected mutation in 3,922 Korean breast cancer patients based on pooled BRCA1/2 data collected since the first Korean BRCA1 mutation report (with the exception of the KOHBRA Study data) [14].
Table 2.
The candidates for the Korean founder mutation (n=148)
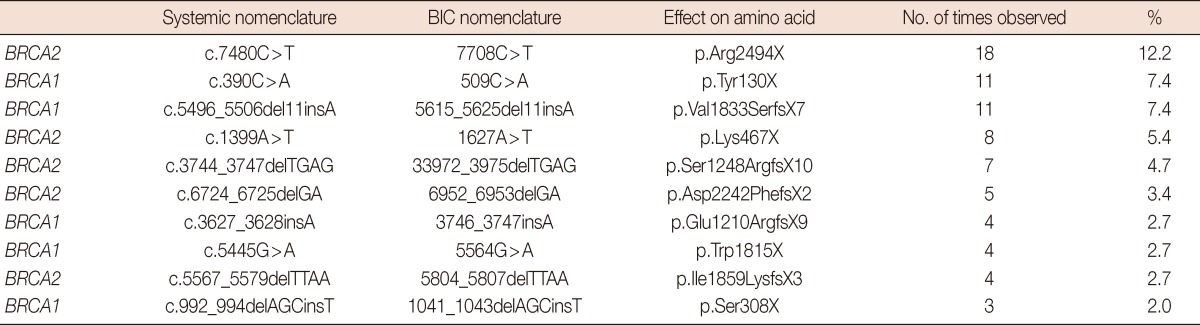
BIC=breast cancer information core.
BREAST AND OVARIAN CANCER RISKS ASSOCIATED WITH BRCA MUTATIONS
Individuals with BRCA mutations receive personalized management strategies including intensive surveillance and prophylactic surgeries according to their cancer risks. In a meta-analysis, the risks of developing breast and ovarian cancers among BRCA1/2 mutation carriers by the age of 70 years were 57% (95% confidence interval [CI], 47%-66%) and 40% (95% CI, 35%-46%) for BRCA1 mutation carriers and 49% (95% CI, 40%-57%) and 18% (95% CI, 13%-23%) for BRCA2 mutation carriers, respectively [15]. The penetrance of BRCA1/2 mutations varies according to country and race because various genetic and environmental factors have been linked to the development of breast cancer. To assist in decision-making for cancer prevention based on evidence from Korean studies, the KOHBRA Study group estimated the cumulative risk of breast and ovarian cancers among 61 BRCA1 and 47 BRCA2 mutation carrier families using Kaplan-Meier analyses [16]. The average cumulative risk of breast and ovarian cancers to age 70 years was estimated to be 72.1% (95% CI, 59.5%-84.8%) and 24.6% (95% CI, 0%-50.3%) for BRCA1 mutation carriers and 66.3% (95% CI, 41.2%-91.5%) and 11.1% (95% CI, 0%-31.6%) for BRCA2 mutation carriers, respectively (Table 3). These results are similar to those from a meta-analysis of previous studies performed in Western populations. According to these findings, Koreans with BRCA mutations should be informed of their cancer risks and appropriate cancer prevention strategies should be implemented. However, the limitations of this study included the small number of cases, the high proportion of probands, the short follow-up period, and the large CIs. We expect to provide a more conclusive answer regarding the penetrance of BRCA mutations from the prospective follow-up of a large number of families carrying deleterious BRCA1 and BRCA2 mutations in the KOHBRA Study.
Table 3.
Cumulative risk till each age of breast and ovarian cancer among family members with BRCA1/2 mutation carriers
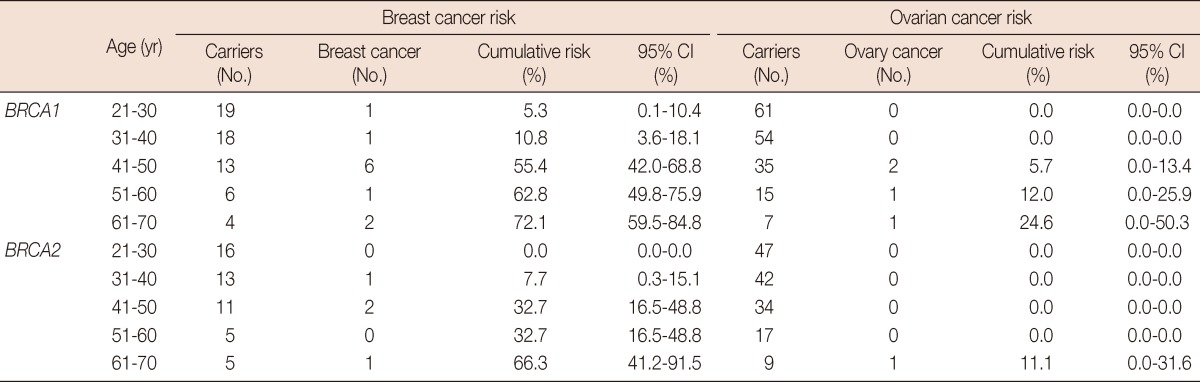
CI=confidence interval.
BREAST CANCER SURVIVAL IN BRCA1/2 MUTATION CARRIERS
Previous studies comparing the survival of BRCA1/2 mutation carriers and noncarriers with breast cancer have reported inconsistent findings. Some studies observed significantly worse survival in BRCA1 mutation carriers than in sporadic breast cancer patients [17,18], whereas others reported similar outcomes between BRCA1/2 mutations carriers and noncarriers [19,20]. Recently, a large population study found similar 10-year survival rates among BRCA1 and BRCA2 mutation carriers and noncarriers. Therefore, it is generally accepted that the prognosis of BRCA1/2 mutation carriers is not different from that of noncarriers [21].
The inconsistent findings of the previous studies of breast cancer survival in BRCA1/2 mutation carriers may be due to the differences between BRCA1 and BRCA2, the relatively small number of BRCA carriers, and the different primary outcomes and follow-up periods. To overcome these limitations, the KOHBRA Study group performed a meta-analysis of 11 studies of BRCA mutations and the risk of death or recurrence to evaluate the short and long-term overall survival (OS) and disease-free survival (DFS) rates of BRCA1 and BRCA2 mutation carriers relative to that of noncarriers [22]. Breast cancer patients with BRCA1 mutations had significantly lower short-term and long-term OS rates than noncarriers (hazard ratio [HR], 1.92 [95% CI, 1.45-2.53]; HR, 1.33 [95% CI, 1.12-1.58]). Conversely, short-term and long-term OS rates were similar in BRCA2 mutation carriers and noncarriers (HR, 1.30 [95% CI, 0.95-1.76]; HR, 1.12 [95% CI, 0.86-1.45]). BRCA1 mutation carriers had a significantly worse short-term DFS rate than noncarriers (HR, 1.54; 95% CI, 1.12-2.12), whereas short-term DFS rate was similar for BRCA2 mutation carriers and noncarriers (HR, 1.23; 95% CI, 0.96-1.58). These findings suggested that BRCA1 mutations worsen short and long-term OS rates and short-term DFS rate, whereas BRCA2 mutations do not influence short or long-term OS rates or short-term DFS rate.
RISK ASSESSMENT FOR HBOC IN KOREA
The first step of genetic counseling and testing for HBOC is the risk assessment for clinically significant BRCA1/2 mutations. Genetic testing is usually recommended for individuals with strong family histories of breast and ovarian cancers, early-onset breast cancer, bilateral breast cancer, and both breast and ovarian cancer. Several BRCA risk prediction models are also used to accurately evaluate the probability that an individual carries a pathogenic BRCA1 or BRCA2 mutation. The most widely used models are the Myriad II [23], BRCAPRO [24], Breast and Ovarian Analysis of Disease Incidence and Carrier Estimation Algorithm [25], and Manchester [26] models, which were developed using data obtained from Caucasians. BRCAPRO and Myriad II were validated for various races, and these models underestimated the proportion of BRCA1/2 mutation carriers among Asians [27].
In the second phase of the KOHBRA Study, the accuracy of the BRCAPRO and Myriad II models was evaluated in 236 Korean female breast cancer patients who underwent BRCA1/2 mutation testing [28]. We found that these Western models significantly underestimated the overall number of BRCA1/2 mutations (observed mutation rate, 19.5%; BRCAPRO predicted rate, 9.0%; Myriad II predicted rate, 5.6%). The observed mutation rates were >10% for patients with family histories of breast cancer (proband diagnosed at age >50 years), only 1 relative with breast cancer, early-onset breast cancer, and bilateral breast cancer; however, the predicted mutation rates in these groups were less than 10%. The results of this study demonstrated that these commonly used Western models are not appropriate for identifying candidates for BRCA mutation testing in the Korean population. Therefore, new BRCA risk prediction models were developed for the Korean population using the KOHBRA prevalence data. Approximately 1,600 female patients were used to construct the model, and logistic regression analysis was used to determine the predictive factors for pathogenic BRCA1/2 mutations and develop a model to predict mutation probability. Two models were constructed based on family history of breast and ovarian cancers: familial and nonfamilial. Factors included in the familial model were age at breast cancer diagnosis, bilateral breast cancer, triple-negative breast cancer (TNBC), and number of relatives with breast or ovarian cancer. Breast cancer diagnosis at age <35 years, bilateral breast cancer, both breast and ovarian cancers, and TNBC were factors included in the nonfamilial model. When all of this information was entered, the estimated probability of BRCA1/2 mutations and the observed prevalence data were calculated depending on the input. This BRCA mutation prediction model was named KOHCal (KOHBRA BRCA Risk Calculator) and is available on the KOHBRA Study website (www.kohbra.kr). We expect that our models will help select more suitable candidates for BRCA mutation testing and assist in the decision to perform genetic testing in the Korean population.
GENETIC COUNSELING FOR INDIVIDUALS AT RISK FOR HBOC
Genetic counseling is recommended before and after BRCA 1/2 genetic testing and should be performed by a specialized physician or genetic counselor. The purpose of genetic counseling is to help individuals better understand their inherited conditions and cancer risks and the impact on their families. The genetic counseling process includes the ascertainment of a patient's medical and family history; determination and communication of cancer risk; assessment of risk perception; education regarding the genetics of HBOC; discussion of the benefits, risks, and limitations of molecular testing for HBOC; and any necessary follow-up [29].
In 2007, before the first phase of the KOHBRA study, a nationwide survey of 43 healthcare providers was conducted to examine practice patterns for the management of HBOC [30]. Among the respondents, 81.4% ascertained family histories of cancer and 58.1% recommended BRCA1/2 genetic testing for their patients at risk for HBOC. However, only 52% of respondents who recommended genetic testing performed genetic counseling before genetic testing. In most instances, genetic counseling was conducted by doctors (81.3%); however, it was occasionally performed by nurses (18.7%). In 2009, a follow-up survey was conducted to evaluate changes in the practice patterns for managing HBOC after the KOHBRA Study [31]. Among 25 physicians who participated in both surveys, 60% indicated that they drew pedigrees, which was higher than the percentage (48%) in 2007. The proportion of physicians who recommended genetic testing for patients at risk for HBOC was higher in the 2009 survey (84.0%) than in the 2007 survey (64.0%). In the 2009 survey, physicians tended to select BRCA genetic testing criteria more appropriately than in the previous survey (42.4% answered correctly in the 2007 survey vs. 74.4% in the 2009 survey). The results of this survey demonstrated that the KOHBRA Study has played an important role in clarifying the proper protocol for genetic testing and selecting appropriate candidates for genetic testing for HBOC risk (Table 4).
Table 4.
The change of practice patterns for managing hereditary breast cancer after the KOHBRA Study
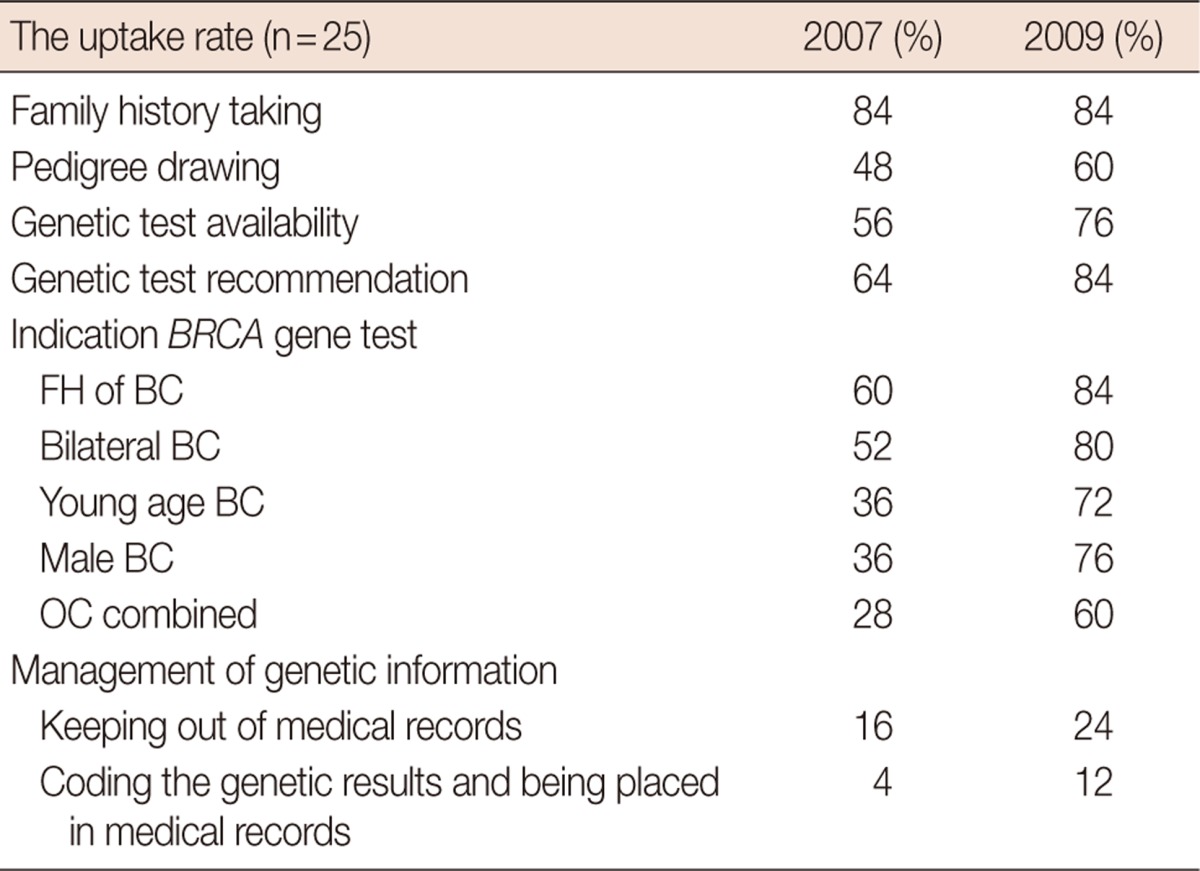
KOHBRA=Korean Hereditary Breast Cancer; FH=family history; BC=breast cancer; OC=ovary cancer.
Despite the contributions of the KOHBRA study, a lack of genetic counselors and a systematic protocol are unresolved issues impeding genetic counseling in Korea. Therefore, in the second phase of the KOHBRA Study, the KOHBRA Study group performed various tasks to improve the quality and availability of genetic counseling including constructing a nationwide network of genetic counseling; developing a textbook [32] and a manual [33] for HBOC; and training genetic counselors. The nationwide network for genetic counseling is composed of 9 regional hospitals (Ajou University Hospital, Busan National University Hospital, Chonnam National University Hwasun Hospital, Hallym University Sacred Heart Hospital, Konkuk University Medical Center, Seoul National University Bundang Hospital, Soonchunhyang University Cheonan Hospital, Soonchunhyang University Seoul Hospital, Yeungnam University Medical Center) from 4 provinces. This nationwide network has improved the accessibility of genetic counseling and enhanced the management of HBC. The Korean Breast Cancer Society created a certification system and training courses for HBOC counseling in 2011, and, to date, 30 genetic counselors have been certified for HBC. Through the KOHBRA Study, interactive computer programs were also developed to educate individuals about HBOC and genetic testing. These programs will be valuable resources to increase understanding and shorten counseling time when used before counseling. These programs are also available on the KOHBRA Study website (www.kohbra.kr).
The identification of a mutation in an affected member of the family confirms the clinical diagnosis of HBOC and provides an opportunity to evaluate and reduce the cancer risk for other family members. Therefore, understanding how families communicate information about HBOC and BRCA test results is important in the genetic counseling process. The KOHBRA Study group previously examined the disclosure patterns of positive test results to family members for 106 probands who carry pathogenic BRCA1/2 mutations [34]. Most participants (93.4%) shared the test result with at least 1 at-risk relative, and they informed a first-degree relative about their positive result. The communication of test results with second- or third-degree relatives occurred significantly less frequently, with only 31.3% of participants sharing their results with these family members. In this study, factors associated with disclosure of test results to more distant relatives included marital status and length of time since posttest counseling. The primary reason for disclosure was to provide information about cancer risk and to suggest genetic testing. These findings highlight the importance of encouraging patients to communicate with extended relatives through systematic genetic counseling.
MANAGEMENT OF BRCA MUTATION CARRIERS
Management options for women with BRCA mutations include close surveillance, chemoprevention, and risk-reducing surgery (RRS). According to the NCCN guidelines, monthly breast self-examinations beginning at age 18, clinical breast examinations twice annually beginning at age 25, and annual mammography and breast magnetic resonance imaging screening beginning at age 25 are recommended for breast cancer surveillance. Biannual ovarian cancer screening with transvaginal ultrasonography and CA-125 serology beginning at age 35 are recommended for ovarian cancer surveillance [12]. Because ovarian cancer screening is not sufficiently sensitive to detect ovarian cancer at an early stage, the preferred option for ovarian cancer prevention is risk-reducing salpingo-oophorectomy (RRSO) [35]. RRSO is recommended for BRCA mutation carriers the aged between 35 and 40 years (after the completion of childbearing) and reduces the risk of ovarian and breast cancers by 95% and 50%, respectively [36]. RRSO has also been associated with a reduction of all-cause, breast cancer-specific, and ovarian cancer-specific mortality [37]. The NCCN guidelines recommend discussing risk-reducing mastectomy (RRM) with BRCA1/2 mutation carriers, and reconstructive surgery and psychological consultation should also be considered in the decision-making process for RRM [12]. Chemopreventive agents such as tamoxifen for breast cancer and oral pills for ovary cancer may be considered to reduce cancer risk, and the benefits and risks of these agents should be discussed.
In Korea, the first case of a contralateral prophylactic mastectomy and RRSO in a BRCA mutation carrier with breast cancer was reported in 2008 [38], and the first case of bilateral prophylactic mastectomy in an asymptomatic BRCA mutation carrier was reported in 2010 [39]. However, chemoprevention and RRS for breast and ovarian cancer prevention are not widely performed in Korea. In 2011, the KOHBRA Study group reported the results of a study that investigated the usage patterns of surveillance, chemoprevention, and RRS for breast and ovarian cancer prevention in 67 BRCA1/2 mutation carriers in a single institution [40]. Among the 47 carriers affected with breast cancer, 89.4% received intensive surveillance only, 4.3% received tamoxifen, and 6.4% underwent contralateral prophylactic mastectomies for breast cancer prevention. Among the 17 unaffected carriers, only 23.5% underwent breast and ovarian cancer screening, and the others did not select any preventive option. This finding suggested that most Korean women with BRCA mutations chose intensive surveillance for cancer prevention. In addition, previous nationwide surveys of the management patterns of HBOC in 2007 and 2009 revealed the low uptake of chemoprevention and RRS for breast and ovarian cancer prevention in Korea [30,31].
A number of studies have examined the uptake of cancer risk management and associated factors among BRCA1/2 mutation carriers. Recently, the KOHBRA Study evaluated the factors affecting the decision to undergo RRSO among women with BRCA mutations in a single institution [41]. Among 71 carriers eligible for RRSO, 29.6% underwent RRSO. Although the uptake rate of RRSO in this particular institution was relatively high compared with that in other hospitals in Korea, it was lower than the rates in Western countries. The rate of RRSO was significantly higher in the fifth decade of life (52.6%) than in the fourth decade of life (33.3%) and sixth and later decades of life (10.7%). The rate of RRSO uptake was higher in carriers with a personal history of breast cancer than in those without a personal history of breast cancer (39.2% vs. 5.0%, p=0.004). A family history of breast or ovarian cancer was also associated with the uptake of RRSO in univariate analysis. The multivariate analysis revealed that age (fourth and fifth decades of life) and personal history of breast cancer were independent factors affecting the uptake of RRSO. Therefore, age, personal history of breast cancer, and other factors affecting the decision to undergo RRSO should be considered in the counseling process for BRCA mutation carriers. This study was limited by the small sample size and the single-institution design. Despite these limitations, this is the first study to evaluate the RRSO uptake rate and factors affecting the decision to undergo RRSO in BRCA1/2 carriers in an Asian country.
FUTURE OF THE KOHBRA STUDY
The KOHBRA Study established the prevalence of BRCA mutations in the Korean population according to risk factors, which will help healthcare providers select proper candidates for BRCA genetic testing. The risks of breast and ovarian cancers by age 70 years in Korean BRCA mutation carriers are similar to those of Western populations. Although the study has some limitations, we have been able to provide appropriate cancer prevention strategies based on the penetrance data. In the KOHBRA Study, we confirmed that BRCAPRO and Myriad II, 2 widely used Western BRCA mutation prediction models, underestimated the risk of BRCA1/2 mutations in Koreans. Therefore, a new BRCA risk calculator was developed for the Korean population. We determined the status of genetic counseling and management for HBOC, the psychological impact of genetic testing, and familial communication about HBOC in Korea by conducting various surveys. Based on this information, we explored methods to improve genetic counseling and management strategies for HBOC. To improve the quality of genetic counseling, the KOHBRA Study group developed a nationwide network of genetic counseling; developed a textbook, a manual, and animations for HBOC; and created a certification system and training courses for genetic counselors.
The KOHBRA Study group performed various domestic and international collaborative studies to identify genetic variants associated with breast cancer risk through genome-wide association studies [42-44]. We are also participating in the International BRCA1/2 Carrier Cohort Study and the Consortium of Investigators of Modifiers of BRCA1/2 to identify epidemiologic factors and genetic modifiers of cancer risk in BRCA1 and BRCA2 mutation carriers. In addition to these collaborative studies, the KOHBRA Study group established the Asian BRCA (ABRCA) Consortium in 2011, which initially consisted of Korea, Malaysia, Hong Kong, Japan, China, Indonesia, and Singapore. The aims of the ABRCA Consortium are to share knowledge about HBOC among Asian countries, improve the quality of care for patients with HBOC in Asia, and undertake collaborative studies on HBOC in Asia. To date, the annual meeting has been held in 2 rounds, in Malaysia (2012) and Hong Kong (2013), and includes participants from India, the Philippines, and Vietnam. The ABRCA working groups are conducting collaborative studies to review the BRCA mutation spectrum and founder mutations in Asia and evaluate the status of genetic counseling and genetic testing for HBOC in Asian countries. The working groups also plan to study the lifestyle modifiers of breast cancer and estimate the penetrance of BRCA mutations in Asian populations.
CONCLUSION
Over the past 6 years, we exerted great efforts to realize most of the goals of this 10-year project. This year, the first CPGs for HBOC will be published and incorporated into the 5th edition of the Korean breast cancer CPGs. The KOHBRA Study plans to identify the prognostic factors and genetic modifiers of BRCA-related breast cancer in Korea. We will also attempt to complete the remaining projects including a penetrance study conducted via the prospective follow-up of BRCA carriers and intervention studies to evaluate the efficacy of various cancer prevention options among BRCA mutation carriers.
ACKNOWLEDGEMENTS
We thank all participants and investigators of the KOHBRA Study: Beom Seok Kwak, Byeong-Woo Park, Byung Ho Son, Byung-In Moon, Cha Kyong Yom, Chan Heun Park, Chan Seok Yoon, Chang Hyun Lee, Dae Sung Yoon, Dong-Young Noh, Doo Ho Choi, Eundeok Chang, Eun-Kyu Kim, Eunyoung Kang, Hae Kyung Lee, Hai-Lin Park, Hyde Lee, Hyeong-Gon Moon, Hyun-Ah Kim, Il-Kyun Lee, Jeong Eon Lee, Jihyoun Lee, Jong Won Lee, Jong-Han Yu, Joon Jeong, Jung Han Yoon, Jung-Hyun Yang, Keumhee Kwak, Ki-Tae Hwang, Ku Sang Kim, Lee Su Kim, Min Hee Hur, Min Ho Park, Min Hyuk Lee, Myung Chul Chang, Nam Sun Paik, Sang Ah Han, Sang Seol Jung, Sang Uk Woo, Se Jeong Oh, Sehwan Han, Sei Joong Kim, Sei-Hyun Ahn, Seok-Jin Nam, Seung Sang Ko, Sung Hoo Jung, Sung Soo Kang, Sung Yong Kim, Sung-Won Kim, Tae Hyun Kim, Tae Wan Won, Tae Woo Kang, Wonshik Han, Woo-Chul Noh, Yong Lai Park, Yongsik Jung, Young Jin Suh, Young Tae Bae, Young Up Cho, Young-Ik Hong, Sue K. Park, Yoon Joo Jung, Su Yun Choi, Young Bum Yoo, Soo-Jung Lee.
Footnotes
This study was supported by a grant from the National R&D Program for Cancer Control, Ministry for Health, Welfare, and Family Affairs, Republic of Korea (No. 1020350).
The authors declare that they have no competing interests.
References
- 1.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 2.Jung KW, Park S, Kong HJ, Won YJ, Lee JY, Seo HG, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2009. Cancer Res Treat. 2012;44:11–24. doi: 10.4143/crt.2012.44.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Claus EB, Schildkraut JM, Thompson WD, Risch NJ. The genetic attributable risk of breast and ovarian cancer. Cancer. 1996;77:2318–2324. doi: 10.1002/(SICI)1097-0142(19960601)77:11<2318::AID-CNCR21>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 4.Stratton MR, Rahman N. The emerging landscape of breast cancer susceptibility. Nat Genet. 2008;40:17–22. doi: 10.1038/ng.2007.53. [DOI] [PubMed] [Google Scholar]
- 5.Miki Y, Swensen J, Shattuck-Eidens D, Futreal PA, Harshman K, Tavtigian S, et al. A strong candidate for the breast and ovarian cancer susceptibility gene BRCA1. Science. 1994;266:66–71. doi: 10.1126/science.7545954. [DOI] [PubMed] [Google Scholar]
- 6.Wooster R, Bignell G, Lancaster J, Swift S, Seal S, Mangion J, et al. Identification of the breast cancer susceptibility gene BRCA2. Nature. 1995;378:789–792. doi: 10.1038/378789a0. [DOI] [PubMed] [Google Scholar]
- 7.Fackenthal JD, Olopade OI. Breast cancer risk associated with BRCA1 and BRCA2 in diverse populations. Nat Rev Cancer. 2007;7:937–948. doi: 10.1038/nrc2054. [DOI] [PubMed] [Google Scholar]
- 8.Oh JH, Noh DY, Choe KJ, Kang SB, Kim LS, Ro MS, et al. Germline mutation of BRCA1 gene in Korean breast and ovarian cancer patients. J Korean Cancer Assoc. 1995;27:1061–1070. [Google Scholar]
- 9.Son BH, Ahn SH, Kim SW, Kang E, Park SK, Lee MH, et al. Prevalence of BRCA1 and BRCA2 mutations in non-familial breast cancer patients with high risks in Korea: the Korean Hereditary Breast Cancer (KOHBRA) Study. Breast Cancer Res Treat. 2012;133:1143–1152. doi: 10.1007/s10549-012-2001-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Han SA, Park SK, Ahn SH, Lee MH, Noh DY, Kim LS, et al. The Korean Hereditary Breast Cancer (KOHBRA) study: protocols and interim report. Clin Oncol (R Coll Radiol) 2011;23:434–441. doi: 10.1016/j.clon.2010.11.007. [DOI] [PubMed] [Google Scholar]
- 11.Han SA, Kim SW, Kang E, Park SK, Ahn SH, Lee MH, Nam SJ, et al. The prevalence of BRCA mutations among familial breast cancer patients in Korea: results of the Korean Hereditary Breast Cancer study. Fam Cancer. 2013;12:75–81. doi: 10.1007/s10689-012-9578-7. [DOI] [PubMed] [Google Scholar]
- 12.Genetic/familial high-risk assessment: breast and ovarian. National Comprehensive Cancer Network; [Accessed August 27th, 2012]. http://www.nccn.org. [Google Scholar]
- 13.Seong MW, Cho S, Noh DY, Han W, Kim SW, Park CM, et al. Comprehensive mutational analysis of BRCA1/BRCA2 for Korean breast cancer patients: evidence of a founder mutation. Clin Genet. 2009;76:152–160. doi: 10.1111/j.1399-0004.2009.01202.x. [DOI] [PubMed] [Google Scholar]
- 14.Kim H, Cho DY, Choi DH, Choi SY, Shin I, Park W, et al. Characteristics and spectrum of BRCA1 and BRCA2 mutations in 3,922 Korean patients with breast and ovarian cancer. Breast Cancer Res Treat. 2012;134:1315–1326. doi: 10.1007/s10549-012-2159-5. [DOI] [PubMed] [Google Scholar]
- 15.Chen S, Parmigiani G. Meta-analysis of BRCA1 and BRCA2 penetrance. J Clin Oncol. 2007;25:1329–1333. doi: 10.1200/JCO.2006.09.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Han SA, Park SK, Ahn SH, Son BH, Lee MH, Choi DH, et al. The breast and ovarian cancer risks in Korea due to inherited mutations in BRCA1 and BRCA2: a preliminary report. J Breast Cancer. 2009;12:92–99. [Google Scholar]
- 17.Stoppa-Lyonnet D, Ansquer Y, Dreyfus H, Gautier C, Gauthier-Villars M, Bourstyn E, et al. Familial invasive breast cancers: worse outcome related to BRCA1 mutations. J Clin Oncol. 2000;18:4053–4059. doi: 10.1200/JCO.2000.18.24.4053. [DOI] [PubMed] [Google Scholar]
- 18.Robson ME, Chappuis PO, Satagopan J, Wong N, Boyd J, Goffin JR, et al. A combined analysis of outcome following breast cancer: differences in survival based on BRCA1/BRCA2 mutation status and administration of adjuvant treatment. Breast Cancer Res. 2004;6:R8–R17. doi: 10.1186/bcr658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nicoletto MO, Donach M, De Nicolo A, Artioli G, Banna G, Monfardini S. BRCA-1 and BRCA-2 mutations as prognostic factors in clinical practice and genetic counselling. Cancer Treat Rev. 2001;27:295–304. doi: 10.1053/ctrv.2001.0233. [DOI] [PubMed] [Google Scholar]
- 20.El-Tamer M, Russo D, Troxel A, Bernardino LP, Mazziotta R, Estabrook A, et al. Survival and recurrence after breast cancer in BRCA1/2 mutation carriers. Ann Surg Oncol. 2004;11:157–164. doi: 10.1245/aso.2004.05.018. [DOI] [PubMed] [Google Scholar]
- 21.Rennert G, Bisland-Naggan S, Barnett-Griness O, Bar-Joseph N, Zhang S, Rennert HS, et al. Clinical outcomes of breast cancer in carriers of BRCA1 and BRCA2 mutations. N Engl J Med. 2007;357:115–123. doi: 10.1056/NEJMoa070608. [DOI] [PubMed] [Google Scholar]
- 22.Lee EH, Park SK, Park B, Kim SW, Lee MH, Ahn SH, et al. Effect of BRCA1/2 mutation on short-term and long-term breast cancer survival: a systematic review and meta-analysis. Breast Cancer Res Treat. 2010;122:11–25. doi: 10.1007/s10549-010-0859-2. [DOI] [PubMed] [Google Scholar]
- 23.Frank TS, Deffenbaugh AM, Reid JE, Hulick M, Ward BE, Lingenfelter B, et al. Clinical characteristics of individuals with germline mutations in BRCA1 and BRCA2: analysis of 10,000 individuals. J Clin Oncol. 2002;20:1480–1490. doi: 10.1200/JCO.2002.20.6.1480. [DOI] [PubMed] [Google Scholar]
- 24.Parmigiani G, Berry D, Aguilar O. Determining carrier probabilities for breast cancer-susceptibility genes BRCA1 and BRCA2. Am J Hum Genet. 1998;62:145–158. doi: 10.1086/301670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Antoniou AC, Pharoah PP, Smith P, Easton DF. The BOADICEA model of genetic susceptibility to breast and ovarian cancer. Br J Cancer. 2004;91:1580–1590. doi: 10.1038/sj.bjc.6602175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Evans DG, Lalloo F, Wallace A, Rahman N. Update on the Manchester Scoring System for BRCA1 and BRCA2 testing. J Med Genet. 2005;42:e39. doi: 10.1136/jmg.2005.031989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kurian AW, Gong GD, Chun NM, Mills MA, Staton AD, Kingham KE, et al. Performance of BRCA1/2 mutation prediction models in Asian Americans. J Clin Oncol. 2008;26:4752–4758. doi: 10.1200/JCO.2008.16.8310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kang E, Park SK, Yang JJ, Park B, Lee MH, Lee JW, et al. Accuracy of BRCA1/2 mutation prediction models in Korean breast cancer patients. Breast Cancer Res Treat. 2012;134:1189–1197. doi: 10.1007/s10549-012-2022-8. [DOI] [PubMed] [Google Scholar]
- 29.Berliner JL, Fay AM Practice Issues Subcommittee of the National Society of Genetic Counselors' Familial Cancer Risk Counseling Special Interest Group. Risk assessment and genetic counseling for hereditary breast and ovarian cancer: recommendations of the National Society of Genetic Counselors. J Genet Couns. 2007;16:241–260. doi: 10.1007/s10897-007-9090-7. [DOI] [PubMed] [Google Scholar]
- 30.Kim KS, Kim SW, Lee MH, Ahn SH, Park SK Korean Breast Cancer Society. Practice patterns of surgeons for the management of hereditary breast cancer in Korea. J Breast Cancer. 2008;11:95–101. [Google Scholar]
- 31.Kang E, Ahn SH, Noh WC, Noh DY, Jung Y, Kim LS, et al. The change of practice patterns of the hereditary breast cancer management in Korea after the Korean Hereditary Breast Cancer Study. J Breast Cancer. 2010;13:418–430. [Google Scholar]
- 32.Korean Hereditary Breast Cancer Study Group; Korean Breast Cancer Society. Hereditary Breast Cancer. Seoul: Koonja; 2012. [Google Scholar]
- 33.Korean Hereditary Breast Cancer Study Group; Korean Breast Cancer Society. Manual for Hereditary Breast Cancer Counseling. Seoul: Koonja; 2012. [Google Scholar]
- 34.Kang E, Park SK, Kim KS, Choi DH, Nam SJ, Paik NS, et al. Communication with family members about positive BRCA1/2 genetic test results in Korean hereditary breast cancer families. J Genet Med. 2011;8:105–112. [Google Scholar]
- 35.Stirling D, Evans DG, Pichert G, Shenton A, Kirk EN, Rimmer S, et al. Screening for familial ovarian cancer: failure of current protocols to detect ovarian cancer at an early stage according to the International Federation of Gynecology and Obstetrics system. J Clin Oncol. 2005;23:5588–5596. doi: 10.1200/JCO.2005.05.097. [DOI] [PubMed] [Google Scholar]
- 36.Rebbeck TR, Lynch HT, Neuhausen SL, Narod SA, Van't Veer L, Garber JE, et al. Prophylactic oophorectomy in carriers of BRCA1 or BRCA2 mutations. N Engl J Med. 2002;346:1616–1622. doi: 10.1056/NEJMoa012158. [DOI] [PubMed] [Google Scholar]
- 37.Domchek SM, Friebel TM, Singer CF, Evans DG, Lynch HT, Isaacs C, et al. Association of risk-reducing surgery in BRCA1 or BRCA2 mutation carriers with cancer risk and mortality. JAMA. 2010;304:967–975. doi: 10.1001/jama.2010.1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kim KS, Kim S, Han SA, Kang E, Jeon YT, Ha TH, et al. Contralateral prophylactic mastectomy and prophylactic salphingo-oophorectomy in a BRCA1-positive breast cancer patient: a case report. J Breast Cancer. 2008;11:218–222. [Google Scholar]
- 39.Choi MY, Lee JE, Kim SW, Lee SK, Hur SM, Kim S, et al. Incidental detection of ductal carcinoma in situ of the breast from bilateral prophylactic mastectomy of asymptomatic BRCA2 mutation carrier: a case report. J Breast Cancer. 2010;13:311–317. [Google Scholar]
- 40.Koo DH, Chung IY, Kang E, Han SA, Kim SW. Usage patterns of surveillance, chemoprevention and risk-reducing surgery in Korean BRCA mutation carriers: 5 years of experience at a single institution. J Breast Cancer. 2011;14(Suppl 1):S17–S23. [Google Scholar]
- 41.Kim D, Kang E, Hwang E, Sun Y, Hwang Y, Yom CK, et al. Factors affecting the decision to undergo risk-reducing salpingo-oophorectomy among women with BRCA gene mutation. Fam Cancer. doi: 10.1007/s10689-013-9625-z. Epub 2013 Mar 16. http://dx.doi.org/10.1007/s10689-013-9625-z. [DOI] [PubMed] [Google Scholar]
- 42.Kim HC, Lee JY, Sung H, Choi JY, Park SK, Lee KM, et al. A genome-wide association study identifies a breast cancer risk variant in ERBB4 at 2q34: results from the Seoul Breast Cancer Study. Breast Cancer Res. 2012;14:R56. doi: 10.1186/bcr3158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Long J, Cai Q, Sung H, Shi J, Zhang B, Choi JY, et al. Genome-wide association study in east Asians identifies novel susceptibility loci for breast cancer. PLoS Genet. 2012;8:e1002532. doi: 10.1371/journal.pgen.1002532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zheng W, Zhang B, Cai Q, Sung H, Michailidou K, Shi J, et al. Common genetic determinants of breast-cancer risk in East Asian women: a collaborative study of 23 637 breast cancer cases and 25 579 controls. Hum Mol Genet. 2013;22:2539–2550. doi: 10.1093/hmg/ddt089. [DOI] [PMC free article] [PubMed] [Google Scholar]