Abstract
Aims
The objective of the Aliskiren Trial on Acute Heart Failure Outcomes (ASTRONAUT) was to determine whether aliskiren, a direct renin inhibitor, would improve post-discharge outcomes in patients with hospitalization for heart failure (HHF) with reduced ejection fraction. Pre-specified subgroup analyses suggested potential heterogeneity in post-discharge outcomes with aliskiren in patients with and without baseline diabetes mellitus (DM).
Methods and results
ASTRONAUT included 953 patients without DM (aliskiren 489; placebo 464) and 662 patients with DM (aliskiren 319; placebo 343) (as reported by study investigators). Study endpoints included the first occurrence of cardiovascular death or HHF within 6 and 12 months, all-cause death within 6 and 12 months, and change from baseline in N-terminal pro-B-type natriuretic peptide (NT-proBNP) at 1, 6, and 12 months. Data regarding risk of hyperkalaemia, renal impairment, and hypotension, and changes in additional serum biomarkers were collected. The effect of aliskiren on cardiovascular death or HHF within 6 months (primary endpoint) did not significantly differ by baseline DM status (P = 0.08 for interaction), but reached statistical significance at 12 months (non-DM: HR: 0.80, 95% CI: 0.64–0.99; DM: HR: 1.16, 95% CI: 0.91–1.47; P = 0.03 for interaction). Risk of 12-month all-cause death with aliskiren significantly differed by the presence of baseline DM (non-DM: HR: 0.69, 95% CI: 0.50–0.94; DM: HR: 1.64, 95% CI: 1.15–2.33; P < 0.01 for interaction). Among non-diabetics, aliskiren significantly reduced NT-proBNP through 6 months and plasma troponin I and aldosterone through 12 months, as compared to placebo. Among diabetic patients, aliskiren reduced plasma troponin I and aldosterone relative to placebo through 1 month only. There was a trend towards differing risk of post-baseline potassium ≥6 mmol/L with aliskiren by underlying DM status (non-DM: HR: 1.17, 95% CI: 0.71–1.93; DM: HR: 2.39, 95% CI: 1.30–4.42; P = 0.07 for interaction).
Conclusion
This pre-specified subgroup analysis from the ASTRONAUT trial generates the hypothesis that the addition of aliskiren to standard HHF therapy in non-diabetic patients is generally well-tolerated and improves post-discharge outcomes and biomarker profiles. In contrast, diabetic patients receiving aliskiren appear to have worse post-discharge outcomes. Future prospective investigations are needed to confirm potential benefits of renin inhibition in a large cohort of HHF patients without DM.
Keywords: Aliskiren, Diabetes, Outcomes, Post-discharge
See page 3097 for the editorial comment on this article (doi:10.1093/eurheartj/eht366)
Introduction
There are over 1 million primary hospitalizations for heart failure (HHF) annually in the USA alone,1 and this population continues to experience poor post-discharge outcomes despite available therapies.2 The heterogeneity of clinical profiles among these patients is well established and the majority have a history of cardiovascular (CV) and non-CV comorbidities.2,3 Approximately 40% of HHF patients have a history of diabetes mellitus (DM) and observational and clinical trial data have explored the associated prognostic implications.4,5
Recently, the Aliskiren Trial on Acute Heart Failure Outcomes (ASTRONAUT) confirmed the high prevalence of DM among HHF patients with reduced left ventricular ejection fraction (LVEF).6 In this study, the addition of aliskiren to standard therapy had no significant effect on CV death or heart failure (HF) rehospitalization within 6 or 12 months. Although the overall study results were neutral, pre-specified subgroup analysis found the effect of the study drug on all-cause death within 12 months to differ by the presence of comorbid DM, with aliskiren associated with a higher risk of death in diabetics and lower risk of death in non-diabetics. These data were consistent with previous reports of poor outcomes with aliskiren in diabetics already taking renin–angiotensin–aldosterone system (RAAS) inhibitors.7 The ASTRONAUT trial affords the opportunity to perform an in-depth characterization of patients with HHF by the presence or absence of DM to better understand this possible bidirectional effect of aliskiren on outcomes. Given the potentially improved survival with aliskiren among nearly 60% of ASTRONAUT patients without diabetes and the current lack of therapies proven to improve outcomes in HHF, these data deserve further analysis.
Methods
Study design
The study design8 and primary results of the ASTRONAUT trial have been previously described.6 Briefly, the ASTRONAUT trial was a prospective, multicentre, multinational, randomized, double-blind, placebo-controlled trial investigating the role of oral aliskiren, a direct renin inhibitor, on outcomes among HHF patients. Patients were randomized a median 5 days after hospital admission to 150 mg daily (increased to 300 mg daily as tolerated) of aliskiren or placebo, in addition to standard therapy. All patients were 18 years of age or older with LVEF ≤ 40%, elevated natriuretic peptides [B-type natriuretic peptide (BNP) ≥400 pg/mL or N-terminal pro-B-type natriuretic peptide (NT-proBNP) ≥1600 pg/mL], and signs and symptoms of fluid overload that necessitated hospitalization. Before randomization, patients were required to be haemodynamically stable, defined as systolic blood pressure ≥110 mmHg for at least 6 h and no use of intravenous vasodilators (except nitrates) or intravenous inotropes from time of hospital presentation to randomization. Exclusion criteria included estimated glomerular filtration rate (eGFR) <40 mL/min/1.73 m2, serum potassium level >5.0 mEq/L, hyponatraemia <130 mEq/L, recent myocardial infarction (MI), cardiac surgery or stroke, and comorbid conditions with expected survival <3 years. Local institutional review boards or ethics committees at each centre approved the study protocol and patients provided written informed consent for participation. Efficacy analysis by patient history of DM (as determined by the investigator) was a protocol pre-specified subgroup analysis prospectively planned prior to database lock and included all patients from both treatment arms used for efficacy analysis. Safety analysis by baseline DM status was performed post hoc.
The primary endpoint in ASTRONAUT was the first occurrence of CV death or HF rehospitalization within 6 months after randomization. Secondary endpoints included CV death or HF rehospitalization within 12 months (key secondary endpoint), first CV event (defined as CV death, HF rehospitalization, non-fatal MI, non-fatal stoke, and resuscitated sudden death) within 12 months, all-cause death within 6 and 12 months, and change from baseline in NT-proBNP level at 1, 6, and 12 months. Additional data regarding biomarker levels (plasma renin activity, plasma troponin I, plasma aldosterone) were also collected and analysed. An independent, clinical events committee adjudicated specific causes of death and hospitalization (Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA).
Statistical analysis
Categorical variables are reported as number (percentage), while continuous variables are expressed as means ± standard deviation if normally distributed or as median (inter-quartile range) if not normally distributed.
The time-to-event data were assumed to follow a proportional hazard model and hazard ratios (HR) and corresponding 95% confidence intervals (CI) are provided. The assumption of proportional hazards was verified using a Cox proportional hazards regression model which included treatment and a time-dependent explanatory variable created through the interaction between log time and treatment. The estimate of the interaction term was presented in terms of the change in effect from 1 month to the next. In addition, a plot of the log–log survivor function vs. log time for each treatment group was performed. Approximate parallelism between the curves for treatment groups provided supportive evidence of the proportional hazards assumption. Analyses were performed for the primary endpoint and the selected secondary endpoints (CV death or HF rehospitalization within 12 months, all-cause death within 6 and 12 months, first CV event within 12 months). Testing for interaction between all endpoints and baseline DM status was performed. Cumulative event rate estimates (1 – estimated survival function, described in %) vs. time of follow-up (in years) were calculated based on the Kaplan–Meier estimates.
Biomarker data were analysed for diabetic and non-diabetic groups, and changes in NT-proBNP (pg/mL), plasma renin activity (ng/mL/h), plasma troponin I (ng/mL), and plasma aldosterone (pmol/L) were calculated using log-transformation and summarized in a geometric mean with 95% CI on a geometric mean. In addition, a repeated measurement model was performed on change from baseline log-transformed for biomarker variables. All the results were back-transformed to provide the geometric least squares means (presented as a ratio to baseline), the ratio for aliskiren vs. placebo, and the 95% CI around the ratio for each time point (1, 6, and 12 months).
Adverse events of special interest including hyperkalaemia, renal impairment or renal failure, and hypotension and corresponding rates of treatment discontinuation for these events were calculated. Additionally, incidence of post-baseline potassium ≥6 mmol/L and eGFR <30 mL/min/1.73 m2 were summarized by treatment group. Relative risk and corresponding 95% CI were used in treatment comparison, and interaction analysis was performed by baseline DM status.
The cohort used for efficacy analysis was from the full-analysis set, defined as all randomized patients who received at least 1 dose of the study drug. Following the intent-to-treat principle, patients were analysed according to the treatment assigned at randomization. Safety was analysed in all patients who received study drug and had at least one post-baseline safety assessment. All statistical analyses were performed using SAS version 9.2 (SAS Institute), and two-sided P < 0.05 was considered to be statistically significant.
Results
Baseline characteristics
The current study included 1615 patients from the final ASTRONAUT efficacy analysis cohort, of which 953 patients were without a documented history of DM (59%). The median follow-up in the overall population was 11.3 months (inter-quartile range 9.1–12.4 months). Table 1 describes the baseline demographic, clinical, and laboratory profile for all patients in this analysis by underlying DM history and treatment group. Baseline characteristics by treatment arm did not significantly differ by DM status with the following exceptions: age, ischaemic HF aetiology, systolic blood pressure, eGFR, serum sodium, and angiotensin II receptor blocker (ARB) use. Among patients with DM, 42% were receiving insulin therapy and 53% were receiving oral antihyperglycemic agents.
Table 1.
Baseline characteristics of non-diabetic and diabetic patients
| Non-diabetics |
Diabetics |
|||
|---|---|---|---|---|
| Characteristic | Aliskiren (n = 489) | Placebo (n = 464) | Aliskiren (n = 319) | Placebo (n = 343) |
| Age (years), mean (SD) | 64.1 (13.3) | 63.4 (13.0) | 65.6 (11.0) | 66.0 (10.1) |
| Male, n (%) | 394 (80.6) | 345 (74.4) | 243 (76.2) | 265 (77.3) |
| Race, n (%) | ||||
| Caucasian | 342 (69.9) | 325 (70.0) | 232 (72.7) | 241 (70.3) |
| Black | 22 (4.5) | 24 (5.2) | 14 (4.4) | 18 (5.2) |
| Asian | 101 (20.7) | 94 (20.3) | 66 (20.7) | 75 (21.9) |
| Other | 24 (4.9) | 21 (4.5) | 7 (2.2) | 9 (2.6) |
| NYHA class at Visit 1, n (%) | ||||
| III | 304 (62.2) | 281 (60.6) | 194 (60.8) | 204 (59.5) |
| IV | 185 (37.8) | 183 (39.4) | 125 (39.2) | 139 (40.5) |
| NYHA class at Visit 2, n (%) | ||||
| I | 14 (2.9) | 9 (1.9) | 3 (0.9) | 8 (2.3) |
| II | 166 (33.9) | 152 (32.8) | 101 (31.7) | 94 (27.4) |
| III | 268 (54.8) | 258 (55.6) | 173 (54.2) | 204 (59.5) |
| IV | 35 (7.2) | 38 (8.2) | 33 (10.3) | 33 (9.6) |
| Ischaemic heart failure aetiology, n (%) | 287 (58.7) | 248 (53.4) | 233 (73.0) | 259 (75.5) |
| Prior heart failure hospitalization, n (%) | 309 (63.2) | 313 (67.5) | 230 (72.1) | 232 (67.6) |
| Ejection fraction (%), mean (SD) | 28 (7.3) | 27 (7.5) | 28 (7.3) | 28 (6.9) |
| Systolic blood pressure (mmHg), mean (SD) | 123 (12.8) | 123 (12.2) | 125 (14.2) | 124 (13.8) |
| Heart rate (b.p.m.), mean (SD) | 77 (16.0) | 78 (16.5) | 79 (16.0) | 78 (15.3) |
| eGFR (mL/min/1.73 m2), mean (SD), Visit 2 | 68.5 (20.4) | 67.0 (19.9) | 65.5 (19.1) | 64.9 (20.0) |
| eGFR (mL/min/1.73 m2) group, n (%), Visit 2 | ||||
| <60 | 181 (37.0) | 169 (36.4) | 137 (42.9) | 146 (42.6) |
| ≥60 | 291 (59.5) | 275 (59.3) | 166 (52.0) | 183 (53.4) |
| NT-proBNP (pg/mL), median (IQR), Visit 1 | 4471 (2840–8540) | 4472 (2715–8924) | 4015 (2615–6679) | 3738 (2682–7461) |
| NT-proBNP (pg/mL), median (IQR), Visit 2 | 2851 (1510–5344) | 2651 (1555–5257) | 2736 (1523–5097) | 2699 (1536–5074) |
| BNP (pg/mL), mean (IQR), Visit 1 | 936 (592–1650) | 842 (533–1570) | 908 (541–1567) | 866 (558–1655) |
| BNP (pg/mL), mean (IQR), Visit 2 | 466 (239–900) | 437 (220–910) | 480 (238–920) | 390 (206–773) |
| Sodium (mmol/L), mean (SD) | 139 (3.7) | 139 (3.8) | 139 (3.3) | 138 (3.8) |
| Potassium (mmol/L), mean (SD) | 4.3 (0.8) | 4.3 (0.7) | 4.3 (0.5) | 4.3 (0.6) |
| Troponin I (ng/mL), median (IQR) | 0.0 (0.0–0.1) | 0.0 (0.0–0.1) | 0.0 (0.0–0.1) | 0.0 (0.0–0.1) |
| Atrial fibrillation on ECG, n (%), Visit 2 | 154 (31.5) | 148 (31.9) | 88 (27.6) | 96 (28.0) |
| Medical history, n (%) | ||||
| Hypertension | 353 (72.2) | 330 (71.1) | 259 (81.2) | 283 (82.5) |
| Coronary artery disease | 240 (49.1) | 203 (43.8) | 203 (63.6) | 235 (68.5) |
| Renal insufficiency | 67 (13.3) | 79 (17.0) | 93 (29.2) | 93 (27.1) |
| Chronic obstructive pulmonary disease | 97 (19.8) | 78 (16.8) | 71 (22.3) | 76 (22.2) |
| Background therapies, n (%) | ||||
| Diuretic (not including mineralocorticoid receptor antagonist) | 469 (95.9) | 445 (95.9) | 306 (95.9) | 328 (95.6) |
| Angiotensin-converting enzyme inhibitors | 324 (66.3) | 318 (68.5) | 203 (63.6) | 211 (61.5) |
| Angiotensin II receptor blockers | 87 (17.8) | 65 (14.0) | 72 (22.6) | 80 (23.3) |
| Beta-blockers | 385 (78.7) | 391 (84.3) | 275 (86.2) | 282 (82.2) |
| Mineralocorticoid receptor antagonist | 276 (56.4) | 281 (60.6) | 172 (53.9) | 192 (56.0) |
BNP, B-type natriuretic peptide; b.p.m., beat per minute; ECG, electrocardiogram; eGFR, estimated glomerular filtration rate; IQR, inter-quartile range; NT-proBNP, N-terminal pro-B-type natriuretic peptide; NYHA, New York Heart Association; SD, standard deviation.
Data pertain to Visit 2 unless otherwise specified. Visit 1 refers to time point when the diagnosis of worsening chronic heart failure and study eligibility were confirmed. Visit 2 refers to time point when stabilized patients were randomized to aliskiren or placebo, in addition to standard therapy.
Study endpoints
Outcome analyses for non-diabetic and diabetic patients are displayed in Table 2. Overall, the influence of aliskiren on the primary endpoint of CV death or HF rehospitalization within 6 months did not significantly differ by DM status (P = 0.08 for interaction). The effect of aliskiren on 12-month CV death or HF rehospitalization (P = 0.03 for interaction), first CV event within 12 months (P = 0.02 for interaction) and 12-month all-cause death (P < 0.01 for interaction) significantly differed according to baseline history of DM. There was a borderline significant interaction between treatment arm and diabetes status for all-cause death within 6 months (P = 0.05 for interaction).
Table 2.
Study endpoints by baseline diabetes status
| Endpoint | Aliskiren, n (%) Non-DM (n = 489) DM (n = 319) | Placebo, n (%) Non-DM (n = 464) DM (n = 343) | Hazard ratio (95% CI) | P for interaction (two-sided) |
|---|---|---|---|---|
| Primary endpoint (6 months) | ||||
| CV death or HF rehospitalization | ||||
| Non-DM | 102 (20.9) | 114 (24.6) | 0.80 (0.61–1.04) | |
| DM | 99 (31.0) | 100 (29.2) | 1.13 (0.86–1.50) | 0.08 |
| Secondary endpoints (12 months, unless otherwise specified) | ||||
| CV death or HF rehospitalization | ||||
| Non-DM | 148 (30.3) | 165 (35.6) | 0.80 (0.64–0.99) | |
| DM | 135 (42.3) | 136 (39.7) | 1.16 (0.91–1.47) | 0.03 |
| First CV event | ||||
| Non-DM | 154 (31.5) | 177 (38.1) | 0.75 (0.61–0.94) | |
| DM | 139 (43.6) | 144 (42.0) | 1.11 (0.88–1.40) | 0.02 |
| All-cause death (6 months) | ||||
| Non-DM | 43 (8.8) | 51 (11.0) | 0.75 (0.50–1.13) | |
| DM | 42 (13.2) | 38 (11.1) | 1.38 (0.88–2.15) | 0.05 |
| All-cause death | ||||
| Non-DM | 72 (14.7) | 91 (19.6) | 0.69 (0.50–0.94) | |
| DM | 72 (22.6) | 57 (16.6) | 1.64 (1.15–2.33) | <0.01 |
CI, confidence interval; CV, cardiovascular; DM, diabetes mellitus; HF, heart failure.
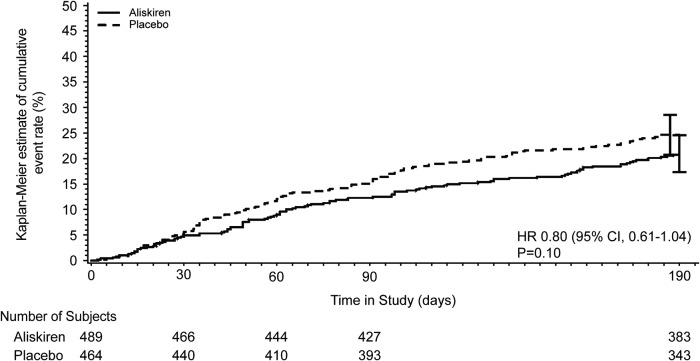
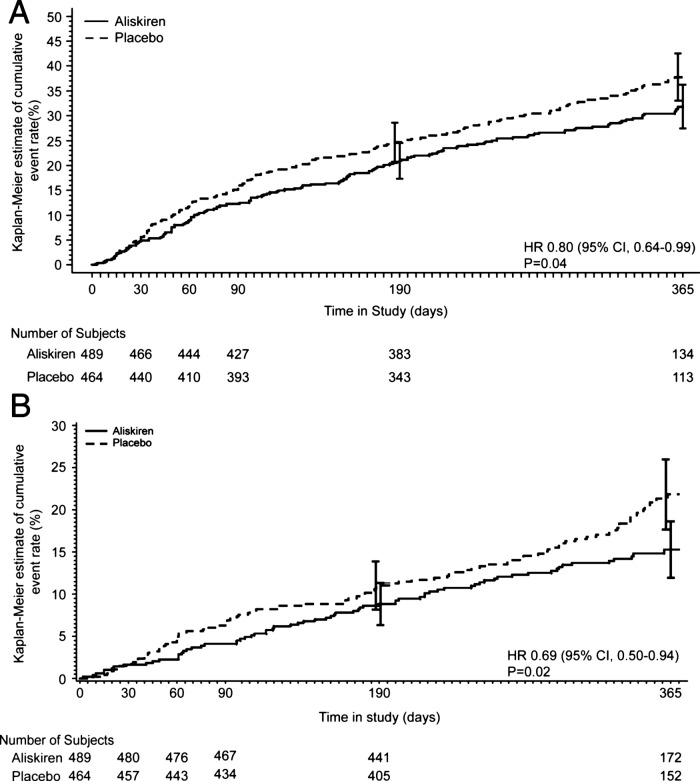
Among non-diabetics, 102 patients in the aliskiren group (20.9%) and 114 patients in the placebo group (24.6%) experienced the primary endpoint (HR: 0.80; 95% CI: 0.61–1.04) (Figure 1). In regard to 12-month secondary endpoints, non-diabetics receiving aliskiren were significantly less likely to experience CV death or HF hospitalization (HR: 0.80; 95% CI: 0.64–0.99), first CV event (HR: 0.75; 95% CI: 0.61–0.94) and all-cause death (HR: 0.69; 95% CI: 0.50–0.94) when compared with placebo (Figure 2).
Figure 1.
Kaplan–Meier analysis of the cumulative event rate of cardiovascular death or heart failure hospitalization within 6 months in patients without diabetes mellitus.
Figure 2.
Kaplan–Meier analysis of the cumulative event rate of cardiovascular death or heart failure hospitalization (A) and all-cause death (B) within 12 months in patients without baseline diabetes mellitus.
Similar to the non-diabetic group, there was no significant difference in the rate of the primary endpoint between treatment groups among patients with DM (HR: 1.13; 95% CI: 0.86–1.50). However, diabetics receiving aliskiren were significantly more likely to die within 12 months (HR: 1.64; 95% CI: 1.15–2.33).
Adjudicated causes of death
Table 3 presents descriptive data on adjudicated causes of death by treatment arm and DM status for all the patients included in efficacy analysis plus three additional placebo patients (one patient missing informed consent, two patients with associated Good Clinical Practice violations). During the double-blind period, the rates of CV death among non-diabetics receiving aliskiren and placebo were 13.7 and 18.9%, respectively. Major contributors to reduced CV death with aliskiren were decreased rates of pump failure (aliskiren 4.7%; placebo 7.1%) and presumed CV death (aliskiren 0.8%; placebo 2.2%). In contrast, among diabetic patients, aliskiren was associated with a higher rate of CV death (aliskiren 21.0%; placebo 16.2%), pump failure (aliskiren 9.7%; placebo 6.7%) and sudden death (aliskiren 5.6%; placebo 4.3%). Rates of non-CV death in ASTRONAUT were low in both non-diabetic and diabetic patients.
Table 3.
Adjudicated causes of death among non-diabetic and diabetic patients
| Non-diabetics |
Diabetics |
|||
|---|---|---|---|---|
| Adjudicated cause of death, n (%) | Aliskiren (n = 489) | Placebo (n = 465) | Aliskiren (n = 319) | Placebo (n = 345) |
| CV death | 67 (13.7) | 88 (18.9) | 67 (21.0) | 56 (16.2) |
| Fatal myocardial infarction | 3 (0.6) | 6 (1.3) | 1 (0.3) | 6 (1.7) |
| Pump failure | 23 (4.7) | 33 (7.1) | 31 (9.7) | 23 (6.7) |
| Sudden death | 28 (5.7) | 30 (6.5) | 18 (5.6) | 15 (4.3) |
| Presumed sudden death | 3 (0.6) | 1 (0.2) | 4 (1.3) | 2 (0.6) |
| Presumed CV death | 4 (0.8) | 10 (2.2) | 7 (2.2) | 4 (1.2) |
| Other CV death | 0 | 0 | 0 | 2 (0.6) |
| Fatal stroke | 3 (0.6) | 5 (1.1) | 3 (0.9) | 2 (0.6) |
| CV procedural | 1 (0.2) | 0 | 0 | 1 (0.3) |
| Unknown | 2 (0.4) | 3 (0.7) | 3 (0.9) | 1 (0.3) |
| Non-CV death | 8 (1.6) | 5 (1.1) | 10 (3.1) | 4 (1.2) |
| Accidental | 1 (0.2) | 0 | 3 (0.9) | 0 |
| Pulmonary | 0 | 0 | 1 (0.3) | 0 |
| Infection | 3 (0.6) | 1 (0.2) | 6 (1.9) | 2 (0.6) |
| Malignancy | 2 (0.4) | 1 (0.2) | 0 | 0 |
| Gastrointestinal | 1 (0.2) | 3 (0.7) | 0 | 2 (0.6) |
| Renal | 0 | 0 | 0 | 0 |
| Other non-CV death | 1 (0.2) | 0 | 0 | 0 |
CV, cardiovascular.
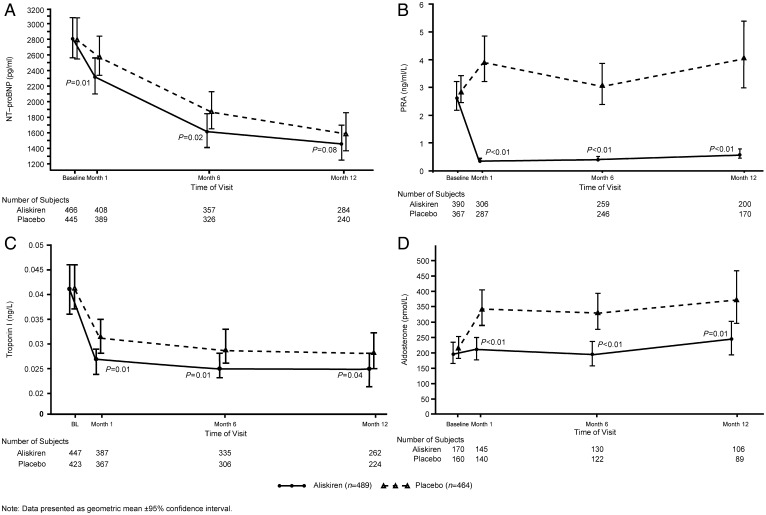
Effect on biomarkers
The effects of aliskiren on CV biomarkers in patients with and without baseline DM are displayed in Table 4. Among non-diabetics, aliskiren was associated with a statistically significant greater decrease in NT-proBNP level compared with placebo at 1 and 6 months post-randomization (P ≤ 0.02), but not 12 months (P = 0.08) (Figure 3). Plasma renin activity was significantly reduced with aliskiren at each time point tested (all P < 0.01). Similarly, aliskiren reduced plasma aldosterone and plasma troponin I levels across all time points, relative to placebo (all P ≤ 0.04).
Table 4.
Change from baseline in biomarkers among diabetic and non-diabetic patients
| Non-diabetic patients |
Diabetic patients |
||||||
|---|---|---|---|---|---|---|---|
| Time point | Treatment | n | Ratio: endpoint/ baseline; adjusted geometric mean (95% CI) | Ratio: aliskiren/placebo (95% CI) | n | Ratio: endpoint/baseline; adjusted geometric mean (95% CI) | Ratio: aliskiren/placebo (95% CI) |
| NT-proBNP (pg/mL) | |||||||
| Month 1 | Aliskiren | 405 | 0.82 (0.76, 0.89) | 264 | 0.92 (0.85–0.99) | ||
| Placebo | 388 | 0.93 (0.86, 1.01) | 0.88 (0.80, 0.97) | 287 | 0.98 (0.91–1.06) | 0.94 (0.85–1.03) | |
| Month 6 | Aliskiren | 354 | 0.61 (0.55, 0.68) | 215 | 0.70 (0.62–0.78) | ||
| Placebo | 324 | 0.74 (0.66, 0.83) | 0.83 (0.71, 0.97) | 232 | 0.79 (0.71–0.88) | 0.88 (0.76–1.03) | |
| Month 12 | Aliskiren | 281 | 0.58 (0.51, 0.66) | 166 | 0.70 (0.60–0.81) | ||
| Placebo | 237 | 0.68 (0.60, 0.78) | 0.85 (0.71, 1.02) | 188 | 0.83 (0.72–0.96) | 0.84 (0.68–1.03) | |
| Plasma renin activity (ng/mL/h) | |||||||
| Month 1 | Aliskiren | 306 | 0.15 (0.12–0.18) | 216 | 0.17 (0.13–0.21) | ||
| Placebo | 287 | 1.54 (1.28–1.85) | 0.10 (0.08–0.12) | 220 | 1.20 (0.95–1.50) | 0.14 (0.10–0.19) | |
| Month 6 | Aliskiren | 259 | 0.16 (0.13–0.20) | 168 | 0.20 (0.15–0.25) | ||
| Placebo | 246 | 1.27 (1.03–1.56) | 0.13 (0.10–0.17) | 177 | 1.17 (0.92–1.49) | 0.17 (0.12–0.23) | |
| Month 12 | Aliskiren | 200 | 0.23 (0.19–0.30) | 124 | 0.22 (0.17–0.29) | ||
| Placebo | 170 | 1.40 (1.10–1.80) | 0.17 (0.12–0.23) | 133 | 1.16 (0.89–1.52) | 0.19 (0.13–0.27) | |
| Plasma troponin I (ng/mL) | |||||||
| Month 1 | Aliskiren | 387 | 0.66 (0.61–0.72) | 253 | 0.75 (0.67–0.84) | ||
| Placebo | 367 | 0.77 (0.70–0.84) | 0.86 (0.77–0.97) | 262 | 0.90 (0.80–1.00) | 0.84 (0.72–0.97) | |
| Month 6 | Aliskiren | 335 | 0.64 (0.58–0.71) | 208 | 0.67 (0.60–0.76) | ||
| Placebo | 306 | 0.76 (0.68–0.84) | 0.84 (0.73–0.96) | 209 | 0.75 (0.67–0.84) | 0.90 (0.77–1.05) | |
| Month 12 | Aliskiren | 262 | 0.65 (0.58–0.73) | 158 | 0.69 (0.60–0.79) | ||
| Placebo | 224 | 0.77 (0.68–0.87) | 0.85 (0.73–0.99) | 174 | 0.81 (0.71–0.92) | 0.85 (0.71–1.02) | |
| Plasma aldosterone (pmol/L) | |||||||
| Month 1 | Aliskiren | 145 | 1.08 (0.93–1.26) | 122 | 1.13 (0.96–1.34) | ||
| Placebo | 140 | 1.69 (1.44–1.98) | 0.64 (0.52–0.78) | 118 | 1.49 (1.25–1.77) | 0.76 (0.61–0.95) | |
| Month 6 | Aliskiren | 130 | 1.00 (0.84–1.19) | 98 | 1.53 (1.28–1.82) | ||
| Placebo | 122 | 1.64 (1.37–1.97) | 0.61 (0.48–0.76) | 91 | 1.53 (1.28–1.83) | 1.00 (0.79–1.25) | |
| Month 12 | Aliskiren | 106 | 1.28 (1.05–1.57) | 72 | 1.38 (1.12–1.71) | ||
| Placebo | 89 | 1.85 (1.49–2.29) | 0.69 (0.52–0.92) | 76 | 1.64 (1.32–2.03) | 0.84 (0.64–1.12) | |
CI, confidence interval; NT-proBNP, N-terminal pro-B-type natriuretic peptide.
Figure 3.
Measures of serum biomarkers (mean ± 95% confidence interval) at baseline and 1, 6, and 12 months post-randomization for non-diabetic patients receiving aliskiren and placebo. P values represent comparison between treatment arms of the change from baseline for a given biomarker. The figure reflects all available data for each biomarker at each time point. For NT-proBNP, note that the number of subjects for each time point differs slightly from the number of subjects reported in the repeated measure analysis displayed in Table 4. NT-proBNP, N-terminal pro-B-type natriuretic peptide; PRA, plasma renin activity.
By comparison, among diabetics, aliskiren was not associated with a decrease in NT-proBNP compared with placebo at any time point tested (all P ≥ 0.10). Aliskiren significantly reduced plasma aldosterone at 1 month relative to placebo (P = 0.01), but not at 6 or 12 months (P ≥ 0.23). Likewise, diabetics treated with aliskiren had significant decreases in troponin I at 1 month compared to placebo (P = 0.02), but not at other time points (P ≥ 0.08). Similar to patients without DM, diabetics had significant reductions in plasma renin activity at each time point tested relative to placebo (all P < 0.01).
Safety
Table 5 displays data for adverse events of special interest among non-diabetic and diabetic patients. There was a trend towards differing risk of post-baseline potassium level ≥6 mmol/L with aliskiren by underlying DM status (non-DM: HR: 1.17, 95% CI: 0.71–1.93; DM: HR: 2.39, 95% CI: 1.30–4.42; P = 0.07 for interaction). No other notable interactions were seen (all P ≥ 0.32 for interaction).
Table 5.
Adverse events of special interest by treatment group among non-diabetics and diabetics (safety set)
| Aliskiren, n (%) Non-DM (n = 489) DM (n = 319) | Placebo, n (%) Non-DM (n = 465) DM (n = 345) | Aliskiren vs. Placebo relative risk (95% CI) | P for interaction (two-sided) | |
|---|---|---|---|---|
| Adverse event of special interest | ||||
| Hyperkalaemiaa | ||||
| Non-DM | 96 (19.6) | 74 (15.9) | 1.23 (0.94–1.62) | |
| DM | 73 (22.9) | 68 (19.7) | 1.16 (0.87–1.56) | 0.80 |
| Renal impairment or renal failureb | ||||
| Non-DM | 75 (15.3) | 48 (10.3) | 1.49 (1.06–2.09) | |
| DM | 59 (18.5) | 50 (14.5) | 1.28 (0.90–1.80) | 0.57 |
| Hypotensionc | ||||
| Non-DM | 88 (18.0) | 56 (12.0) | 1.49 (1.10–2.04) | |
| DM | 50 (15.7) | 46 (13.3) | 1.18 (0.81–1.70) | 0.33 |
| Rate of treatment discontinuation due to adverse events | ||||
| Hyperkalaemiaa | ||||
| Non-DM | 16 (3.3) | 10 (2.2) | 1.52 (0.70–3.32) | |
| DM | 20 (6.3) | 13 (3.8) | 1.66 (0.84–3.29) | 0.85 |
| Renal impairment or renal failureb | ||||
| Non-DM | 19 (3.9) | 9 (1.9) | 2.01 (0.92–4.39) | |
| DM | 13 (4.1) | 12 (3.5) | 1.17 (0.54–2.53) | 0.34 |
| Hypotensionc | ||||
| Non-DM | 18 (3.7) | 9 (1.9) | 1.90 (0.86–4.19) | |
| DM | 11 (3.5) | 10 (2.9) | 1.19 (0.51–2.76) | 0.43 |
| Maximum or minimum post-baseline values | ||||
| Potassium ≥6 (mmol/L) | ||||
| Non-DM | 32 (6.5) | 26 (5.6) | 1.17 (0.71–1.93) | |
| DM | 31 (9.7) | 14 (4.1) | 2.39 (1.30–4.42) | 0.07 |
| eGFR <30 (mL/min/1.73 m2) | ||||
| Non-DM | 46 (9.4) | 42 (9.0) | 1.04 (0.70–1.55) | |
| DM | 38 (11.9) | 29 (8.4) | 1.42 (0.90–2.24) | 0.32 |
aHyperkalaemia and increased blood potassium level.
bAbnormal renal function test, acute renal failure, decreased urine output, increased blood creatinine, acute pre-renal failure, renal impairment, renal failure, decreased glomerular filtration rate, and increased blood urea.
cDecreased blood pressure, postural dizziness, hypotension, orthostatic hypotension, and procedural hypotension.
CI, confidence interval; DM, diabetes mellitus; eGFR, estimated glomerular filtration rate.
Among non-diabetics, aliskiren was associated with significantly higher rates of investigator-reported renal impairment and hypotension, but there was no significant difference in rates of treatment discontinuation due to these adverse effects. When objective cutoffs were used to evaluate post-baseline risk of severe hyperkalaemia (potassium ≥6 mmol/L) or severe renal impairment (eGFR <30 mL/min/1.73 m2), no significant differences between aliskiren and placebo were seen.
In contrast to non-diabetics, patients with DM who received aliskiren did not demonstrate a higher risk of investigator reported hyperkalaemia, renal impairment, or hypotension, nor did they have an increased risk of study drug discontinuation for these effects. However, using objective measures, diabetic patients were at significantly increased risk of post-baseline severe hyperkalaemia, but not severe renal impairment.
Discussion
In the ASTRONAUT trial, nearly 60% of patients had no history of DM. At baseline, >80% of patients were receiving an angiotensin-converting enzyme (ACE) inhibitor/ARB and >50% were receiving a mineralocorticoid receptor antagonist (MRA). The effect of aliskiren on the primary endpoint of CV death or HF rehospitalization within 6 months did not significantly differ by baseline DM status. However, analysis of 12-month CV death or HF rehospitalization and all-cause death revealed statistically significant interactions by baseline DM status with non-diabetic patients tending to experience favourable outcomes. Among non-diabetics, aliskiren significantly reduced NT-proBNP through 6 months and plasma renin activity, troponin I and aldosterone through 12 months, as compared to placebo. There was a trend towards interaction favouring less risk of post-baseline potassium ≥6 mmol/L with aliskiren in non-diabetics as compared to diabetics.
While the above findings regarding HHF patients without DM may be considered encouraging, they must be viewed in the context of a subgroup analysis and the corresponding statistical limitations, including a smaller number of patients per treatment group and issues with multiplicity.9 However, this efficacy analysis was protocol pre-specified. Furthermore, although the ASTRONAUT protocol planned for the analysis of >26 subgroups of interest, stratifying patients by underlying DM status was the only analysis to demonstrate a statistically significant interaction of P < 0.05, albeit for secondary, not primary, endpoints. While the number of pre-specified subgroups tested supports the possibility of one or two groups reaching statistical significance by chance alone, the diabetes findings in ASTRONAUT are consistent with previous prospective data with aliskiren,7 thus making coincidence less likely.
Our data extend the current body of knowledge in multiple ways and serve to generate hypotheses regarding an underlying mechanism for a potential differential impact of aliskiren on outcomes by DM status. One potential explanation relates to differences in safety profile. Our results suggest that in non-diabetic patients, there was a discrepancy between the subjective and objective risk of the three adverse events of special interest. Although investigators were more likely to report renal impairment and hypotension in patients receiving aliskiren, they were no more likely to discontinue the drug due to these effects, perhaps suggesting they were not severe. Moreover, rates of post-baseline severe hyperkalaemia and renal impairment, as assessed by objective laboratory cutoffs, were no different between treatment arms. These findings contrast with those of the diabetic cohort where incidence of subjective, investigator reported adverse events of special interest and corresponding rates of drug discontinuation did not differ by treatment, yet a greater risk of post-baseline potassium ≥6 mmol/L was seen with aliskiren with a trend towards interaction by DM status. Existing data in diabetics suggest that hyperkalaemia, hypotension, and worsening eGFR with RAAS blockade predict poor prognosis.10,11 In ASTRONAUT, it is possible that an increased incidence of hyperkalaemia in diabetics receiving aliskiren, in addition to standard therapy including an ACE inhibitor/ARB, beta-blocker and MRA, contributed to poor outcomes by overshadowing any positive effects of the drug. Likewise, lack of severe hyperkalaemia in non-diabetics may have allowed favourable effects of the drug to predominate.
A second possible mechanism for improved outcomes with aliskiren in non-diabetics is the corresponding biomarker profile. Most notably, among non-diabetics, aliskiren significantly reduced NT-proBNP and plasma aldosterone levels compared with placebo through 6 months. This effect on plasma aldosterone was sustained and significant at 12 months. In diabetic patients, relative to placebo, aldosterone was only significantly reduced at 1 month and NT-proBNP was not significantly reduced at any follow-up time point. Given that NT-proBNP levels were significantly decreased over 12 months in the overall ASTRONAUT cohort without improvements in patient outcomes, it is unlikely that the effect of aliskiren on natriuretic peptides alone is responsible for the potential bidirectional effect of aliskiren by DM status.6 Rather, it is noteworthy that although absolute levels of plasma aldosterone tended to rise over time in all patients, this rise was blunted in non-diabetic patients receiving aliskiren. This significant sustained ability of aliskiren to attenuate increases in aldosterone, the final downstream neurohormone in the RAAS, may have contributed to the lower event rates in non-diabetics receiving the drug.12 This hypothesis is consistent with the established chronic HF paradigm that incremental increases in RAAS blockade with ACE inhibitors, ARB, and MRA improve patient outcomes.13–16 In patients without DM, simultaneous use of aliskiren with other established RAAS therapies may maximize RAAS suppression and produce further clinical benefits.
In aggregate, the results of the Aliskiren Trial in Type 2 Diabetes Using Cardiorenal Disease Endpoints (ALTITUDE) and ASTRONAUT do not support a role for aliskiren in HHF patients already receiving an ACE inhibitor or ARB, particularly in those with comorbid DM. However, the potential benefits of aliskiren in non-diabetics should not be overlooked. Although outcomes in chronic ambulatory HF have improved in recent decades, treatment and outcomes for patients admitted to the hospital for HF remain largely unchanged despite guideline recommended therapy.17–19 Hospital admission for HF portends a poor prognosis and ASTRONAUT confirmed an unacceptably high post-discharge event rate among clinically and haemodynamically stable hospitalized patients.6,20 Novel therapeutics are urgently needed and our data generate the hypothesis that aliskiren is safe, effective, and associated with a favourable neurohormonal profile in non-diabetic patients. Further insights may come from the ongoing long-term Aliskiren Trial on Minimizing Outcomes in Patients with Heart Failure (ATMOSPHERE).21 In that study, analyses by baseline DM status have again been pre-specified and may further define the risks and benefits of aliskiren in diabetic and non-diabetic patients.
The aforementioned features inherent to subgroup analyses constitute the major limitations of this work and these results must be considered hypothesis generating only. An additional limitation is the definition of DM used. The presence or absence of underlying DM was determined solely by the investigator and it was not mandatory to use objective criteria such as baseline use of diabetic medications or previous haemoglobin A1c values. Thus, it is possible that the DM status reported in ASTRONAUT may not perfectly overlap with the true biological DM status of this population.
Conclusions
In the pre-specified subgroup of ASTRONAUT patients with and without DM, the addition of aliskiren to standard therapy in non-diabetics appeared to improve post-discharge outcomes and biomarker profile, and was generally well-tolerated. In contrast, diabetic patients receiving aliskiren appeared to have worse post-discharge outcomes. Given the persistently high post-discharge event rate despite available therapies, future prospective investigations are encouraged to confirm potential benefits of renin inhibition in a large cohort of HHF patients without DM.
Funding
The ASTRONAUT study is funded by Novartis Pharma AG, Basel, Switzerland under the guidance of the ASTRONAUT Executive Committee.
Conflict of interest: A.P.M. has served on committees of clinical studies sponsored by Amgen, Bayer, Abbott Vascular, Cardiorentis, Johnson & Johnson, and Novartis Pharma AG. S.J.G. has no disclosures to report. G.C.F. has received grants from GlaxoSmithKline, the National Institutes of Health, and the Agency for Healthcare Research and Quality; served on speakers' bureaus for Boston Scientific/Guidant, GlaxoSmithKline, Medtronic, Merck, Novartis, Pfizer, and St Jude Medical; served as a consultant for Amgen, Gambro, GlaxoSmithKline, Medtronic, Merck, Novartis, Pfilzer, Relypsa, Sdos, St Jude Medical, Medicines Company, Johnson & Johsnon, and Takeda. M.B. has served as a consultant for AstraZeneca, Bayer, Boehringer-Ingelheim, Daiichi-Sankyo, AWD Dresden, Berlin-Chemie, MSD, Novartis, Pfizer, Sanofi-Aventis, and Servier. F.Z. has received grant funding from Novartis, BG Medicine, and Roche Diagnostics; served on a board for Boston Scientific; and served as a consultant for Novartis, Takeda, AstraZeneca, Boehringer-Ingelheim, GE Healthcare, Relypsa, Servier, Boston Scientific, Bayer, Johnson & Johnson, and ResMed. S.D.S. has received grant funding, consultant fees, and travel support from Novartis. E.F.L. has received grant funding and other support from Novartis. F.B. is an employee of Novartis and has received consultant fees, travel support, stock options, and other funding from Novartis. T.A.H. is an employee of Novartis and has received travel support and stock options from Novartis. C.R.G. is an employee of Novartis and has received stock and stock options from Novartis. A.L. is an employee of Novartis and reported receiving consulting fees, travel support, stock options, and other funding from Novartis. M.G. has been a consultant for Abbott Laboratories, Astellas, AstraZeneca, Bayer HealthCare AG, CorThera, Cytokinetics, DebioPharm S.A., Errekappa Terapeutici, GlaxoSmithKline, Ikaria, Johnson & Johnson, Medtronic, Merck, Novartis Pharma AG, Otsuka Pharmaceuticals, Palatin Technologies, Pericor Therapeutics, Protein Design Laboratories, Sanofi-Aventis, Sigma Tau, Solvay Pharmaceuticals, Takeda Pharmaceutical, and Trevena Therapeutics.
ASTRONAUT Trial Investigators
Silvina Ramos, Alejandra Luna, Santiago Miriuka, Mirta Diez, Eduardo Perna, Hugo Luquez, Jorge Garcia Pinna, Jorge Castagnino, Pablo Alvarenga, Julio Ibañez, Eduardo Salmon Blumberg, Claudio Dizeo, Rodolfo Ahuad Guerrero, Pablo Schygiel, Rodolfo Milesi, Carlos Sosa, Miguel Hominal, Lilia Lobo Marquez, Carlos Poy, Eduardo Hasbani, Marisa Vico, Alberto Fernandez, Nestor Vita (Argentina); Johan Vanhaecke, Gilles De Keulenaer, Harry Striekwold, Geert Vervoort, Mathias Vrolix, Philippe Henry, Paul Dendale, Walter Smolders, Patrick Marechal, Hans Vandekerckhove (Belgium); Mucio Oliveira Jr., Fernando Neuenschwande, Gilmar Reis, Jose Saraiva, Luiz Bodanese, Manoel Canesin, Oswaldo Greco, Roberto Bassan, Roberto Luis Marino (Brazil); Nadia Giannetti, Gordon Moe, Bruce Sussex, Richard Sheppard, Thao Huynh, Robert Stewart, Haissam Haddad (Canada); Luis Echeverria, Adalberto Quintero, Adriana Torres, Mónica Jaramillo, Mónica Lopez, Fernan Mendoza, Noel Florez, Carlos Cotes, Magali Garcia (Colombia); Jan Belohlavek, Jaromir Hradec, Martin Peterka, Pavel Gregor, Zdenek Monhart, Petr Jansky, Jiri Kettner, Petr Reichert, Jindrich Spinar, Tomas Brabec, Martin Hutyra, Miroslav Solar (Czech Republic); Mikko Pietilä, Kai Nyman, Risto Pajari (Finland); Ariel Cohen, Michel Galinier, Philippe Gosse, Bernard Livarek, Yannick Neuder, Patrick Jourdain, François Picard, Richard Isnard (France); Uta Hoppe, Stefan Kaeaeb, Stefan Rosocha, Roland Prondzinsky, Stephan Felix, Hans-Dirk Duengen, Hans-Reiner Figulla, Sven Fischer, Steffen Behrens, Philipp Stawowy, Juergen Kruells-Muench, Fabian Knebel, Christoph Nienaber, Dierk Werner, Wilma Aron, Bjoern Remppis, Rainer Hambrecht, Klaus Kisters, Nikos Werner, Stefan Hoffmann, Siegbert Rossol, Ernst Geiss, Kristof Graf, Frank Hamann, Wolfgang von Scheidt, Robert Schwinger, Ulrich Tebbe, Angelika Costard-Jaeckle, Stephan Lueders, Thomas Heitzer, Marie-Louise Leutermann-Oei, Ruediger Braun-Dullaeus, Jens-Uwe Roehnisch, Gerhard Muth, Andreas Goette, Achim Rotter, Henning Ebelt, Hans-Georg Olbrich, Veselin Mitrovic, Christian Hengstenberg, Sebastian Schellong (Germany); Karoly Zamolyi, Andras Vertes, Andras Matoltsy, Attila Palinkas, Bela Herczeg, Dezso Apro, Geza Lupkovics, Janos Tomcsanyi, Kalman Toth, (Hungary); Atul Mathur, Darshan Banker, Anil Bharani, Jaspal Arneja, Aziz Khan, Milind Gadkari, Jagdish Hiremath, Nitin Patki, Makund Kumbla, Santosh M.J., Ravikishore A.G., Rajpal Abhaichand, Vijayakukmar Maniyal, Manjunath Nanjappa, P. Naveen Reddy, Kulasekaran Chockalingam, Rajendra Premchand, Vijay Mahajan (India); Basil Lewis, Dov Wexler, Michael Shochat, Andre Keren, Muhamad Omary, Amos Katz, Alon Marmor (Israel); Giuseppe Lembo, Salvatore Di Somma, Alessandro Boccanelli, Mario Barbiero, Giuseppe Pajes, Stefano De Servi, Dott Cosimo Greco, Fernando De Santis, Agata Floresta, Luigi Oltrona Visconti, Giancarlo Piovaccari, Claudio Cavallini, Matteo Di Biase, Dott Franco Masini, Corrado Vassanelli, Maurizio Viecca, Dott Francesco Cangemi, Salvatore Pirelli, Claudio Borghi, Massimo Volpe, Angelo Branzi, Dott Giovanni Percoco, Silvia Severi, Alberto Santini, Ettore De Lorenzi, Marco Metra, Valerio Zacà, Andrea Mortara (Italy); Francisco P Tranquilino, Noe A Babilonia, Arthur M Ferrolino, Benjamin Jr Manlutac (Philippines); Miroslaw Dluzniewski, Zofia Dzielinska, Ewa Nowalany-Kozie, Walentyna Mazurek, Jerzy Wierzchowiecki, Andrzej Wysokinski, Joanna Szachniewicz, Witold Romanowski, Magdalena Krauze-Wielicka, Piotr Jankowski, Piotr Berkowski, Kasprzak, Roman Szelemej, Andrzej Kleinrok, Zdzislawa Kornacewicz-Jac (Poland); Marius Vintila, Mircea Vladoianu, Constantin Militaru, Gheorghe Dan, Maria Dorobantu, Stefan Dragulescu (Romania); Victor Kostenko, Alexandr Vishnevsky, Boris Goloschekin, Vadim Tyrenko, Alexander Gordienko, Oxana Kislyak, Sergey Martsevich, Alexey Kuchmin, Yurii Karpov, Igor Fomin, Yury Shvarts, Olga Orlikova, Olga Ershova, Olga Berkovich, Maria Sitnikova, Inna Pakhomova, Svetlana Boldueva, Tatiana Tyurina, Vladimir Simanenkov, Mikhail Boyarkin, Nina Novikova, Sergey Tereschenko, Vladimir Zadionchenko, Zaur Shogenov, Ivan Gordeev, Valentin Moiseev (Russia); Raymond Wong, Hean Yee Ong, Ju Le Tan (Singapore); Eva Goncalvesova, CSc., Frantisek Kovar, Ivan Skalina, Viera Kasperova, Silvia Hojerova, Miroslav Szentivanyi, Branislav Stancak, Marian Babcak, Peter Kycina, Pavol Poliacik, Peter Toth, Jana Sirotiakova (Slovakia [Slovak Republic]); Esteban Lopez de Sa, Manuel Gomez Bueno, Manuel Martinez Selles, Jose Angel Cabrera, Ramon Bover Freire, Jose Ramon Gonzalez Juanatey, Josep Comin, Francisco Ridocci Soriano, Alejandro Lopez, Raul Vicho, Manuel Geraldia Lama (Spain); Maria Schaufelberger, Richard Brunotte, Bengt Ullman, Inger Hagerman, Stella Cizinsky (Sweden); Wen-Jin Cherng, Wen-Chung Yu, Chi-Tai Kuo, Kuan-Cheng Chang, Wen-Ter Lai, Jen-Yuan Kuo (Taiwan); Dilek Ural, Ozer Badak, Mustafa Akin, Zerrin Yigit, Mehmet Yokusoglu, Mehmet Yilmaz, Adnan Abaci, Haksun Ebinc (Turkey); Richard Perlman, David Parish, James Bergin, Kenneth Burnham, Christopher Brown, Justin Lundbye, Celeste Williams, Howard Eisen, Elizabeth Juneman, Susan Joseph, Mary Ann Peberdy, Jennifer Peura, Vishal Gupta, Kalim Habet, William French, Freny Mody, Susan Graham, Monica Hazelrigg, Eugene Chung, Stephanie Dunlap, Lazaros Nikolaidis, Samer Najjar, Richard Katz, Srinivas Murali, Joseph L. Izzo, Tracy Callister, Roland Phillips, Nicholas Lippolis, John Winterton, Sheba Meymandi, Karl Heilman III, Ron Oren, Ronald Zolty, Michael Brottman, D.R. Gunawardena, Kirkwood Adams, Denise Barnard, Marc Klapholz, James Fulmer (USA).
Study Executive Committee
M.G. (chair), A.P.M. (co-chair), M.B., G.C.F., F.Z.
Study Data Monitoring Committee
Karl Swedberg (chair), Jeffrey S. Borer, Bertram Pitt, Stuart Pocock, Jean Rouleau.
Central Endpoint Committee
S.D.S. (chair), E.F.L., Peter Finn, Howard Hartley, Larry Weinrauch, Ebrahim Barkoudah, Kayode Odutayo.
Acknowledgements
We thank Pravin Bolshete, BAMS, MSc (Novartis Healthcare, Hyderabad, India), for his help in formatting the manuscript, tables, and figures and Albert Kandra (Novartis, Basel, Switzerland) for statistical input.
References
- 1.Blecker S, Paul M, Taksler G, Ogedegbe G, Katz S. Heart failure associated hospitalizations in the United States. J Am Coll Cardiol. 2013;61:1259–1267. doi: 10.1016/j.jacc.2012.12.038. doi:10.1016/j.jacc.2012.12.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gheorghiade M, Vaduganathan M, Fonarow GC, Bonow RO. Rehospitalization for heart failure: problems and perspectives. J Am Coll Cardiol. 2013;61:391–403. doi: 10.1016/j.jacc.2012.09.038. doi:10.1016/j.jacc.2012.09.038. [DOI] [PubMed] [Google Scholar]
- 3.Cleland JG, Swedberg K, Follath F, Komajda M, Cohen-Solal A, Aguilar JC, Dietz R, Gavazzi A, Hobbs R, Korewicki J, Madeira HC, Moiseyev VS, Preda I, van Gilst WH, Widimsky J, Freemantle N, Eastaugh J, Mason J. The EuroHeart Failure survey programme—a survey on the quality of care among patients with heart failure in Europe. Part 1: patient characteristics and diagnosis. Eur Heart J. 2003;24:442–463. doi: 10.1016/s0195-668x(02)00823-0. doi:10.1016/S0195-668X(02)00823-0. [DOI] [PubMed] [Google Scholar]
- 4.Greenberg BH, Abraham WT, Albert NM, Chiswell K, Clare R, Stough WG, Gheorghiade M, O'Connor CM, Sun JL, Yancy CW, Young JB, Fonarow GC. Influence of diabetes on characteristics and outcomes in patients hospitalized with heart failure: a report from the Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF) Am Heart J. 2007;154:e271–e278. doi: 10.1016/j.ahj.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 5.Sarma S, Mentz RJ, Kwasny MJ, Fought AJ, Huffman M, Subacius H, Nodari S, Konstam M, Swedberg K, Maggioni AP, Zannad F, Bonow RO, Gheorghiade M. Association between diabetes mellitus and post-discharge outcomes in patients hospitalized with heart failure: findings from the EVEREST trial. Eur J Heart Fail. 2013;15:194–202. doi: 10.1093/eurjhf/hfs153. doi:10.1093/eurjhf/hfs153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gheorghiade M, Bohm M, Greene SJ, Fonarow GC, Lewis EF, Zannad F, Solomon SD, Baschiera F, Botha J, Hua TA, Gimpelewicz CR, Jaumont X, Lesogor A, Maggioni AP. Effect of aliskiren on postdischarge mortality and heart failure readmissions among patients hospitalized for heart failure: the ASTRONAUT randomized trial. JAMA. 2013;309:1125–1135. doi: 10.1001/jama.2013.1954. doi:10.1001/jama.2013.1954. [DOI] [PubMed] [Google Scholar]
- 7.Parving HH, Brenner BM, McMurray JJ, de Zeeuw D, Haffner SM, Solomon SD, Chaturvedi N, Persson F, Desai AS, Nicolaides M, Richard A, Xiang Z, Brunel P, Pfeffer MA. Cardiorenal end points in a trial of aliskiren for type 2 diabetes. N Engl J Med. 2012;367:2204–2213. doi: 10.1056/NEJMoa1208799. doi:10.1056/NEJMoa1208799. [DOI] [PubMed] [Google Scholar]
- 8.Gheorghiade M, Albaghdadi M, Zannad F, Fonarow GC, Bohm M, Gimpelewicz C, Botha J, Moores S, Lewis EF, Rattunde H, Maggioni A. Rationale and design of the multicentre, randomized, double-blind, placebo-controlled aliskiren trial on acute heart failure outcomes (ASTRONAUT) Eur J Heart Fail. 2011;13:100–106. doi: 10.1093/eurjhf/hfq209. doi:10.1093/eurjhf/hfq209. [DOI] [PubMed] [Google Scholar]
- 9.Wang R, Lagakos SW, Ware JH, Hunter DJ, Drazen JM. Statistics in medicine—reporting of subgroup analyses in clinical trials. N Engl J Med. 2007;357:2189–2194. doi: 10.1056/NEJMsr077003. doi:10.1056/NEJMsr077003. [DOI] [PubMed] [Google Scholar]
- 10.Miao Y, Dobre D, Heerspink HJ, Brenner BM, Cooper ME, Parving HH, Shahinfar S, Grobbee D, de Zeeuw D. Increased serum potassium affects renal outcomes: a post hoc analysis of the Reduction of Endpoints in NIDDM with the Angiotensin II Antagonist losartan (RENAAL) trial. Diabetologia. 2011;54:44–50. doi: 10.1007/s00125-010-1922-6. doi:10.1007/s00125-010-1922-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mann JF, Schmieder RE, McQueen M, Dyal L, Schumacher H, Pogue J, Wang X, Maggioni A, Budaj A, Chaithiraphan S, Dickstein K, Keltai M, Metsarinne K, Oto A, Parkhomenko A, Piegas LS, Svendsen TL, Teo KK, Yusuf S investigators O. Renal outcomes with telmisartan, ramipril, or both, in people at high vascular risk (the ONTARGET study): a multicentre, randomised, double-blind, controlled trial. Lancet. 2008;372:547–553. doi: 10.1016/S0140-6736(08)61236-2. doi:10.1016/S0140-6736(08)61236-2. [DOI] [PubMed] [Google Scholar]
- 12.Girerd N, Pang PS, Swedberg K, Fought A, Kwasny MJ, Subacius H, Konstam MA, Maggioni A, Gheorghiade M, Zannad F for the Ei. Serum aldosterone is associated with mortality and re-hospitalization in patients with reduced ejection fraction hospitalized for acute heart failure: analysis from the everest trial. Eur J Heart Fail. 2013 doi: 10.1093/eurjhf/hft100. doi:10.1093/eurjhf/hft100 (published ahead of print 19 June 2013) [DOI] [PubMed] [Google Scholar]
- 13.Zannad F, McMurray JJ, Krum H, van Veldhuisen DJ, Swedberg K, Shi H, Vincent J, Pocock SJ, Pitt B Group E-HS. Eplerenone in patients with systolic heart failure and mild symptoms. N Engl J Med. 2011;364:11–21. doi: 10.1056/NEJMoa1009492. doi:10.1056/NEJMoa1009492. [DOI] [PubMed] [Google Scholar]
- 14.McMurray JJ, Ostergren J, Swedberg K, Granger CB, Held P, Michelson EL, Olofsson B, Yusuf S, Pfeffer MA. Effects of candesartan in patients with chronic heart failure and reduced left-ventricular systolic function taking angiotensin-converting-enzyme inhibitors: the CHARM-Added trial. Lancet. 2003;362:767–771. doi: 10.1016/S0140-6736(03)14283-3. doi:10.1016/S0140-6736(03)14283-3. [DOI] [PubMed] [Google Scholar]
- 15.Cohn JN, Tognoni G Valsartan Heart Failure Trial I. A randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failure. N Engl J Med. 2001;345:1667–1675. doi: 10.1056/NEJMoa010713. doi:10.1056/NEJMoa010713. [DOI] [PubMed] [Google Scholar]
- 16.Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, Palensky J, Wittes J. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N Engl J Med. 1999;341:709–717. doi: 10.1056/NEJM199909023411001. doi:10.1056/NEJM199909023411001. [DOI] [PubMed] [Google Scholar]
- 17.Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Soliman EZ, Sorlie PD, Sotoodehnia N, Turan TN, Virani SS, Wong ND, Woo D, Turner MB. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation. 2012;125:e2–e220. doi: 10.1161/CIR.0b013e31823ac046. doi:10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen J, Normand SL, Wang Y, Krumholz HM. National and regional trends in heart failure hospitalization and mortality rates for medicare beneficiaries, 1998–2008. JAMA. 2011;306:1669–1678. doi: 10.1001/jama.2011.1474. doi:10.1001/jama.2011.1474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Bohm M, Dickstein K, Falk V, Filippatos G, Fonseca C, Gomez-Sanchez MA, Jaarsma T, Kober L, Lip GY, Maggioni AP, Parkhomenko A, Pieske BM, Popescu BA, Ronnevik PK, Rutten FH, Schwitter J, Seferovic P, Stepinska J, Trindade PT, Voors AA, Zannad F, Zeiher A. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology: developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2012;33:1787–1847. doi: 10.1093/eurheartj/ehs104. doi:10.1093/eurheartj/ehs104. [DOI] [PubMed] [Google Scholar]
- 20.Solomon SD, Dobson J, Pocock S, Skali H, McMurray JJ, Granger CB, Yusuf S, Swedberg K, Young JB, Michelson EL, Pfeffer MA. Influence of nonfatal hospitalization for heart failure on subsequent mortality in patients with chronic heart failure. Circulation. 2007;116:1482–1487. doi: 10.1161/CIRCULATIONAHA.107.696906. doi:10.1161/CIRCULATIONAHA.107.696906. [DOI] [PubMed] [Google Scholar]
- 21.Krum H, Massie B, Abraham WT, Dickstein K, Kober L, McMurray JJ, Desai A, Gimpelewicz C, Kandra A, Reimund B, Rattunde H, Armbrecht J ATMOSPHERE investigators. Direct renin inhibition in addition to or as an alternative to angiotensin converting enzyme inhibition in patients with chronic systolic heart failure: Rationale and design of the Aliskiren Trial to Minimize Outcomes in Patients with Heart Failure (ATMOSPHERE) study. Eur J Heart Fail. 2011;13:107–114. doi: 10.1093/eurjhf/hfq212. doi:10.1093/eurjhf/hfq212. [DOI] [PubMed] [Google Scholar]