Abstract
AIM: To study a retrospective analysis of patients who presented to the emergency departments (ED) with complaints related to foreign body ingestions.
METHODS: Patients older than 16 years of age who presented to the ED between January 1st and December 31st of 2010 with complaints related to swallowed foreign bodies were identified from electronic health records and patient charts.
RESULTS: A total of 100 patients presented with a complaint of foreign body ingestion during the study period. Overall, an X-ray was performed on 75 patients, and a fiberoptic evaluation was performed on 45 patients. A foreign body was detected in 46 (46%) patients. The diagnostic yield of the X-ray was 27 (36%) out of 75 patients, while the diagnostic yield of the fiberoptic evaluations was 21 (47%) out of 45 patients. The detected foreign bodies were mostly located in the esophagus (17 out of 46 foreign bodies detected). When the types of ingested foreign bodies were evaluated, 52 (52%) patients reported ingesting food, and 19 (19%) patients reported swallowing pins. An X-ray was performed on 33 patients with accidental food ingestions but yielded a positive result in only two cases. In 12 out of 21 patients with accidental food ingestion who underwent fiberoptic evaluation, the foreign material was detected and removed.
CONCLUSION: Plain radiography is helpful in the localization of radiopaque swollen foreign bodies, while fiberoptic methods are useful as both diagnostic and therapeutic tools, regardless of radiopacity.
Keywords: Foreign body, Ingestion, Gastrointestinal tract, Endoscopy, Emergency
Core tip: The majority of foreign bodies swallowed by patients who present to the emergency departments cannot be detected using standard imaging studies and evaluation. Plain radiography is especially useful in the localization of radiopaque foreign bodies, while fiberoptic methods can be used as both diagnostic and therapeutic tools, regardless of the radiopacity of the foreign body ingested.
INTRODUCTION
Visits related to gastrointestinal foreign bodies are relatively common causes of admission to emergency departments (ED)[1,2]. The ingestion or insertion of a foreign body into the gastrointestinal (GI) tract can be a clinically serious condition with associated risks for morbidity and mortality[2,3]. An estimated 1500 to 1600 patients die in the United States each year as a result of complications related to the ingestion or insertion of foreign bodies into the GI tract[1,3-5]. Although this problem can be encountered in every age group, almost 80% of cases comprise patients in early childhood (18-48 mo), with a majority of cases resulting from swallowing coins, toys, crayons, or pen caps[3,4]. The ingestion of foreign bodies is rarely seen in adults, is generally accidental and is commonly seen in the form of food (meat and bones) ingestion. Other risk groups for this type of injury include patients with psychiatric disorders, adults without teeth, prisoners and patients under the influence of substances that obscure judgment[3,5-7]. The clinical presentation, symptoms and management of foreign bodies depend on their location within the GI tract. Depending on the size and shape, almost 80%-90% of such foreign bodies pass freely from the GI tract without any complication[4,7,8].
The purpose of the present study was to conduct a retrospective analysis of patients who presented to our ED with complaints related to foreign body ingestions.
MATERIALS AND METHODS
Patients older than 16 years of age who presented to the Emergency Department between January 1st and December 31st of 2010 with complaints related to swallowed foreign bodies were analyzed retrospectively using the data obtained from electronic health records and patient charts. The patients’ present complaints, demographic characteristics, previous medical history and medication use, physical exam findings, diagnostic studies performed, type and location of the foreign body, treatment provided, need for conservative or invasive/surgical treatment, complication rates, radiological findings and rate of survival/mortality were all recorded.
RESULTS
During the study period, we identified a total of 100 patients (42 male, 58 female; mean age 38 years, range 16-88 years) who were admitted with a complaint of foreign body ingestion. Of those, 65 (65%) localized their complaints to the pharynx, while 35 (35%) told us that they had ingested the foreign bodies. Among the list of complaints, 53 (53%) patients had difficulty swallowing; 33 (33%) had pain in the throat; 6 (6%) had difficulty breathing; 5 (5%) had abdominal pain; 4 (4%) had vomiting; 4 (4%) had bleeding from the mouth; 2 (2%) had a foreign body sensation in the throat; 2 (2%) had coughing; and 1 (1%) had chest pain. The incident was self-reported as accidental in all patients. When facilitating factors were considered, 3 (3%) patients were undergoing dental interventions, and another 3 (3%) patients had dental plates. None of the study patients had any established diagnosis of psychiatric disease or history of substance abuse, alcohol or sedative use. Physical examination revealed oropharyngeal foreign bodies in 7 patients, epigastric tenderness in 1 patient, and rhonchus in 1 patient.
The diagnostic approaches to our patients are summarized in Figure 1. A foreign body was detected in 46 (46%) patients. The diagnostic yield of X-rays was 27 (36%) among the 75 patients evaluated by lateral neck, chest or abdominal X-ray. The foreign bodies were detected for 10 out of 51 patients using the chest X-ray, for 14 out of 29 patients using the abdominal X-ray and for 3 out of 52 patients using the lateral neck X-ray. The diagnostic yield was 21 (47%) out of 45 for all patients undergoing fiberoptic evaluations (Figure 1). The detected foreign bodies were mostly located in the esophagus (17 out of 46 foreign bodies detected) (Table 1). When the types of ingested foreign bodies were evaluated, 52 (52%) patients reported ingesting food, and 19 (19%) patients reported swallowing pins (Figure 2, Table 2). With respect to the types of ingested food, 20 were fish bones, 9 were bone fragments (Figure 3), and 23 were unknown food parts.
Figure 1.
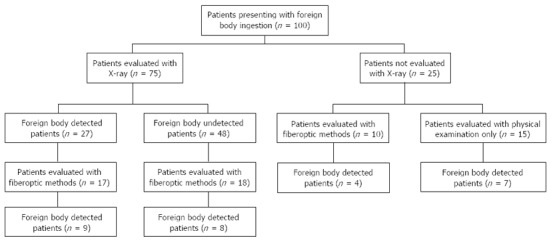
Diagnostic approach to patients presenting with foreign body ingestions.
Table 1.
Location of the foreign bodies (n = 100)
| Foreign body location | n (%) |
| Esophagus | 17 (17) |
| Oropharynx | 8 (8) |
| Small intestine | 6 (6) |
| Stomach | 6 (3) |
| Trachea | 2 (2) |
| Larynx | 3 (3) |
| Colon | 3 (3) |
| Undetermined location | 1 (1) |
| Undetected | 54 (54) |
Figure 2.
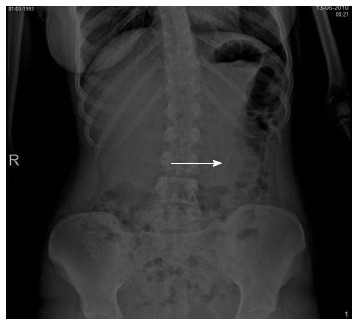
Plain abdominal X-ray showing a pin (white arrow) in the bowel in an adult. The pin passed spontaneously.
Table 2.
Types of foreign bodies swallowed
| Foreign body type | Total detected foreign bodies | Patients underwent X-ray | Foreign bodies detected with X-ray | Patients who underwent fiberoptic evaluation | Foreign bodies detected with endoscopy | |
| n | n | n | n | n | n | |
| Food | 52 | 20 | 33 | 2 | 21 | 12 |
| Pin | 19 | 17 | 19 | 17 | 10 | 6 |
| Toothpick | 5 | 1 | 3 | - | 4 | 1 |
| Dental instrument | 5 | 2 | 5 | 2 | 2 | - |
| Tooth filling | 4 | 2 | 4 | 2 | 2 | 1 |
| Nail | 2 | 2 | 2 | 2 | 2 | 1 |
| Water gel beads (pearl shape crystal soil) | 1 | - | 1 | - | - | - |
| Gelatin paper | 1 | - | - | - | 1 | - |
| Pen cap | 1 | - | - | - | 1 | - |
| Earring | 1 | - | 1 | - | 1 | - |
| Coin | 1 | 1 | 1 | 1 | - | - |
| Medication | 2 | - | 1 | - | - | - |
| Chewing gum | 1 | 1 | 1 | 1 | 1 | - |
| Unknown | 5 | - | 4 | - | - | - |
| Total | 100 | 46 | 75 | 27 | 45 | 21 |
Figure 3.

Lateral neck X-ray showing a bone fragment (white arrow). The fragment was removed by fiberoptic means.
In 53 (53%) of the patients, a conservative approach for management was considered. Nineteen (19%) patients were followed with serial radiological examinations. In 21 patients, of whom 17 were undergoing upper GI endoscopy, 2 were undergoing laryngoscopy and 2 were undergoing bronchoscopy, the foreign body was removed by fiberoptic means. In total, 19 (19%) of the study patients were admitted for further evaluation and treatment. Out of all the patients, the clinical course was complicated by aspiration (food material) in two patients, by GI bleed (pin) in 1 patient and by mediastinitis (food material) secondary to perforation in 1 patient.
DISCUSSION
The medical history obtained from the patient is highly critical in the diagnosis of swollen GI foreign bodies. Therefore, the planning of the diagnostic work-up and the extent and urgency of a possible intervention are decided according to the information provided by the patient regarding the type of foreign body ingested, together with the clinical complaints and physical examination[6,9-12]. Most GI foreign-body ingestions occur in pediatric patients aged between 6 mo and 6 years[5,7,9]. GI foreign body exposure tends to be accidental in adults, with food particles and bones constituting the majority of the foreign bodies[4,13]. The rest of the cases occur in the setting of facilitating factors, such as adults without teeth or with dental plates, prisoners and psychiatric patients[4,6,9,14,15]. Our results were also similar among all of the patients evaluated in the study reporting accidental intake. Patients who suffer foreign body ingestion can present with a wide range of symptoms, which can vary based on the physical characteristics and the content that is absorbed in the GI tract. Diagnosis is based on the patient’s history and complaints, which typically include the sudden onset of difficulty of swallowing during eating, chest pain, odynophagia or insufficiency in tolerating secretions. However, symptoms range from mild to life-threatening, including shortness of breath, abdominal pain, vomiting, hematemesis, foreign body sensation, coughing and chest pain[3,5,9,11,16,17]. In agreement with the literature, the majority of patients in our cohort presented with difficulty in swallowing and foreign body sensations in the throat.
Different types of foreign bodies are observed in the GI tract based on the age group. During childhood, swallowed coins, small toys, crayons or batteries are observed, whereas during adulthood, food, bones and dental-related foreign bodies are more common[4,6,7,9,13,16,17]. The types of foreign bodies may also differ by country. The high number of pin ingestions in our study group is thought to be related to the regional dress code, which results in women holding pins between their lips before attaching their headscarves. While certain conditions, such as parental attitudes and dietary habits, can provide clues for the types of foreign bodies that are ingested, prevention strategies are also dependent on various cultural, social, religious and economic factors[7,11,17-19].
The presentation, clinical findings, and management of foreign bodies are distinct and based upon the anatomical region where the foreign body is located[4,9,11,17]. Determining the type and location of the foreign body in the ED changes the treatment approach[5,9,16]. In our study, most of the foreign bodies were detected in the upper GI tract. The majority of the radiopaque foreign bodies in the GI tract can be detected using radiography. This simple modality provides crucial information, such as the number, size, location and direction of the foreign body, as well as the presence of sharp edges[2,3,6,8]. However, the presence of fish bones, chicken bones, glass, wood and thin metals cannot be ruled out by plain radiographies[2,3,6,11,13,20]. Neck, chest and abdominal radiographies are able to show perforations as well as metal objects and bones[6,13]. In our study, we detected a foreign body with plain radiography in 27 (36%) out of 75 patients evaluated by X-rays; all of these foreign bodies were radiopaque. All of the 19 patients with radiopaque foreign bodies in whom an emergency intervention was not planned were admitted for serial radiographic evaluations to determine the passage of the foreign body. Serial radiographic studies can be used to determine the passage of the foreign body and the complications resulting from it. If perforation is suspected based on the clinical or radiological findings, neck, chest or abdominal computed tomography is then indicated[13]. Computed tomography (CT) is especially useful when radiolucent materials cannot be detected with plain X-rays. A three-dimensional reconstruction with CT also increases the sensitivity of the detection modality[2,6,21-23]. CT can also be useful in determining, treatment options and complications.
Foreign bodies in the GI tract are typically treated conservatively, based on the type of foreign body and the patient’s clinical condition. Between 80% and 90% of foreign bodies pass through the GI tract freely, while 10% to 20% require an endoscopic intervention, and 1% require surgery[4,6-9,11,13,17,24,25]. Physicians should determine if and when an intervention is needed. The patient management strategies depend on a patient’s age and clinical condition, the type and size of the foreign body, the presence of sharp edges, the anatomical location and the endoscopic capability of the treating unit[2,3,5]. In general, foreign bodies larger than 2.5 cm in diameter cannot pass the pylorus, while objects longer than 6 cm cannot pass the duodenal curve. Therefore, these objects require endoscopic removal[2,6,19,26]. Endoscopic intervention is also indicated if the patient’s condition is not stable or if the foreign body is impacted or presents risks of further damage to the patient[13,27]. An emergent endoscopic removal should be performed in patients with esophageal obstruction (e.g., cannot swallow secretions), those with disc batteries in the esophagus and those who have swallowed pointed objects[6,13]. However, endoscopic removal is contraindicated if the foreign body is above the upper esophageal sphincter or if there is clinical or radiological evidence of perforation. Objects containing illegal drugs must be removed with endoscopy, but this technique should be avoided in cases where ruptured cocaine packages are present in the GI tract[6,13]. Objects located proximal to the upper esophageal sphincters are suggested to be removed by ear-nose-throat specialists[6,13]. Emergent endoscopy should be performed to remove magnets if they are within the reach of the technique[6]. Monitoring of the spontaneous passage of coins in asymptomatic patients is recommended. If there is no spontaneous passage, then removal within 24 h of ingestion is recommended[6,9]. We conducted conservative monitoring in slightly over half of our patients (53 out of 100). The diagnostic yield was 21 (47%) out of 45 for all patients undergoing fiberoptic evaluations. Endoscopic treatment options for meat or other food impactions included food extraction and advancement of the bolus into the stomach[6,9]. In our study, an X-ray was performed on 33 patients with accidental food ingestions but yielded a positive result in only two cases. By contrast, among 21 patients with accidental food ingestion who underwent fiberoptic evaluation, 12 patients were found to have a foreign material, and the material was removed. Food ingestion, a subjective feeling of foreign body sensation, and other properties of foreign bodies may have resulted in the poor yield of standard imaging studies and endoscopic and physical examinations[11,27].
An alternative radiological tool that was not systematically assessed in our study was ultrasonography, which is uncommonly used to diagnose GI foreign bodies in adults[28]. However, there are reports in the literature where ultrasonography proves to be useful in the detection of abdominal foreign bodies[9,29]. However, abdominal ultrasonography can be used as an initial imaging modality in the diagnosis of GI foreign bodies in pediatric patients[30].
Conditions such as acute abdomen due to intestinal perforations are seen in nearly 1% of patients who have ingested foreign bodies[8,31]. This condition can lead to severe complications and even death[32]. The most common complication of foreign body ingestion is perforation[33]; the ingestion of a sharp and pointed object is more likely to cause perforations[9,33,34]. Approximately 30%-35% of such objects can penetrate the GI tract, requiring endoscopic management[35]. In the presence of complications or in the case of unsuccessful endoscopic interventions, emergency surgery is preferred[35,36]. The majority of foreign bodies pass through the GI tract freely, without any complication, and only a small percentage of these cases require intervention[4,9].
In conclusion, a majority of the swallowed foreign bodies in patients presenting to the ED cannot be detected using standard imaging studies and evaluation. Plain radiography is especially useful in the localization of radiopaque foreign bodies, while fiberoptic methods can be used both as diagnostic and therapeutic tools, regardless of the radiopacity of the foreign body ingested. The goal of ED management is to refer patients with clinical significance to the appropriate departments for further evaluation and treatment. It is therefore important to evaluate the type and location of the foreign body and to identify complications that might develop as a result of this entity.
ACKNOWLEDGMENTS
The authors would like to thank Murat Arsava and Anıl Barak Dolgun for their contributions to the manuscript and data analysis.
COMMENTS
Background
Ingestions or insertions of foreign bodies are rarely seen in adults, are generally accidental and are commonly seen in the form of food ingestion (such as meat and bones). Nonetheless, foreign body ingestions into the gastrointestinal tract can lead to clinically serious conditions with significant morbidity and mortality. Approximately 80%-90% of the foreign bodies pass through the gastrointestinal tract freely, while 10%-20% require an endoscopic intervention, and 1% require surgery.
Research frontiers
The majority of swallowed foreign bodies in patients presenting to emergency departments cannot be detected using standard imaging tools. The research hotspot discussed here is that fiberoptic methods were implemented in both the diagnosis and treatment of gastrointestinal foreign bodies.
Innovations and breakthroughs
The most common approach for the detection of ingested foreign bodies in the gastrointestinal tract is physical examination combined with radiological studies. While radiological examinations are especially helpful in the detection of radiopaque foreign bodies, these studies are unyielding in a significant proportion of patients, depending on the timing of presentation and the nature of the ingested foreign body. Early evaluation with fiberoptic methods helps not only in the diagnosis and localization of the foreign body but also in its removal.
Applications
Dietary habits and various cultural factors can provide clues for the types of foreign bodies likely to be ingested. Fiberoptic methods can be used to diagnose and treat accidental foreign body ingestions in an emergency department setting.
Peer review
The present study is a retrospective analysis of 100 patients with complaints related to foreign body ingestions. The data suggest that plain radiography is especially useful in the localization of radiopaque foreign bodies, while fiberoptic methods can be used as both diagnostic and therapeutic tools, regardless of the radiopacity of the foreign body ingested. This study highlights interesting points regarding the clinical treatment of complaints related to foreign body ingestions.
Footnotes
P- Reviewers Tohda G, Triantopoulou C, Xu WX S- Editor Cui XM L- Editor A E- Editor Zhang DN
References
- 1.Katsinelos P, Kountouras J, Paroutoglou G, Zavos C, Mimidis K, Chatzimavroudis G. Endoscopic techniques and management of foreign body ingestion and food bolus impaction in the upper gastrointestinal tract: a retrospective analysis of 139 cases. J Clin Gastroenterol. 2006;40:784–789. doi: 10.1097/01.mcg.0000225602.25858.2c. [DOI] [PubMed] [Google Scholar]
- 2.Lee JH, Kim HC, Yang DM, Kim SW, Jin W, Park SJ, Kim HJ. What is the role of plain radiography in patients with foreign bodies in the gastrointestinal tract? Clin Imaging. 2012;36:447–454. doi: 10.1016/j.clinimag.2011.11.017. [DOI] [PubMed] [Google Scholar]
- 3.Ayantunde AA, Oke T. A review of gastrointestinal foreign bodies. Int J Clin Pract. 2006;60:735–739. doi: 10.1111/j.1368-5031.2006.00709.x. [DOI] [PubMed] [Google Scholar]
- 4.Anderson KL, Dean AJ. Foreign bodies in the gastrointestinal tract and anorectal emergencies. Emerg Med Clin North Am. 2011;29:369–400, ix. doi: 10.1016/j.emc.2011.01.009. [DOI] [PubMed] [Google Scholar]
- 5.Eisen GM, Baron TH, Dominitz JA, Faigel DO, Goldstein JL, Johanson JF, Mallery JS, Raddawi HM, Vargo JJ, Waring JP, et al. Guideline for the management of ingested foreign bodies. Gastrointest Endosc. 2002;55:802–806. doi: 10.1016/s0016-5107(02)70407-0. [DOI] [PubMed] [Google Scholar]
- 6.Ikenberry SO, Jue TL, Anderson MA, Appalaneni V, Banerjee S, Ben-Menachem T, Decker GA, Fanelli RD, Fisher LR, Fukami N, et al. Management of ingested foreign bodies and food impactions. Gastrointest Endosc. 2011;73:1085–1091. doi: 10.1016/j.gie.2010.11.010. [DOI] [PubMed] [Google Scholar]
- 7.Li ZS, Sun ZX, Zou DW, Xu GM, Wu RP, Liao Z. Endoscopic management of foreign bodies in the upper-GI tract: experience with 1088 cases in China. Gastrointest Endosc. 2006;64:485–492. doi: 10.1016/j.gie.2006.01.059. [DOI] [PubMed] [Google Scholar]
- 8.Velitchkov NG, Grigorov GI, Losanoff JE, Kjossev KT. Ingested foreign bodies of the gastrointestinal tract: retrospective analysis of 542 cases. World J Surg. 1996;20:1001–1005. doi: 10.1007/s002689900152. [DOI] [PubMed] [Google Scholar]
- 9.Ambe P, Weber SA, Schauer M, Knoefel WT. Swallowed foreign bodies in adults. Dtsch Arztebl Int. 2012;109:869–875. doi: 10.3238/arztebl.2012.0869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Webb WA. Management of foreign bodies of the upper gastrointestinal tract: update. Gastrointest Endosc. 1995;41:39–51. doi: 10.1016/s0016-5107(95)70274-1. [DOI] [PubMed] [Google Scholar]
- 11.Chiu YH, Hou SK, Chen SC, How CK, Lam C, Kao WF, Yen DH, Huang MS. Diagnosis and endoscopic management of upper gastrointestinal foreign bodies. Am J Med Sci. 2012;343:192–195. doi: 10.1097/MAJ.0b013e3182263035. [DOI] [PubMed] [Google Scholar]
- 12.Ginsberg GG. Management of ingested foreign objects and food bolus impactions. Gastrointest Endosc. 1995;41:33–38. doi: 10.1016/s0016-5107(95)70273-3. [DOI] [PubMed] [Google Scholar]
- 13.Telford JJ. Management of ingested foreign bodies. Can J Gastroenterol. 2005;19:599–601. doi: 10.1155/2005/516195. [DOI] [PubMed] [Google Scholar]
- 14.Conway WC, Sugawa C, Ono H, Lucas CE. Upper GI foreign body: an adult urban emergency hospital experience. Surg Endosc. 2007;21:455–460. doi: 10.1007/s00464-006-9004-z. [DOI] [PubMed] [Google Scholar]
- 15.Lyons MF, Tsuchida AM. Foreign bodies of the gastrointestinal tract. Med Clin North Am. 1993;77:1101–1114. doi: 10.1016/s0025-7125(16)30212-7. [DOI] [PubMed] [Google Scholar]
- 16.Jayachandra S, Eslick GD. A systematic review of paediatric foreign body ingestion: presentation, complications, and management. Int J Pediatr Otorhinolaryngol. 2013;77:311–317. doi: 10.1016/j.ijporl.2012.11.025. [DOI] [PubMed] [Google Scholar]
- 17.Zhang S, Cui Y, Gong X, Gu F, Chen M, Zhong B. Endoscopic management of foreign bodies in the upper gastrointestinal tract in South China: a retrospective study of 561 cases. Dig Dis Sci. 2010;55:1305–1312. doi: 10.1007/s10620-009-0900-7. [DOI] [PubMed] [Google Scholar]
- 18.Chotigavanich C, Ballali S, Foltran F, Passali D, Bellussi L, Gregori D. Foreign bodies injuries in children: analysis of Thailand data. Int J Pediatr Otorhinolaryngol. 2012;76 Suppl 1:S80–S83. doi: 10.1016/j.ijporl.2012.02.019. [DOI] [PubMed] [Google Scholar]
- 19.Palta R, Sahota A, Bemarki A, Salama P, Simpson N, Laine L. Foreign-body ingestion: characteristics and outcomes in a lower socioeconomic population with predominantly intentional ingestion. Gastrointest Endosc. 2009;69:426–433. doi: 10.1016/j.gie.2008.05.072. [DOI] [PubMed] [Google Scholar]
- 20.Ngan JH, Fok PJ, Lai EC, Branicki FJ, Wong J. A prospective study on fish bone ingestion. Experience of 358 patients. Ann Surg. 1990;211:459–462. doi: 10.1097/00000658-199004000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shihada R, Goldsher M, Sbait S, Luntz M. Three-dimensional computed tomography for detection and management of ingested foreign bodies. Ear Nose Throat J. 2009;88:910–911. [PubMed] [Google Scholar]
- 22.Coulier B, Tancredi MH, Ramboux A. Spiral CT and multidetector-row CT diagnosis of perforation of the small intestine caused by ingested foreign bodies. Eur Radiol. 2004;14:1918–1925. doi: 10.1007/s00330-004-2430-1. [DOI] [PubMed] [Google Scholar]
- 23.Marco De Lucas E, Sádaba P, Lastra García-Barón P, Ruiz-Delgado ML, González Sánchez F, Ortiz A, Pagola MA. Value of helical computed tomography in the management of upper esophageal foreign bodies. Acta Radiol. 2004;45:369–374. doi: 10.1080/02841850410005516. [DOI] [PubMed] [Google Scholar]
- 24.Binder L, Anderson WA. Pediatric gastrointestinal foreign body ingestions. Ann Emerg Med. 1984;13:112–117. doi: 10.1016/s0196-0644(84)80573-9. [DOI] [PubMed] [Google Scholar]
- 25.Sung SH, Jeon SW, Son HS, Kim SK, Jung MK, Cho CM, Tak WY, Kweon YO. Factors predictive of risk for complications in patients with oesophageal foreign bodies. Dig Liver Dis. 2011;43:632–635. doi: 10.1016/j.dld.2011.02.018. [DOI] [PubMed] [Google Scholar]
- 26.Smith MT, Wong RK. Foreign bodies. Gastrointest Endosc Clin N Am. 2007;17:361–82, vii. doi: 10.1016/j.giec.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 27.Stack LB, Munter DW. Foreign bodies in the gastrointestinal tract. Emerg Med Clin North Am. 1996;14:493–521. doi: 10.1016/s0733-8627(05)70264-9. [DOI] [PubMed] [Google Scholar]
- 28.Coulier B. [Diagnostic ultrasonography of perforating foreign bodies of the digestive tract] J Belge Radiol. 1997;80:1–5. [PubMed] [Google Scholar]
- 29.Piotto L, Gent R, Kirby CP, Morris LL. Preoperative use of ultrasonography to localize an ingested foreign body. Pediatr Radiol. 2009;39:299–301. doi: 10.1007/s00247-008-1096-2. [DOI] [PubMed] [Google Scholar]
- 30.Moammar H, Al-Edreesi M, Abdi R. Sonographic diagnosis of gastric-outlet foreign body: case report and review of literature. J Family Community Med. 2009;16:33–36. [PMC free article] [PubMed] [Google Scholar]
- 31.Pinero Madrona A, Fernández Hernández JA, Carrasco Prats M, Riquelme Riquelme J, Parrila Paricio P. Intestinal perforation by foreign bodies. Eur J Surg. 2000;166:307–309. doi: 10.1080/110241500750009140. [DOI] [PubMed] [Google Scholar]
- 32.Rodríguez-Hermosa JI, Codina-Cazador A, Sirvent JM, Martín A, Gironès J, Garsot E. Surgically treated perforations of the gastrointestinal tract caused by ingested foreign bodies. Colorectal Dis. 2008;10:701–707. doi: 10.1111/j.1463-1318.2007.01401.x. [DOI] [PubMed] [Google Scholar]
- 33.Syrakos T, Zacharakis E, Antonitsis P, Zacharakis E, Spanos C, Georgantis G, Kiskinis D. Surgical intervention for gastrointestinal foreign bodies in adults: a case series. Med Princ Pract. 2008;17:276–279. doi: 10.1159/000129605. [DOI] [PubMed] [Google Scholar]
- 34.Tsesmeli NE, Savopoulos CG, Hatzitolios AI, Karamitsos DT. Public health and potential complications of novel fashion accessories: an unusual foreign body in the upper gastrointestinal tract of an adolescent. Cent Eur J Public Health. 2007;15:172–174. doi: 10.21101/cejph.b0043. [DOI] [PubMed] [Google Scholar]
- 35.Chang JJ, Yen CL. Endoscopic retrieval of multiple fragmented gastric bamboo chopsticks by using a flexible overtube. World J Gastroenterol. 2004;10:769–770. doi: 10.3748/wjg.v10.i5.769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Park JH, Park CH, Park JH, Lee SJ, Lee WS, Joo YE, Kim HS, Choi SK, Rew JS, Kim SJ. [Review of 209 cases of foreign bodies in the upper gastrointestinal tract and clinical factors for successful endoscopic removal] Korean J Gastroenterol. 2004;43:226–233. [PubMed] [Google Scholar]


