Abstract
Duodenal duplication cysts are benign rare congenital anomalies reported mainly in the pediatric population, but seldom in adults. Symptoms depend on the type and location and can present as abdominal pain, distension, dysphagia or dyspepsia. They have been reported to be responsible for duodenal obstruction, pancreatitis and, in rare cases, gastrointestinal bleeding. We present a case of a duodenal duplication cyst in a 43-year-old man presenting as melena. Initial gastroduodenoscopy and colonoscopy did not reveal any bleeding focus. However, the patient began passing melena after 3 d, with an acute decrease in hemoglobin levels. Subsequent studies revealed a duplication cyst in the second portion of the duodenum which was surgically resected. Histology revealed a duodenal duplication cyst consisting of intestinal mucosa. There was no further bleeding and the patient recovered completely. In rare cases, duodenal duplication cysts might cause gastrointestinal bleeding and should be included in the differential diagnosis.
Keywords: Gastrointestinal hemorrhage, Duodenum, Duplication
Core tip: Duodenal duplication cysts are rare congenital anomalies that have been seldom reported in adults. Most cases of duodenal duplication have been associated with pancreatitis or jaundice and few have been reported as a cause of gastrointestinal hemorrhage. We submit a case of duodenal duplication cyst causing gastrointestinal hemorrhage. In rare cases, duodenal duplication cysts may cause gastrointestinal bleeding and must be included in the differential diagnosis.
INTRODUCTION
Duplication cysts are rare congenital anomalies of the gastrointestinal (GI) tract. Duodenal duplication cysts are extremely rare, representing only 2%-12% of GI tract duplications[1]. Most duplication cysts are detected in children and fewer than 30% of all duplications are diagnosed in adults[2]. They are difficult to diagnose, as the presenting symptoms are nonspecific and are closely related to the type, size and location of the lesion[1]. We report a rare case of duodenal duplication with duodenoduodenal intussusception presenting as GI bleeding.
CASE REPORT
A 43-year-old man was admitted to the emergency department complaining of melena. He had complained of recurrent burning, nonradiating upper abdominal pain, usually lasting for several minutes, irregular in nature and relieved by taking food since childhood. Ten years previously, he had been diagnosed with a gastric ulcer and had taken medications for 1 year.
His vital signs upon admission were a blood pressure of 120/80 mmHg and a heart rate of 105 beats/min. Initial laboratory studies revealed a hemoglobin level of 9.7 g/dL (normal range, 14-18 g/dL), hematocrit 28.8% (normal range, 42.0%-52.0%) and mean red corpuscular volume 88.4 fL (normal range, 80-94 fL). A nasogastric tube was inserted, but no blood was aspirated.
An initial gastroduodenoscopy showed no evidence of active bleeding or obvious focus. A colonoscopic examination was unremarkable, except for the presence of internal hemorrhoids. After a blood transfusion of 220 mL packed red blood cells, his hemoglobin level rose to 10.3 g/dL and there was no clinical evidence of further bleeding.
On the third day of hospitalization, the patient passed about 200 mL of melena and his hemoglobin levels fell to 7.6 g/dL. Gastroduodenoscopy revealed fresh blood oozing without a definite bleeding focus in the second portion of the duodenum. As there was no obvious bleeding focus, a high-resolution computed tomography (CT) scan of the abdomen was done. It revealed a circumferential cystic lesion in the proximal duodenum arising from a duodenoduodenal intussusception (Figure 1). As the patient did not have any symptoms except for melena and physical examinations did not reveal any palpable sausage-shaped abdominal mass suggestive of intussusception, an upper GI series was done. This demonstrated a large elongated sac-like 10 cm long mass in the second and proximal third portion of the duodenum (Figure 2). The junction of the first and second portions of the duodenum, where the mass began, was narrowed locally and the second portion of the duodenum was enlarged. This feature suggested a large elongated communicating duplication cyst (about 10 cm long) in the second and proximal third portion of the duodenum with duodenoduodenal intussusception.
Figure 1.
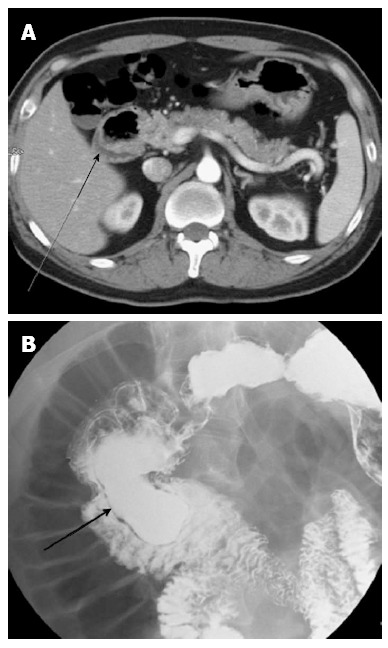
Computed tomography image. A: A high resolution computed tomography image of the abdomen reveals a circumferential cystic lesion (arrow) in the vicinity of the second part of the duodenum; B: Upper gastrointestinal series showing an large elongated sac-like mass (about 10 cm in length, arrow) arising from the second and proximal third portion of the duodenum.
Figure 2.
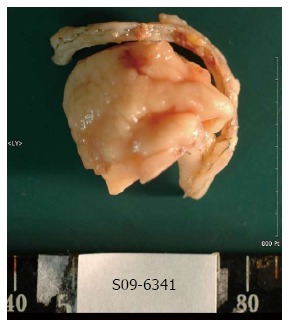
Gross specimen of the excised duodenal duplication cyst.
As rare cases of GI cysts with malignancies have been reported in the literature, bleeding from a cancer could not be ruled out. Because of the recurrent bleeding symptoms and the possibility of a cancer being present, we chose surgical resection. This revealed a mass attached to the second and third portion of the duodenum. After duodenotomy, the cyst was opened and blood clots were found in its cavity. Subtotal resection of the cyst was done followed by primary closure of the duodenum. A macroscopic examination showed an irregular, flat mass measuring 4 cm × 4 cm × 0.5 cm, covered with intestinal mucosa and with hemorrhagic contents (Figure 3). Microscopy revealed showed the cyst wall to be composed of two mucosal layers sharing a common muscle layer (Figure 3). The patient had an uneventful recovery and was discharged 12 d later. Follow-up visits at our outpatient clinic have revealed no sign of further GI bleeding.
Figure 3.
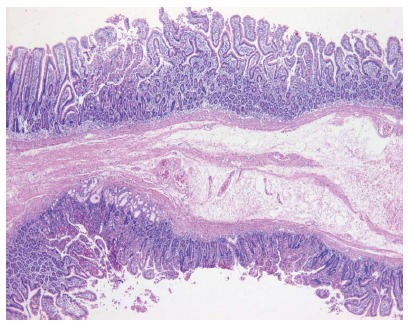
Histology of the duplication cyst showing two mucosal layers sharing a submucosal layer with muscular layer. Some of the mucosa are comprised of duodenal mucosa and the majority are jejunal mucosa (hematoxylin and eosin stain, × 40).
DISCUSSION
GI duplication cysts are rare congenital anomalies formed during the embryonic development of the alimentary tract. They are defined by a smooth muscle coat, an intimate attachment to the native GI tract and a GI mucosal lining[3]. They can occur anywhere along the GI tract, with varying types, shapes and sizes. GI duplication cysts are most commonly found in the distal ileum, followed by the esophagus, colon and jejunum[4].
Duodenal duplication cysts are among the rarest of all intestinal duplications. Most are located in the second or third portion of the duodenum. The cysts are usually filled with clear fluid, but might contain gallstones, bile or pancreatic fluid depending on communication with the biliary or pancreatic systems[5]. Most are diagnosed in childhood, with diverse, nonspecific clinical presentations[6]. The most common symptoms reported are abdominal pain and nausea/vomiting. The most common complication is pancreatitis, reported in up to 53% of patients. Other manifestations such as intussusceptions, infection or weight loss have also been reported[1]. Though rare, GI bleeding can result from peptic ulceration of the ectopic gastric mucosa within the cyst and be a cause of unexplained GI bleeding[5]. The bleeding can be painless, brisk and life threatening, as shown in our patient. The bleeding in our case was made more interesting by the fact that histology did not reveal any ectopic gastric mucosa within the cyst, contrary to previous reports[1,7,8].
The diagnosis of duodenal duplication cysts is difficult. The site of origin, such as an intraluminal or intramural position, and the presence or absence of luminal communication has to be taken into account. If the cyst is intraluminal, differentiation must be made between a pedunculated neoplastic lesion or a duodenal diverticulum. In the case of an intramural mass, a distended duodenal duplication has to be differentiated from other cystic masses belonging to the duodenal-choledochal- pancreatic area such as cystic dystrophy of the duodenal wall, choledochal cyst, pseudocysts, cystic tumors of the pancreas, cystic lymphangiomas, or mesenteric cysts. An empty duodenal duplication shows a solid structure and has to be differentiated from neoplastic or inflammatory duodenal or pancreatic lesions[9].
The preoperative diagnosis of duodenal duplications is often inaccurate. Diagnosis is usually done using imaging modalities such as ultrasonography or CT scans. On ultrasonography, duodenal duplication is seen as having an echogenic inner mucosa surrounded by a hypoechoic outer muscular layer[4]. CT scans often reveal a cystic mass associated with the alimentary tract and is more useful in demonstrating the precise anatomical relationship between the cyst and surrounding structures[4]. Magnetic resonance images as well as endoscopic ultrasonography allow us to suspect duplications and are useful in evaluating upper GI tract masses[3,9]. On contrast CT series of the GI, duodenal duplication cysts can present as smooth submucosal or extrinsic masses, or as oval filling defects in the duodenum, as can be seen in our case. In case of bleeding, the most sensitive tool is gastroduodenoscopy, which can locate the bleeding duplication in the duodenum[8]. However, all modalities allow us only to suspect the presence of an abnormal lesion, and diagnostic confirmation is possible only after resection.
Treatment of duodenal duplication has classically involved surgical resection. However, cases of endoscopical treatment have been reported, especially in cases where the duplication is in close proximity to the adjacent structures such as the major duodenal papillae[10]. In our case, endoscopical treatment was not possible because the duplication was not visible by endoscopy, leading to the need for surgical excision. Treatment of asymptomatic cases remains controversial. However, as neoplasms have been reported within duodenal duplication cysts, surgical resection must be considered[1].
In conclusion, duodenal duplication cysts are rare congenital anomalies that are seldom reported in adults. Clinical presentations are diverse, but there are a few reports of GI bleeding. Here we report a case of a duodenal duplication cyst with overt GI bleeding and suggest that such cysts should be considered in cases of undiagnosed GI bleeding.
Footnotes
P- Reviewer Kate V S- Editor Gou SX L- Editor A E- Editor Zhang DN
References
- 1.Chen JJ, Lee HC, Yeung CY, Chan WT, Jiang CB, Sheu JC. Meta-analysis: the clinical features of the duodenal duplication cyst. J Pediatr Surg. 2010;45:1598–1606. doi: 10.1016/j.jpedsurg.2010.01.010. [DOI] [PubMed] [Google Scholar]
- 2.Browning RW. Duodenal duplications. Rev Surg. 1963;20:226–229. [PubMed] [Google Scholar]
- 3.Chang HC, Huang SC, Wu RC, Yu MC. Duodenal duplication cyst: a rare cause of geriatric gastrointestinal bleeding. J Chin Med Assoc. 2011;74:233–236. doi: 10.1016/j.jcma.2011.03.010. [DOI] [PubMed] [Google Scholar]
- 4.Lee NK, Kim S, Jeon TY, Kim HS, Kim DH, Seo HI, Park do Y, Jang HJ. Complications of congenital and developmental abnormalities of the gastrointestinal tract in adolescents and adults: evaluation with multimodality imaging. Radiographics. 2010;30:1489–1507. doi: 10.1148/rg.306105504. [DOI] [PubMed] [Google Scholar]
- 5.Lad RJ, Fitzgerald P, Jacobson K. An unusual cause of recurrent pancreatitis: duodenal duplication cyst. Can J Gastroenterol. 2000;14:341–345. doi: 10.1155/2000/152809. [DOI] [PubMed] [Google Scholar]
- 6.Kirtley JA, Matuska RA. Enterogenous cyst of the duodenum. Ann Surg. 1957;145:265–268. doi: 10.1097/00000658-195702000-00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Knight CD, Allen MJ, Nagorney DM, Wold LE, DiMagno EP. Duodenal duplication cyst causing massive bleeding in an adult: an unusual complication of a duplication cyst of the digestive tract. Mayo Clin Proc. 1985;60:772–775. doi: 10.1016/s0025-6196(12)60419-4. [DOI] [PubMed] [Google Scholar]
- 8.Rubin RB, Saltzman JR, Zawacki JK, Khan A, Swanson R. Duodenal duplication cyst with massive gastrointestinal bleeding. J Clin Gastroenterol. 1995;21:72–74. doi: 10.1097/00004836-199507000-00015. [DOI] [PubMed] [Google Scholar]
- 9.Rotondo A, Scialpi M, Pellegrino G, Salzano De Luna F, Coppola L, Angelelli G. Duodenal duplication cyst: MR imaging appearance. Eur Radiol. 1999;9:890–893. doi: 10.1007/s003300050762. [DOI] [PubMed] [Google Scholar]
- 10.Antaki F, Tringali A, Deprez P, Kwan V, Costamagna G, Le Moine O, Delhaye M, Cremer M, Devière J. A case series of symptomatic intraluminal duodenal duplication cysts: presentation, endoscopic therapy, and long-term outcome (with video) Gastrointest Endosc. 2008;67:163–168. doi: 10.1016/j.gie.2007.08.006. [DOI] [PubMed] [Google Scholar]


