Abstract
There is a need for successful models of how to recruit, train, and retain bench scientists at the earliest stages of their careers into translational research. One recent, promising model is the University of California Davis Howard Hughes Medical Institute Integrating Medicine into Basic Science (HHMI‐IMBS) program, part of the HHMI Med into Grad initiative. This paper outlines the HHMI‐IMBS program's logic, design, and curriculum that guide the goal of research that moves from bedside to bench. That is, a curriculum that provides graduate students with guided translational training, clinical exposure, team science competencies, and mentors from diverse disciplines that will advance the students careers in clinical translational research and re‐focusing of research to answer clinical dilemmas. The authors have collected data on 55 HHMI‐IMBS students to date. Many of these students are still completing their graduate work. In the current study the authors compare the initial two cohorts (15 students) with a group of 29 control students to examine the program success and outcomes. The data indicate that this training program provides an effective, adaptable model for training future translational researchers. HHMI‐IMBS students showed improved confidence in conducting translational research, greater interest in a future translational career, and higher levels of research productivity and collaborations than a comparable group of predoctoral students.
Keywords: translational training, medical education, graduate students
Biomedical researchers have made great strides uncovering the underlying mechanisms of disease. However, they have encountered many challenges translating their basic research findings to the treatment of patients.1, 2, 3, 4 In a recent literature review, Heller and de Melo‐Martin5 found that barriers generally fell into three main categories: research workforce, research operations, and organizational silos. Among the specific challenges were an insufficient number of researchers skilled in translational research, a lack of institutional support for this type of research, and poor communication between researchers in different disciplines and fields.
Organizational and institutional barriers to translational research have proven very difficult to overcome even for institutions that have developed centers for translational research.5 Heller and de Melo‐Martin argue that this is because of the limited control centers have over many aspects of their broader institutions. Although large‐scale institutional barriers will eventually need to be addressed to move translational research forward, centers and other entities that want to promote translational research may find that the most direct avenue for supporting and promoting translational research is through structured mentoring and training for future translational researchers.4, 6
In 2005, the Howard Hughes Medical Institute (HHMI) created the “Med‐Into‐Grad” Initiative to establish training programs that would expose graduate students to medicine and produce a cadre of translational researchers who could conduct high‐quality science, and also understand and make the links necessary to eventually apply new discoveries to improve human health. As one of the initial 13 institutions funded by the Med‐Into‐Grad Initiative, the University of California, Davis developed the Integrating Medicine into Basic Science (IMBS) program that set the groundwork for an innovative translational training program for basic science and engineering predoctoral students. In this paper, we describe the development of this training program, the key elements of its adaptable curriculum, and the initial impact of the program on both the participating graduate students and faculty. The program has evolved into a flexible, highly effective model that is now a sustainable anchor of the UC Davis translational research education curriculum. Evaluation of early outcomes data suggest that the HHMI‐IMBS can serve as a successful model both institutionally and nationally for training translational researchers.
Training Program Design
In 2006, the HHMI Med‐Into‐Grad initiative provided $10 million in funding for training programs that would introduce PhD students in the biomedical sciences and related disciplines to the world of clinical medicine. The stated objective was to train researchers to have the necessary knowledge and skills to investigate clinically significant biological questions from a basic science viewpoint. Such trainees would have the potential to become future leaders in translational health research. As one of the initial 13 institutions funded by the HHMI Med‐Into‐Grad Initiative, the University of California, Davis developed an innovative translational training program, Integrating Medicine into Basic Science (IMBS), for basic science and engineering predoctoral students.
Program Development and Leadership
The ideas for the program initially developed from conversations between two of the authors (AB and JR) about the need for training scientists about medicine to foment translational research that would lead to new developments on disease treatment. Once establishing the actual program came about, one of the authors (AK) translated the original ideas to an actual curriculum with the advice of two authors (AB and JR). Further enhancement in development of the training program and the development of an effective and informative evaluation system were done with the input of all the authors.
Launched in 2006, the UC Davis HHMI‐IMBS training program annually selects 8 basic science and engineering graduate students who are interested in integrating science and medicine. Students can be from any year of graduate school beyond the first year of graduate school. With this approach, students have already established the PI with whom they will do their thesis work and completed more than half of their course work, if not all. Students come from diverse backgrounds, such as biomedical engineering, molecular biology, chemistry, and nutrition. The training program was based on the premise that success is critically dependent on changing the research culture from one of silos to a team‐based approach wherein basic scientists and clinicians work shoulder‐to‐shoulder in research. To create this new research training model, the program pursues a unique strategy which consists of: (1) immersing scholars in the clinical milieu; (2) providing scholars with opportunities for clinical co‐mentoring and collaborative partnerships; and (3) creating curriculum reinforcing the integration of excellent science with translational research.
Curriculum
Summer institute
An important objective of the program is for scholars to understand the culture and language of medicine through exposure to a range of clinical experiences. In the first years of the program, the focus was confined to cardiovascular (CV) disease, which is the area of expertise of three of the founding faculty, which facilitates organizing clinical rotations and teaching the translational focus. There was strong commitment in cardiology from the Division Chair as well as individual faculty to the development of new therapies, and all saw the training program as an opportunity for development of new treatments for CV disease. Furthermore, there is a strong emphasis on teaching at the university. The entire faculty participated in the program without compensation, and most of the involved faculties have participated for many years with tremendous commitment and enthusiasm. For most faculty time commitments were 16–20 hours per year with most activities involving introducing the scholars to various clinical activities, such as the cath lab. Teaching the courses involved a greater time commitment, and running the program takes about 15–20% of time per year. Although the program became more self‐sustaining over time, continued involvement of the Directors is required, particularly as the curriculum is ever evolving rather than stagnant.
The plan from the start was to add additional clinical tracks, once the CV track was well‐established. In 2008, we began offering one cancer course and in 2009 we added a full cancer track. The curriculum begins with an intensive, 5‐week summer institute that provides immersion in the clinical environment, but leaves some time free each week for laboratory work. The summer was chosen to avoid scheduling conflicts with regular graduate coursework. Table 1 provides an overview of the curriculum and Table 2 shows the details of training for the intensive Summer Institute.
Table 1.
Overview of the curriculum for the year
| June–August | Kickoff event |
|---|---|
| Intensive Summer Institute for 5 weeks scholar have one free day each week for lab (thesis) work, depending on rotations | |
| Fall quarter | Directed reading of the literature |
| Grant writing course | |
| Learning groups meet monthly (1 hour) | |
| Patient management conference (2 hours) | |
| Group trip to local scientific conference (optional) | |
| Winter quarter | Molecular mechanisms of disease |
| Learning groups meet monthly (1 hour) | |
| Patient Management Conference (2 hours) | |
| Spring quarter | Team science course |
| Learning groups meet monthly (1 hour) | |
| Patient Management Conference (2 hours) | |
| Day trip to local biotechnology companies, such as Genentech (optional) | |
| Wrap‐up event |
Table 2.
Summarizes Summer Institute Curriculum
| Monday | Tuesday | Wednesday | Thursday | Friday |
|---|---|---|---|---|
| Cardiothoracic OR 2 students 6:45–11 a.m. | Introduction to clinical research 8–10 a.m. | Center for virtual care 9–11:15 a.m. | ||
| Cath Lab 2 students 9 a.m.–noon | Intro to anatomy, pathology, and pathophysiology 10–11:30 a.m. | Directed reading of the literature 11 a.m.–noon | ||
| Program integration lunch noon–2 p.m. | ||||
| Echo Lab 1–4 p.m. 2 students | Hot topics in translational research 2–4 p.m. | |||
| Emergency room 2 students 4–10 p.m. | Heart failure clinic 2–5 p.m. 2 students | Emergency room 2 students 4–10 p.m. |
Each student would do one or two rotations (cardiothoracic OR, ER, cath lab, etc.) in a week. All rotations are completed over a 5‐week period. Every student has one free day per week, if possible, to allow lab work on thesis project. Shaded boxes are classes and other activities attended by all students. Students also have one class each on EKGs, cardiac imaging, and HIPAA regulations. Flexibility is key, as sometimes there is overlap in timing of rotations and classes.
Summer Institute Coursework
CV. anatomy, physiology, and pathophysiology
We needed to give the students an understanding of how the body works so that they would have a foundation on which to understand disease. The overall approach of our program is to give the students enough information to understand how the body functions, but not to convert them to medical students. A single faculty member teaches this course three times a week, and in later sessions the students are taken to the clinical simulator to see the effect of changes in cardiac function on physiologic parameters.
Directed reading of the literature
Recognizing the need for a forum to provide examples of translational research, training in critical thinking, and in‐depth discussion of translational research studies, a weekly Directed Reading of the Literature course was created. Directed Reading selects high‐quality papers on translational biomedical research targeted to the scientific interests of the students, who present in rotating pairs. Directed Reading is geared to scholars’ own backgrounds, but demonstrates how their research could be extended to translational questions. Scientific articles are selected to pique student interest to create a direct link between their ongoing research and unsolved problems or needs for care improvement. At the same time, Directed Reading exposes scholars to topical issues and controversies in interdisciplinary translational research, with an emphasis on a critical assessment of the biomedical and health sciences literature. For example, a student whose thesis was on bone formation worked with another student to present a paper on calcification of the coronary arteries and the role of Msx2 and Wnt signaling. Another student whose basic research was focused on yeast mitochondria presented a paper with a therapeutic bent, the cardiotoxicity of Imatinib (Gleevec), a new designer chemotherapy that targets the Bcr‐Abl protein in chronic myelogenous leukemia. Unexpectedly, Gleevec caused congestive heart failure in a number of patients. The paper investigated mechanisms of toxicity, where the mitochondrion has a central role. Thus, the student experienced first‐hand how her research in mitochondrial abnormalities is directly related to life‐threatening disease in humans. This course reinforces that the students can do excellent science that has translational application. This course is repeated in the fall to reinforce the concept.
Clinical rotations
Clinical rotations are one time experiences lasting several hours to sometimes all night for the ER rotation. The students go in pairs to the rotations so that they have a buddy with whom to discuss the experience. Students rotate in the cardiac catheterization laboratory, the echocardiography laboratory, heart failure clinic, the electrophysiology laboratory, a night in the emergency room, and the cardiothoracic operating room. In each venue, experienced clinical faculty explains the clinical environment, problems, and challenges. These clinical experiences expose scholars, who are used to the controlled environment of the lab, to the unpredictability of the clinical setting. They also provide opportunities for students and clinical faculty to discuss areas where basic science and clinical medicine intersect, such as where new instruments or new understanding could be beneficial.
Hot topics in translational research
It is a seminar that brings together basic scientists and clinicians who serve as role models for multidisciplinary collaborative research. Three different investigators in basic, translational, and clinical research with interwoven and complementary areas of work discuss their research programs as well as the cutting edge areas in their fields. Each investigator gives an initial 20‐minute presentation on his or her work to facilitate discussion and interaction among the faculty and the scholars. The forum helps to bring the scholars full circle from clinical experiences to the bench and back to clinical practice again. These sessions have led to new collaborations both among the faculty and students. For example, an interventional cardiologist, who had never performed research, is now working with stem cell biologists to deliver stem cells to patients with myocardial infarction.
Weekly wrap‐up
The scholars have many new experiences, particularly in the clinical rotations, and every Friday the faculty and students meet for lunch to discuss their experiences over the week and to discuss ties between the students’ basic research and clinical problems. This weekly discussion is important because students will sometimes see things that are disturbing or that prompt discussion. For example, occasionally a patient will die, particularly in the ER, and discussion of this is important.
Curriculum in Fall, Winter, and Spring Quarters
Translational learning groups
These groups, comprised of four students, their principal investigators and both clinical and basic science faculty meet monthly throughout the year beginning in the fall. In an informal setting, the groups discuss and emphasize translational research, foster new faculty/student interactions and give each student an opportunity to present their own research to an audience of both clinical and basic research mentors. These sessions reinforce translational ideas and approaches and provide the students with a group of mentors.
Patient management conferences
Students are also exposed to clinical problems and critical thinking through quarterly patient management conferences, in which expert clinicians describe real medical cases and challenge the scholars to explore how their scientific work could potentially inform the care or treatment of patients.
Directed reading
It is repeated in the fall quarter to reinforce translational thinking.
Molecular mechanisms of disease
It is a course conducted in the winter quarter, provides a capstone event in the students’ training. The objective of this intensive course is to encourage the scholars to independently design translational research projects. In a series of seminars, the students are introduced to research on heart failure and are challenged to design a project that applies their science to a cardiac problem. Student pairs present their projects receiving expert clinical feedback. For example, one pair developed a robotic arm using hydrogel to augment contraction in vivo to treat heart failure. The pairs then write a 5–10 page grant proposal, which is critiqued by the faculty for their ability to apply their own basic research to a medical problem.
Team science course
It provides an interactive learning experience to build skills required to participate effectively in multidisciplinary research teams. The course brings HHMI‐IMBS scholars together with students in related training programs and includes case‐based learning from real life scenarios in academia, aviation safety, and earthquake survival, and engages scholars in discussions that challenge perceptions and build teamwork skills. This provides further training in a critical competency for translational science, the ability to work in diverse interdisciplinary teams, the program also provides an innovative teamwork training experience.
An important element of the program is to actively engage physicians, who do basic research and see patients, as key mentors/facilitators. Because they have experience in “both camps,” they serve as models and provide resources for students, bringing both clinical medicine and basic science together for the scholars.
In sum, the training program design combines direct clinical experiences, courses, and seminars that introduce scholars to active translational researchers, the culture and language of clinical medicine, and the skills necessary to collaborate and succeed as future translational scientists.
Costs
The program supported 50% of the costs for fees and stipends for the students for the year. Other costs included the optional group trip to a local conference and the weekly lunches during the Summer Institute.
Program Outcomes
The HHMI‐IMBS program employs a rigorous comprehensive evaluation for both continuous quality improvement and outcomes assessment. An experienced evaluation team (JAR, SH) uses a mixed‐methods approach to collect both qualitative data derived from interviews and focus groups as well as quantitative data from annual surveys, program documents, and public sources. The evaluation activities and data collection were approved by the UC Davis Institutional Review Board since 2006. The HHMI‐IMBS scholars complete the Annual Survey of Scholars upon entering the program and then annually for 5 years. The Annual Survey of Scholars combines closed‐ and open‐ended questions to measure research productivity and collaborations (e.g., abstracts, proposals, grants submitted and received, publications, poster and oral presentations, and patent applications), attitudes and career goals, and career path information. Data from the surveys are collected by Survey Monkey and analyzed using SAS version 9.3.* Open‐ended questions from the surveys and facilitator notes from quarterly student feedback sessions are reviewed, summarized, and presented to the program directors quarterly for discussion and program improvement.
Comparison students
In 2006 and 2007, a group of predoctoral students from the same program year and academic disciplines as the initial 2 cohorts of HHMI‐IMBS scholars (n = 15 students) were invited to complete the Annual Survey of Scholars. To recruit the comparison students, department chairs agreed to send an e‐mail to their doctoral students asking them to contact the HHMI‐IMBS program evaluator if they were interested in answering an IRB‐approved annual survey about their graduate careers and interests. Students who responded and were from the same graduate groups with a comparable date of enrollment as the HHMI‐IMBS scholars were eligible. Interested students provided background information on their gender, graduate (UC Davis) GPA, date of enrollment and expected date of graduation. To keep the past academic records of the two groups equivalent, interested students with less than a 3.4 GPA (minimum GPA for the HHMI cohort) were not selected for the comparison group. Comparison students receive a $20 gift card after completing their annual survey. There are 25 comparison students who have completed the survey annually for 5 years (2006–2010). Characteristic of the comparison students are shown in Table 3.†
Table 3.
HHMI‐IMBS scholars and comparison group matching characteristics
| Characteristics | Comparison students | HHMI‐IMBS scholars 2006–2007 |
|---|---|---|
| Scholars | 25 | 15 |
| Female | 14 (56.0%) | 10 (66.7%) |
| Doctoral program enrollment year | ||
| 2003–2004 | 28 (100.0%) | 15 (100.0%) |
| Expected graduation year | ||
| 2008 | 13 (52.0%) | 8 (53.3%) |
| 2009 | 12 (48.0%) | 7 (46.7%) |
| Discipline 1 | ||
| Engineering/biomedical engineering | 9 (36.0%) | 4 (26.7%) |
| Life sciences/biological or biomedical | 15 (60.0%) | 9 (60.0%) |
| Physical sciences/chemistry | 1 (4.0%) | 2 (13.3%) |
The disciplines of students were coded using the area classifications of the Survey of Earned Doctorates, NORC, University of Chicago.
Since programs designed to train predoctoral researchers cannot observe important long‐term outcomes, such as obtaining independent research funding, until many years after a trainee has completed the program, we describe some early indications of program success, such as scholar self‐efficacy for conducting research, attitudes about interdisciplinary research, and early career publication counts.6, 7 Statistical tests were performed on changes in mean scores on measures of the 5 research self‐efficacy items and 6 career attitude items included in the Annual Survey of Scholars. Comparisons were made for (a) mean change from program entry to the end of the HHMI‐IMBS program year among all 5 cohorts of HHMI‐IMBS scholars (N = 39), and (b) differences in mean scores at program entry and end of 1 year among comparison students (N = 25) versus the HHMI‐IMBS scholars (N = 15) from the first 2 program cohorts. These differences in group means were assessed using t‐tests. The p‐values for these statistical tests are shown in Tables 4, 5, 6, 7.
Table 4.
Self‐efficacy items, program entry and program end, HHMI‐IMBS scholars 2006–2010 (N = 39)
| Self‐efficacy items (1=strongly disagree to 5=strongly agree) | HHMI‐IMBS scholars program entry mean (SD) | HHMI‐IMBS scholars program end mean (SD) | p‐value1 |
|---|---|---|---|
| I am confident in my ability to translate scientific information to nonscientists | 4.03 (0.74) | 4.38 (0.59) | 0.0236 |
| I would like to acquire the skills and knowledge necessary to recognize clinical problems that can be approached scientifically | 4.82 (0.39) | 4.74 (0.44) | 0.3982 |
| I have enough training now to plan and execute scientific studies that help solve a clinical problem | 2.56 (0.79) | 3.67 (0.83) | <0.0001 |
| I am comfortable working in a mixed group of scientists and clinicians | 4.23 (0.78) | 4.51 (0.56) | 0.0725 |
| Given my research interests, I am likely to produce work that will someday improve human health | 4.46 (0.72) | 4.54 (0.56) | 0.5855 |
p‐value (two‐tailed) for t‐test comparing group means, HHMI Scholars Program Entry versus Program End.
Table 5.
Self‐efficacy items, program entry and program end, HHMI‐IMBS scholars 2006–2007 (N=15) and comparison students 2006–2007 (N=25)
| HHMI‐IMBS scholars 2006—2007 | HHMI‐IMBS scholars 2006–2007 | Comparison students 2006–2007 | Comparison students 2006–2007 | |||
|---|---|---|---|---|---|---|
| Program entry | Program end | Entry year | Year end | |||
| Self‐efficacy items (1=strongly disagree to 5=strongly agree) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | p‐value, Entry1 | p‐value, End2 |
| I am confident in my ability to translate scientific information to nonscientists | 4.33 (0.72) | 4.53 (0.51) | 3.92 (0.70) | 4.20 (0.58) | 0.0840 | 0.0767 |
| I would like to acquire the skills and knowledge necessary to recognize clinical problems that can be approached scientifically | 4.87 (0.35) | 4.80 (0.41) | 3.68 (0.95) | 3.72 (0.84) | <0.0001 | <0.0001 |
| I have enough training now to plan and execute scientific studies that help solve a clinical problem | 2.67 (0.96) | 3.73 (0.80) | 2.08 (0.95) | 2.76 (0.97) | 0.0658 | 0.0024 |
| I am comfortable working in a mixed group of scientists and clinicians | 4.67 (0.62) | 4.73 (0.46) | 4.04 (0.73) | 4.16 (0.69) | 0.0082 | 0.0073 |
| Given my research interests, I am likely to produce work that will someday improve human health | 4.73 (0.60) | 4.73 (0.60) | 3.96 0.98 | 3.96 (0.93) | 0.0093 | 0.0068 |
p‐value (two‐tailed) for t‐test comparing group means, HHMI Scholars versus Comparison Students, Program Entry/Entry Year.
p‐value (two‐tailed) for t‐test comparing group means, HHMI Scholars versus Comparison Students, Program End/Year End.
Table 6.
Attitude items, program entry and program end, HHMI‐IMBS scholars 2006–2010 (N = 39)
| Attitude items (1=strongly disagree to 5=strongly agree) | HHMI‐IMBS scholars program entry mean (SD) | HHMI‐IMBS scholars program end mean (SD) | p‐value1 |
|---|---|---|---|
| It is important that my lifetime of work helps bridge the gaps between basic science and clinical medicine | 4.56 (0.68) | 4.56 (0.60) | 0.4931 |
| Someone with graduate training in both basic science and clinical medicine has more promising career opportunities | 4.49 (0.72) | 4.41 (0.85) | 0.6551 |
| The number of basic scientists being cross‐trained in clinical medicine needs to increase | 4.35 (0.62) | 4.59 (0.55) | 0.0745 |
| It does not really matter to me whether my research has applicability to human beings | 1.31 (0.73) | 1.28 (0.51) | 0.8339 |
| Breakthroughs in basic science rarely translate into improvements in public health | 3.03 (1.09) | 2.76 (1.18) | 0.2972 |
| A successful researcher is one who can collaborate with scientists in other fields | 4.33 (0.74) | 4.54 (0.55) | 0.1403 |
p‐value (two‐tailed) for t‐test comparing group means, HHMI Scholars Program Entry versus Program End.
Table 7.
Attitude items, program entry and program end, HHMI‐IMBS scholars 2006–2007 (N=15) and comparison students 2006–2007 (N = 25)
| Attitude items (1=strongly disagree to 5=strongly agree) | HHMI‐IMBS scholars 2006–2007 program entry mean (SD) | HHMI‐IMBS scholars 2006–2007 program end mean (SD) | Comparison students 2006–2007 entry year mean (SD) | Comparison students 2006–2007 year end mean (SD) | p‐value, entry1 | p‐value, end2 |
|---|---|---|---|---|---|---|
| It is important that my lifetime of work helps bridge the gaps between basic science and clinical medicine | 4.73 (0.46) | 4.80 (0.41) | 3.64 (1.08) | 3.68 (0.75) | 0.0007 | <0.0001 |
| Someone with graduate training in both basic science and clinical medicine has more promising career opportunities | 4.40 (0.91) | 4.33 (0.98) | 3.76 (0.93) | 3.80 (0.87) | 0.0403 | 0.0832 |
| The number of basic scientists being cross‐trained in clinical medicine needs to increase | 4.40 (0.63) | 4.40 (0.63) | 3.72 (0.98) | 3.68 (0.85) | 0.0214 | 0.0072 |
| It does not really matter to me whether my research has applicability to human beings | 1.53 (1.06) | 1.27 (0.59) | 1.92 (1.00) | 2.16 (1.21) | 0.2501 | .0015 |
| Breakthroughs in basic science rarely translate into improvements in public health | 3.13 (1.12) | 2.73 (1.09) | 2.44 1.12 | 2.64 (1.08) | 0.0669 | .8006 |
| A successful researcher is one who can collaborate with scientists in other fields | 4.53 (0.64) | 4.73 (0.46) | 4.12 0.67 | 4.32 (0.63) | 0.0644 | .0347 |
p‐value (two‐tailed) for t‐test comparing group means, HHMI scholars versus comparison students, program entry/entry year.
p‐value (two‐tailed) for t‐test comparing group means, HHMI scholars versus comparison students, program end/year end.
Changes in Self‐Efficacy and Attitudes
Participation in a clinical research training program has been found to be associated with research self‐efficacy.7, 8 For example both predoctoral and postdoctoral scholars in a Clinical and Translational Science Award affiliated research training program reported increased skills and confidence in their ability to perform clinical research‐related tasks, such as study design, data analysis and interpreting, reporting or presenting research results.9 To look at the program's impact on research self‐efficacy and attitudes, we analyzed responses on the Annual Scholar Survey among the 5 cohorts of HHMI‐IMBS to see if confidence and interest to conduct translational research increased at the end of their program year. We also compared changes in the HHMI 2006–2007 students’ attitudes to those of the comparison students.
Self‐efficacy
Among the HHMI‐IMBS scholars, there were some notable changes in self‐efficacy from entry to the end of the program year. We compared the mean responses of all cohorts HHMI scholars combined (N = 39) at program entry and program exit using t‐tests (Table 4). At the end of their program year, HHMI‐IMBS scholars reported more confidence in their “ability to translate scientific information to nonscientists” (p < 0.03) and were more likely to say they “have enough training now to plan and execute scientific studies that help solve a clinical problem” (p < 0.001). Although not statistically significant, the scholars said they were also more “comfortable working in a mixed group of scientists and clinicians” at the end of the HHMI‐IMBS year (p < 0.08).
Table 5 compares the reported self‐efficacy of the 2006–2007 HHMI‐IMBS students (N = 15) to the comparison students (N = 25). The HHMI‐IMBS scholars report responses that indicate greater self‐efficacy at the beginning of their program year. While both the HHMI‐IMBS scholars and comparisons students report increased self‐efficacy at the end of the year, HHMI‐IMBS scholars report significantly higher efficacy than the comparison students at year end for 4 of the 5 efficacy items.
Career attitudes
The HHMI‐IMBS students have generally very positive attitudes toward their training (Table 6). Although there are no significant differences between the preprogram and year‐end attitudes, the majority of scholars in all cohorts strongly agreed that it is “important to me that my lifetime of work helps bridge the gap between basic science and clinical medicine” and that “A successful researcher is one who can collaborate with scientist in fields other than their own.” Scholars also were likely to agree that the “number of basic scientist being cross‐trained in clinical medicine needs to increase.”
Table 7 compares the attitudes of 2006–2007 HHMI‐IMBS students (N = 15) to the comparison students (N = 25). The HHMI‐IMBS scholars differ from their counterparts in the comparison group at the beginning of their program year in terms of how important it is to them that their “lifetime of work helps bridge the gaps between basic science and clinical medicine,” whether they believe “someone with graduate training in both basic science and clinical medicine has more promising career opportunities,” and whether the “number of basic scientists being cross‐trained in clinical medicine needs to increase.” At the end of the program year, the HHMI‐IMBS scholars are significantly more likely to say that it is important that their work “bridge the gap between basic science and clinical medicine” and that “the number of basic scientist being cross trained in clinical medicine needs to increase.” And the HHMI‐IMBS scholars disagree more with the statement that “It does not really matter to me whether my research has applicability to human beings.”
Research Interests and Career Goals
HHMI‐IMBS scholars report great interest in pursuing research at the interface of basic science and clinical medicine. The annual survey data indicates that at the end of the HHMI‐IMBS experience, the scholars have career goals that continue to be oriented toward basic science research, but with an added translational focus. At the end of the training year, 86% of the HHMI‐IMBS 2006–2007 students reported that they were very interested in an academic position involving translational. A majority (52%) of HHMI‐IMBS students say they are interested in teaching in a medical school environment.
Students credit the connections they established in the HHMI‐IMBS program with the direction and success of their work. A year after completion of the program, all scholars said the program had helped them meet people at UC Davis and elsewhere who were instrumental in their careers; half indicated that the program had provided them with direct opportunities for authorship on publications. In addition, program scholars’ report that their research and theses became more translational in focus with high potential clinical relevance as a result of the program. Several scholars said that their projects had been changed in some way to make it more focused on a specific clinically relevant medical problem. For instance, one 2009 scholar wrote:
I think the HHMI‐IMBS program has gone a long way in shaping me as a striving academician and making my project more translational. My PI has mentioned to me on multiple occasions how he thinks I have really matured over the course of the program with respect to my experimental designs, confidence in discussing ideas, and presentation skills. In addition, I have been able to shape my project from shooting for an idealized goal to something that is more realistically attainable, more likely to be successful, and more relevant to clinical applications.
Comments from alumni scholars suggest that this shift has a lasting impact on their work.
Becoming familiar with speaking with clinicians, being in a clinical setting, and observing first hand patient/doctor interactions and clinician responses to patient/doctor interactions really gave me confidence that the clinical world is not as daunting as it seems. This also helped me see [how] to implement my ideas for improving technologies for health care.
Peer‐Review Publications
Although the scholars are early in their careers, we examined the publication records of the HHMI‐IMBS scholars to see if they differ from their counterparts in the comparison group. Students reported their publications in the annual survey and these were independently verified by searching PubMed and Web of Science. A comparison of the initial HHMI‐IMBS cohorts with the comparison students at 5 time points (entry year, end of program year, and at postprogram years 2–3) indicates that the HHMI‐IMBS students differ from their comparisons (Figure 1). As shown in the figure below, the HHMI‐IMBS students have slightly more published manuscripts at program entry than the comparison students reflecting the program's selection of students who are somewhat more accomplished. The HHMI‐IMBS scholars continue to maintain their publication pace after leaving the program.
Figure 1.
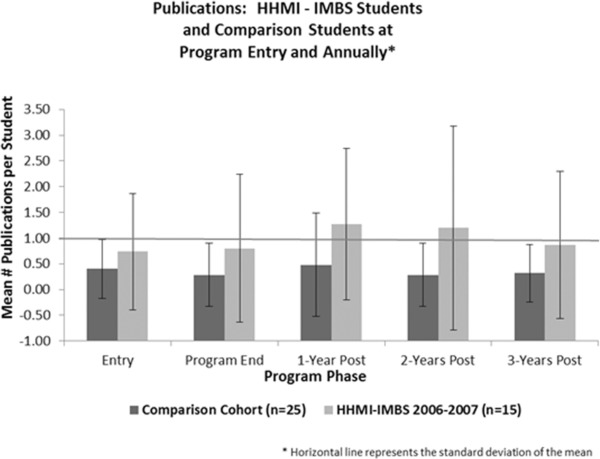
Mean publications per student compared to control group
Other data support the finding that the HHMI‐IMBS students are productive during their graduate training. Scholars report approximately 3 poster or verbal presentations each versus 1 per student among the comparisons. HHMI‐IMBS scholars have received significant awards for their achievements, scholarships and prizes; two received NSF Graduate Research Fellowships; one received the outstanding graduate student teaching award; and one received the distinguished oral presentation award at the UC system‐wide bioengineering symposium.
Building Collaborations
Annual survey data also show that connections made by the basic science and engineering students in the HHMI‐IMBS program have led to collaborations with clinicians. Among the initial cohorts, the HHMI‐IMBS scholar's network contained more clinical collaborators on publications and presentations at the end of the HHMI‐IMBS year than the comparison students (14% vs. 1%). One year after the program, MD collaborators for HHMI‐IMBS scholars had increased to 40%. Findings from focus groups with students confirmed that students took advantage of program sponsored opportunities to network. All of the scholars said their opportunities to meet and collaborate with clinicians, especially during the patient management conferences and learning groups, were “valuable” or “extremely valuable.” Comments from HHMI‐IMBS scholars in quarterly evaluation focus groups illustrate these results. For example, one scholar reported:
“I think the most influential experience was getting to talk with the clinicians and hear how they solve problems in the hospital. It made it clear that there is a gap between the scientific realm and the clinical realm that must be connected to achieve better therapies and treatments.”
A second scholar noted,
“I received a lot of helpful feedback about my project from the other students and faculty, especially the clinicians. The feedback helped me to think about aspects of my project I had not previously considered.”
Discussion
The UC Davis HHMI‐IMBS program has been effective in recruiting and training translational researchers. The didactic and clinical experiences have improved the skills and confidence of students, increased the number of translational research successes of scholars, and provided opportunities for translational research collaboration. The HHMI‐IMBS program scholars are more productive during and after the HHMI‐IMBS year and have more research products than their counterparts in a comparison student group. Furthermore, the HHMI‐IMBS scholars complete their training with a greater understanding of and commitment to translational research, a more diverse research network, and increased clinical collaborations than a comparison group. These findings contradict the notion that participating in an intensive program such as HHMI‐IMBS would slow down scholars’ achievements. In fact, all students in the HHMI‐IMBS program reported that they had progressed as expected in their regular graduate program during the HHMI‐IMBS year.
Expansion and Sustainability
The early success of the HHMI‐IMBS program has led directly to an integration of its elements and values into new key programs, such as the translational research training provided by the Clinical and Translational Science Center (CTSC). A natural progression was to engage the many relevant T32 training programs already in existence at UC Davis, creating a mechanism for sustainability that also enhances the T32 training experiences. Investment in the IMBS program and its early success has led to an expanded number of training tracks. In addition to the initial focus on CV medicine, HHMI‐IMBS now includes a cancer biology track and a neuroscience track is scheduled to be added in the coming year.
Limitations of Study
It was not feasible to perform a randomized trial given the nature of the training program. Instead volunteer control graduate students were recruited as discussed, and it was not possible to identify matched controls for the scholars. Thus, the control students were similar to the trainees, but differed some at the start of the training program (Tables 3, 4, and 5 compare controls with the scholars).
Institutional Culture
The translational research training success through IMBS has had direct impact on the institutional culture at UC Davis. The institution's top leaders—including deans, department chairs, and program directors from both clinical medicine and basic science—are fully supportive of an integrated, sustainable translational research program. A strong cross‐disciplinary team of mentors and collaborators, including volunteer front‐line faculty, current students from diverse backgrounds who share training experiences, and graduates of the HHMI‐IMBS program continue to be engaged participants. This arrangement has been mutually beneficial, allowing the program to play a role in identifying and disseminating best practices throughout the institution and nationally. Moreover, the ethos of the HHMI‐IMBS training program has permeated the graduate studies culture at UC Davis through the creation of degrees and certificates for translational research. There are three degrees offered to doctoral candidates that provide multiple credits for a specialized program in translational research: (1) Masters of Advanced Studies in Clinical Research; (2) Designated Emphasis in Translational Research (DETR); and (3) Certificate in Translational Research. Students participating in the HHMI‐IMBS program may pursue any of these, with most electing to earn the Designated Emphasis in Translational Research or the newer Certificate Program in Translational Research. The HHMI‐IMBS has served as the cornerstone for this institutional change in how basic scientists are trained and how translational research may evolve.
Acknowledgments
Disclosure of Funding
HHMI Med‐Into‐Grad Initiative Grant 56006769.
National Center for Research Resources UL1RR024146.
Footnotes
*Data analysis for this paper was generated using SAS/STAT software, Version 9.3 of the SAS System for Windows, Copyright©2002–2010, SAS Institute Inc. SAS and all other SAS Institute Inc. product or service names are registered trademarks or trademarks of SAS Institute Inc., Cary, NC, USA.
†Although the HHMI‐IMBS program has matriculated cohorts of students since 2006, the comparison students, who were selected in 2007, are comparable to only the first two HHMI‐IMBS cohorts (2006 and 2007 matriculants). We lacked sufficient resources to select a unique comparison group for each cohort, thus have followed just this one group for the past 5 years.
References
- 1. Keramaris NC, Kanakaris NK, Tzioupis C, Kontakis G, Giannoudis PV. Translational research: from benchside to bedside. Injury 2008; 39: 643–650. [DOI] [PubMed] [Google Scholar]
- 2. Hartmann KE, Heitman E, Brown NJ. Training basic, clinical and translational investigators In: Robertson D. and Williams GH, eds. Clinical and Translational Science: Principles of Human Research. San Diego, CA: Academic Press; 2009: 191–200. [Google Scholar]
- 3. Meyers FJ. Recombinant innovation and translational science trainees. Sci Trans Med. 2010; 2: 39ed5. [DOI] [PubMed] [Google Scholar]
- 4. Rubio DM, Schoenbaum EE, Lee LS, Schteingart DE, Marantz PR, Anderson KE, Platt LD, Baez A, Esposito K. Defining translational research: implications for training. Acad Med. 2010; 85: 470–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Heller C, de Melo‐Martin I. Clinical and Translational Science Awards: can they increase the efficiency and speed of clinical and translational research? Acad Med. 2009; 84: 424–432. [DOI] [PubMed] [Google Scholar]
- 6. Rosenblum, D , Alving, B . The role of clinical and translational science awards program in improving the quality and efficiency of clinical research. Chest 2011; 140: 764–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fang D, Meyer RE. Effect of two Howard Hughes Medical Institute research training programs for medical students on the likelihood of pursuing research careers. Acad Med. 2003; 78: 1271–1280. [DOI] [PubMed] [Google Scholar]
- 8. Zier K, Friedman E, Smith L. Supportive programs increase medical students’ research interest and productivity. J Invest Med. 2006; 54: 201–207. [DOI] [PubMed] [Google Scholar]
- 9. Lipira L, Jeffe DB, Krauss M, Garbutt J, Piccirillo J, Evanoff B, Fraser V. Evaluation of clinical research training programs using the clinical research appraisal inventory. Clin Trans Sci. 2010; 3: 243–248. [DOI] [PMC free article] [PubMed] [Google Scholar]


