Abstract
Background
Reducing hospital readmission rates is a national priority; however, evidence about hospital strategies that are associated with lower readmission rates is limited. We sought to identify hospital strategies that were associated with lower readmission rates for patients with heart failure.
Methods and Results
Using data from a Web-based survey of hospitals participating in national quality initiatives to reduce readmission (N=599; 91% response rate) during 2010–2011, we constructed a multivariable linear regression model, weighted by hospital volume, to determine strategies independently associated with risk-standardized 30-day readmission rate (RSRR) adjusted for hospital teaching status, geographic location, and number of staffed beds. Strategies that were associated with lower hospital RSRR included: 1) partnering with community physicians or physician groups to reduce readmission (0.33 percentage point lower RSRR, P-value = 0.017), 2) partnering with local hospitals to reduce readmissions (0.34 percentage point, P-value = 0.020), 3) having nurses responsible for medication reconciliation (0.18 percentage point, P-value = 0.002), 4) arranging follow-up appointments before discharge (0.19 percentage point, P-value = 0.037), 5) having a process in place to send all discharge paper or electronic summaries directly to the patient's primary physician (0.21 percentage point, P-value = 0.004), and 6) assigning staff to follow up on test results that return after the patient is discharged (0.26 percentage point, P-value =0.049). Although statistically significant, the magnitude of the effects was modest with individual strategies associated with less than half a percentage point reduction in RSRR; however, hospitals that implemented more strategies had significantly lower RSRRs (reduction of 0.34 percentage point for each additional strategy).
Conclusions
Several strategies were associated with lower hospital RSRR for patients with heart failure.
Keywords: Heart failure, readmissions, quality
Reducing hospital readmission rates is a national priority. Approximately 20% of Medicare beneficiaries are readmitted within 30 days of discharge, and these readmissions have been estimated to cost the American public more than $15 billion per year.1 The National Quality Forum has endorsed hospital risk-standardized readmission rates (RSRR) as performance measures, and the Centers for Medicare & Medicaid Services publicly report these rates. The Patient Protection Affordable Care Act of 2010 has created new incentives to reduce readmissions using the publicly reported measures, as hospitals with high readmission rates can lose up to 3 percent of their Medicare reimbursement by 2015. In response, dozens of national, state-based, and local quality campaigns and collaboratives have emerged to help hospitals reduce readmissions.
Evidence about how best to reduce readmissions is nonetheless limited. Several randomized trials2–12 have reported discharge and follow-up interventions that reduced readmissions, but less is known about the effectiveness of these strategies outside the context of a controlled trial. Observational studies of heart failure have examined a limited set of strategies, such as physician follow up after discharge and nurse staffing,13–17 or evaluated more strategies but with small sample sizes of 100 or fewer hospitals.8, 18–24 We previously documented substantial variation in strategies implemented by hospitals to reduce readmissions,25 but there remains a need to determine how these strategies are related to hospital RSRRs.
Accordingly, we linked survey data about hospitals' strategies with their RSRRs to determine which hospital strategies are associated with lower readmission rates in a large, national sample of hospitals. We focused on patients with heart failure due to the higher readmission rates for this group26 and their inclusion in the national incentive program. Findings from this study may provide needed knowledge about effective strategies to reduce readmissions and improve quality of care. These methods employ an approach that is similar to those used for investigating the strategies associated with faster door-to-balloon times27 for patients with an ST-segment elevation myocardial infarction.
Methods
Study Design and Sample
We conducted a cross-sectional study using a Web-based survey of hospitals to examine their reported use of specific hospital strategies intended to reduce readmissions for patients with heart failure. We contacted all hospitals that enrolled in either of two national quality initiatives to reduce readmission (i.e., the H2H (Hospital to Home) National Quality Improvement Initiative28 or STAAR, the State Action on Avoidable Rehospitalizations Initiative29) by July 1, 2010 (n=658); surveys were competed between November 2010 – May 2011, as previously described.25 Of these 658 hospitals, 599 completed the survey for a response rate of 91.0%; 532 were hospitals enrolled in H2H, 55 were hospitals enrolled in STAAR, and 12 were hospitals enrolled in both H2H and STAAR. We invited hospital participation by contacting the person registered with H2H or STAAR. Respondents were asked to coordinate with other relevant staff to complete the survey. Respondents reported various roles in the hospital, and many reported having more than one role; nearly 60% were from quality management departments, 25% were from other clinical departments, 24% were from cardiology departments, 17% were from case management or care coordination, and 8% reported working in non-clinical roles. We obtained Internal Review Board exemption (protocol number 1008007300) for our study which waived the need for participant consent because no identifying participant information was obtained. Additionally, all participants were provided with an information sheet to let them know what information would be collected, how it would be used and disseminated, and any risks that would be encountered by participation.
Survey development
We developed the hospital survey by compiling items based on recommended strategies to reduce readmissions promulgated by quality initiatives including H2H, STAAR, and Better Outcomes for Older adults through Safe Transitions (BOOST) campaigns and collaboratives, existing literature,21 and clinical experience. We pre-tested the survey for its comprehensibility and comprehensiveness with 5 professional colleagues in roles similar to intended respondents and revised or excluded items that were ambiguous or imprecise. We then contacted the individual registered as the primary contact for the H2H or STAAR initiative to inform them of the purpose of the study and request participation. We instructed the individual to seek input from clinical and administrative staff to coordinate a single hospital response to the items, which were entered electronically and transmitted to a database for analysis.
Measures
Survey items were all closed-ended and included approximately 30 hospital strategies, which we organized in 3 conceptual domains (See Appendix for full questionnaire). These domains were: 1) quality improvement efforts and performance monitoring (e.g., presence of a quality improvement team, partnering with community-based agencies to reduce readmission); 2) medication management (e.g., how the medical reconciliation practice is conducted, use of the teach-back techniques); and 3) discharge and follow up procedures (e.g., timing of follow-up appointments, home visits). We used principal components factor analysis to investigate potential approaches to summarizing the use of strategies and found evidence to support the existence of only 1 factor. Therefore we created a summary count score (possible range 0–10) by assigning a 1 to every strategy implemented that was positively associated with RSRR and by assigning a 1 to every strategy not implemented that was negatively associated with RSRR. All items with 4-point responses for describing the frequency with which a strategy was implemented were dichotomized (1= usually or always; 0= sometimes or never).
We attained data from the Annual Survey of the American Hospital Association (AHA) from 2009 for hospital characteristics including number of staffed hospital beds, teaching status (member of the Council of Teaching Hospitals and Health Systems (COTH),30 which is an association of approximately 400 major teaching hospitals; having a residency program only but not a member of COTH; and non-teaching), multihospital affiliation (yes or no) and ownership (for-profit, nonprofit, or government). We determined census regions from the U.S. Census Bureau, and we ascertained the urban, suburban, or rural location designation using the 2003 Urban Influence Codes.31 We ascertained participation in H2H, STAAR, or both initiatives from the enrollment records of each initiative.
Our outcome was hospital 30-day risk-standardized readmission rate (RSRR), derived using the same methods as used by CMS for public reporting of 30-day RSRR,32, 33 applied to the most recent year of Medicare data available (July 2010 to June 2011).
Data analysis
We first generated means and frequencies to describe the sample of hospitals and the prevalence of each hospital practice. We also generated RSRR means and standard errors, weighted by hospital volume, for each level of our explanatory variables. We examined associations between hospital characteristics and RSRR. Prior to multivariable analyses, we assessed candidate independent variables for possible multicollinearity and found that no two variables were over-correlated (all correlation coefficients < 0.45). We constructed a weighted multivariate linear regression model using backwards elimination, where we removed, one by one, non-significant explanatory variables (p values > 0.05), adjusted for hospital teaching status, geographic location, and number of staffed beds. The removal of variables did not significantly affect the fitting of the model. We also fit a similar multivariable model using the summary count score of selected strategies implemented. In exploratory analysis, we also examined whether the effects of the strategies varied across subgroups identified by hospital teaching status and by number of beds, using appropriate interaction terms. Analyses excluded cases with missing values because the frequency of missing data was low (< 3%). All analyses were conducted in SAS, version 9.2 (Carey, NC). The research was funded by the Commonwealth Fund and the Center for Cardiovascular Outcomes Research at Yale University, supported by the National Heart Lung, and Blood Institute.
Results
Hospital characteristics
Of the 599 hospitals that completed the survey (91% response rate), 14 hospitals (2.3%) were missing RSRR data and excluded, resulting in a total sample size of 585 hospitals for this study. The 14 hospitals with missing data did not differ significantly from the remaining hospital in terms of number of beds, teaching status, geographical region, and rural/urban location (P-values > 0.05). Of these 585 hospitals, 571 had no missing data on any of the independent variables used for modeling. Approximately 15% of the full sample were COTH members and an additional nearly 20% had an accredited residency program (Table 1). Almost 30% had 400 beds or more, and about 85% were urban hospitals. The mean RSRR for patients with heart failure was 24.7% with a range from 20.4% to 30.1%, which is similar to the RSRR for heart failure nationally.34
Table 1.
Descriptive Characteristics of Surveyed Hospitals (N=585)
| N (%)* | RSRR†,‡ Mean (SE) |
P-value§ | |
|---|---|---|---|
| Hospital teaching status | <0.001 ‖ | ||
| Council of Teaching Hospitals member | 90 (15.4%) | 25.1 (0.15) | |
| Has accredited residency training | 114 (19.6%) | 24.4 (0.15) | |
| Nonteaching | 379 (65.0%) | 24.7 (0.08) | |
| Number of staffed beds | 0.898 | ||
| < 200 beds | 196 (33.8%) | 24.6 (0.10) | |
| 200–399 beds | 216 (37.2%) | 24.8 (0.11) | |
| 400–599 beds | 98 (16.9%) | 24.7 (0.13) | |
| 600+ beds | 70 (12.1%) | 24.7 (0.21) | |
| Census region | 0.083 | ||
| New England | 39 (6.7%) | 24.6 (0.24) | |
| Middle Atlantic | 57 (9.8%) | 25.1 (0.28) | |
| East North Central | 123 (21.1%) | 24.9 (0.13) | |
| West North Central | 45 (7.7%) | 24.5 (0.24) | |
| South Atlantic | 119 (20.5%) | 24.6 (0.13) | |
| East South Central | 51 (8.8%) | 24.9 (0.19) | |
| West South Central | 52 (8.9%) | 24.4 (0.11) | |
| Mountain | 33 (5.7%) | 24.8 (0.33) | |
| Pacific | 63 (10.8%) | 24.2 (0.16) | |
| Geographic location | 0.362 | ||
| Urban | 493 (84.7%) | 24.8 (0.07) | |
| Suburban | 59 (10.1%) | 24.7 (0.18) | |
| Rural | 30 (5.2%) | 24.2 (0.32) | |
| Ownership type | 0.631 | ||
| For-profit | 126 (21.7%) | 24.6 (0.12) | |
| Nonprofit | 401 (68.9%) | 24.7 (0.08) | |
| Government | 55 (9.5%) | 24.8 (0.21) | |
| Multihospital affiliation | 0.288 | ||
| Yes | 416 (71.5%) | 24.7 (0.07) | |
| No | 166 (28.5%) | 24.8 (0.14) | |
| Participation in quality initiative | 0.220 | ||
| H2H# only | 519 (88.7%) | 24.7 (0.07) | |
| STAAR** only | 54 (9.2%) | 25.1 (0.20) | |
| Both H2H and STAAR | 12 (2.1%) | 24.6 (0.30) | |
| Risk standardized readmission rate (RSRR) | 24.7 (1.4) | ||
| Mean (SD) | 24.6 | ||
| Median | 24.1 | ||
| Mode | 1.83 | ||
| Variance | 20.4 – 30.1 | ||
| Range |
Number missing by item ranged from 2 to 5; percents are based on valid responses
Risk-standardized readmission rate
RSRR per 100 patients, weighted by hospital volume
P-values derived from t-tests and analyses of variance as appropriate
RSRRs for nonteaching hospitals significantly different from Council of Teaching Hospitals (COTH) member hospitals (P-value=0.016) and from hospitals with an accredited residency program (P-value = 0.033); RSRRs for COTH hospitals significantly different from residency hospitals (P-value < 0.001).
Hospital to Home (H2H) Initiative
State Action on Avoidable Rehospitalizations Initiative
Associations between reported hospital strategies and RSRR
In multivariable analysis adjusted for number of staffed beds, teaching status, and census region, 6 strategies were associated with significantly lower RSRRs (Table 2). These included: 1) partnering with community physicians or physician groups to reduce readmission (0.33 percentage point lower RSRR, P-value = 0.017), 2) partnering with local hospitals to reduce readmissions (0.34 percentage point, P-value = 0.020), 3) having nurses responsible for medication reconciliation (0.18 percentage point, P-value= 0.002), 4) arranging a follow-up appointment before discharge (0.19 percentage point, P-value = 0.037), 5) having a process in place to send all discharge paper or electronic summaries directly to the patient's primary physician (0.21 percentage point, P-value = 0.004), and 6) assigning staff to follow up on test results that return after the patient is discharged (0.26 percentage point, P-value = 0.049). Many of these strategies were implemented by less than two-thirds of the hospitals (Table 3).
Table 2.
Adjusted Associations between Risk-Standardized 30-day Readmission Rates (RSRR) for Patients with Heart Failure and Hospital Strategies*(N=571)
| Percentage point change in RSRR |
P-value | |
|---|---|---|
| Hospital has partnered with community physicians or physician groups to reduce readmission rates |
−0.33 (0.14) | 0.017 |
| Hospital has partnered with other local hospitals to reduce readmission rates |
−0.34 (0.15) | 0.020 |
| Higher frequency of nurses responsible for conducting medication reconciliation at discharge1 |
−0.18 (0.06) | 0.002 |
| Greater frequency with which patients leave the hospital with an outpatient follow-up appointment already arranged1 |
−0.19 (0.09) | 0.037 |
| Greater proportion of patients for whom a paper or electronic discharge summary sent directly to the patient's primary MD2 |
−0.21 (0.07) | 0.004 |
| Someone within the hospital is assigned to follow up on test results that return after the patient is discharged |
−0.26 (0.13) | 0.049 |
| Higher frequency of outpatient and inpatient prescription records linked electronically1 |
0.18 (0.06) | 0.003 |
| All patients or their caregivers receive written emergency plan upon discharge1 |
0.38 (0.13) | 0.004 |
| Reliable process is in place to ensure outpatient physicians are alerted to the patient's discharge within 48 hours of discharge |
0.42 (0.14) | 0.003 |
| Hospital regularly calls patients after discharge to either follow up on post-discharge needs or to provide additional education1 |
0.34 (0.13) | 0.010 |
| Hospital teaching status | ||
| Council of Teaching Hospitals member | 0.61 (0.21) | 0.005 |
| Has residency training | −0.23 (0.16) | NS |
| Nonteaching | REF | --- |
| Census region | ||
| New England | −0.25 (0.29) | NS |
| Middle Atlantic | REF | --- |
| East North Central | −0.07 (0.21) | NS |
| West North Central | −0.28 (0.29) | NS |
| South Atlantic | −0.14 (0.23) | NS |
| East South Central | 0.45 (0.27) | NS |
| West South Central | −0.47 (0.29) | NS |
| Mountain | 0.02 (0.39) | NS |
| Pacific | −0.73 (0.29) | 0.013 |
| Number of staffed beds | ||
| < 200 beds | 0.29 (0.24) | NS |
| 200–399 beds | 0.52 (0.19) | 0.007 |
| 400–599 beds | 0.36 (0.19) | NS |
| 600+ beds | REF | --- |
RSRR is a percentage; model was weighted by hospital volume and independent variables were derived with backwards elimination, removing variables with p values >0.05.
Modeled as a 4-point variable (never, sometimes, usually, always); change in RSRR is for a 1-unit change in this 4-point measure.
Modeled as a 4-point variable (none, some, most, all); change in RSRR is for a 1-unit change in this 4-point measure. NS = non-significant (P-values > 0.050) Model R-squared = 16.9%
Table 3.
Hospital Use of Strategies to Reduce Readmissions (N=571)
| N (%) | |
|---|---|
| Hospital has partnered with community physicians or physician groups to reduce readmission rates |
|
| Yes | 297 (52.0%) |
| No | 274 (48.0%) |
| Hospital has partnered with other local hospitals to reduce readmission rates |
|
| Yes | 147 (25.7%) |
| No | 424 (74.3%) |
| Frequency with which nurses are responsible for conducting medication reconciliation at discharge |
|
| Never | 64 (11.2%) |
| Sometimes | 62 (10.9%) |
| Usually | 53 (9.3%) |
| Always | 392 (68.7%) |
| Frequency with which patients leave the hospital with an outpatient follow-up appointment already arranged |
|
| Never | 21 (3.7%) |
| Sometimes | 246 (43.1%) |
| Usually | 250 (43.8%) |
| Always | 54 (9.5%) |
| Proportion of patients for whom a paper or electronic discharge summary sent directly to the patient's primary MD |
|
| None | 43 (7.5%) |
| Some | 163 (28.6%) |
| Most | 213 (37.3%) |
| All | 152 (26.6%) |
| Someone within the hospital is assigned to follow up on test results that return after the patient is discharged |
|
| Yes | 206 (36.1%) |
| No | 365 (63.9%) |
| Frequency with which outpatient and inpatient prescription records linked electronically |
|
| Never | 344 (60.3%) |
| Sometimes | 104 (18.2%) |
| Usually | 68 (11.9%) |
| Always | 55 (9.6%) |
| All patients or their caregivers receive written emergency plan upon discharge |
|
| Yes | 326 (57.1%) |
| No | 245 (42.9%) |
| Reliable process is in place to ensure outpatient physicians are alerted to the patient's discharge within 48 hours of discharge |
|
| Yes | 231 (40.5%) |
| No | 340 (59.5%) |
| Hospital regularly calls patients after discharge to either follow up on post-discharge needs or to provide additional education |
|
| Yes | 357 (62.5%) |
| No | 214 (37.5%) |
Some reported strategies were associated with higher RSRRs in multivariable analysis (Table 2). These included: 1) more frequently linking outpatient and inpatient prescription records electronically (0.18 percentage point higher RSRR, P-value = 0.003), 2) providing all patients or their caregivers a written emergency plan upon discharge (0.38 percentage point, P-value = 0.004), 3) having a reliable process to ensure outpatient physicians were alerted about the patient's discharge within 48 hours of discharge (0.42 percentage point, P-value = 0.003), and 4) regularly calling patients after discharge to follow up on post-discharge needs or to provide additional education (0.34 percentage point, P-value 0.010).
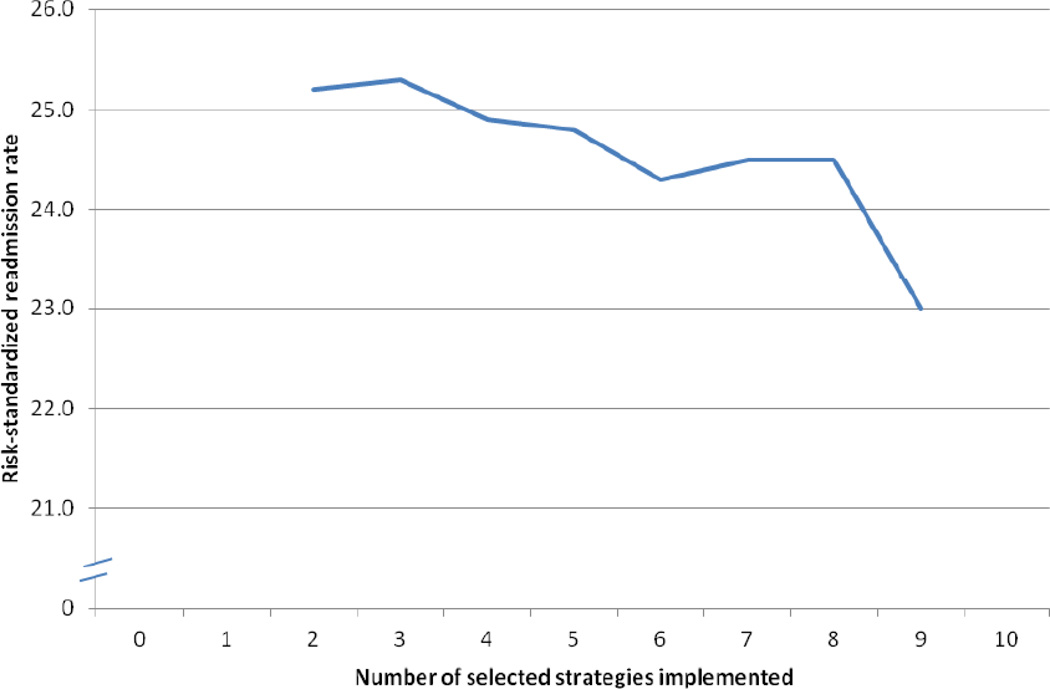
Hospitals that had a higher summary score for strategies had significantly lower RSRRs (B = - 0.34, SE = 0.04, P < 0.001) (Figure 1). Dummy variables for participation in H2H compared with STAAR, for geographic location, and for ownership types were non-significant in multivariable analysis and dropped from the final model. The results did not differ significantly among subgroups of hospitals of differing teaching status or number of beds (P-values for interactions > 0.05), although we had limited statistical power to examine subgroup effects.
Figure 1. Number of selected strategies implemented and RSRR.
Note: B = - 0.34, SE = 0.04, P < 0.001 in multivariable model adjusting for teaching status, region, and number of hospital beds
Number of selected strategies (possible range 0–10) was calculated by assigning a 1 to every strategy implemented that was positively associated with RSRR and by assigning a 1 to every strategy not implemented that was negatively associated with RSRR.
Adjusted R-Square = 0.14
Discussion
Several hospital strategies were associated with lower RSRR in this national study, and implementing more of the selected strategies was associated with greater reductions in RSRR. The effect sizes of individual strategies were modest, which might be expected given the many factors involved with the readmission process as well as the likelihood of inconsistent implementation of strategies. Nevertheless, together the strategies had a more prominent effect. Given the prevalence of heart failure, even relatively modest effects could improve transitions in care for more than 87,000 patients per year and also could have effects for the readmission penalty of any individual hospital. Among the 6 strategies that were associated with lower RSRR, most were implemented by less than 30% of hospitals, and only 7% of hospitals implemented all 6 strategies. COTH hospitals also had higher RSRRs than nonteaching hospitals, possibly due to the challenges of a complex care environment.
Many of the strategies associated with lower RSRRs are consistent with the widely endorsed belief that better integration of hospital care and primary care is needed to reduce readmissions. Previous studies have documented that many discharged patients do not attain prompt outpatient follow-up visits,15, 35 and for those who do, discharge summaries are frequently incomplete at the time of that visit.36 In this study, several strategies stood out that may reflect more effective communication links between the hospital and follow-up care. Hospitals that arranged a follow-up appointment before discharge, that had a process in place to send all discharge paper or electronic summaries directly to the patient's primary physician, and that assigned staff to follow up on test results that return after the patient is discharged had significantly lower RSRRs. Furthermore, the strategy with the largest association with lower RSRR was partnering with local health care providers (with community physicians or physician groups and with local hospitals) to reduce readmissions. Our findings highlight the importance of the full system of care and underscore the potential value of greater coordination between hospital and other providers for addressing readmissions.
Unexpectedly, we also found that some strategies, which seem to link hospitals and outpatient care more closely and have been recommended by quality alliances, were associated with higher RSRRs. This paradoxical finding could be the result of reverse causation, but may also be conveying unintended consequences of these interventions. If this is reverse causation, it is not clear why we would have also observed several recommended strategies that were associated with lower RSRR. Another possibility is that the quality of implementation of reported strategies may vary, with some hospitals reporting the strategy but not implementing it in the most effective way, or the measurement of the strategy may be imperfect. These measurement issues would dampen the observed effects and may explain smaller effect sizes, in both directions, and non-significant findings.
Also, it is possible that the unanticipated results may signal unintended effects of implementing more comprehensive discharge and follow-up processes. Providing emergency plans detailing for patients and family caregivers when and how to return to the hospital, contacting patients to assess follow-up needs, and linking the inpatient and outpatient medication records easily may all contribute to reducing the difficulty of coordinating a return to the hospital and of readmission. Reducing the informational and logistical barriers to hospitalization may increase readmissions when the practice is designed to reduce readmissions. These interventions may inadvertently lower the threshold for readmission. This effect was apparent in one randomized controlled trial,34 which found patients with extensive post-discharge follow up by physicians and nurses experienced higher readmission rates. Although post-discharge follow up may improve overall communication, these may also result in higher RSRRs. Such an explanation would lead to caution for hospitals assuming that such strategies can only improve their RSRRs. It may be that these interventions are useful but must be implemented in a way that supports outpatient care.
Our findings should be interpreted in light of several limitations. First, the data are cross-sectional and therefore may be limited by residual measured or unmeasured confounders, and causality may not be inferred. Nevertheless, several of the associations are plausible and consistent with some randomized controlled trials, and having contemporary and national data provides greater description of current strategies and their links with RSRR. Second, we have limited information about the methods of implementation, and although some strategies were not significantly associated with RSRR in this national sample, they may be effective in individual hospitals. Experimentation to tailor strategies to fit local circumstances should be encouraged. In addition, some strategies reported at the time of survey may not have been implemented for long enough to be reflected in the RSRR data. Third, we did not assess the influence of socioeconomic patient profiles of hospitals, such as race or income composition, which is beyond the scope of the present inquiry. We did, however, use the same methodology applied by Centers for Medicare & Medicaid Services (CMS) to calculate hospital RSRRs. Fourth, hospitals that participated in this study are self-selected and may have a particular interest in quality improvement for heart failure care. Findings from this study therefore may not be representative of the experience of patients treated in other hospitals in the United States. Last, we were unable to assess organizational culture in this quantitative study, which has been shown in multiple outcomes studies20, 37–40 to be an essential component of improvement efforts. Future work, which examines more nuanced features of successful hospitals and partnering outpatient clinicians, using qualitative methods, would be beneficial for understanding the key components and trajectories of improvement in the area of readmissions.
In sum, our study has identified several strategies that are more prominent in hospitals with lower RSRR; these add to the literature as they reflect national patterns of current strategies and outcomes. These strategies were implemented by a minority of hospitals. At the same time, the study highlights some unexpected findings that suggest some strategies meant to reduce readmissions may be associated with increased RSRR, potentially due to removal of communication or informational barriers to readmission. These findings raise questions about the implementation of these strategies and suggest that reducing readmissions for the 875,000 patients per year hospitalized with heart failure may require interventions that extend beyond those hospitals are currently implementing. Overall, our knowledge of the factors that affect readmissions is still in an early phase. Recognition of the importance of readmissions as a measure of quality is still very recent. We may need to employ more mixed methods techniques, with qualitative studies of hospital strategies and culture, as well as engagement with outpatient organizations, to understand which complex interventions are influential, and in which settings they are most effective.
Hospital Strategies Associated with 30-Day Readmission Rates for Patients with Heart Failure.
What is known about hospital strategies associated with 30-day readmission rates for patients with heart failure
Readmission of patients with heart failure is common and costly.
The Patient Protection Affordable Care Act of 2010 has created new incentives to reduce readmissions, and hospitals with high readmissions rates can lose up to 3 percent of their Medicare reimbursement by 2015.
Hospitals vary widely in the strategies they use to reduce readmissions.
Several randomized controlled trials have reported discharge and follow-up interventions that have reduced readmissions, but less is known outside the context of controlled trails.
What this article adds
This paper links hospital survey data on strategies being implemented with hospital readmission rates to identify strategies that are associated with higher or lower rates.
Completed surveys were from a national sample of 599 hospitals enrolled in the Hospital-to-Home quality campaign sponsored by the American College of Cardiology (91% response rate)
Six strategies were significantly associated with lower risk-standardized 30-day readmission rates in multivariable analysis; these were partnering with community physicians and physician groups, partnering with local hospitals, having nurses responsible for medication reconciliation, arranging for follow-up visits before discharge, having a process in place to send all discharge or electronic summaries directly to the patient's primary care physician, and assigning staff to follow up on test results after the patient is discharged.
Many of these strategies were being implemented by a minority of hospitals, highlighting substantial opportunities for improvement.
Acknowledgments
Funding Sources:
The Commonwealth Fund, One East 75th Street, New York, NY 10021 and Center for Cardiovascular Outcomes Research at Yale University, supported by the National Heart Lung, and Blood Institute, Bethesda, MD(U01HL105270-03).
Dr. Horwitz is supported by the National Institute on Aging, Bethesda, MD (K08 AG038336) and by the American Federation for Aging Research, New York, NY through the Paul B. Beeson Career Development Award Program. Dr. Horwitz is a Pepper Scholar with support from the Claude D. Pepper Older Americans Independence Center at Yale University School of Medicine, New Haven, CT (#P30AG021342 NIH/NIA)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures:
No funding source had any role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the article for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of The Commonwealth Fund, the National Institute on Aging, the National Institutes of Health, or the American Federation for Aging Research.
Dr. Krumholz reports that he is the recipient of a research grant from Medtronic through Yale University and chairs a cardiac scientific advisory board for United Health. Dr Walsh reports serving as a consultant to United Health Care and Eli Lilly.
References
- 1.Medicare Payment Advisory Commission (MedCAP) [Accessed on September 16]; Report to the Congress: creating greater efficiiency in Medicare http://www.medpac.gov/documents/Jun07_EntireReport.pdf.
- 2.Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006;166:1822–1828. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- 3.Koehler BE, Richter KM, Youngblood L, Cohen BA, Prengler ID, Cheng D, Masica AL. Reduction of 30-day postdischarge hospital readmission or emergency department (ED) visit rates in high-risk elderly medical patients through delivery of a targeted care bundle. J Hosp Med. 2009;4:211–218. doi: 10.1002/jhm.427. [DOI] [PubMed] [Google Scholar]
- 4.Krumholz HM, Amatruda J, Smith GL, Mattera JA, Roumanis SA, Radford MJ, Crombie P, Vaccarino V. Randomized trial of an education and support intervention to prevent readmission of patients with heart failure. J Am Coll Cardiol. 2002;39:83–89. doi: 10.1016/s0735-1097(01)01699-0. [DOI] [PubMed] [Google Scholar]
- 5.McDonald K, Ledwidge M, Cahill J, Kelly J, Quigley P, Maurer B, Begley F, Ryder M, Travers B, Timmons L, Burke T. Elimination of early rehospitalization in a randomized, controlled trial of multidisciplinary care in a high-risk, elderly heart failure population: the potential contributions of specialist care, clinical stability and optimal angiotensin-converting enzyme inhibitor dose at discharge. Eur J Heart Fail. 2001;3:209–215. doi: 10.1016/s1388-9842(00)00134-3. [DOI] [PubMed] [Google Scholar]
- 6.Naylor M, Brooten D, Jones R, Lavizzo-Mourey R, Mezey M, Pauly M. Comprehensive discharge planning for the hospitalized elderly. A randomized clinical trial. Ann Intern Med. 1994;120:999–1006. doi: 10.7326/0003-4819-120-12-199406150-00005. [DOI] [PubMed] [Google Scholar]
- 7.Naylor MD, Brooten D, Campbell R, Jacobsen BS, Mezey MD, Pauly MV, Schwartz JS. Comprehensive discharge planning and home follow-up of hospitalized elders: a randomized clinical trial. JAMA. 1999;281:613–620. doi: 10.1001/jama.281.7.613. [DOI] [PubMed] [Google Scholar]
- 8.Parry C, Min SJ, Chugh A, Chalmers S, Coleman EA. Further application of the care transitions intervention: results of a randomized controlled trial conducted in a fee-for-service setting. Home Health Care Serv Q. 2009;28:84–99. doi: 10.1080/01621420903155924. [DOI] [PubMed] [Google Scholar]
- 9.Phillips CO, Wright SM, Kern DE, Singa RM, Shepperd S, Rubin HR. Comprehensive discharge planning with postdischarge support for older patients with congestive heart failure: a meta-analysis. JAMA. 2004;291:1358–1367. doi: 10.1001/jama.291.11.1358. [DOI] [PubMed] [Google Scholar]
- 10.Rainville EC. Impact of pharmacist interventions on hospital readmissions for heart failure. Am J Health Syst Pharm. 1999;56:1339–1342. [PubMed] [Google Scholar]
- 11.Rich MW, Beckham V, Wittenberg C, Leven CL, Freedland KE, Carney RM. A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure. N Engl J Med. 1995;333:1190–1195. doi: 10.1056/NEJM199511023331806. [DOI] [PubMed] [Google Scholar]
- 12.Riegel B, Carlson B, Kopp Z, LePetri B, Glaser D, Unger A. Effect of a standardized nurse case-management telephone intervention on resource use in patients with chronic heart failure. Arch Intern Med. 2002;162:705–712. doi: 10.1001/archinte.162.6.705. [DOI] [PubMed] [Google Scholar]
- 13.Forster AJ, Clark HD, Menard A, Dupuis N, Chernish R, Chandok N, Khan A, Letourneau M, van Walraven C. Effect of a nurse team coordinator on outcomes for hospitalized medicine patients. Am J Med. 2005;118:1148–1153. doi: 10.1016/j.amjmed.2005.04.019. [DOI] [PubMed] [Google Scholar]
- 14.Harrison PL, Hara PA, Pope JE, Young MC, Rula EY. The impact of postdischarge telephonic follow-up on hospital readmissions. Popul Health Manag. 2011;14:27–32. doi: 10.1089/pop.2009.0076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hernandez AF, Greiner MA, Fonarow GC, Hammill BG, Heidenreich PA, Yancy CW, Peterson ED, Curtis LH. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303:1716–1722. doi: 10.1001/jama.2010.533. [DOI] [PubMed] [Google Scholar]
- 16.Joynt KE, Jha AK. Who has higher readmission rates for heart failure, and why? Implications for efforts to improve care using financial incentives. Circ Cardiovasc Qual Outcomes. 2011;4:53–59. doi: 10.1161/CIRCOUTCOMES.110.950964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McHugh MD, Ma C. Hospital nursing and 30-day readmissions among Medicare patients with heart failure, acute myocardial infarction, and pneumonia. Med Care. 2013;51:52–59. doi: 10.1097/MLR.0b013e3182763284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Anderson C, Deepak BV, Amoateng-Adjepong Y, Zarich S. Benefits of comprehensive inpatient education and discharge planning combined with outpatient support in elderly patients with congestive heart failure. Congest Heart Fail. 2005;11:315–321. doi: 10.1111/j.1527-5299.2005.04458.x. [DOI] [PubMed] [Google Scholar]
- 19.Azevedo A, Pimenta J, Dias P, Bettencourt P, Ferreira A, Cerqueira-Gomes M. Effect of a heart failure clinic on survival and hospital readmission in patients discharged from acute hospital care. Eur J Heart Fail. 2002;4:353–359. doi: 10.1016/s1388-9842(02)00013-2. [DOI] [PubMed] [Google Scholar]
- 20.Hansen LO, Williams MV, Singer SJ. Perceptions of hospital safety climate and incidence of readmission. Health Serv Res. 2011;46:596–616. doi: 10.1111/j.1475-6773.2010.01204.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155:520–528. doi: 10.7326/0003-4819-155-8-201110180-00008. [DOI] [PubMed] [Google Scholar]
- 22.Kociol RD, Peterson ED, Hammill BG, Flynn KE, Heidenreich PA, Pina IL, Lytle BL, Albert NM, Curtis LH, Fonarow GC, Hernandez AF. National survey of hospital strategies to reduce heart failure readmissions: findings from the Get With the Guidelines-Heart Failure registry. Circ Heart Fail. 2012;5:680–687. doi: 10.1161/CIRCHEARTFAILURE.112.967406. [DOI] [PubMed] [Google Scholar]
- 23.Mudge A, Denaro C, Scott I, Bennett C, Hickey A, Jones MA. The paradox of readmission: effect of a quality improvement program in hospitalized patients with heart failure. J Hosp Med. 2010;5:148–153. doi: 10.1002/jhm.563. [DOI] [PubMed] [Google Scholar]
- 24.VanSuch M, Naessens JM, Stroebel RJ, Huddleston JM, Williams AR. Effect of discharge instructions on readmission of hospitalised patients with heart failure: do all of the Joint Commission on Accreditation of Healthcare Organizations heart failure core measures reflect better care? Qual Saf Health Care. 2006;15:414–417. doi: 10.1136/qshc.2005.017640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bradley EH, Curry L, Horwitz LI, Sipsma H, Thompson JW, Elma M, Walsh MN, Krumholz HM. Contemporary evidence about hospital strategies for reducing 30-day readmissions: a national study. J Am Coll Cardiol. 2012;60:607–614. doi: 10.1016/j.jacc.2012.03.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ross JS, Chen J, Lin Z, Bueno H, Curtis JP, Keenan PS, Normand SL, Schreiner G, Spertus JA, Vidan MT, Wang Y, Wang Y, Krumholz HM. Recent national trends in readmission rates after heart failure hospitalization. Circ Heart Fail. 2010;3:97–103. doi: 10.1161/CIRCHEARTFAILURE.109.885210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bradley EH, Herrin J, Wang Y, Barton BA, Webster TR, Mattera JA, Roumanis SA, Curtis JP, Nallamothu BK, Magid DJ, McNamara RL, Parkosewich J, Loeb JM, Krumholz HM. Strategies for reducing the door-to-balloon time in acute myocardial infarction. N Engl J Med. 2006;355:2308–2320. doi: 10.1056/NEJMsa063117. [DOI] [PubMed] [Google Scholar]
- 28.H2H Quality Improvement Initiative. [Accessed on September 2012]; http://www.h2hquality.org/
- 29.Boutwell AE, Johnson MB, Rutherford P, Watson SR, Vecchioni N, Auerbach BS, Griswold P, Noga P, Wagner C. An early look at a four-state initiative to reduce avoidable hospital readmissions. Health Aff (Millwood) 2011;30:1272–1280. doi: 10.1377/hlthaff.2011.0111. [DOI] [PubMed] [Google Scholar]
- 30.Association of American Medical Colleges (AAMC) [Accessed on February 26, 2013]; Council of Teaching Hospitals and Health Systems® (COTH®) https://www.aamc.org/members/coth/
- 31.U.S. Department of Agriculture. [Accessed on August 19, 2011]; Urban Influence Codes http://www.ers.usda.gov/data-products/urban-influence-codes.aspx.
- 32.Keenan PS, Normand SL, Lin Z, Drye EE, Bhat KR, Ross JS, Schuur JD, Stauffer BD, Bernheim SM, Epstein AJ, Wang Y, Herrin J, Chen J, Federer JJ, Mattera JA, Wang Y, Krumholz HM. An administrative claims measure suitable for profiling hospital performance on the basis of 30-day all-cause readmission rates among patients with heart failure. Circ Cardiovasc Qual Outcomes. 2008;1:29–37. doi: 10.1161/CIRCOUTCOMES.108.802686. [DOI] [PubMed] [Google Scholar]
- 33.Krumholz HM, Lin Z, Drye EE, Desai MM, Han LF, Rapp MT, Mattera JA, Normand SL. An administrative claims measure suitable for profiling hospital performance based on 30-day all-cause readmission rates among patients with acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2011;4:243–252. doi: 10.1161/CIRCOUTCOMES.110.957498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Weinberger M, Oddone EZ, Henderson WG. Does increased access to primary care reduce hospital readmissions? Veterans Affairs Cooperative Study Group on Primary Care and Hospital Readmission. N Engl J Med. 1996;334:1441–1447. doi: 10.1056/NEJM199605303342206. [DOI] [PubMed] [Google Scholar]
- 35.Kiefe CI, Heudebert G, Box JB, Farmer RM, Michael M, Clancy CM. Compliance with post-hospitalization follow-up visits: rationing by inconvenience? Ethn Dis. 1999;9:387–395. [PubMed] [Google Scholar]
- 36.Kripalani S, Jackson AT, Schnipper JL, Coleman EA. Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med. 2007;2:314–323. doi: 10.1002/jhm.228. [DOI] [PubMed] [Google Scholar]
- 37.Curry LA, Spatz E, Cherlin E, Thompson JW, Berg D, Ting HH, Decker C, Krumholz HM, Bradley EH. What distinguishes top-performing hospitals in acute myocardial infarction mortality rates? A qualitative study. Ann Intern Med. 2011;154:384–390. doi: 10.7326/0003-4819-154-6-201103150-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Huang DT, Clermont G, Kong L, Weissfeld LA, Sexton JB, Rowan KM, Angus DC. Intensive care unit safety culture and outcomes: a US multicenter study. Int J Qual Health Care. 2010;22:151–161. doi: 10.1093/intqhc/mzq017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mardon RE, Khanna K, Sorra J, Dyer N, Famolaro T. Exploring relationships between hospital patient safety culture and adverse events. J Patient Saf. 2010;6:226–232. doi: 10.1097/PTS.0b013e3181fd1a00. [DOI] [PubMed] [Google Scholar]
- 40.Vogus TJ, Sutcliffe KM. The impact of safety organizing, trusted leadership, and care pathways on reported medication errors in hospital nursing units. Med Care. 2007;45:997–1002. doi: 10.1097/MLR.0b013e318053674f. [DOI] [PubMed] [Google Scholar]