The pathogenesis of type 2 diabetes is characterized by two major features: peripheral insulin resistance and impaired insulin secretion from pancreatic β cells (1, 2). The application of transgenic mouse technology to the study of diabetes has been extensively reviewed (3). Here, I review the application of a complementary approach, gene knockout technology, to the problem of understanding insulin resistance and its sequelae. After reviewing the phenotypes of animals with individual targeted mutations in homozygous or heterozygous form, I turn to the effects of double mutations and show that interactions between mediators of insulin signaling can account for the development of overt diabetes.
Gene knockout technology allows the investigator to generate homozygous null mutant mice and to examine the effects of a total lack of a particular gene product. Resultant phenotypes are expected to reflect physiological functions of the specific gene in vivo. The effects of gene dosage can be studied by focusing on heterozygous null mutants. Moreover, crossing of various heterozygous and/or homozygous knockout animals can be used to reconstitute alterations in multiple genes. Conditional (i.e., tissue-specific or inducible) knockouts can also be created using the Cre/loxP system (4). This tool expands the application of the knockout approach to allow the study of mutations that would be lethal if expressed systemically, and it allows the study of specific effects of mutations in a particular tissue without influences from the other tissues.
Knockout mice lacking the insulin receptor (IR)
The gene targeting approach has been applied to inactivate the IR gene in mice (5, 6). At birth, IR-deficient homozygous null (IR–/–) pups could not be distinguished from their wild-type or heterozygous littermates, but IR deficiency leads to a number of major metabolic alterations soon after suckling begins. IR–/– pups develop a severe form of diabetes with ketoacidosis, and their triglycerides and FFA levels are raised, leading to hepatic steatosis. The absence of insulin signaling in the liver also results in reduced hepatic glycogen content, and IR–/– pups show a marked postnatal growth retardation and skeletal muscle hypotrophy. White and brown adipose tissue are present, but in decreased amounts. Interestingly, the number of fat cells in these animals appears normal, and all stages of differentiation can be observed, but the cell fat content was markedly decreased (7). All of these disorders lead to the death of IR–/– pups within 1 week after birth. Heterozygous null mutants (IR+/–), conversely, do not show any major metabolic abnormalities and had normal glucose tolerance following an intraperitoneal glucose tolerance test. Their insulin levels are not significantly different from those of wild-type mice (5), although Brüning et al. (8) report that IR+/– mutants show increased insulin levels at the age of 4–6 months. Despite this insulin resistance, only about 10% of IR+/– animals (depending on the genetic background) ever develop type 2 diabetes.
More recently, a muscle-specific IR knockout was achieved using the Cre/loxP system (9). Mice carrying an altered IR gene with exon 4 flanked by loxP sites were generated and bred with transgenic mice that express the Cre recombinase under the control of the muscle creatine kinase promoter/enhancer. The resultant muscle-specific IR knockout (MIRKO) offspring show a >95% reduction in IR expression specifically in skeletal muscle and a parallel decrease in insulin-stimulated IR and insulin receptor substrate-1 phosphorylation. Despite impaired insulin-stimulated glucose uptake in skeletal muscle, these mice have elevated fat mass, serum triglycerides, and FFAs, but their blood glucose, serum insulin, and glucose tolerance are normal. Thus, insulin resistance in muscle contributes to the altered fat metabolism associated with type 2 diabetes, but tissues other than muscle appear to be more involved in insulin-regulated glucose disposal than was previously recognized.
Physical exercise promotes glucose uptake into skeletal muscle and makes the working muscles more sensitive to insulin. While MIRKO mice show normal resting 2-deoxyglucose (2DG) uptake in soleus muscles, with no significant response to insulin, they exhibit normal exercise-stimulated 2DG uptake and a normal synergistic activation of muscle 2DG uptake with the combination of exercise plus insulin (10). Glycogen content and glycogen synthase activity in resting muscle were normal in MIRKO mice, and exercise, but not insulin, increased glycogen synthase activity. Thus, this animal model showed that normal expression of muscle insulin receptors is not needed for the exercise-mediated increase in glucose uptake and glycogen synthase activity in vivo.
Tissue-specific knockout of the IR gene in the pancreatic β cell has also been achieved by breeding the same mice used to generate the MIRKO with transgenic mice expressing the Cre recombinase under the control of the rat insulin promoter (11). The resultant mice exhibit a selective loss of insulin secretion in response to glucose and a progressive impairment of glucose tolerance. These data indicate an important functional role for IR in glucose-sensing by the pancreatic β cell and suggest that defective insulin signaling at the level of the β cell contributes to the insulin secretion deficit in type 2 diabetes. Another tissue-specific knockout of the IR gene in the liver, in which the Cre recombinase was under the control of the rat albumin promoter (12), generated mice with severe insulin resistance associated with glucose intolerance at the age of 2 months. However, by 4 months of age, the fasting hyperglycemia had returned to normal levels. Therefore, isolated liver insulin resistance is sufficient to cause severe defects in glucose homeostasis, but not uncontrolled fasting hyperglycemia or diabetes.
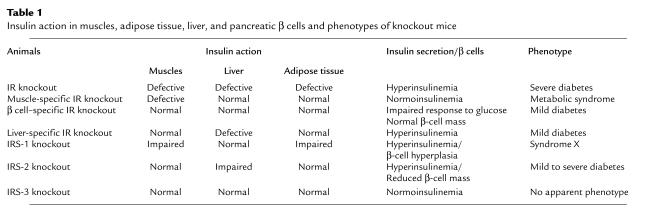
Changes in insulin action in various tissues and the phenotypes resulting from systemic or tissue-specific deficiency in the insulin receptor or its known substrates (IRSs) are summarized in Table 1.
Table 1.
Insulin action in muscles, adipose tissue, liver, and pancreatic β cells and phenotypes of knockout mice
Knockout mice lacking IRSs
IRS-1 is the major substrate of insulin receptor and IGF-1 receptor tyrosine kinases. To clarify the physiological roles of IRS-1 in vivo, we (13) and Ron Kahn’s group (14) made mice with a targeted disruption of the IRS-1 gene. IRS-1–/– mice were born alive but had retarded embryonal and postnatal growth (13, 14), indicating that IRS-1 plays an important role in the growth-promoting function of IGFs and insulin. These animals were also resistant to the glucose-lowering effects of insulin, IGF-1, and IGF-2. Despite their insulin resistance, they showed normal fasting glycemia and normal or mild glucose intolerance by virtue of increased insulin secretion by pancreatic β cells (13, 14). This compensatory hyperinsulinemia was caused by selective β-cell hyperplasia (15), as will be discussed below in more detail. In light of the relatively mild phenotypes of IRS-1–/– animals, the more severe effects seen in IR–/– animals (5) strongly suggest the existence of both IRS-1–dependent and IRS-1–independent pathways for transduction of insulin and IGF signals (13, 14).
To identify IRS-1–independent pathways, Ron Kahn’s group and ours examined the insulin-stimulated tyrosine-phosphorylated proteins in livers of wild-type and IRS-1–/– mice (14, 16, 17). Patti et al. (16) first demonstrated that the insulin-stimulated tyrosine-phosphorylated protein in the liver of IRS-1–/– mice was in fact IRS-2 — also known as IL-4 phosphotyrosine substrate (4-PS) (18) or, in our work (17), as pp190. We found that this molecule, like IRS-1, could bind both the 85-kDa subunit of phosphatidylinositol (PI) 3-kinase and the growth factor–bound protein 2 (Grb2) molecule, suggesting that it could participate in insulin signal transduction and perhaps compensate for the absence of IRS-1.
We also used IRS-1–/– mice to investigate the roles of IRS-1 in specific target organs. IRS-1–/– muscle showed low levels of insulin-induced PI 3-kinase activation, glucose transport, p70 S6 kinase activation, and mitogen-activated protein (MAP) kinase activation (19). In contrast, insulin-induced PI 3-kinase and MAP kinase activation were essentially normal in the liver. The differential use of IRS-2 as an alternative substrate may account for the different physiological effects of the mutation in these two organs. Thus, in the liver, the amount of tyrosine-phosphorylated IRS-2 in IRS-1–/– livers roughly matched the amount of tyrosine-phosphorylated IRS-1 in wild-type tissue. In the muscle, conversely, tyrosine-phosphorylated IRS-2 accumulated to levels only 20–30% of the amount of tyrosine-phosphorylated IRS-1 usually seen.
These phenotypic data suggest that IRS-1 plays central roles in two major biological actions of insulin in muscles, glucose transport and protein synthesis. They also indicate that the insulin resistance of IRS-1–/– mice is mainly due to resistance in the muscles. Finally, it appears that the degree of compensation for IRS-1 deficiency correlates with the amount of tyrosine-phosphorylated IRS-2 in the mutant, relative to that of IRS-1 in wild-type mice (19). Very similar conclusions were drawn by Brüning et al (20).
In adipose tissues, another target tissue of insulin, glucose transport occurs via the translocation of GLUT4 from an intracellular pool to the cell surface. Insulin-induced PI 3-kinase activity is substantially reduced in IRS-1–/– adipocytes (21), but yet another IRS, termed pp60 or IRS-3 (22), represents the major tyrosine-phosphorylated protein associated with PI 3-kinase. Tyrosine phosphorylation of IRS-2 and association of this molecule with PI 3-kinase were very low in these experiments (21). Glucose transport and GLUT4 translocation at maximal insulin stimulation are also decreased in IRS-1–/– adipocytes. These data suggest that both IRS-1 and IRS-3 play major roles in insulin-induced glucose transport in these cells and that IRS-3 is predominantly involved in regulating this process in the absence of IRS-1 (21).
More recently, we reported that IRS-1–/– mice show features of syndrome X, such as hypertriglyceridemia and hypertension (23). The former effect may be due to decreased lipoprotein lipase activity, arising from insulin resistance in the adipose tissue. We have also suggested that hypertension in IRS-1–/– animals results in part from impaired vascular relaxation in the insulin-resistant endothelium. Thus, insulin resistance due to IRS-1 deficiency per se was sufficient to cause syndrome X but not to cause type 2 diabetes, which, as discussed below, requires a simultaneous defect in insulin secretion (15).
Targeted disruption of the IRS-2 gene was reported by Morris White’s group (24), and we have also generated IRS-2 knockout mice (25). The phenotype obtained differs strikingly from that of IRS-1–deficient animals. Heterozygous mice (IRS-2+/–) are of normal birth size and phenotype. IRS-2–/– mice are born 10% smaller than wild-type, and this difference persists into adulthood. These mice develop a marked and progressive glucose intolerance and have full-blown diabetes at 10 weeks, although the phenotype is milder in our IRS-2–/– animals (25) than in those studied by Withers et al. (24). It appears that IRS-2 deficiency not only causes peripheral insulin resistance (much as IRS-1 deficiency does) but also prevents β-cell compensation for insulin resistance. Histological analysis revealed that, as early as 4 weeks, β-cell mass is reduced by 17% compared with wild-type, in marked contrast to the 85% increase in β-cell mass in IRS-1–/– islets (25). Interestingly, even though β-cell hyperplasia is defective in IRS-2 knockout mice, we have found that individual β cells show normal or increased insulin secretion in response to glucose (25). Thus a single gene mutation in this animal model can induce both the peripheral insulin resistance and the β-cell deficiency seen in typical type 2 diabetes.
With regard to insulin signaling, Withers et al. (24) report that the degree of stimulation of PI 3-kinase activity associated with IRS-1 in liver and muscle of IRS-2–/– is reduced by >50%, due in part to an increased basal activity. This finding contrasts with the marked enhancement of insulin-stimulated PI 3-kinase associated with IRS-2 seen in IRS-1–/– mice. These authors proposed that the defect in PI 3-kinase regulation in IRS-2–/– is the major factor underlying defective glucose metabolism. We have found, however, that insulin-induced PI 3-kinase activation is significantly impaired in the livers of IRS-2–/– mice, whereas PI 3-kinase activation in the skeletal muscles is essentially normal (25). Moreover, IRS-1–mediated PI 3-kinase activity is essentially normal in both of these tissues. Thus, IRS-1 and IRS-2 mediate common and specific effects of insulin and IGF-1 in peripheral tissues and β cells.
To explore the interactions between these IRS proteins, Withers et al. intercrossed mice heterozygous for two null alleles (IRS-1+/– and IRS-2+/–) and investigated growth and glucose metabolism in mice with viable genotypes (26). They showed that IRS-1 and IRS-2 are critical for embryonic and postnatal growth, with IRS-1 having the predominant role. Although both IRS-1 and IRS-2 are involved in peripheral carbohydrate metabolism, IRS-2 plays the major role in β-cell development and compensation for peripheral insulin resistance. These authors also intercrossed mice heterozygous for null alleles of the genes for the IGF-1 receptor and IRS-2 (26), and they found that IGF-1 receptors promote β-cell development and survival through the IRS-2 signaling pathway, thus establishing a role for the IGF-1 receptor in β cells. Evidently, IRS-2 integrates the effects of insulin in peripheral target tissues with those of IGF-1 in pancreatic β cells to maintain glucose homeostasis.
Since IRS-1 and IRS-2 are each required for normal growth and glucose homeostasis, Liu et al. generated mice with a targeted disruption of the IRS-3 gene (27). Homozygous IRS-3–deficient mice showed normal body weight throughout development, normal blood glucose and insulin levels, and normal glucose transport in adipocytes. It should be noted, however, that important roles for IRS-3 in adipocytes or β cells may be masked by compensation by either IRS-1 or IRS-2 in these tissues.
Knockout mice lacking PI 3-kinase
A role for PI 3-kinase activity in insulin-stimulated glucose transport and GLUT4 translocation has been suggested from in vitro work, but its role in vivo and the molecular link between activation of PI 3-kinase and translocation have not yet been elucidated. To determine the role of PI 3-kinase in glucose homeostasis, we generated mice with a targeted disruption of the Pik3r1 gene, encoding the p85α regulatory subunit of PI 3-kinase (28). The p85 regulatory subunit associates through its SH2 domain with IRS molecules, interactions that lead to PI 3-kinase activation. Pik3r1–/– mice show increased insulin sensitivity and hypoglycemia due to increased glucose transport in skeletal muscle and adipocytes. Insulin-stimulated PI 3-kinase activity associated with IRSs is mediated by full-length p85α in wild-type mice, but by the p50α alternative splicing isoform of the same gene (29) in Pik3r1–/–. This isoform switch is associated with an increase in insulin-induced generation of PI(3, 4, 5)triphosphate in Pik3r1–/– adipocytes, as well as heightened GLUT4 translocation to the plasma membrane. These results provide the first direct evidence that PI 3-kinase contributes to glucose homeostasis (28), which may be influenced by the expression of alternative isoforms of the PI 3-kinase regulatory subunits.
Knockout mice lacking GLUT4
Gene targeting has also been used to generate mice carrying a null mutation in the GLUT4 gene (30). Because GLUT4 is dysregulated in diabetes and obesity, it was expected that genetic ablation of GLUT4 would result in abnormal glucose homeostasis. Homozygous null mutants (GLUT4–/–), however, did not show a diabetic phenotype. Indeed, blood glucose levels in females are not significantly elevated in either the fasted or fed states, and males exhibit lower glucose levels in both states. Insulin resistance is seen in animals of both sexes, as evidenced by five- to sixfold higher postprandial hyperinsulinemia and impaired glucose response to insulin tolerance test. GLUT4 deficiency resulted in decreased levels of lactate and FFAs in both the fasting and fed states, and of β-hydroxybutyrate in the fasting state. These changes are the opposite of those seen with GLUT4 overproduction and also the opposite of those seen in the diabetic phenotype. There was a marked reduction in fat tissue deposition in GLUT4–/– mutants, contrasting with the increased adiposity of mice overproducing GLUT4 in adipocytes. GLUT4–/– mice are small and suffer significant cardiac hypertrophy, which may be related to hyperinsulinemia and a decreased supply of FFAs. Possibly as a result of abnormal cardiac function, GLUT4–/– mice generally live only 5–7 months. Increased expression of other glucose-transporter genes was detected in liver (GLUT2) and heart (GLUT1), but not in skeletal muscle. Recently, Tsao et al. (31) obtained GLUT4-deficient mice in which GLUT4 expression was reconstituted in skeletal muscle. The alterations in glucose metabolism due to GLUT4 deficiency could be corrected by GLUT4 expression in skeletal muscle alone, but the transgene did not restore normal adipose-tissue function, since fat-pad weight and FFA levels remained lower in these mice (31).
Heterozygous GLUT4+/– mice are born with normal phenotype and are fertile. Interestingly, although the male mice do not become obese as they age, they develop hyperinsulinemia and subsequently hypertension and hyperglycemia (32), despite the fact that there is no evidence of β-cell deficiency. GLUT4 content and glucose uptake in muscles of hyperinsulinemic mice are also markedly reduced. There was a drastic decrease in GLUT4 expression in adipose tissue as well, with no change in total mass, but average cell volume increased by 35%. To investigate the impact of a partial deficiency in the level of GLUT4 on in vivo insulin action, Rossetti et al. (33) examined glucose disposal and hepatic glucose production during hyperinsulinemic clamp studies in these heterozygous mice. Since the disruption of one allele of GLUT4 led to severe peripheral, but not hepatic, insulin resistance, they concluded that varying levels of GLUT4 protein in striated muscle and adipose tissue can markedly alter whole-body glucose disposal. The mice also showed diabetic histopathologies (diabetic cardiomyopathy and liver steatosis) in the heart and liver, similar to those of humans with type 2 diabetes (34). Thus, male GLUT4+/– mice represent a good model for studying the development of type 2 diabetes without the complications associated with obesity.
To determine whether development of the diabetic phenotype in GLUT4+/– can be blocked by preventing the onset of impaired muscle GLUT4 expression and glucose utilization, Tsao et al. introduced into GLUT4+/– animals a GLUT4 transgene under control of the myosin light chain (MLC) promoter, which directs expression into fast-twitch muscles (34). GLUT4 expression and 2DG uptake levels were normal in the fast-twitch muscles of these MLC-GLUT4+/– mice. These mice differ from nontransgenic GLUT4+/– animals in that their whole-body glucose utilization is normal. Moreover, the development of hyperinsulinemia and hyperglycemia as seen in the GLUT4+/– strain was prevented in MLC-GLUT4+/–, and diabetic heart histopathology in MLC-GLUT4+/– occurred at control levels. Based on these results, the authors proposed that the onset of a diabetic phenotype in GLUT4+/– can be avoided by preventing decreases in muscle GLUT4 expression and glucose uptake.
More recently, a muscle-specific knockout was achieved using the Cre/loxP system (35). These animals show a 90–95% reduction in GLUT4 expression in skeletal muscle, with no compensatory increase in GLUT1. In contrast to mice with a muscle-specific IR knockout, muscle-specific GLUT4 knockout mice had more severe insulin resistance, fasting hyperglycemia, and glucose intolerance. This difference may be due to the fact that contraction-induced glucose uptake in muscle is intact in the muscle-specific IR knockout, whereas it is abolished in the muscle-specific GLUT4 knockout.
Knockout mice lacking peroxisome proliferator–activated receptor γ
Agonist-induced activation of peroxisome proliferator–activated receptor γ (PPARγ) is known to cause adipocyte differentiation and to promote insulin sensitivity (36, 37). To investigate the biological role of this molecule, we and others generated PPARγ-deficient mice by gene targeting (38–40). Homozygous mutant embryos died at 10.5–11.5 days postcoitum due to placental dysfunction (38, 39). More interestingly, however, PPARγ+/– heterozygous mice proved resistant to the usual effects of high dietary fat intake on glucose metabolism. Unlike wild-type mice given high-fat diets, these animals fail to become obese and insulin resistant, and they maintain the expression of GLUT4 in their white adipose tissue. Despite reduced adipose tissue mass and adipocyte size in PPARγ+/– animals, leptin expression is increased, due to a partial suppression of PPARγ-mediated inhibition of leptin gene expression by loss of one PPARγ allele, possibly accounting for this protective effect. Similar results were also reported by another group (41).
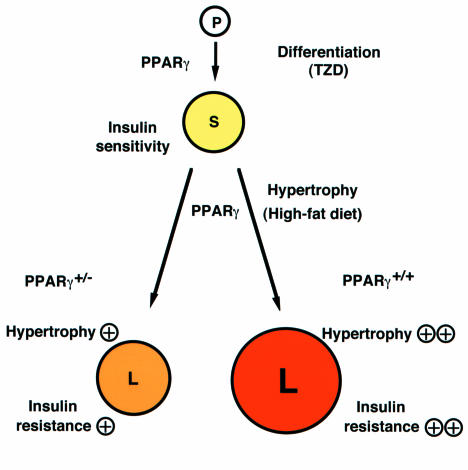
We hypothesize that PPARγ also participates in the regulation of adipocyte hypertrophy (i.e., the conversion of small adipocytes into large adipocytes) in the insulin-resistant state (Figure 1). In wild-type mice, a high-fat diet leads to adipocyte hypertrophy, which induces factors such as TNF-α and FFAs and thus promotes insulin resistance. Since heterozygous PPARγ deficiency prevented adipocyte hypertrophy and the development of insulin resistance under a high-fat diet, it appears that the amount of PPARγ plays a critical role in adipocyte hypertrophy and development of insulin resistance. Thus, it seems likely that PPARγ plays dual roles in the regulation of insulin sensitivity. In the presence of potent synthetic ligands such as thiazolidinedione (and, presumably, during childhood), the differentiation of adipocytes and, hence, the number of adipocytes depend upon activation of PPARγ (37–40). In adults under a high-fat diet, however, adipocyte hypertrophy and, hence, the size of adipocytes depend upon the level of PPARγ expression. PPARγ stimulation results in adipocyte differentiation to generate small adipocytes and insulin sensitivity in the former context and adipocyte hypertrophy to generate large adipocytes and insulin resistance in the latter context.
Figure 1.
Roles of PPARγ in the adipocyte. In this model, PPARγ acts at two steps to regulate adipocyte size and insulin sensitivity. First, PPARγ promotes the differentiation of pre-adipocytes (P) to normal, insulin-sensitive, small adipocytes (S), a step that can be activated by providing artificial PPARγ agonists, the thiazolidinediones (TZD). PPARγ also plays a critical role in adipocyte hypertrophy and development of insulin resistance under a high-fat diet. In wild-type mice, such a diet promotes adipocyte hypertrophy, which converts small adipocytes (S) into large adipocytes (L). These latter cells, in turn, induce factors such as TNF-α and FFAs, which promote insulin resistance. PPARγ+/– animals therefore enjoy some protection from adipocyte hypertrophy and the development of insulin resistance under a high-fat diet. Adapted from ref. 38.
PPARγ appears to facilitate energy storage under a high-fat diet in part by inhibiting expression in adipocytes of leptin, the major hormonal regulator of energy homeostasis. It seems that PPARγ is an example of a “thrifty” gene (36, 38), variations in which promote efficient storage of energy as fat. Consistent with this possibility, subjects with the Pro12 Ala variant of the PPARγ gene, which causes a modest reduction of PPARγ activity, have a decreased body mass index and decreased insulin resistance, as well as protection from type 2 diabetes (42, 43). The identification of a novel role for PPARγ in obesity and insulin resistance may inspire novel therapeutic strategies such as a PPARγ antagonist for obesity and obesity-linked insulin resistance.
Interplay between genetic defects in the development of type 2 diabetes
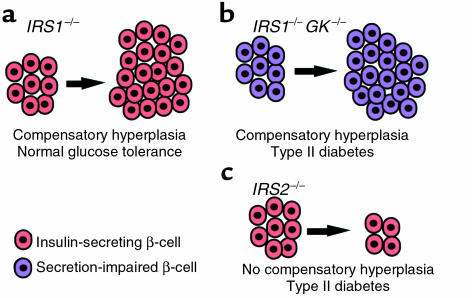
The peripheral insulin resistance and impaired insulin secretion from pancreatic β cells seen in type 2 diabetes (1, 2) may be genetic in origin or may be augmented by environmental factors and by ongoing hyperglycemia itself. These factors may interact in a complex manner to cause and sustain hyperglycemia. Previous prospective studies have demonstrated that both insulin resistance (often accompanied by hyperinsulinemia) and low insulin response to glucose are predictors of human type 2 diabetes (1, 2, 44–46). To investigate the interactions between insulin resistance and insulin secretory defects in the development of diabetes, we generated an animal model with these two genetic defects by crossing IRS-1–deficient mice and mice with a β cell–specific GK deficiency (ref. 15; see also Cavaghan et al., this Perspective series, ref. 47). As described above, IRS-1–/– mice are insulin-resistant but maintain normal glucose tolerance because of compensatory hyperinsulinemia (13, 14). We have also generated a mouse strain with a β cell–specific reduction in glucokinase expression, which shows mild glucose intolerance due to an impaired insulin response to glucose (48). Crossing the two strains generated a double knockout with features of both lines: insulin resistance and impaired insulin secretion (Figure 2). These animals showed overt diabetes (15).
Figure 2.
Three patterns of response of pancreatic β cells to insulin resistance. (a) In IRS–/– animals, glucose tolerance remains normal in the face of insulin resistance because their β cells (red) proliferate to compensate for reduced insulin responses. (b) In mice lacking both glucokinase and IRS-1 (GK–/–/IRS-1 double knockouts), a similar compensatory β-cell hyperplasia occurs, but the animals develop type 2 diabetes because their β cells (purple) are defective in glucose-stimulated insulin secretion. (c) IRS-2–/– mice, similarly, become overtly diabetic. These animals have functional β cells (red) that are unable to undergo hyperplasia to compensate for insulin resistance. Together, these results indicate that the compensatory response of β cells to insulin resistance plays a crucial role in preventing the development of type 2 diabetes. KO, knockout.
As shown in Figure 2, whereas IRS-1–/– mice show normal glucose tolerance due to compensatory β-cell hyperplasia, the GK/IRS-1 double-knockout mice develop type 2 diabetes. The latter mice show β-cell hyperplasia, but their diminished expression of GK evidently causes a severe enough defect in glucose-stimulated insulin secretion that this hyperplasia is insufficient to compensate for insulin resistance. In contrast, IRS-2–/– mice fail to induce β-cell hyperplasia in response to insulin resistance and therefore develop type 2 diabetes, despite normal or even increased induction of insulin secretion by glucose in individual β cells.
Thus, genetic variations can cooperate to cause overt diabetes. In this case, mild insulin resistance and a slight defect in insulin secretion, when combined, lead to the development of diabetes. Another example of this principle comes from the study of mice doubly heterozygous for null alleles in IR and IRS-1. Singly heterozygous mice, as described above, have no obvious clinical phenotype. Brüning et al. (8) generated double-heterozygous mutant mice carrying one null allele for both IR and IRS-1. Such animals were indistinguishable from their littermates at birth, but the expression of IR and IRS-1 in livers and muscles of these mice was diminished by 60%. As a consequence, insulin-stimulated autophosphorylation of IR, tyrosine-phosphorylation of IRS-1 and IRS-2, and association of the p85 subunit of PI 3-kinase with IRS-1 are all reduced. Blood glucose is normal and remains so up to the age of 4–6 months, but insulin levels are already higher at 2 months in the double heterozygotes than in either of the single mutants. At 4–6 months, these animals develop a marked insulin resistance, as evidenced by severely elevated levels of plasma insulin and blunted response to exogenous insulin. At 6 months, 40% of double-heterozygous null mutants for IR and IRS-1 become overtly diabetic. The development of insulin resistance is accompanied by an increase in β-cell mass, which is most pronounced in the diabetic animals. It therefore appears that the combination of minor defects in the insulin signaling cascade can act synergistically to cause insulin resistance and type 2 diabetes in an age-dependent manner (8).
Human type 2 diabetes is a polygenic disease requiring the interactions of multiple genetic factors and environmental factors to become manifest. Genetic dissection of type 2 diabetes in humans is clearly limited for both practical and ethical reasons. In this respect, use of inbred animal models that spontaneously reproduce the main features of type 2 diabetes offers an important strategy for genetic investigations. Since whole-genome mapping and identification of human type 2 diabetes genes are progressing rapidly (49), the genetic reconstitution of multiple defects in human type 2 diabetes genes in mice should shed light on the molecular mechanism and actual biochemical pathways of human type 2 diabetes.
Acknowledgments
I am grateful to Kazuyuki Tobe and Yasuo Terauchi for useful suggestions and comments for this review. Yasuo Terauchi contributed to Figure 2. This work was supported by a grant-in-aid for creative basic research (10NPO201) from the Ministry of Education, Science, Sports and Culture of Japan.
References
- 1.Kadowaki T, et al. Risk factors for worsening to diabetes in subjects with impaired glucose tolerance. Diabetologia. 1984;26:44–49. doi: 10.1007/BF00252262. [DOI] [PubMed] [Google Scholar]
- 2.Taylor SI, Accili D, Imai Y. Insulin resistance or insulin deficiency: which is the primary cause of NIDDM? Diabetes. 1994;43:735–740. doi: 10.2337/diab.43.6.735. [DOI] [PubMed] [Google Scholar]
- 3.Moller DE. Transgenic approaches to the pathogenesis of NIDDM. Diabetes. 1994;43:1394–1401. doi: 10.2337/diab.43.12.1394. [DOI] [PubMed] [Google Scholar]
- 4.Rajewsky K, et al. Conditional gene targeting. J Clin Invest. 1996;98:600–603. doi: 10.1172/JCI118828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Accili D, et al. Early neonatal death in mice homozygous for a null allele of the insulin receptor gene. Nat Genet. 1996;12:106–109. doi: 10.1038/ng0196-106. [DOI] [PubMed] [Google Scholar]
- 6.Joshi RL, et al. Targeted disruption of the insulin receptor gene in the mouse results in neonatal lethality. EMBO J. 1996;15:1542–1547. [PMC free article] [PubMed] [Google Scholar]
- 7.Cinti S, Eberbach S, Castellucci M, Accili D. Lack of insulin receptors affects the formation of white adipose tissue in mice. A morphometric and ultrastructural analysis. Diabetologia. 1998;41:171–177. doi: 10.1007/s001250050886. [DOI] [PubMed] [Google Scholar]
- 8.Brüning JC, et al. Development of a novel polygenic model of NIDDM in mice heterozygous for IR and IRS-1 null alleles. Cell. 1997;88:561–572. doi: 10.1016/s0092-8674(00)81896-6. [DOI] [PubMed] [Google Scholar]
- 9.Brüning JC, et al. A muscle-specific insulin receptor knockout exhibits features of the metabolic syndrome of NIDDM without altering glucose tolerance. Mol Cell. 1998;2:559–569. doi: 10.1016/s1097-2765(00)80155-0. [DOI] [PubMed] [Google Scholar]
- 10.Wojtaszewski JF, et al. Exercise modulates postreceptor insulin signaling and glucose transport in muscle-specific insulin receptor knockout mice. J Clin Invest. 1999;104:1257–1264. doi: 10.1172/JCI7961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kulkarni RN, et al. Tissue-specific knockout of the insulin receptor in pancreatic beta cells creates an insulin secretory defect similar to that in type 2 diabetes. Cell. 1999;96:329–339. doi: 10.1016/s0092-8674(00)80546-2. [DOI] [PubMed] [Google Scholar]
- 12.Michael MD, et al. Loss of insulin signalling in hepatocytes leads to severe insulin resistance and progressive hepatic dysfunction. Mol Cell. 2000;6:87–97. [PubMed] [Google Scholar]
- 13.Tamemoto H, et al. Insulin resistance and growth retardation in mice lacking insulin receptor substrate-1. Nature. 1994;372:182–186. doi: 10.1038/372182a0. [DOI] [PubMed] [Google Scholar]
- 14.Araki E, et al. Alternative pathway of insulin signaling in mice with targeted disruption of the IRS-1 gene. Nature. 1994;372:186–190. doi: 10.1038/372186a0. [DOI] [PubMed] [Google Scholar]
- 15.Terauchi Y, et al. Development of non-insulin-dependent diabetes mellitus in the double knockout mice with disruption of insulin receptor substrate-1 and β cell glucokinase genes: genetic reconstitution of diabetes as a polygenic disease. J Clin Invest. 1997;99:861–866. doi: 10.1172/JCI119250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Patti ME, et al. 4PS/insulin receptor substrate (IRS)-2 is the alternative substrate of the insulin receptor in IRS-1-deficient mice. J Biol Chem. 1995;270:24670–24673. doi: 10.1074/jbc.270.42.24670. [DOI] [PubMed] [Google Scholar]
- 17.Tobe K, Tamemoto H, Yamauchi T, Yazaki Y, Kadowaki T. Identification of a 190-kDa protein as a novel substrate for the insulin receptor kinase functionally similar to insulin receptor substrate-1. J Biol Chem. 1995;270:5698–5701. doi: 10.1074/jbc.270.11.5698. [DOI] [PubMed] [Google Scholar]
- 18.Sun XJ, et al. Role of IRS-2 in insulin and cytokine signalling. Nature. 1995;377:173–177. doi: 10.1038/377173a0. [DOI] [PubMed] [Google Scholar]
- 19.Yamauchi T, et al. Insulin signalling and insulin actions in the muscle and liver of insulin resistant IRS-1 deficient mice. Mol Cell Biol. 1996;16:3074–3084. doi: 10.1128/mcb.16.6.3074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brüning JC, Winnay J, Cheatham B, Kahn RC. Differential signaling by insulin receptor substrate 1 (IRS-1) and IRS-2 in IRS-1-deficient cells. Mol Cell Biol. 1997;17:1513–1521. doi: 10.1128/mcb.17.3.1513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kaburagi Y, et al. Role of insulin receptor substrate-1 and pp60 in the regulation of insulin-induced glucose transport and GLUT4 translocation in primary adipocytes. J Biol Chem. 1997;272:25839–25844. doi: 10.1074/jbc.272.41.25839. [DOI] [PubMed] [Google Scholar]
- 22.Lavan BE, Lane WS, Lienhard GE. The 60-kDa phosphotyrosine protein in insulin-treated adipocytes is a new member of the insulin receptor substrate family. J Biol Chem. 1997;272:11439–11443. doi: 10.1074/jbc.272.17.11439. [DOI] [PubMed] [Google Scholar]
- 23.Abe H, et al. Hypertension, hypertriglyceridemia, and impaired endothelium-dependent vascular relaxation in mice lacking insulin receptor substrate-1. J Clin Invest. 1998;101:1784–1788. doi: 10.1172/JCI1594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Withers DJ, et al. Disruption of IRS-2 causes type 2 diabetes in mice. Nature. 1998;391:900–904. doi: 10.1038/36116. [DOI] [PubMed] [Google Scholar]
- 25.Kubota, N., et al. 2000. Disruption of insulin receptor substrate-2 causes type 2 diabetes due to liver insulin resistance and lack of compensatory β-cell hyperplasia. Diabetes. In press. [DOI] [PubMed]
- 26.Withers DJ, et al. Irs-2 coordinates Igf-1 receptor-mediated beta-cell development and peripheral insulin signalling. Nat Genet. 1999;23:32–40. doi: 10.1038/12631. [DOI] [PubMed] [Google Scholar]
- 27.Liu SC, Wang Q, Lienhard GE, Keller SR. Insulin receptor substrate 3 is not essential for growth or glucose homeostasis. J Biol Chem. 1999;274:18093–18099. doi: 10.1074/jbc.274.25.18093. [DOI] [PubMed] [Google Scholar]
- 28.Terauchi Y, et al. Increased insulin sensitivity and hypoglycaemia in mice lacking the p85α subunit of phosphoinositide 3-kinase. Nat Genet. 1999;21:230–235. doi: 10.1038/6023. [DOI] [PubMed] [Google Scholar]
- 29.Fruman DA, Cantley LC, Carpenter CL. Structural organization and alternative splicing of the murine phosphoinositide 3-kinase p85α gene. Genomics. 1996;37:113–121. doi: 10.1006/geno.1996.0527. [DOI] [PubMed] [Google Scholar]
- 30.Katz EB, Stenbit AE, Hatton K, DePinho R, Charron MJ. Cardiac and adipose tissue abnormalities but not diabetes in mice deficient in GLUT4. Nature. 1995;377:151–155. doi: 10.1038/377151a0. [DOI] [PubMed] [Google Scholar]
- 31.Tsao TS, et al. Muscle-specific transgenic complementation of GLUT4-deficient mice. Effects on glucose but not lipid metabolism. J Clin Invest. 1997;100:671–677. doi: 10.1172/JCI119579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stenbit AE, et al. GLUT4 heterozygous knockout mice develop muscle insulin resistance and diabetes. Nat Med. 1997;3:1096–1101. doi: 10.1038/nm1097-1096. [DOI] [PubMed] [Google Scholar]
- 33.Rossetti L, et al. Peripheral but not hepatic insulin resistance in mice with one disrupted allele of the glucose transporter type 4 (GLUT4) gene. J Clin Invest. 1997;100:1831–1839. doi: 10.1172/JCI119711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tsao TS, et al. Prevention of insulin resistance and diabetes in mice heterozygous for GLUT4 ablation by transgenic complementation of GLUT4 in skeletal muscle. Diabetes. 1999;48:775–782. doi: 10.2337/diabetes.48.4.775. [DOI] [PubMed] [Google Scholar]
- 35.Zisman, A., et al. 2000. Targeted disruption of the glucose transporter 4 selectively in muscle causes insulin resistance and glucose intolerance. Nat. Med. In press. [DOI] [PubMed]
- 36.Auwerx J. PPARγ, the ultimate thrifty gene. Diabetologia. 1999;42:1033–1049. doi: 10.1007/s001250051268. [DOI] [PubMed] [Google Scholar]
- 37.Okuno A, et al. Troglitazone increases the number of small adipocytes without the change of white adipose tissue mass in obese Zucker rats. J Clin Invest. 1998;101:1354–1361. doi: 10.1172/JCI1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kubota N, et al. PPARγ mediates high-fat diet-induced adipocyte hypertrophy and insulin resistance. Mol Cell. 1999;4:597–609. doi: 10.1016/s1097-2765(00)80210-5. [DOI] [PubMed] [Google Scholar]
- 39.Barak Y, et al. PPAR gamma is required for placental, cardiac, and adipose tissue development. Mol Cell. 1999;4:585–595. doi: 10.1016/s1097-2765(00)80209-9. [DOI] [PubMed] [Google Scholar]
- 40.Rosen ED, et al. PPAR gamma is required for the differentiation of adipose tissue in vivo. Mol Cell. 1999;4:611–617. doi: 10.1016/s1097-2765(00)80211-7. [DOI] [PubMed] [Google Scholar]
- 41.Miles PD, Barak Y, He W, Evans RM, Olefsky JM. Improved insulin-sensitivity in mice heterozygous for PPAR gamma deficiency. J Clin Invest. 2000;105:287–292. doi: 10.1172/JCI8538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Deeb SS, et al. A Pro 12 Ala substitution in PPARgamma2 associated with decreased receptor activity, low body mass index and improved insulin sensitivity. Nat Genet. 1998;20:284–287. doi: 10.1038/3099. [DOI] [PubMed] [Google Scholar]
- 43.Hara K, et al. A Pro12Ala polymorphism in PPARg2 may confer resistance to type II diabetes. Biochem Biophys Res Commun. 2000;271:212–216. doi: 10.1006/bbrc.2000.2605. [DOI] [PubMed] [Google Scholar]
- 44.Martin BC, et al. Role of glucose and insulin resistance in the development of type 2 diabetes mellitus: results of a 25-year follow-up study. Lancet. 1992;340:925–929. doi: 10.1016/0140-6736(92)92814-v. [DOI] [PubMed] [Google Scholar]
- 45.Johnston C, Ward WK, Beard JC, McKnight B, Porte D., Jr Islet function and insulin sensitivity in the non-diabetic offspring of conjugal type 2 diabetic patients. Diabet Med. 1990;7:119–125. doi: 10.1111/j.1464-5491.1990.tb01345.x. [DOI] [PubMed] [Google Scholar]
- 46.Haffner SM, Miettinen H, Gaskill SP, Stern MP. Decreased insulin secretion and increased insulin resistance are independently related to the 7-year risk of NIDDM in Mexican-Americans. Diabetes. 1995;44:1386–1391. doi: 10.2337/diab.44.12.1386. [DOI] [PubMed] [Google Scholar]
- 47.Cavaghan MK, Ehrmann DA, Polonsky KS. Interactions between insulin resistance and insulin secretion in the development of glucose intolerance. J Clin Invest. 2000;106:329–333. doi: 10.1172/JCI10761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Terauchi Y, et al. Pancreatic β-cell-specific targeted disruption of glucokinase gene. Diabetes mellitus due to defective insulin secretion to glucose. J Biol Chem. 1995;270:30253–30256. doi: 10.1074/jbc.270.51.30253. [DOI] [PubMed] [Google Scholar]
- 49.Cox NJ, et al. Loci on chromosome 2 (NIDDM1) and 15 interact to increase susceptibility to diabetes in Mexican Americans. Nat Genet. 1999;21:213–215. doi: 10.1038/6002. [DOI] [PubMed] [Google Scholar]