Abstract
Background
Chronically ill people experience frequent changes in health status accompanied by multiple transitions between care settings and care providers. Discharge planning provides support services, follow-up activities, and other interventions that span pre-hospital discharge to post-hospital settings.
Objective
To determine if discharge planning is effective at reducing health resource utilization and improving patient outcomes compared with standard care alone.
Data Sources
A standard systematic literature search was conducted for studies published from January 1, 2004, until December 13, 2011.
Review Methods
Reports, randomized controlled trials, systematic reviews, and meta-analyses with 1 month or more of follow-up and limited to specified chronic conditions were examined. Outcomes included mortality/survival, readmissions and emergency department (ED) visits, hospital length of stay (LOS), health-related quality of life (HRQOL), and patient satisfaction.
Results
One meta-analysis compared individualized discharge planning to usual care and found a significant reduction in readmissions favouring individualized discharge planning.
A second meta-analysis compared comprehensive discharge planning with postdischarge support to usual care. There was a significant reduction in readmissions favouring discharge planning with postdischarge support. However, there was significant statistical heterogeneity.
For both meta-analyses there was a nonsignificant reduction in mortality between the study arms.
Limitations
There was difficulty in distinguishing the relative contribution of each element within the terms “discharge planning” and “postdischarge support.” For most studies, “usual care” was not explicitly described.
Conclusions
Compared with usual care, there was moderate quality evidence that individualized discharge planning is more effective at reducing readmissions or hospital LOS but not mortality, and very low quality evidence that it is more effective at improving HRQOL or patient satisfaction.
Compared with usual care, there was low quality evidence that the discharge planning plus postdischarge support is more effective at reducing readmissions but not more effective at reducing hospital LOS or mortality. There was very low quality evidence that it is more effective at improving HRQOL or patient satisfaction.
Plain Language Summary
Chronically ill people experience frequent changes in their health status and multiple transitions between care settings and care providers (e.g., hospital to home). Discharge planning provides support services, follow-up activities and other interventions that span pre-hospital discharge to post-hospital settings.
A review of the effects of different discharge plans was conducted. After searching for relevant studies, 11 studies were found that compared discharge planning with routine discharge care.
This review indicates that:
Individualized discharge planning reduces initial hospital length of stay and subsequent readmission to hospital but does not reduce mortality. The effect on health-related quality of life (HRQOL) or patient satisfaction is uncertain.
Discharge planning plus postdischarge support reduces readmissions but does not reduce the initial hospital length of stay or mortality after discharge. The effect on HRQOL or patient satisfaction is uncertain.
Background
In July 2011, the Evidence Development and Standards (EDS) branch of Health Quality Ontario (HQO) began developing an evidentiary framework for avoidable hospitalizations. The focus was on adults with at least 1 of the following high-burden chronic conditions: chronic obstructive pulmonary disease (COPD), coronary artery disease (CAD), atrial fibrillation, heart failure, stroke, diabetes, and chronic wounds. This project emerged from a request by the Ministry of Health and Long-Term Care for an evidentiary platform on strategies to reduce avoidable hospitalizations.
After an initial review of research on chronic disease management and hospitalization rates, consultation with experts, and presentation to the Ontario Health Technology Advisory Committee (OHTAC), the review was refocused on optimizing chronic disease management in the outpatient (community) setting to reflect the reality that much of chronic disease management occurs in the community. Inadequate or ineffective care in the outpatient setting is an important factor in adverse outcomes (including hospitalizations) for these populations. While this did not substantially alter the scope or topics for the review, it did focus the reviews on outpatient care. HQO identified the following topics for analysis: discharge planning, in-home care, continuity of care, advanced access scheduling, screening for depression/anxiety, self-management support interventions, specialized nursing practice, and electronic tools for health information exchange. Evidence-based analyses were prepared for each of these topics. In addition, this synthesis incorporates previous EDS work, including Aging in the Community (2008) and a review of recent (within the previous 5 years) EDS health technology assessments, to identify technologies that can improve chronic disease management.
HQO partnered with the Programs for Assessment of Technology in Health (PATH) Research Institute and the Toronto Health Economics and Technology Assessment (THETA) Collaborative to evaluate the cost-effectiveness of the selected interventions in Ontario populations with at least 1 of the identified chronic conditions. The economic models used administrative data to identify disease cohorts, incorporate the effect of each intervention, and estimate costs and savings where costing data were available and estimates of effect were significant. For more information on the economic analysis, please contact either Murray Krahn at murray.krahn@theta.utoronto.ca or Ron Goeree at goereer@mcmaster.ca.
HQO also partnered with the Centre for Health Economics and Policy Analysis (CHEPA) to conduct a series of reviews of the qualitative literature on “patient centredness” and “vulnerability” as these concepts relate to the included chronic conditions and interventions under review. For more information on the qualitative reviews, please contact Mita Giacomini at giacomin@mcmaster.ca.
The Optimizing Chronic Disease Management in the Outpatient (Community) Setting mega-analysis series is made up of the following reports, which can be publicly accessed at http://www.hqontario.ca/evidence/publications-and-ohtac-recommendations/ohtas-reports-and-ohtac-recommendations.
Optimizing Chronic Disease Management in the Outpatient (Community) Setting: An Evidentiary Framework
Discharge Planning in Chronic Conditions: An Evidence-Based Analysis
In-Home Care for Optimizing Chronic Disease Management in the Community: An Evidence-Based Analysis Continuity of Care: An Evidence-Based Analysis
Advanced (Open) Access Scheduling for Patients With Chronic Diseases: An Evidence-Based Analysis
Screening and Management of Depression for Adults With Chronic Diseases: An Evidence-Based Analysis
Self-Management Support Interventions for Persons With Chronic Diseases: An Evidence-Based Analysis
Specialized Nursing Practice for Chronic Disease Management in the Primary Care Setting: An Evidence-Based Analysis
Electronic Tools for Health Information Exchange: An Evidence-Based Analysis
Health Technologies for the Improvement of Chronic Disease Management: A Review of the Medical Advisory Secretariat Evidence-Based Analyses Between 2006 and 2011
Optimizing Chronic Disease Management Mega-Analysis: Economic Evaluation
How Diet Modification Challenges Are Magnified in Vulnerable or Marginalized People With Diabetes and Heart Disease: A Systematic Review and Qualitative Meta-Synthesis
Chronic Disease Patients’ Experiences With Accessing Health Care in Rural and Remote Areas: A Systematic Review and Qualitative Meta-Synthesis
Patient Experiences of Depression and Anxiety With Chronic Disease: A Systematic Review and Qualitative Meta-Synthesis
Experiences of Patient-Centredness With Specialized Community-Based Care: A Systematic Review and Qualitative Meta-Synthesis
Objective of Analysis
The objective of this analysis was to determine if discharge planning bundles (e.g., support services, follow-up activities, and other interventions that span pre-hospital discharge to the home setting) are effective at reducing health resource utilization and improving patient outcomes compared with usual care alone.
Clinical Need and Target Population
Chronically Ill People and Transitions Between Care Settings
Chronically ill people experience frequent changes in health status accompanied by multiple transitions between care settings and care providers. (1) It is during these transitions that mistakes frequently occur, for example, information about medication that a patient was prescribed while in hospital may not be accurately communicated to the family physician. Transitions may also give rise to adverse clinical events, patients’ serious needs not being met, and poor satisfaction with care. (1)
Transitions have also been reported to be associated with increased rates of potentially avoidable hospitalizations. (1) Innovative solutions that aim to improve integration and continuity across episodes of care discourage patterns of frequent use of health care services among the chronically ill and address the negative effects on quality and costs. Such solutions are referred to as “discharge planning.”
Discharge Planning
The few definitions of hospital discharge planning indicate that this is a process that takes place between hospital admission and the discharge event. (2) Pre-hospital discharge and communication is important as a start to the discharge planning process: it provides an opportunity to summarize the visit, teach patients how to safely care for themselves at home, and address any remaining questions or concerns. Discharge planning helps patients communicate with caregivers and primary care providers about how best to manage their chronic needs after leaving the hospital.
(3)
The emphasis on discharge planning varies between countries. (4) Discharge planning is mandatory in the United States in hospitals that participate in the Medicare and Medicaid programmes. In the United Kingdom, the Department of Health has published guidelines on discharge practice for health and social care. However, procedures vary between specialities in the same hospital, and discharge planning may be embedded in another intervention, such as specialized assessment units. (4) These differences make it difficult to interpret data on the effectiveness of discharge planning.
Ontario Context
There is a process for discharge planning in approximately 80%–90% of hospitals in Ontario. However, this practice is not standardized throughout the province. It is likely more of an organic process with varying elements tailored to suit the needs of the community(e.g., some hospitals may have discharge planners and some may use the services of Community Care Access Centres in order to try and bridge the care a patient receives from the hospital to that from their health care provider).
Evidence-Based Analysis
Research Questions
What is the effectiveness of discharge planning bundles at reducing health resource utilization and improving patient outcomes compared to usual care alone?
Research Methods
Literature Search
Search Strategy
A literature search was performed on December 13, 2011, using OVID MEDLINE, OVID MEDLINE In-Process and Other Non-Indexed Citations, OVID EMBASE, EBSCO Cumulative Index to Nursing & Allied Health Literature (CINAHL), the Wiley Cochrane Library, and the Centre for Reviews and Dissemination database for studies published from January 1, 2004, until December 13, 2011. Studies published from 2004 onwards were of interest because a meta-analysis of discharge planning for patients with heart failure was published in that year. Abstracts were reviewed by a single reviewer and, for those studies meeting the eligibility criteria, full-text articles were obtained. Reference lists were also examined for any additional relevant studies not identified through the search.
Inclusion Criteria
English language full-text reports
published between January 1, 2004, and December 13, 2011
randomized controlled trials (RCTs), systematic reviews, and meta-analyses
enrolled adult patients
≥ 1 month follow-up
-
limited to identified chronic conditions
– chronic obstructive pulmonary disease (COPD)
– coronary artery disease (CAD)
– congestive heart failure
– atrial fibrillation
– diabetes
– stroke
– chronic wounds
-
also included general terms
– chronic conditions
– multiple chronic conditions/multi-morbidity
explicitly described bundles of services to ensure transition from inpatient to community (outpatient) care (e.g., discharge planning, support services, follow-up activities, monitoring and/or other interventions that span pre-hospital discharge to the home setting)
Exclusion Criteria
studies where discrete results on discharge planning cannot be extracted
studies that examined pediatric patients
observational studies
Outcomes of Interest
mortality/survival
acute hospital admissions (readmissions)
emergency department (ED) visits
hospital length of stay (LOS)
health-related quality of life (HRQOL)
functional status
disease-specific clinical measures
patient satisfaction
Quality of Evidence
The quality of the body of evidence for each outcome is examined according to the GRADE Working Group criteria. (5) The overall quality is determined to be very low, low, moderate or high using a step-wise, structural methodology.
Study design is the first consideration; the starting assumption is that RCTs are high quality, whereas observational studies are low quality. Five additional factors—risk of bias, inconsistency, indirectness, imprecision and publication bias—are then taken into account. Limitations or serious limitations in these areas result in downgrading the quality of evidence. Finally, 4 factors are considered which may raise the quality of evidence: large magnitude of effect, dose response gradient and accounting for all residual confounding. (5) For more detailed information, please refer to the latest series of GRADE articles. (5)
As stated by the GRADE Working Group, the final quality score can be interpreted using the following definitions:
| High | Very confident that the true effect lies close to that of the estimate of the effect |
| Moderate | Moderately confident in the effect estimate – the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different |
| Low | Confidence in the effect estimate is limited – the true effect may be substantially different from the estimate of the effect |
| Very Low | Very little confidence in the effect estimate – the true effect is likely to be substantially different from the estimate of effect |
Results of Evidence-Based Analysis
The database search yielded 2,707 citations published between January 1, 2004, and December 13, 2011 (with duplicates removed). Articles were excluded based on information in the title and abstract. The full texts of potentially relevant articles were obtained for further assessment. Figure 1 shows the breakdown of when and for what reason citations were excluded in the analysis.
Figure 1: Citation Flow Chart.
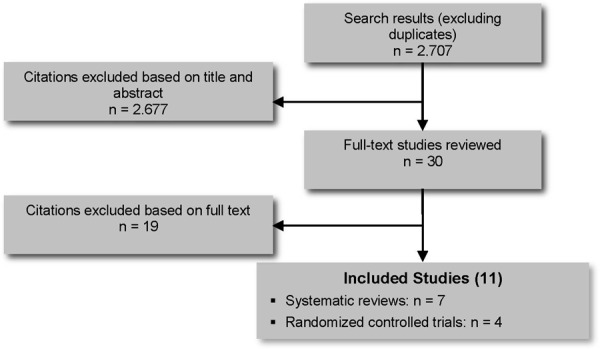
Eleven studies (7 systematic reviews and 4 RCTs) met the inclusion criteria.
For each included study, the study design was identified. These are summarized in Table 1, which is a modified version of a hierarchy of study design by Goodman. (6)
Table 1: Body of Evidence Examined According to Study Design.
| Study Design | Number of Eligible Studies |
|---|---|
| RCT Studies | |
| Systematic review of RCTs | 7 |
| Large RCT | 4 |
| Small RCT | |
| Observational Studies | |
| Systematic review of non-RCTs with contemporaneous controls | |
| Non-RCT with non-contemporaneous controls | |
| Systematic review of non-RCTs with historical controls | |
| Non-RCT with historical controls | |
| Database, registry, or cross-sectional study | |
| Case series | |
| Retrospective review, modelling | |
| Studies presented at an international conference | |
| Expert opinion | |
| Total | 11 |
Abbreviation: RCT, randomized controlled trial
Systematic Reviews
Table 2 includes a summary of the results and limitations for the 7 systematic reviews. (1;4;7-11) Four of these (1;8-10) were of low quality for a number of reasons including a lack of reported literature search cut-off dates; a lack of critical assessments of the studies in the narrative reviews; an unbalanced focus on studies that showed positive effects of discharge planning; the inclusion of numerous studies written by the lead author of the systematic review; the inclusion of grey literature; and uncritical narrative review of systematic reviews.
Table 2: Summary of Systematic Reviews.
| Author, Year, Country | Purpose | Inclusion Criteria | Results | Conclusion | Limitations |
|---|---|---|---|---|---|
| Hansen et al, 2011 (7) United States Literature search up to January 2011 |
Describe interventions evaluated in studies aimed at reducing rehospitalization within 30 days of discharge | RCTs (the authors also included observational studies, but HQO did not examine them in this analysis) Adults Interventions did not require disease-specific approaches (e.g., measurement of brain natriuretic peptide before HF discharge) |
43 studies (16 RCTs) identified and divided into: -predischarge interventions; -patient education, medication reconciliation, discharge planning, and scheduling of follow-up appointments before discharge; -postdischarge interventions; -follow-up telephone calls, patient-activated hotlines, timely communication with ambulatory providers, timely ambulatory provider follow-up, and postdischarge home visits; -bridging interventions; and -transition coaches, physician continuity across the inpatient and outpatient setting, and patient-centred discharge instruction. 5 of 16 RCTs documented statistically significant improvement in rehospitalization outcomes within 30 days. Of these 5 trials, 1 consisted of a single intervention in which high-risk patients received early discharge planning or usual care; the treatment group experienced an absolute 11 percentage point reduction in 30-day rehospitalization. The remaining 4 RCTs tested multicomponent discharge bundles. However, 1 RCT did not report results for 30-day readmission but for 2 weeks, and 1 RCT combined readmission and ED visits. The 2 remaining RCTs demonstrated absolute reductions in 30-day readmission of between 3.6 and 6.0 percentage points. The patient-centred discharge instructions and postdischarge telephone call were included in all 4 RCTs showing significantly effective discharge bundles. |
No single intervention implemented alone was regularly associated with reduced risk for 30-day rehospitalization. | Inadequate description of individual studies’ interventions precluded meta-analysis of effects. Many studies were single-institution assessments of quality improvement activities rather than those with experimental designs. Several interventions have not been studied outside of multicomponent “discharge bundles.” |
| Naylor et al, 2011 (1) United States Literature search cut-off date not reported |
To identify and synthesize available evidence regarding discharge planning for adult, chronically ill populations | RCTs conducted in the United States Adults |
21 RCTs identified. Naylor et al focused on 9 studies (3 of which were by the lead author) demonstrating positive effects of discharge planning on readmissions. “Because a key aim of the Affordable Care Act is to reduce avoidable hospital readmissions, we were particularly interested in the 9 interventions that reported a statistically significant positive effect on at least one measure of readmissions…” All but 1 of the 9 studies reported reductions in all-cause readmissions through at least 30 days after discharge. Of the remaining 8 interventions, 3 found positive, long-term effects in all-cause readmissions through 6 or 12 months following the index hospital discharge. These included 2 comprehensive discharge planning and follow-up interventions with home visits that were conducted by the lead author of the systematic review. The third intervention was a telehealth-facilitated intervention in which HF patients received either a videophone or telephone postdischarge support program. The study reported reduced all-cause readmissions through 12 months only when the 2 interventions groups were combined. There were no differences between the intervention group and the control group at 3 or 6 months. Discharge planning was not examined in this study. |
“Our evidence review reveals nearly a dozen interventions that have demonstrated some positive effect on hospital readmissions.” | No overall systematic assessment of the 21 RCTs. Authors focused solely on the 9 studies that demonstrated positive effects of discharge planning on readmissions. Seven of the 21 studies focused on discharge management plus follow-up. Meta-analysis was not conducted due to heterogeneity of study design. “The nature and practice of transitional care is evolving, and a standardized definition has not yet been established. The Affordable Care Act’s interpretation of transitional care is broad, so we chose to be inclusive in our search. Thus the interventions retained in our synthesis are diverse and in some cases could reasonably be categorized in other ways (for example, as telehealth and case management interventions).” |
| Shepperd et al, 2010 (4) United Kingdom Literature search up to March 2009 |
To determine the effectiveness of planning the discharge of patients moving from hospital | RCTs that compared an individualized discharge plan with routine discharge care that was not tailored to the individual patient | 21 RCTs (7,234 patients). Follow-up ranged from 2 weeks to 9 months. Readmission to hospital was significantly reduced for patients allocated to discharge planning (readmission rates RR, 0.85; 95% CI, 0.74–0.97, 11 trials). For elderly patients with a medical condition (usually HF), there was insufficient evidence for a difference in mortality (RR, 1.04; 95% CI, 0.74–1.46, 4 trials). In 3 trials, patients allocated to discharge planning reported increased satisfaction. |
A structured discharge plan tailored to the individual patient probably brings about small reductions in readmission rates for older people admitted to hospital with a medical condition. The impact of discharge planning on mortality and health outcomes remains uncertain. | Key issue in interpreting the evidence is the definition of the intervention and the subsequent understanding of the relative contribution of each element. It was not possible to assess how some components of the process compared between trials. Inclusion of the caregiver or family was mentioned by some of the trials, but the degree to which this was done was not always apparent or reported. Monitoring of patient discharge planning differed (e.g., telephone or visiting primary care clinics). Three trials examined the effectiveness of a pharmacy discharge plan. The context in which an intervention such as discharge planning is delivered may also play a role, not only in the way the intervention is delivered, but in the way services are configured for the control group. Orientation of primary care services differs between countries, which may affect communication between services. Different perceptions of care by professionals of alternative care settings and country-specific funding arrangements may also influence discharge. Two studies reported discharge planning commencing from the time a patient was admitted to hospital, and another reported that discharge planning was implemented 3 days prior to discharge. The timing of delivery of discharge planning, which depends on other services, will have some bearing on how quickly these services can begin providing care. The patient population may also impact outcome (e.g., patients experiencing major complications from their chronic disease combined with an intervention designed to increase the intensity of primary care services may explain the observed increase in readmission days for those receiving the intervention.) Shepperd et al excluded RCTs evaluating interventions where discharge planning was not the main focus of a multifaceted package of care. |
| Scott, 2010 (8) Australia Literature search up to March 2009 |
To determine the relative efficacy of peridischarge interventions categorized into 2 groups: -single component interventions (sole or predominant) implemented either before or after discharge -integrated multicomponent interventions that have pre- and postdischarge elements |
Controlled trials or systematic reviews that reported data on interventions targeting hospitalized patients and measured readmission rates | 7 systematic reviews were key sources of data for analysis. Studies (not all RCTs) summarized as a narrative review. Formal meta-analysis not applied due to considerable study heterogeneity in design and outcome measures. Single component interventions that reduced readmissions: -intense self-management -transition coaching of high-risk patients -nurse home visits Telephone support of patients with HF Multicomponent interventions that reduced readmissions: -early assessment of discharge needs -enhanced patient and caregiver education and counselling -early postdischarge follow-up of high-risk patients |
Peridischarge interventions are highly heterogeneous and reported outcomes show considerable variation. Multicomponent interventions targeted at high-risk populations that include pre- and postdischarge elements seem to be more effective in reducing readmissions than most single component interventions that do not span the hospital-community interface. |
No critical review of single studies within the systematic review was undertaken Non-RCTs included in some of the systematic reviews “It is not an exhaustive systematic review of all individual trials of clinical interventions that relate to discharge processes in some way.” |
| Kumar and Grimmer-Somers, 2007 (9) Australia Literature search cut-off dates not reported |
To systematically evaluate the secondary literature on hospital avoidance and discharge programs using a framework of best practice principles in health care (safety, effectiveness, timeliness, equity, efficiency, and patient-centredness) | Systematic reviews and grey literature reflecting the descriptive reviews of published and unpublished literature Patients of any age and with any condition who had been discharged from hospital to home RCTs and observational studies |
48 publications “Overall, the health outcome, hospital LOS, and readmission rates associated with community/home-based care were no worse than those derived from hospital-based care. However, patients and caregivers mostly preferred care provided out of hospital, and this was often reflected in positive functional change and improved satisfaction scores.” |
“While there was evidence for improved patient-centred outcomes, the evidence for safety, effectiveness, and efficiency of hospital avoidance and discharge programs was equivocal.” | Lack of description in many of the publications of “standard hospital care” as a comparator |
| Mistiaen et al, 2007 (10) Netherlands Literature search up to November 2006 |
To systematically examine reviews of the effectiveness of interventions aimed at reducing postdischarge problems in adults discharged home from an acute general care hospital | Systematic reviews Adult patients hospitalized primarily for a physical problem. Outcomes measured include patient status at discharge, patient functioning within 3 months of discharge, or health care service use and costs after discharge |
15 systematic reviews All reviews dealt with considerable heterogeneity in interventions, populations and outcomes making synthesizing and pooling difficult. Although a statistically significant effect was occasionally found, most review authors reached no firm conclusions about the effectiveness of the discharge interventions. Limited evidence that some interventions may improve patients’ knowledge, may help in keeping patients at home, or may reduce readmissions to hospital Interventions that combine discharge planning and discharge support tend to lead to the greatest effects. There is little evidence that discharge interventions have an impact on hospital LOS, discharge destination, or dependency at discharge. No evidence that discharge interventions have a positive impact on the physical status of patients after discharge or on health care use after discharge. |
Based on 15 high quality systematic reviews, there is some evidence that some interventions, particularly those with educational components and those that combine predischarge and postdischarge interventions, may have a positive impact. However, on the whole there is limited summarized evidence that discharge planning and discharge support interventions have a positive impact on patient status at hospital discharge, on patient functioning after discharge, or on health care use after discharge and costs. | “The umbrella concept of ‘discharge interventions’ is too broad to endeavour synthesizing by means of a review of systematic reviews already dealing with vast heterogeneity.” Poor description of interventions and control conditions |
| Phillips et al, 2004 (11) United States Literature search up to October 2003. |
To evaluate the effect of comprehensive discharge planning plus postdischarge support on the rate of readmission, all-cause mortality, hospital LOS, and HRQOL | RCTs that described interventions to modify hospital discharge for older patients with HF compared with usual care Studies with clearly defined inpatient and outpatient components Studies that reported readmission as the primary outcome |
18 RCTs (3,304 patients) Mean follow-up 8 months (range 3–12 months) Intervention vs. usual care: Readmission 555/1590 vs. 741/1714 RR, 0.75; 95% CI, 0.64–0.88 All-cause mortality RR, 0.87; 95% CI, 0.73–1.03; n = 14 studies Percent improvement in HRQOL scores compared with baseline 25.7% (95% CI, 11.0%–40.4%) vs. 13.5% (95% CI, 5.1%–22.0%), n = 6, P = 0.01 |
Comprehensive discharge planning plus postdischarge support for older patients with HF significantly reduced readmission rates and may improve health outcomes such as survival and HRQOL. | For most studies, usual care was not explicitly described. No studies evaluated the efficacy of comprehensive discharge planning without components for postdischarge support for patients with HF. The duration of components for postdischarge support was not consistently reported and varied by study. Components for postdischarge support varied by study. Unable to ascertain whether events that occurred distant from the index discharge were related to the initial DRG or new problems for patients who were readmitted or those who died. |
Abbreviations: CI, confidence interval; DRG, diagnosis related group; ED, emergency department; HF, heart failure; HQO, Health Quality Ontario; HRQOL, health-related quality of life; LOS, length of stay; RCT, randomized controlled trial; RR, relative risk.
Overall General Results of Published Meta-Analyses
Of the 3 high quality systematic reviews, 2 included a meta-analysis. (4;11) Hansen et al (7) did not conduct a meta-analysis because “inadequate description of individual studies’ interventions precluded meta-analysis of effects.”
Table 3 shows a comparison of the summary statistics reported in the meta-analyses. Shepperd et al (4) compared individualized discharge planning with usual care, and Phillips et al (11) compared comprehensive discharge planning plus postdischarge support to usual care. There was a significant reduction in readmissions favouring individualized discharge planning compared with usual care (with no significant statistical heterogeneity). There was also significant reduction in readmissions favouring discharge planning with postdischarge support compared with usual care, though in this case heterogeneity was significant (despite that Phillips et al (11) removed a large study from the meta-analysis due to significant heterogeneity).
Table 3: Results of Two Meta-Analyses – Comparison of Individualized Discharge Planning Versus Usual Care and Comprehensive Discharge Planning With Postdischarge Support Versus Usual Care.
| Intervention/Author | Summary Statistic RR (95% CI) |
Number of RCTs | N | Heterogeneity P Value |
|---|---|---|---|---|
| Readmission to Hospital | ||||
| Individualized discharge planning Shepperd et al, 2009a (4) |
0.85 (0.74–0.97) (Follow-up from 2 weeks to 9 months) |
11 | 2,552 | 0.47 |
| Individualized discharge planning WITH postdischarge support Phillips et al, 2004b (11) |
0.74 (0.67–0.81) (Follow-up from 3–12 months; mean, 8 months) |
17 | 2,941 | 0.04 (significant heterogeneity remained even after a large study was removed due to considerable significant heterogeneity [P < 0.001] in 18 studies) |
| Mortality | ||||
| Individualized discharge planning Shepperd et al, 2009a (4) |
1.04 (0.74–1.46) | 4 | 978 | 0.44 |
| Individualized discharge planning WITH postdischarge support Phillips et al, 2004 (11) |
0.87 (0.73–1.03) | 14 | 2,847 | 0.06 |
| Length of Stay | ||||
| Individualized discharge planning Shepperd et alb, 2009 (4) |
Mean difference –0.91 (–1.55 to –0.27) | 10 | 1,765 | 0.50 |
| Individualized discharge planning WITH postdischarge support Phillips et al, 2004 (11) |
Mean difference –0.37 (–0.15 to 0.60) | 10 | 1,682 | Not reported |
Abbreviations: CI, confidence interval; RCT, randomized controlled trials; RR, relative risk.
This systematic review specifically focused on discharge planning. Studies were excluded if it was not possible to separate the effects of discharge planning from the other components of the intervention, if discharge planning appeared to be a minor part of a multifaceted intervention, or if the focus was on the provision of care after discharge from hospital. The control group had to receive standard care with no structured discharge planning.
Included studies specifically addressed congestive heart failure, described components for inpatient care plus postdischarge support, compared the effects with usual care, and reported readmission rates as the primary outcome.
For both meta-analyses, there was a nonsignificant reduction in mortality between the study arms.
Shepperd et al (4) found a significant difference in the hospital LOS favouring individualized discharge planning. Conversely, Phillips et al (11) did not find a significant difference in LOS between discharge planning with postdischarge support compared with usual care.
Detailed Results of Published Systematic Reviews
Systematic Review of Interventions Aimed at Reducing 30-Day Rehospitalization
The objective of the most recent systematic review identified in the literature search was to describe interventions evaluated in studies aimed at reducing rehospitalization within 30 days of discharge. (7) Hansen et al. (7) identified 16 RCTs (12-27) from a literature search that spanned from January 1975 to January 2011. Because of the overlapping nature of intervention components and the heterogeneity of interventions in these included studies, meta-analysis of interventions was not feasible and the authors reported a narrative synthesis.
The authors developed a taxonomy for categorizing individual components of interventions into 3 groups:
Predischarge interventions
Postdischarge interventions
Interventions active both before and after discharge as a “bridge” across care settings. These “bridge interventions” provided a longitudinal service with activity spanning the pre- and postdischarge periods.
Table 4 shows a listing of interventions in each of the 3 categories.
Table 4: Summary of Interventions Tested in Randomized Controlled Trials Included in Systematic Review.
| Author, Year, Size, Country | Population | Interventions | EPOC Quality Criteria Satisfied (9 possible), n | Absolute Risk Reduction, percentage points | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predischarge Interventions | Postdischarge Interventions | Interventions Bridging the Transition | |||||||||||||
| Patient Education | Discharge Planning | Medication Reconciliation | Appointment Scheduled Before Discharge | Timely PCP Communication | Timely Clinic Follow-up | Follow-up Telephone Call | Postdischarge Hotline | Home Visit | Transition Coach | Patient-Centred Discharge Instructions | Provider Continuity | ||||
| Balaban et al, 2008 (12) N = 96 United States |
Community hospital | X | X | X | 5 | –0.3 | |||||||||
| Braun et al, 2009 (13) N = 309 Israel |
General medicine ward | X | 5 | 0.5 | |||||||||||
| Coleman et al, 2006 (14) N = 750 United Sates |
Geriatric | X | X | X | X | 5 | 3.6a | ||||||||
| Dudas et al, 2001 (15) N = 221 United States |
General medicine ward | X | 4 | 10 | |||||||||||
| Dunn et al, 1994 (16) N = 59 United Kingdom |
Geriatric | X | 4 | –2 | |||||||||||
| Evans et al, 1993 (17) N = 835 United States |
Veterans Affairs; high risk | X | 4 | 11.0a | |||||||||||
| Forster et al, 2005 (18) N = 620 Canada |
General medicine ward | X | 5 | –7.8 (readmission or death) | |||||||||||
| Jaarsma et al, 1999 N = 179 Netherlands |
HF | X | X | X | X | X | 5 | 2 | |||||||
| Jack et al, 2009 N = 738 United States |
Medical/ surgical ward | X | X | X | X | X | X | 6 | 6.0a | ||||||
| Koehler et al, 2009 (21) N = 41 United States |
Geriatric, high risk | X | X | X | X | X | X | X | 6 | 28.1a (readmission or ED visit) | |||||
| Kwok et al, 2004 (22) N = 149 Hong Kong |
Chronic lung disease, geriatric | X | X | 6 | –10 | ||||||||||
| McDonald et al, 2001 (23) N = 70 Ireland |
HF, geriatric | X | X | 4 | 0 | ||||||||||
| Naylor et al, 1994 (24) N = 142 United States |
Cardiac (medical/surgical), geriatric | X | X | X | X | X | X | 5 | 12.0a (2 weeks, medical); 4 (surgical) | ||||||
| Parry et al, 2009 N = 98 (25) United States |
Geriatric | X | X | X | X | X | X | X | 7 | 9.9 | |||||
| Rainville, 1999 (26) N = 34 United States |
HF | X | 7 | 7.1 | |||||||||||
| Wong et al, 2008 (27) N = 332 Hong Kong |
General medicine ward | X | 5 | 2.4 | |||||||||||
Abbreviations: ED, emergency department; EPOC, Effective Practice and Organization of Care Group; HF, heart failure; PCP, primary care provider.
Statistically significant improvement in rehospitalization outcomes within 30 days.
Source: Hansen et al, 2011 (7)
Of the 16 RCTs Hansen et al. (7) identified, 5 documented a statistically significant improvement in rehospitalization outcomes within 30 days. (14;17;20;21;24) One of the 5 trials consisted of a single intervention in which high-risk patients received early discharge planning or usual care; the treatment group experienced an absolute 11 percentage point reduction in 30-day rehospitalization. (17) Hansen et al (7) stated that isolated interventions may have small effects, but bundled interventions may have an additive effect or additional value through change in cultural or organizational factors.
The remaining 4 RCTs tested multicomponent discharge bundles. However, Naylor et al (24) did not report results for 30-day readmission (results were reported at 2 weeks), and Koehler et al (21) combined readmission and ED visits. The 2 remaining RCTs (14;20) demonstrated absolute reductions in 30-day readmission of between 3.6 and 6.0 percentage points. Interventions common to these 4 RCTs were the postdischarge telephone call (either by a hospital, or more usually, a nurse from the primary provider’s office) and patient-centred discharge instructions. However, 2 separate RCTs (12;25) that included these 2 interventions with others in a bundle did not show significant reductions in rehospitalization within 30 days, and 2 RCTs that tested them in isolation found no effect. (13;15) This difference, along with the higher frequency of bundled interventions in RCTs showing effect, may suggest limited efficacy of isolated interventions.
Eleven RCTs identified in the review by Hansen et al (7) did not show a significant effect of isolated or bundled interventions. These included negative studies of isolated application of discharge planning (18), patient education (26), home visits (16;27), and postdischarge telephone calls. (13;15)
Limitations to the systematic review included the following:
Diverse interventions or scant details which made it difficult to analyze the relative efficacy of individual interventions. Staffing and scope of intervention components or the population targeted for intervention varied between studies, and in particular for patient education and discharge planning.
A paucity of high quality RCTs. The 2 highest quality studies (25;26), which scored 7 out of 9 on the Cochrane Collaboration’s Effective Practice and Organization of Care (EPOC) Group Risk of Bias Criteria used by the authors, did not demonstrate a significantly reduced 30-day rehospitalization in the intervention groups. Details about the quality of the studies are shown in Appendix 2, Table A2-1.
The RCTs examining the effectiveness of discharge planning care predominantly focused on the academic health care environment, and the results may not transfer to non-academic sites of care. (7) The importance of organizational context to organizational change raises concerns that many hospitals may be frustrated if they seek improvement by replicating the processes reviewed. (7)
Systematic Review of Discharge Planning From Hospital to Home
Shepperd et al (4) conducted a systematic review of RCTs to determine the effectiveness of planning patient discharge from hospital to home. The objectives were to determine the effectiveness of discharge planning on
unscheduled readmission rates compared with usual care
length of stay (LOS) in hospital compared with usual care
incidence of complications related to the initial admission compared with usual care
mortality rate compared with usual care
patient health outcomes compared with usual care
patients’ and caregivers’ satisfaction compared with usual care
The researchers defined discharge planning as the “development of an individualized discharge plan for a patient prior to them leaving hospital for home.” (4) The discharge planning process was divided into the following steps:
preadmission assessment (where possible);
case finding on admission;
inpatient assessment and preparation of a discharge plan based on individual patient needs, e.g., multidisciplinary assessment involving the patient and their family and communication between relevant professionals within the hospital;
implementation of the discharge plan;
monitoring.
Shepperd et al excluded those studies
that did not include an assessment and implementation phase of discharge planning;
where it was not possible to separate the effects of discharge planning from the other components of the intervention or if discharge planning appeared to be a minor part of a multifaceted intervention; and/or
if the focus was on the provision of care after discharge from hospital.
The control group had to receive standard care with no structured discharge planning. The literature search cut-off date was March 2009.
Shepperd et al (4) identified 21 RCTs (N = 7,234 patients), details of which are shown in Appendix 2, Tables A2-2 and A2-3. (12;17;20;24;28-44) Follow-up duration ranged from 2 weeks to 9 months. The trials evaluated a broadly similar intervention of discharge planning that included an assessment, planning, implementation and monitoring phase, although 6 trials (17;33;34;38;42;43) did not describe a monitoring phase. The interventions were implemented at different times during the patient’s stay in hospital, from admission to 3 days prior to discharge. Three trials (28;36;42) evaluated a pharmacy discharge plan implemented by a hospital pharmacy. The patient’s medication was rationalized, the family physician, community pharmacist, or both were sent a pharmacy discharge plan, and patients were given information about their medication.
The description of the type of care the control group received varied. One trial (31) did not describe the care received by the control group. Sixteen trials (12;17;20;24;29;30;32-35;37-41;44) described the control group as receiving usual care with some discharge planning but without a formal link through a coordinator to other departments and services although other services were available on request from nursing or medical staff. The control groups in the 3 trials (28;36;42) that evaluated the effectiveness of a pharmacy discharge plan did not have access to a review and discharge plan by a pharmacist. The control group in one trial (43) received multidisciplinary care that was not defined in advance but was determined by the patients’ progress.
Twelve RCTs reported adequate concealment of allocation. (20;29;31;34-36;38;39;41-44) All but 2 trials (12;37) collected data at baseline, and 15 trials reported blinded measurement of outcomes (mostly for objective outcomes such as hospital LOS and readmission). (12;17;20;30-38;40;41;44)
Results of discharge planning compared with usual care are shown in Table 5.
Table 5: Results of Discharge Planning Compared with Usual Care.
| Outcome | Summary Statistic (95% CI) | Number of Trials | N |
|---|---|---|---|
| Readmission within 3 months of discharge from hospital | RR, 0.85 (0.74–0.97) | 11 | 2,552 |
| Hospital LOS (days) | Mean difference, –0.91 (–1.55 to –0.27) | 10 | 1,765 |
| Mortality at 6–9 months | RR, 1.04 (0.74–1.46) | 4 | 978 |
Abbreviations: CI, confidence interval; LOS, length of stay; RCT, randomized controlled trial; RR, relative risk.
Source: Shepperd et al, 2009 (4)
Patients’ and caregivers’ satisfaction were reported in 3 studies. (33;36;44) Overall, results were inconsistent. Moher et al (33) reported on a subgroup of 40 patients; 18 in the treatment group and 21 in the control group responded. The difference in terms of their satisfaction was significantly in favour of the treatment group (89% vs. 62%; mean difference, 27%; 95% CI, 2% - 52%, P < 0.05) on day 4 of their hospital stay. Nazareth et al (36) reported results from a client satisfaction questionnaire, but found no significant difference between the treatment and control groups at 3- or 6-months’ follow-up. Weinberger et al (44) measured patient satisfaction at 1 and 6 months and found the intervention group significantly more satisfied than the control group (P < 0.001 at both time points).
Ten trials (17;24;29;31;36;37;39;41;43;44) measured patient outcomes including functional status, mental well-being, perception of health, self-esteem, and affect. Of these, 3 (24;31;44) did not report follow-up data, and 5 trials (17;29;36;37;39) observed no significant difference between study arms. Rich et al (41) reported a significant improvement on the total score for the Chronic Heart Failure Questionnaire (mean [SD] difference = 22.1 [20.8]); P < 0.01). Sulch et al (43) recruited patients recovering from a stroke and reported a significant functional improvement between 4 and 12 weeks’ follow-up for the control group using the Barthel score (median within-group change of 6 points for the control group vs. 2 points for the treatment group; P < 0.01). However, between-group differences of the Barthel score were not statistically significant. HRQOL measured using the EuroQol showed significant between-group differences at 26 weeks’ follow-up in favour of the control group (control group 72 points vs. treatment group 63 points; P < 0.005) but no differences were reported between groups for the Rankin score and the Hospital Anxiety and Depression Scale.
The systematic review by Shepperd et al (4) had a number of limitations:
The reporting of different outcomes restricted the ability to pool data.
-
A key issue in interpreting the evidence was the definition of the intervention and the subsequent understanding of the relative contribution of each element.
– Authors of the trials did describe the interventions, but it was not possible to assess how some components of the process compared between trials. For example, the trial by Naylor et al (24) formalized the inclusion of the patient’s caregiver into the assessment process and the development of the discharge plan. Inclusion of the caregiver or family was mentioned by some of the other trials (17;30-32;35), but the degree to which this was done was not always apparent.
– In terms of the discharge planning, one trial included a predischarge home visit by an occupational therapist and rehabilitation doctor, (37) another trial had hospital and community nurses working together on the discharge plan, (29) and 2 trials used an assessment tool to find cases eligible for discharge planning. (17;38)
The majority of trials included a patient education component within the discharge planning process.
The monitoring of discharge planning differed among trials. For example, one trial (24) did this primarily by telephone, while in another, (44) patients were given appointments to attend a primary care clinic.
Three trials evaluated the effectiveness of a pharmacy discharge plan. (28;36;42)
Assessing the extent to which contamination between the intervention and control groups occurred was difficult.
-
The context in which discharge planning is delivered may play a role not only for the intervention but in the way services are configured for the control group.
– Studies in the review were based in the United States, United Kingdom, Canada, Australia, Denmark, and France. In each country the orientation of primary care services differs in a way that may affect communication between services.
– Different perceptions of care by professionals of alternative care settings and country-specific funding arrangements may also influence discharge.
The point when discharge planning was implemented also varied across studies. For example, 2 trials (38;43) commenced discharge planning when patients were admitted to hospital, while another (44) implemented discharge planning 3 days prior to discharge.
The patient population may also affect outcome. For example, 99 patients in the trial by Weinberger et al (44) had major complications related to their chronic disease. This, together with an intervention designed to increase the intensity of primary care services, may explain the observed increase in readmission days for those receiving the intervention.
Systematic Review of Comprehensive Discharge Planning with Postdischarge Support for Older Patients with Congestive Heart Failure
Phillips et al (11) evaluated the effect of comprehensive discharge planning plus postdischarge support for patients with congestive heart failure. Outcomes of interest included:
rate of readmission
all-cause mortality
hospital LOS
HRQOL
Inclusion criteria consisted of RCTs that
described interventions to identify hospital discharge for older patients with congestive heart failure,
delineated clearly defined inpatient and outpatient components,
compared efficacy with usual care, and
reported readmission as the primary outcome.
The literature search cut-off date was October 2003.
The analysis included 18 RCTs. (19;24;26;29;32;40;41;44-55) Characteristics of these are shown in Appendix 2, Tables A2-4 and A2-5.
Studies were assessed for quality using the Jadad scale. The most common reason for point deduction was the absence of double blinding, which was impossible due to the nature of the interventions. Of the 18 studies, 16 received a Jadad score of 4 out of 5, whereas 2 (26;51) received a score of 3 because they did not report data for loss to follow-up and blinding. However, most studies reported blinded assessment of outcomes. The pooled attrition rate due to nonresponse, withdrawals, or loss to follow-up was less than 5%, except for 1 study (32) with a rate of 8%.
Overall, fewer patients in the intervention group had to be readmitted compared with usual care (RR, 0.75; 95% CI, 0.64–0.88; P for heterogeneity < 0.001). Most of the heterogeneity was accounted for by results from a single large study. When this was omitted from the analysis, heterogeneity was reduced but nevertheless remained significant (RR, 0.74; 95% CI, 0.67–0.81; P for heterogeneity = 0.04). Results for the studies are shown in Table 6.
Table 6: Readmission Rates with Comprehensive Discharge Planning Plus Postdischarge Support Compared with Usual Care.
| Author, Year | Intervention Events/Patients (%) | Control Events/Patients (%) | Absolute Risk Reduction, % | Relative Risk Reduction (95% CI) | P Value for Heterogeneity | Single or Combination (for “and/or” interventions) |
|---|---|---|---|---|---|---|
| Single Home Visit | ||||||
| Stewart et al, 1998 (45) | 24/49 (49) | 31/48 (65) | 16 | 0.76 (0.53–1.08) | NA | |
| Stewart et al, 1999 (46) | 40/100 (40) | 51/100 (51) | 11 | 0.78 (0.58–1.07) | NA | |
| Jaarsma et al, 1999 (19) | 31/84 (37) | 47/95 (49) | 12 | 0.75 (0.53–1.05) | NA | |
| Subtotal | 95/233 (41) | 129/243 (53) | 12 | 0.76 (0.63–0.93) | 0.97 | |
| Increased Clinic Follow-up and/or Frequent Telephone Contact | ||||||
| Cline et al, 1998 (47) | 22/80 (28) | 43/110 (39) | 13 | 0.70 (0.46–1.08) | Clinic only | |
| Rainville, 1999 (26) | 4/17 (24) | 10/17 (59) | 35 | 0.40 (0.16–1.03) | Telephone only | |
| Oddone et al, 1999 and Weinberger et al. 1996 (44;48) | 124/222 (56) | 97/221 (44) | 12+ | 1.27 (1.05–1.54) | Combination | |
| McDonald et al, 2002 (49) | 1/51 (2) | 11/47 (23) | 21 | 0.08 (0.01–0.62) | Telephone only | |
| Subtotal | 151/370 (41) | 161/395 (41) | 0 | 0.64 (0.32–1.28) | < 0.001 | |
| Home Visits and/or Frequent Telephone Contact | ||||||
| Naylor et al, 1994 (24) | 16/72 (22) | 23/70 (33) | 11 | 0.68 (0.39–1.17) | Combination | |
| Naylor et al, 1999 (50) | 18/52 (35) | 26/56 (46) | 11 | 0.75 (0.47–1.19) | Combination | |
| Serxner et al, 1998 (51) | 15/55 (27) | 27/54 (50) | 23 | 0.55 (0.33–0.91) | Telephone only | |
| Blue et al, 2001 (52) | 47/84 (56) | 49/81 (60) | 4 | 0.92 (0.71–1.20) | Combination | |
| Riegel et al, 2002 (53) | 56/130 (43) | 114/228 (50) | 7 | 0.86 (0.68–1.09) | Telephone only | |
| Krumholz et al, 2002 (54) | 16/44 (36) | 23/44 (52) | 16 | 0.69 (0.43–1.13) | Telephone only | |
| Subtotal | 168/437 (38) | 262/533 (49) | 11 | 0.79 (0.69–0.91) | 0.59 | |
| Extended Home Care Services | ||||||
| Rich et al, 1993 (40) | 21/63 (33) | 16/35 (46) | 12 | 0.73 (0.44–1.02) | NA | |
| Rich et al, 1995 (41) | 41/142 (29) | 59/140 (42) | 13 | 0.69 (0.50–0.95) | NA | |
| Harrison et al, 2002 (29) | 21/92 (23) | 31/100 (31) | 8 | 0.74 (0.46–1.19) | NA | |
| Laramee et al, 2003 (32) | 49/141 (35) | 46/146 (32) | 3+ | 1.10 (0.79–1.53) | NA | |
| Subtotal | 132/438 (30) | 152/421 (36) | 6 | 0.82 (0.68–1.00) | 0.19 | |
| Day Hospital Services (with specialized HF unit)(49) | ||||||
| Capomolla et al, 2002 (55) | 9/112 (8) | 37/122 (30 | 22 | 0.25 (0.15–0.44) | NA | |
| Total | 555/1590 (35) | 741/1714 (43) | 8 | 0.75 (0.64–0.88) | < 0.001 | |
Abbreviations: CI, confidence interval; HF, heart failure; RCT, randomized controlled trial; RR, relative risk; +, increased risk. Source: Phillips et al, 2004 (11)
The evidence did not support the implicit assumption of incremental efficacy with more intensive postdischarge interventions. Comparable benefit resulted from a home visit, home visits and/or frequent telephone follow-up, and extended home care services. Increased clinic visits and/or frequent telephone contact did not result in a significant decrease in readmission rates. Day hospital visits, of which there was only 1 study, yielded a significant reduction in readmissions compared with usual care.
The authors found no significant difference in baseline use of angiotensin-converting enzyme (ACE) inhibitors in 14 trials (P = 0.40). Only 3 studies assessed the use of ACE inhibitors during follow-up (32;44;47;48), and the data did not show a significantly higher rate of ACE inhibitor use among the intervention groups, although these studies also showed no overall effect of the intervention on readmission rates.
Data for all-cause mortality were reported in 14 studies. (19;26;29;32;41;44-48;52-55) There was no significant difference in all-cause mortality between the study arms (RR, 0.87; 95% CI, 0.73–1.03; P for heterogeneity = 0.06).
Ten studies (19;24;26;29;32;44-46;48;50) reported data for initial hospital LOS. This was similar for intervention and control patients (mean [standard error] 8.4 [2.5] vs. 8.5 [2.2] days, P = 0.60). The difference in LOS favoured intervention patients, but this difference was not statistically significant (difference –0.37; 95% CI, –0.15 to 0.60). Heterogeneity was not reported by the authors.
Six studies (19;29;41;46-48) reported data for HRQOL. All except for 2 used different measurement scales to assess this outcome. During 8 months of follow-up (range 3–12 months), HRQOL scores improved from baseline for patients in the intervention group (mean change, 25.7%; 95% CI, 11.0%–40.4%) and usual care group (mean change, 13.5%; 95% CI, 5.1%–22.0%), but the HRQOL scores of intervention patients improved significantly more than for the usual care patients (difference in mean change of scores, 12.2% [95% CI, 3.8%–20.6%], P = 0.01). Heterogeneity was not reported by the authors.
Limitations to the study by Phillips et al (11) included the following:
There was significant heterogeneity among studies.
Most studies did not explicitly describe usual care.
4 studies (26;40;41;52) did not report explicit data for the intervention duration.
The duration of components for postdischarge support varied by study and was not consistently reported.
For those studies that did not show a significant difference in readmission rates between comprehensive discharge planning with postdischarge support versus usual care, patients may already have been receiving optimal care, thereby minimizing the difference in effects of additional treatment.
Several of the studies did not collect or report information about secondary outcomes such as hospital LOS or HRQOL scores.
The optimal arrangement of components for individualized comprehensive discharge and postdischarge support was not determined.
Inability to ascertain whether events that occurred distant from the index hospitalization were related to the initial admission or were new problems for patients who were readmitted or who died.
Recent Studies Not Included in Systematic Reviews
Four identified RCTs were not included in the systematic reviews. (56-59) A summary of results for the 4 studies is shown in Table 7.
Table 7: Summary of Recent Studies Not Included in Systematic Reviews.
| Author, Year, Country | Intervention | Control | Results | Limitations |
|---|---|---|---|---|
| Atienza et al, 2004(59) Spain | n = 164 Patients and families received a predischarge formal education about disease from cardiac nurse Visit with primary care physician scheduled within 2 weeks of discharge Regular follow-up visits at the outpatient Heart Failure Clinic scheduled for every 3 months 24-hour phone contact number available to patients from discharge to end of study if patients experienced worsening symptoms |
n = 174 Discharge planning according to the routine protocol of the study hospitals |
Event-free survival Reduction of 47 events per 100 patients (95% CI, 29–65), P < 0.001 per year of observation in intervention patients Readmissions Reduction of 16% (95% CI, 4%–28%), P = 0.004 in rate of readmitted patients for any cause in intervention group Reduction of 37 all-cause readmissions per 100 patients (95% CI, 21–53), P < 0.001 per year of observation for intervention group Reduction of 19% (95% CI, 0.09–0.29), P < 0.001 in rate of readmitted patients for HF in intervention group Mortality Reduction of 10 deaths per 100 patients (95% CI, 0.02–0.18), P = 0.006 per observation year for intervention patients HRQOL at 1 year (Minnesota Quality of Life Score) Significantly higher improvement in intervention group (P = 0.01) |
Unable to identify which elements of the intervention are responsible beneficial results |
| Naylor et al, 2004 (56) United States |
n = 118 Comprehensive discharge planning and home follow-up directed by APNs APN visited at least daily during index hospitalization At least 8 APN home visits (one within 24 hours of discharge) Weekly visits during the first month (with one visit coinciding with the initial follow-up visit to the patient’s physician); bimonthly visits during the second and third months. Additional APN visits based on patients’ needs APN available by telephone 7 days/week |
n = 121 Usual care for the control group included site-specific HF-patient management and discharge planning critical paths, and if referred, standard home agency care consisting of comprehensive skilled home health services 7 days a week. |
Time to first rehospitalization or death Longer in intervention patients (log rank χ2 = 5.0, P = 0.03) Rehospitalization or death at 52 weeks Intervention (n = 118 patients) vs. control (n = 121 patients) 56 (48%) vs. 74 patients (61%), P = 0.01 Patients rehospitalized (1 time) Intervention (n = 118 patients) vs. control (n = 121 patients) 53 (44.9%) vs. 67 (55.4%), P = 0.12; RR, 1.24 (95% CI, 0.95–1.60) Rehospitalizations at 1 year Intervention (n = 104 rehospitalizations) vs. control (n = 162 rehospitalizations) Index related: 40 vs. 72, P = 0.18 Comorbidity related: 23 vs. 50, P = 0.01 New health problem: 41 vs. 40, P = 0.88 HRQOL At 12 weeks, intervention group reported greater overall HRQOL (P < 0.05) No significant difference observed at other time points Functional status No significant difference observed at any time point Satisfaction with care Greater in intervention patients at 2 and 6 weeks (P < 0.001) No other time periods reported |
Significantly more patients with hypertension in the control group than the treatment group, 71/121 (59%) vs. 54/121 (45%); P = 0.04 The primary outcome was time to first event (a combination of any cause readmission or death). There may not have been sufficient statistical power for assessment of some secondary outcomes e.g., patients rehospitalized or index-related rehospitalization at 1 year |
| Kwok et al, 2008 (57) China |
n = 49 Community nurse visited before discharge, within 7 days of discharge, weekly for 4 weeks, then monthly Community nurses worked closely with designated hospital geriatricians or cardiologists; counselled patients on drug compliance and diet; encouraged patients to contact nurse via telephone hotline during office hours if symptoms developed |
n = 56 Patients received usual care and follow-up in hospital outpatient clinics by same group of designated geriatricians or cardiologists used by intervention patients |
6-month readmission rate No significant difference between intervention and control groups (46% and 57%, respectively, P = 0.23) Authors reported no significant difference for primary causes of readmission (no statistical test reported) Unplanned readmissions No significant difference (intervention: median 0 [quartile range 0, 1] vs. control: median 1 [quartile range 0, 2], P = 0.06) Functional status (6MWT) No significant difference between study groups London Handicap Scale (6 domains) Compared with controls, intervention group became significantly less limited in independence (median change in independence domain score 0 vs. 0.5, P < 0.005). No significant difference observed in other 5 domains |
Intent-to-treat analysis not reported At baseline, more patients in intervention group receiving social security assistance than control group (23/49 [47%] vs. 14/56 [25%], respectively) Statistical comparisons not reported for baseline characteristics |
| Zhao et al, 2009 (58) China |
n = 100 A hospital nurse was responsible for the predischarge phase and 2 nurses in a community hospital were responsible for the postdischarge phase Key areas addressed were patients’ understanding of and adherence to diet, medications, exercise, and health-related lifestyle Based on referral report from the hospital nurse, community nurses continued to follow-up the patients for 4 weeks via 2 home visits and 2 telephone calls. |
n = 100 Physician talked to patients about special points that needed attention on returning home Free educational pamphlets on maintaining healthy eating and lifestyles were made available to patients |
Endpoints measured at 2 days, 4 weeks, and 12 weeks postdischarge Patients in study group had significantly better understanding of diet, medications, and health-related lifestyle behaviour at 2 days, 4 weeks, and 12 weeks postdischarge and better understanding of exercise at weeks 4 and 12 Significant differences favouring intervention group in adherence to diet and health-related lifestyle at day 2, 4 weeks, and 12 weeks, medication at 4 and 12 weeks, and exercise at week 12 No significant difference between study groups for hospital readmission 82% of intervention patients considered community nursing follow-up very helpful, and 80% expressed high satisfaction with service Patient satisfaction not reported for control group |
Instruments used to measure patient understanding, adherence and satisfaction were not standardized, validated measurement scales Outcome measures relied on self-reporting by patients. Data regarding extent of cardiovascular risk for the patients were not reported (e.g., weight, blood pressure, diabetes, etc.). |
Abbreviations: χ2, chi-square; 6MWT, 6-minute walking test; APN, Advanced Practice Nurses; CI, confidence interval; HF, heart failure; HRQOL, health-related quality of life; RR, relative risk.
Although the multicentre RCT by Naylor et al (56) was published in 2004, Hansen et al (7) excluded it from their systematic review because it did not report a 30-day readmission outcome. Similarly, the study by Naylor et al was excluded by Shepperd et al (4) from their systematic review because “the intervention was a complex package of care where the main emphasis was not on discharge planning.” The RCT by Atienza et al, (59) also published in 2004, was excluded from the systematic review by Hansen et al (7) because it did not report a 30-day readmission outcome; however, it is unclear why it was excluded from the review by Shepperd et al. (4)
Atienza et al (59) evaluated the effectiveness of a discharge and outpatient management program in patients hospitalized for heart failure. Patients were randomized to usual care (n = 174) or an intervention (n = 164) consisting of a comprehensive hospital discharge planning and close follow-up at a heart failure clinic.
The intervention consisted of the following:
patients and families received formal education about heart failure from a cardiac nurse before discharge;
a visit with the patient’s primary care physician was scheduled within 2 weeks of discharge;
regular follow-up visits at the outpatient Heart Failure Clinic were scheduled every 3 months; and a 24-hour phone contact number was made available from discharge to the end of the study for patients to use if they experienced worsening symptoms.
The control group received discharge planning according to the routine protocol of the study hospitals.
The primary outcome was event-free survival defined on the basis of time to first event (any cause readmission or death) at 1 year. Secondary endpoints included rate of all-cause and heart failure readmissions per observation year, rate of death per observation year, and HRQOL.
Median follow-up was 509 days (interquartile range 365–649 days). Results are shown in Table 8.
Table 8: Summary of Results.
| Event-Free Survival | Readmissions | Mortality | HRQOL at 1 year (Minnesota Quality of Life Score) |
|---|---|---|---|
| Reduction of 47 events per 100 patients (95% CI, 29–65), P < 0.001 per year of observation in intervention patients. Intervention: 156 events (30 deaths and 126 all-cause readmissions) Control: 250 events (51 deaths 199 all-cause readmissions) |
Reduction of 16% (95% CI, 4%–28%), P = 0.004 in the rate of readmitted patients for any cause in intervention group. Intervention: 68/164 patients Control: 101/174 patients Reduction of 37 all-cause readmissions per 100 patients (95% CI, 21–53), P < 0.001 per year of observation for intervention group. Intervention: 126 all-cause readmissions Control: 199 all-cause readmissions Reduction of 19% (95% CI, 0.09–0.29), P < 0.001 in the rate of readmitted patients for HF in the intervention group Intervention: 39/164 patients readmitted for HF Control: 79/174 patients readmitted for HF |
Death rates per observation year were: Intervention: 0.14 Control: 0.24 Difference in rate of death per observation year: 0.10 (95% CI: 0.02–0.18), P = 0.006 Intervention: 30/164 deaths at end of follow-up Control: 51/174 deaths at end of follow-up |
220 of 257 surviving patients completed questionnaire Significantly higher improvement in intervention group (P = 0.01) Intervention: baseline score 51.6; 1 year score 28.9 Control: baseline score 51.9; 1 year score 35.5 |
Abbreviations: CI, confidence interval; HF, heart failure; HRQOL health-related quality of life.
Source: Atienza et al, 2004 (59)
Limitations to the study by Atienza et al (59) included the following:
The intervention elements that are responsible for beneficial results cannot be identified.
This study had an additional component of postdischarge follow-up that the other studies in the systematic review by Phillips et al (11) did not have, namely patients were required to attend a heart failure clinic.
Naylor et al (56) examined the effect of a 3-month comprehensive discharge planning and home follow-up intervention directed by advanced practice nurses (APNs) compared with usual care for elders (aged 65 years or older) hospitalized with heart failure. The intervention consisted of the following:
an initial APN visit within 24 hours of index hospital admission;
APN visits at least daily during index hospitalization;
at least 8 APN home visits (one visit within 24 hours of discharge);
weekly visits during the first month (with one of these visits coinciding with the initial follow-up visit to the patient’s physician);
bimonthly visits during the second and third months;
additional APN visits based on patients’ needs; and
APN telephone availability 7 days per week (8 AM to 8 PM on weekdays; 8 AM to noon on weekends).
A major focus of the APN’s intervention during the hospitalization phase was collaboration with physicians and other providers to optimize the patient’s health status at discharge, design the discharge plan, and arrange for needed home care services. Special emphasis was placed on preventing functional decline and streamlining medication regimens. After patients were discharged to their homes, APNs conducted assessments to identify changes in patients’ health status and collaborated with each patient’s physician regarding adjustments in medications and other therapies.
Usual care for the control group included site-specific heart failure-patient management and discharge planning critical paths and, if referred, standard home agency care consisting of comprehensive skilled home health services 7 days a week. The attending physician was responsible for determining the discharge date, and the primary nurse, discharge planner and physician collaborated in the design and implementation of the discharge plan. Standards and processes of care for the primary home care sites included use of liaison nurses to facilitate referrals to home care; availability of comprehensive intermittent skilled home care services in patients’ residences 7 days per week and on-call registered nurse availability 24 hours per day. Of the control group, 58% (71/121) received referrals for skilled nursing or physical therapy after the index hospital discharge.
Patient telephone interviews were conducted at 2, 6, 12, 26, and 52 weeks after the index discharge to obtain information about rehospitalizations and unscheduled acute care visits to physicians, clinics, and EDs, HRQOL and functional status. The primary endpoint was time to first rehospitalization or death.
Results for the RCT by Naylor et al (56) are shown in Table 9.
Table 9: Results of Discharge Planning Compared with Usual Care.
| Outcome | Result |
|---|---|
| Time to first rehospitalization or death | Longer in intervention patients (log rank χ2 = 5.0, P = 0.03) Control vs. intervention Incidence density ratio 1.65 (1.13–2.40), P = 0.001 |
| Rehospitalization or death at 52 weeks |
Intervention (n = 118 patients) vs. control (n = 121 patients) 56 (48%) vs. 74 patients (61%), P = 0.01 |
| Patients rehospitalized | Intervention (n = 118 patients) vs. control (n = 121 patients) |
| 1 time | 53 (44.9%) vs. 67 (55.4%), P = 0.12; RR, 1.24 (95% CI, 0.95–1.60) |
| 2 times | 34 (28.8) vs. 44 (36.4%), P = 0.22; RR, 1.20 (95% CI, 0.89–1.60) |
| Rehospitalizations at 1 year |
Intervention (n = 104 rehospitalizations) vs. control (n = 162 rehospitalizations) Index related: 40 vs. 72, P = 0.18 Comorbidity related: 23 vs. 50, P = 0.01 New health problem: 41 vs. 40, P = 0.88 |
| HRQOL | At 12 weeks, intervention group reported greater overall HRQOL (P < 0.05) No significant difference observed at other time points |
| Functional status | No significant difference observed at any time point |
| Patient satisfaction | Satisfaction with care greater in intervention patients at 2 and 6 weeks (P < 0.001) No other time periods reported |
Abbreviations: χ2, chi-square; CI, confidence interval; RCT, randomized controlled trial; RR, relative risk
Source: Naylor et al, 2004 (56)
A limitation to the study by Naylor et al (56) was that the control group had significantly more patients with hypertension at baseline than the treatment group (71/121 [59%] versus 54/121 [45%]; P = 0.04, respectively.
Kwok et al (57) conducted an RCT to evaluate the effectiveness of a postdischarge community nursing program in older patients (aged 60 years or older) with chronic heart failure who had at least one hospital admission for heart failure in the 12 months prior to the index admission.
Patients in the intervention group (n = 49) received community nurse visits before discharge, within 7 days of discharge, weekly for 4 weeks, and then monthly. Community nurses worked closely with designated hospital geriatricians or cardiologists and counselled patients on drug compliance and diet. They also encouraged patients to contact the nurse via a telephone hotline during office hours when they developed symptoms.
Patients in the control group (n = 56) received usual care and were followed up in the hospital outpatient clinics by the same group of designated geriatricians or cardiologists.
The primary outcome was the rate of unplanned readmissions at 6 months postdischarge from hospital. Secondary outcomes included the number of unplanned readmission, the 6-minute walking test (6MWT) and London Handicap Scale domain scores. The 6 domains of handicap in this scale were mobility, independence, occupation, social, orientation, and economic.
Baseline characteristics were similar between the study groups except that more patients in the intervention group were receiving social security assistance than the control group (23/49 [47%] vs. 14/56 [25%], respectively). Statistical comparisons were not reported for baseline characteristics.
There was no significant difference in the 6-month readmission rate between the intervention and control groups (46% and 57% respectively, P = 0.23). The authors reported no significant difference between the groups in terms of primary causes of readmission (no statistical test reported).
There was no significant difference in the median number of unplanned readmissions between the study groups (intervention: median 0 [quartile range 0, 1] vs. control: median 1 [quartile range 0, 2], P = 0.06).
No significant difference was observed between the intervention and control group for change in functional status using 6MWT.
For the London Handicap Scale, there was a significant difference between the groups for the independence domain. Compared with the control group, patients in the intervention arm became significantly less limited in independence (median change in independence domain score 0 vs. 0.5, P < 0.005). No significant difference was observed in the other 5 domains.
Limitations to the RCT by Kwok et al (57) included:
Small sample size. The authors conducted a sample size analysis that required 50 patients per group to have an 80% chance of detecting a 40% relative reduction in readmission rate at a confidence interval of 95%. There were 44/49 intervention patients and 46/56 control group patients who completed the study. Intent-to-treat analysis was not reported by the authors.
A significant difference in economic status between the study arms at baseline.
Zhao et al (58) conducted an RCT (N = 200) to determine the effectiveness of a discharge planning program among patients with newly diagnosed coronary heart disease. Patients in the intervention arm (n = 100) received a discharge planning program consisting of 2 phases. A nurse from the hospital was responsible for the predischarge phase, and 2 nurses in a community hospital were responsible for the postdischarge phase. Key areas addressed by all nurses were patients’ understanding of and adherence to diet, medications, exercise, and health-related lifestyle such as getting enough rest and quitting smoking. Based on the instructions in the hospital nurse’s referral report, the community nurses continued to follow the patients for 4 weeks via 2 home visits and 2 telephone calls.
Patients in the control group (n = 100) received routine care, which involved a physician talking to them about special points that needed attention on returning home. Patients were given educational pamphlets on maintaining healthy eating habits and lifestyles.
Outcome measures were:
patient understanding (ranked high, moderate or low) of diet, medications, exercise, and HRQOL;
patient adherence (ranked high, moderate, or low) to diet, medications, exercise, and health-related lifestyle;
health care utilization; and
satisfaction with care.
The authors did not report a primary outcome. Endpoints were measured at 2 days, 4 weeks, and 12 weeks postdischarge.
Results of the RCT are shown in Table 10. Overall, patients in the study group had a significantly better understanding of diet, their medications, and health-related lifestyle behaviour at 2 days, 4 weeks, and 12 weeks postdischarge and a better understanding of exercise at weeks 4 and 12. In addition, there were significant differences favouring the intervention group in adherence to diet and health-related lifestyle at 2 days, 4 weeks, and 12 weeks; medication at 4 weeks and 12 weeks; and exercise at week 12.
Table 10: Results of Discharge Planning Compared with Usual Care.
| Outcome | Result (Intervention Compared With Control) |
|---|---|
| Understanding of diet, medications, exercise, and HRQOL | |
| Diet | Intervention patients had a significantly better understanding of diet at all endpoints 2 days: P = 0.00; 4 weeks: P = 0.00; 12 weeks: P = 0.00 |
| Medications | Intervention patients had a significantly better understanding of medications at all endpoints 2 days: P = 0.00; 4 weeks: P = 0.00; 12 weeks: P = 0.00 |
| Exercise | Intervention patients had a significantly better understanding of exercise at 4 and 12 weeks 2 days: P = 0.06; 4 weeks: P = 0.00; 12 weeks: P = 0.00 |
| Health-related lifestyle | Intervention patients had a significantly better understanding of health-related lifestyle at all endpoints 2 days: P = 0.00; 4 weeks: P = 0.00; 12 weeks: P = 0.00 |
| Adherence to diet, medications, exercise, and health-related lifestyle | |
| Diet | Intervention patients had significantly better adherence to diet at all endpoints 2 days: P = 0.00; 4 weeks: P = 0.00; 12 weeks: P = 0.02 |
| Medications | Intervention patients had significantly better adherence to medications at 4 and 12 weeks 2 days: P = 0.68; 4 weeks: P = 0.01; 12 weeks: P = 0.00 |
| Exercise | Intervention patients had significantly better adherence to exercise at 12 weeks 2 days: P = 0.92; 4 weeks: P = 0.17; 12 weeks: P = 0.00 |
| Health-related lifestyle | Intervention patients had significantly better adherence to health-related lifestyle at all endpoints 2 days: P = 0.03; 4 weeks: P = 0.00; 12 weeks: P = 0.00 |
| Health care utilization | |
| Readmission related to CHD | No significant difference between intervention and control patients at 12 weeks, P = 0.83 |
| Readmission related to other diseases | No significant difference between intervention and control patients at 12 weeks, P = 0.25 |
| Satisfaction with care | |
| Patient satisfaction | 82% of intervention patients considered postdischarge community nursing very helpful 80% of intervention patients expressed high satisfaction with postdischarge community nursing |
Abbreviations: CHD, coronary heart disease; HRQOL, health-related quality of life.
Source: Zhao et al, 2009 (58)
There was no significant difference between the study groups for hospital readmission at 12 weeks postdischarge, P = 0.83.
Of the intervention patients, 82% considered the community nursing follow-up to be very helpful, and 80% expressed high satisfaction with the service. Patient satisfaction was not reported for the control group.
Limitations to the study by Zhao et al (58) included the following:
The study took place in an affluent city in China, therefore generalizability to other cities is limited.
The instruments used to measure patient understanding, adherence, and satisfaction were not standardized, validated measurement scales.
The outcome measures (including health care utilization) relied on patient self-reports.
Data regarding the extent of cardiovascular risk for the patients were not reported (e.g., weight, blood pressure, diabetes, etc.).
Conclusions
Conclusions for this evidence-based analysis are shown in Table 11. Details about GRADE for each outcome are in Appendix 3.
Table 11: Conclusions of Evidence-Based Review.
| Outcome | Conclusion |
|---|---|
| Individualized Discharge Planning Compared With Usual Care | |
| Readmissions | Moderate quality evidence that individualized discharge planning is more effective at reducing readmissions |
| Hospital LOS | Moderate quality evidence that individualized discharge planning is more effective at reducing initial hospital LOS |
| Mortality | Moderate quality evidence that individualized discharge planning is not more effective at reducing mortality |
| HRQOL | Very low quality evidence that individualized discharge planning is more effective at improving HRQOL |
| Patient Satisfaction | Very low quality evidence that individualized discharge planning is more effective at improving patient satisfaction |
| Individualized Discharge Planning Plus Postdischarge Support Compared With Usual Care | |
| Readmissions | Low quality evidence that discharge planning plus postdischarge support is more effective at reducing readmissions |
| Hospital LOS | Low quality evidence that discharge planning plus postdischarge support is not more effective at reducing LOS |
| Mortality | Low quality evidence that discharge planning plus postdischarge support is not more effective at reducing mortality |
| HRQOL | Very low quality evidence that discharge planning plus postdischarge support is more effective at improving HRQOL |
| Patient Satisfaction | Very low quality evidence that discharge planning plus postdischarge support is more effective at improving patient satisfaction |
Abbreviations: HRQOL, health-related quality of life; LOS, length of stay.
Overall limitations to the studies in this evidence-based analysis were as follows:
It was difficult to distinguish the relative contribution of each element within the umbrella terms “discharge planning” and “postdischarge support.”
The context in which discharge planning is delivered may play a role not only for the intervention but in the way services are configured for the control group (i.e., for different countries, the orientation of primary care services differs, which may affect communication between services).
The specific time point in a patient’s hospital admission when discharge planning was implemented varied across studies (i.e., at time of admission vs. 3 days before discharge). The duration of components for postdischarge support also varied across studies.
For most studies, “usual care” was not explicitly described.
Some studies may have been underpowered to detect a statistically significant difference in outcomes (type 2 error).
Many studies were unable to determine whether events that occurred distant from the index hospitalization were related to the initial admission or whether they were new problems for patients who were readmitted or died.
Acknowledgements
Editorial Staff
Joanna Odrowaz, BSc (Hons)
Medical Information Services
Kaitryn Campbell, BA(H), BEd, MLIS
Kellee Kaulback, BA(H), MISt
Expert Panel for Health Quality Ontario: Optimizing Chronic Disease Management in the Community (Outpatient) Setting
| Name | Title | Organization |
|---|---|---|
| Shirlee Sharkey (chair) | President & CEO | Saint Elizabeth Health Care |
| Theresa Agnew | Executive Director | Nurse Practitioners’ Association of Ontario |
| Onil Bhattacharrya | Clinician Scientist | Li Ka Shing Knowledge Institute, St. Michael’s Hospital, University of Toronto |
| Arlene Bierman | Ontario Women’s Health Council Chair in Women’s Health | Department of Medicine, Keenan Research Centre in the Li Ka Shing Knowledge Institute, St. Michael’s Hospital, University of Toronto |
| Susan Bronskill | Scientist | Institute for Clinical Evaluative Sciences |
| Catherine Demers | Associate Professor | Division of Cardiology, Department of Medicine, McMaster University |
| Alba Dicenso | Professor | School of Nursing, McMaster University |
| Mita Giacomini | Professor | Centre of Health Economics & Policy Analysis, Department of Clinical Epidemiology & Biostatistics |
| Ron Goeree | Director | Programs for Assessment of Technology in Health (PATH) Research Institute, St. Joseph’s Healthcare Hamilton |
| Nick Kates | Senior Medical Advisor | Health Quality Ontario – QI McMaster University Hamilton Family Health Team |
| Murray Krahn | Director | Toronto Health Economics and Technology Assessment (THETA) Collaborative, University of Toronto |
| Wendy Levinson | Sir John and Lady Eaton Professor and Chair | Department of Medicine, University of Toronto |
| Raymond Pong | Senior Research Fellow and Professor | Centre for Rural and Northern Health Research and Northern Ontario School of Medicine, Laurentian University |
| Michael Schull | Deputy CEO & Senior Scientist | Institute for Clinical Evaluative Sciences |
| Moira Stewart | Director | Centre for Studies in Family Medicine, University of Western Ontario |
| Walter Wodchis | Associate Professor | Institute of Health Management Policy and Evaluation, University of Toronto |
Appendices
Appendix 1: Literature Search Strategies
Search date: January 29th, 2012
Databases searched: OVID MEDLINE, OVID MEDLINE In-Process and Other Non-Indexed Citations, OVID EMBASE, Wiley Cochrane, EBSCO CINAHL, Centre for Reviews and Dissemination
Limits: 2004-current; English; MA/SR/HTA/RCT filter
Database: Ovid MEDLINE(R) <1946 to January Week 3 2012>, Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations <January 27, 2012>, Embase <1980 to 2012 Week 04>
Search Strategy:
| # | Searches | Results |
|---|---|---|
| 1 | exp Coronary Artery Disease/ | 212075 |
| 2 | exp Myocardial Infarction/ use mesz | 133578 |
| 3 | exp heart infarction/ use emez | 216992 |
| 4 | (coronary artery disease or cad or heart attack).ti. | 44463 |
| 5 | ((myocardi* or heart or cardiac or coronary) adj2 (atheroscleros* or arterioscleros* or infarct*)).ti. | 149559 |
| 6 | or/1-5 | 539975 |
| 7 | exp Atrial Fibrillation/ use mesz | 28093 |
| 8 | exp heart atrium fibrillation/ use emez | 55522 |
| 9 | ((atrial or atrium or auricular) adj1 fibrillation*).ti,ab. | 73540 |
| 10 | or/7-9 | 99451 |
| 11 | exp heart failure/ | 300981 |
| 12 | ((myocardi* or heart or cardiac) adj2 (failure or decompensation or insufficiency)).ti,ab. | 234590 |
| 13 | 11 or 12 | 381953 |
| 14 | exp Stroke/ | 178088 |
| 15 | exp Ischemic Attack, Transient/ use mesz | 16370 |
| 16 | exp transient ischemic attack/ use emez | 19680 |
| 17 | exp stroke patient/ use emez | 5637 |
| 18 | exp brain infarction/ or exp cerebrovascular accident/ use emez | 101006 |
| 19 | (stroke or tia or transient ischemic attack or cerebrovascular apoplexy or cerebrovascular accident or cerebrovascular infarct* or brain infarct* or CVA).ti,ab. | 281375 |
| 20 | or/14-19 | 391798 |
| 21 | exp Diabetes Mellitus, Type 2/ use mesz | 68223 |
| 22 | exp non insulin dependent diabetes mellitus/ use emez | 101711 |
| 23 | exp diabetic patient/ use emez | 12920 |
| 24 | (diabetes or diabetic* or niddm or t2dm).ti,ab. | 765351 |
| 25 | or/21-24 | 790292 |
| 26 | exp Skin Ulcer/ | 72073 |
| 27 | ((pressure or bed or skin) adj2 (ulcer* or sore* or wound*)).ti,ab. | 28723 |
| 28 | (decubitus or bedsore*).ti,ab. | 8532 |
| 29 | or/26-28 | 90816 |
| 30 | exp Pulmonary Disease, Chronic Obstructive/ use mesz | 17049 |
| 31 | exp chronic obstructive lung disease/ use emez | 54779 |
| 32 | (chronic obstructive adj2 (lung* or pulmonary or airway* or airflow or respiratory) adj (disease* or disorder*)).ti,ab. | 54491 |
| 33 | (copd or coad).ti,ab. | 45716 |
| 34 | chronic airflow obstruction.ti,ab. | 1063 |
| 35 | exp Emphysema/ | 37444 |
| 36 | exp chronic bronchitis/ use emez | 6985 |
| 37 | ((chronic adj2 bronchitis) or emphysema).ti,ab. | 50848 |
| 38 | or/30-37 | 159366 |
| 39 | exp Chronic Disease/ | 340792 |
| 40 | ((chronic* adj2 disease*) or (chronic* adj2 ill*)).ti,ab. | 220217 |
| 41 | 39 or 40 | 506604 |
| 42 | exp Comorbidity/ | 143585 |
| 43 | (comorbid* or co-morbid* or multimorbid* or multi-morbid* or (complex* adj patient*) or “patient* with multiple” or (multiple adj2 (condition* or disease*))).ti,ab. | 203652 |
| 44 | 42 or 43 | 284365 |
| 45 | 6 or 10 or 13 or 20 or 25 or 29 or 38 or 41 or 44 | 2823779 |
| 46 | exp Patient Discharge/ use mesz | 16001 |
| 47 | exp hospital discharge/ use emez | 48313 |
| 48 | ((post-discharge or postdischarge or post-hospital or posthospital or discharge) adj2 (patient or hospital or support* or service* or plan* or summar* or coordinat* or co-ordinat* or manage*)).ti,ab. | 46581 |
| 49 | exp Medication Reconciliation/ use mesz | 85 |
| 50 | exp Medication Errors/pc use mesz | 3717 |
| 51 | exp medication therapy management/ use emez | 736 |
| 52 | exp medication error/pc use emez | 2159 |
| 53 | ((medication* or drug*) adj2 (reconcil* or manage*)).ti,ab. | 9668 |
| 54 | or/46-53 | 108369 |
| 55 | 45 and 54 | 27866 |
| 56 | limit 55 to english language | 25438 |
| 57 | limit 56 to yr=“2004 -Current” | 16734 |
| 58 | limit 57 to (controlled clinical trial or meta analysis or randomized controlled trial) | 1072 |
| 59 | exp Technology Assessment, Biomedical/ or exp Evidence-based Medicine/ use mesz | 63494 |
| 60 | exp Biomedical Technology Assessment/ or exp Evidence Based Medicine/ use emez | 524160 |
| 61 | (health technology adj2 assess*).ti,ab. | 3066 |
| 62 | exp Random Allocation/ or exp Double-Blind Method/ or exp Control Groups/ or exp Placebos/ use mesz | 379985 |
| 63 | Randomized Controlled Trial/ or exp Randomization/ or exp RANDOM SAMPLE/ or Double Blind Procedure/ or exp Triple Blind Procedure/ or exp Control Group/ or exp PLACEBO/ use emez | 902695 |
| 64 | (random* or RCT).ti,ab. | 1256935 |
| 65 | (placebo* or sham*).ti,ab. | 414541 |
| 66 | (control* adj2 clinical trial*).ti,ab. | 35105 |
| 67 | meta analysis/ use emez | 58676 |
| 68 | (meta analy* or metaanaly* or pooled analysis or (systematic* adj2 review*) or published studies or published literature or medline or embase or data synthesis or data extraction or cochrane).ti,ab. | 253317 |
| 69 | or/59-68 | 2167232 |
| 70 | (57 and 69) or 58 | 2889 |
| 71 | remove duplicates from 70 | 2308 |
CINAHL
| # | Query | Limiters/Expanders | Results |
|---|---|---|---|
| S45 | S34 and S40 and S43 | Limiters - Published Date from: 20040101-20121231; English Language; Exclude MEDLINE records Search modes - Boolean/Phrase |
38 |
| S44 | S34 and S40 and S43 | Search modes - Boolean/Phrase | 369 |
| S43 | S41 or S42 | Search modes - Boolean/Phrase | 156355 |
| S42 | random* or sham*or rct* or health technology N2 assess* or meta analy* or metaanaly* or pooled analysis or (systematic* N2 review*) or published studies or medline or embase or data synthesis or data extraction or cochrane or control* N2 clinical trial* | Search modes - Boolean/Phrase | 148276 |
| S41 | (MH “Random Assignment”) or (MH “Random Sample+”) or (MH “Meta Analysis”) or (MH “Systematic Review”) or (MH “Double-Blind Studies”) or (MH “Single-Blind Studies”) or (MH “Triple-Blind Studies”) or (MH “Placebos”) or (MH “Control (Research)”) | Search modes - Boolean/Phrase | 83647 |
| S40 | S35 or S36 or S37 or S38 or S39 | Search modes - Boolean/Phrase | 19853 |
| S39 | medication* N2 reconcil* or drug* N2 reconcil* or drug N2 manage* or medication N2 manage* | Search modes - Boolean/Phrase | 1997 |
| S38 | (MH “Medication Errors/PC”) | Search modes - Boolean/Phrase | 3605 |
| S37 | (MH “Medication Reconciliation”) | Search modes - Boolean/Phrase | 241 |
| S36 | post-discharge or postdischarge or post-hospital or posthospital or discharge N2 plan* or discharge N2 summar* or discharge N2 co-ordinat* or discharge N2 coordinat* or discharge N2 manage*or discharge N2 service* | Search modes - Boolean/Phrase | 5580 |
| S35 | (MH “Patient Discharge+”) | Search modes - Boolean/Phrase | 12852 |
| S34 | S5 OR S8 OR S11 OR S15 OR S19 OR S22 OR S27 OR S30 OR S33 | Search modes - Boolean/Phrase | 221088 |
| S33 | S31 OR S32 | Search modes - Boolean/Phrase | 28945 |
| S32 | comorbid* OR co-morbid* OR multimorbid* OR multi-morbid* OR (complex* N1 patient*) OR “patient* with multiple” OR (multiple N2 (condition* OR disease*)) | Search modes - Boolean/Phrase | 28945 |
| S31 | (MH “Comorbidity”) | Search modes - Boolean/Phrase | 16646 |
| S30 | S28 OR S29 | Search modes - Boolean/Phrase | 43734 |
| S29 | (chronic* N2 disease*) OR (chronic* N2 ill*) | Search modes - Boolean/Phrase | 43734 |
| S28 | (MH “Chronic Disease”) | Search modes - Boolean/Phrase | 23647 |
| S27 | S23 OR S24 OR S25 OR S26 | Search modes - Boolean/Phrase | 8774 |
| S26 | chronic N2 bronchitis OR emphysema | Search modes - Boolean/Phrase | 1820 |
| S25 | (MH “Emphysema”) | Search modes - Boolean/Phrase | 885 |
| S24 | chronic obstructive N2 disease* OR chronic obstructive N2 disorder* OR copd OR coad | Search modes - Boolean/Phrase | 7349 |
| S23 | (MH “Pulmonary Disease, Chronic Obstructive+”) | Search modes - Boolean/Phrase | 5342 |
| S22 | S20 OR S21 | Search modes - Boolean/Phrase | 16179 |
| S21 | pressure N1 ulcer* OR bedsore* OR bed N1 sore* OR skin N1 ulcer* OR pressure N1 wound* OR decubitus | Search modes - Boolean/Phrase | 9574 |
| S20 | (MH “Skin Ulcer+”) | Search modes - Boolean/Phrase | 14845 |
| S19 | S16 OR S17 OR S18 | Search modes - Boolean/Phrase | 70185 |
| S18 | diabetes OR diabetic* OR niddm OR t2dm | Search modes - Boolean/Phrase | 70185 |
| S17 | (MH “Diabetic Patients”) | Search modes - Boolean/Phrase | 3536 |
| S16 | (MH “Diabetes Mellitus, Type 2”) | Search modes - Boolean/Phrase | 18233 |
| S15 | S12 OR S13 OR S14 | Search modes - Boolean/Phrase | 38210 |
| S14 | stroke OR tia OR transient ischemic attack OR cerebrovascular apoplexy OR cerebrovascular accident OR cerebrovascular infarct* OR brain infarct* OR CVA | Search modes - Boolean/Phrase | 37713 |
| S13 | (MH “Cerebral Ischemia, Transient”) | Search modes - Boolean/Phrase | 1903 |
| S12 | (MH “Stroke”) OR (MH “Stroke Patients”) | Search modes - Boolean/Phrase | 25676 |
| S11 | S9 OR S10 | Search modes - Boolean/Phrase | 18862 |
| S10 | myocardi* failure OR myocardial decompensation OR myocardial insufficiency OR cardiac failure OR cardiac decompensation OR cardiac insufficiency OR heart failure OR heart decompensation OR heart insufficiency |
Search modes - Boolean/Phrase | 18850 |
| S9 | (MH “Heart Failure+”) | Search modes - Boolean/Phrase | 14393 |
| S8 | S6 OR S7 | Search modes - Boolean/Phrase | 8072 |
| S7 | atrial N1 fibrillation* OR atrium N1 fibrillation* OR auricular N1 fibrillation* | Search modes - Boolean/Phrase | 8072 |
| S6 | (MH “Atrial Fibrillation”) | Search modes - Boolean/Phrase | 6490 |
| S5 | S1 OR S2 OR S3 OR S4 | Search modes - Boolean/Phrase | 30133 |
| S4 | TI myocardi* N2 infarct* OR TI heart N2 infarct* OR TI cardiac N2 infarct* OR TI coronary N2 infarct* OR TI arterioscleros* OR TI atheroscleros* | Search modes - Boolean/Phrase | 9643 |
| S3 | coronary artery disease OR cad OR heart attack* | Search modes - Boolean/Phrase | 7706 |
| S2 | (MH “Myocardial Infarction+”) | Search modes - Boolean/Phrase | 19219 |
| S1 | (MH “Coronary Arteriosclerosis”) | Search modes - Boolean/Phrase | 4646 |
Wiley Cochrane
| ID | Search | Hits |
|---|---|---|
| #1 | MeSH descriptor Coronary Artery Disease explode all trees | 2183 |
| #2 | MeSH descriptor Myocardial Infarction explode all trees | 7746 |
| #3 | (myocardi* or heart or cardiac or coronary) NEAR/2 (atheroscleros* or arterioscleros* or infarct*):ti or (coronary artery disease or cad or heart attack*):ti | 8469 |
| #4 | MeSH descriptor Atrial Fibrillation explode all trees | 2102 |
| #5 | (atrial NEAR/2 fibrillation* or atrium NEAR/2 fibrillation* or auricular NEAR/2 fibrillation*):ti | 2310 |
| #6 | MeSH descriptor Heart Failure explode all trees | 4710 |
| #7 | (myocardi* NEAR/2 (failure or decompensation or insufficiency)):ti or (heart NEAR/2 (failure or decompensation or insufficiency)):ti or (cardiac NEAR/2 (failure or decompensation or insufficiency)):ti | 5252 |
| #8 | MeSH descriptor Stroke explode all trees | 3899 |
| #9 | MeSH descriptor Ischemic Attack, Transient explode all trees | 466 |
| #10 | (stroke or tia or transient ischemic attack or cerebrovascular apoplexy or cerebrovascular accident or cerebrovascular infarct* or brain infarct* or CVA):ti | 9902 |
| #11 | MeSH descriptor Diabetes Mellitus, Type 2 explode all trees | 6993 |
| #12 | (diabetes or diabetic* or niddm or t2dm):ti | 16585 |
| #13 | MeSH descriptor Skin Ulcer explode all trees | 1572 |
| #14 | (pressure or bed or skin) NEAR/2 (ulcer* or sore* or wound*):ti | 669 |
| #15 | (decubitus or bedsore*):ti | 98 |
| #16 | MeSH descriptor Pulmonary Disease, Chronic Obstructive explode all trees | 1754 |
| #17 | (chronic obstructive NEAR/2 (lung* or pulmonary or airway* or airflow or respiratory)):ti | 2415 |
| #18 | (copd or coad):ti | 3319 |
| #19 | (chronic airflow obstruction):ti | 72 |
| #20 | MeSH descriptor Emphysema explode all trees | 91 |
| #21 | (chronic NEAR/2 bronchitis) or emphysema:ti | 1183 |
| #22 | (Chronic Disease):ti | 4464 |
| #23 | (chronic* NEAR/2 disease* or chronic* NEAR/2 ill*):ti | 1670 |
| #24 | MeSH descriptor Comorbidity explode all trees | 1941 |
| #25 | (comorbid* OR co-morbid* OR multimorbid* OR multi-morbid* OR (complex* NEXT patient*) OR “patient* with multiple” OR (multiple NEAR/2 (condition* OR disease*))):ti | 649 |
| #26 | (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25) | 61123 |
| #27 | MeSH descriptor Patient Discharge explode all trees | 863 |
| #28 | (post-discharge or postdischarge or post-hospital or posthospital or discharge) NEAR/2 (patient or hospital or support* or service* or plan* or summar* or coordinat* or co-ordinat* or manage*):ti | 478 |
| #29 | MeSH descriptor Medication Reconciliation explode all trees | 2 |
| #30 | MeSH descriptor Medication Errors explode all trees with qualifier: PC | 103 |
| #31 | (medication* or drug*) NEAR/2 (reconcil* or manage*):ti | 71 |
| #32 | (#27 OR #28 OR #29 OR #30 OR #31) | 1285 |
| #33 | (#26 AND #32), from 2004 to 2012 | 131 |
Centre for Reviews and Dissemination
| Line | Search | Hits |
|---|---|---|
| 1 | MeSH DESCRIPTOR coronary artery disease EXPLODE ALL TREES | 230 |
| 2 | (coronary artery disease or cad or heart attack*):TI | 213 |
| 3 | ((myocardi* or heart or cardiac or coronary) adj2 (atheroscleros* or arterioscleros* or infarct*)):TI | 224 |
| 4 | MeSH DESCRIPTOR Atrial Fibrillation EXPLODE ALL TREES | 225 |
| 5 | (((atrial or atrium or auricular) adj1 fibrillation*):TI | 0 |
| 6 | ((atrial or atrium or auricular) adj1 fibrillation*):TI | 168 |
| 7 | MeSH DESCRIPTOR heart failure EXPLODE ALL TREES | 418 |
| 8 | ((myocardi* or heart or cardiac) adj2 (failure or decompensation or insufficiency)):TI | 280 |
| 9 | MeSH DESCRIPTOR stroke EXPLODE ALL TREES | 549 |
| 10 | MeSH DESCRIPTOR Ischemic Attack, Transient EXPLODE ALL TREES | 32 |
| 11 | (stroke or tia or transient ischemic attack or cerebrovascular apoplexy or cerebrovascular accident or cerebrovascular infarct* or brain infarct* or CVA):TI | 622 |
| 12 | MeSH DESCRIPTOR Diabetes Mellitus, Type 2 EXPLODE ALL TREES | 511 |
| 13 | (diabetes or diabetic* or niddm or t2dm):TI | 1223 |
| 14 | MeSH DESCRIPTOR Skin Ulcer EXPLODE ALL TREES | 253 |
| 15 | ((pressure or bed or skin) adj2 (ulcer* or sore* or wound*)):TI | 73 |
| 16 | (decubitus or bedsore*):TI | 0 |
| 17 | MeSH DESCRIPTOR Pulmonary Disease, Chronic Obstructive EXPLODE ALL TREES | 237 |
| 18 | (chronic obstructive adj2 (lung* or pulmonary or airway* or airflow or respiratory)):TI | 219 |
| 19 | (copd or coad):TI | 108 |
| 20 | (chronic airflow obstruction):TI | 0 |
| 21 | MeSH DESCRIPTOR Emphysema EXPLODE ALL TREES | 10 |
| 22 | ((chronic adj2 bronchitis) or emphysema):TI | 47 |
| 23 | MeSH DESCRIPTOR Chronic Disease EXPLODE ALL TREES | 687 |
| 24 | ((chronic* adj2 disease*) or (chronic* adj2 ill*)):TI | 252 |
| 25 | MeSH DESCRIPTOR Comorbidity EXPLODE ALL TREES | 146 |
| 26 | ((comorbid* OR co-morbid* OR multimorbid* OR multi-morbid* OR (complex* NEXT patient*) OR “patient* with multiple” OR (multiple adj2 (condition* OR disease*)))):TI | 21 |
| 27 | #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 | 4655 |
| 28 | MeSH DESCRIPTOR Patient Discharge EXPLODE ALL TREES | 146 |
| 29 | (((post-discharge or postdischarge or post-hospital or posthospital or discharge) adj2 (patient or hospital or support* or service* or plan* or summar* or coordinat* or co-ordinat* or manage*))): TI | 27 |
| 30 | MeSH DESCRIPTOR Medication Errors EXPLODE ALL TREES WITH QUALIFIER PC | 19 |
| 31 | (((medication* or drug*) adj2 (reconcil* or manage*))):TI | 20 |
| 32 | #28 OR #29 OR #30 OR #31 | 189 |
| 33 | #27 AND #32 | 32 |
Appendix 2: Results
Table A1: Quality (EPOC) of Randomized Controlled Trialsa.
| Author, Year | Allocation Sequence Random | Allocation Concealed | Baseline Outcomes Similar | Baseline Characteristics Similar | Plan for Missing Data/Incomplete Data for Primary Outcome | Blinding | No Contamination | Free of Selective Outcome Reporting Risk | No Other Bias | EPOC Group Risk of Bias Criteria (9 Maximum Score) |
|---|---|---|---|---|---|---|---|---|---|---|
| Balaban et al, 2008 (12) | 1 | Unclear | Unclear | 1 | 1 | 1 | 0 | 1 | 0 | 5 |
| Braun et al, 2009 (13) | 0 | 1 | Unclear | 0 | 1 | 1 | 1 | 1 | 0 | 5 |
| Coleman et al, 2006 (14) | 1 | 1 | Unclear | 0 | 1 | 1 | 0 | 1 | 0 | 5 |
| Dudas et al, 2001 (15) | 1 | Unclear | Unclear | 1 | Unclear | 1 | 0 | 1 | 0 | 4 |
| Dunn et al, 1994 (16) | 1 | Unclear | Unclear | 0 | 0 | 1 | 1 | 1 | 0 | 4 |
| Evans et al, 1993 (17) | 1 | Unclear | Unclear | 1 | Unclear | 1 | 0 | 1 | 0 | 4 |
| Forster et al, 2005 (18) | 1 | 1 | Unclear | 1 | Unclear | 1 | 0 | 1 | 0 | 5 |
| Jaarsma et al, 1999 (19) | 1 | 1 | Unclear | 1 | Unclear | 1 | 0 | 1 | 0 | 5 |
| Jack et al, 2009 (20) | 1 | 1 | Unclear | 1 | Unclear | 1 | 1 | 1 | 0 | 6 |
| Koehler et al, 2009 (21) | 1 | 1 | Unclear | 1 | Unclear | 1 | 1 | 1 | 0 | 6 |
| Kwok et al, 2004 (22) | 1 | 1 | Unclear | 1 | Unclear | 1 | 1 | 1 | 0 | 6 |
| McDonald et al, 2001 (23) | 1 | Unclear | Unclear | 1 | Unclear | 1 | 1 | Unclear | 0 | 4 |
| Naylor et al, 1994 (24) | 1 | 0 | Unclear | 1 | Unclear | 1 | 1 | 1 | 0 | 5 |
| Parry et al, 2009 (25) | 1 | 1 | Unclear | 1 | 1 | 1 | 1 | 1 | 0 | 7 |
| Rainville, 1999 (26) | 1 | 1 | Unclear | 1 | 1 | 1 | 1 | 1 | 0 | 7 |
| Wong et al, 2008 (27) | 1 | Unclear | Unclear | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
Abbreviations: EPOC, Effective Practice and Organization of Care Criteria.
Source: Hansen et al, 2011. (7)
Table A2: Randomized Controlled Trials.
| Author, Year, Size | Intervention | Patient Population | Outcomes | EPOC Risk of Bias | Limitations/Comments |
|---|---|---|---|---|---|
| Balaban et al, 2008 (12) N = 96 |
A comprehensive patient discharge form was given to patients to identify any communication problems during transition of care (i.e., lack of knowledge about condition and gaps in outpatient follow-up care or test results). Discharge form electronically transferred to the RN at patients’ primary care facility. RN contacted patient and reviewed form and medication included in the discharge plan. RN phoned patient to assess status, review form, assess patient concerns and confirm follow-up appointments. Form and telephone notes forwarded electronically to PCP who reviewed the form. |
Patients admitted to a 100-bed community teaching hospital as an emergency Patients with diabetes, HF, COPD, depression |
Hospital LOS and readmission rates Follow-up at 21 and 31 days |
Adequate sequence generation? Unclear Allocation concealment? Unclear Blinding? Yes Incomplete outcome data addressed? Yes Free of selective reporting? Unclear Baseline data? No |
122 randomized 24 excluded after randomization because discharged to another institution; 2 died during hospital admission |
| Bolas et al, 2004 (28) N = 243 |
Use of a comprehensive medication history service, provision of an intensive clinical pharmacy service including management of patients’ own drugs brought to hospital, personalized drug record and patient counselling to explain changes at discharge. Discharge letter outlining complete drug history on admission and explanation of changes to medication during hospital and variances to discharge prescription faxed to GP and community pharmacist. Personalized drug card, counselling, labelling of dispensed drugs for follow-up. Drug helpline. Control intervention: standard clinical pharmacy services. |
Patients admitted to district general hospital Aged ≥ 55 years and taking ≥ 3 regular drugs |
Patient satisfaction Knowledge of drugs Hoarding of drugs |
Adequate sequence generation? Yes Allocation concealment? Unclear Blinding? No Incomplete outcome data addressed? No Free of selective reporting? Unclear Baseline data? Yes |
Follow-up of patients: 67% (162/243) Low response rate in survey of GPs (55%) and community pharmacists (56%) Unclear how standard clinical pharmacy services differ from intervention. |
| Evans et al, 1993 (17) N = 835 |
Patients screened for risk factors that may prolong hospital LOS, increase risk of readmission, or discharge to a nursing home. During discharge planning, information on support systems, living situation, finances, and areas of need were obtained from medical notes, interviews with the patient and family, and by consulting with the physician and nurse. Discharge planning initiated on day 3 of hospital admission, with patients referred to a social worker. Plans implemented with measureable goals using goal attainment scaling. Control intervention: discharge planning only if referred by medical staff and usually on the 9th day of hospital admission, or not at all. |
Patients screened for risk factors that would prolong their LOS at a VA hospital Older patients with a medical condition, neurological condition, or recovering from surgery | Hospital LOS Readmission to hospital Discharge destination Health status Follow-up at 3 months |
Adequate sequence generation? Unclear Allocation concealment? Unclear Blinding? Yes Incomplete outcome data addressed? Yes Free of selective reporting? Unclear Baseline data? Yes |
Controls could receive discharge planning |
| Harrison et al, 2002 (29) N = 200 |
Patients’ notes were flagged at admission as a signal to the primary nurse to follow a checklist for discharge planning. Hospital and community nurses working together for a smooth transition from hospital to home. A structured protocol was used for counselling and education for HF self-management. Home nursing visits were the same number as the control group. Telephone outreach within 24 hours of discharge. Control intervention: usual care for hospital to home transfer that involved completing a medical history, nursing assessment form, and a multidisciplinary plan. Discharge planning meetings took place weekly. Regional home care co-ordinator consulted with the hospital team as needed. Patients received the same number of home nurse visits as the intervention group. |
Older, cognitively unimpaired people with HF who were expected to be discharged (from a large urban teaching hospital) with home nursing care | HRQOL Symptoms distress and functioning ED visits and readmissions at 12 weeks |
Adequate sequence generation? Yes Allocation concealment? Unclear Blinding? Yes Incomplete outcome data addressed? No Free of selective reporting? Yes Baseline data? Yes |
|
| Hendriksen et al, 1990 (30) N = 273 |
Patients had daily contact with the project nurse who discussed their illness and discharge arrangements with them. Liaison between hospital and primary care staff. Project nurse visited patients at home after discharge and could make one repeat visit. Control intervention: described as “usual care.” |
Elderly patients admitted to a suburban hospital | Hospital LOS Readmission to hospital Discharge destination |
Adequate sequence generation? Unclear Allocation concealment? Unclear Blinding? Yes Incomplete outcome data addressed? Unclear Free of selective reporting? Unclear Baseline data? Yes |
Details of measures of outcome not provided Translated from Danish |
| Jack et al, 2009 (20) N = 749 |
At admission, the nurse discharge advocate completed the discharge intervention components. With information collected from the hospital team and patient, the discharge advocate created the after-hospital care plan that contained medical provider contact information, dates for appointments and tests, an appointment calendar, a colour-coded drug schedule, a list of tests with pending results at discharge, an illustrated description of the discharge diagnosis, and information about what to do if a problem arises. Information for the after-hospital care plan was manually entered into a Microsoft Word template, printed, and bound to produce an individualized booklet. Discharge advocate used scripts from the training manual to review contents of the after-hospital care plan with the patients. On day of discharge, the plan and discharge summary were faxed to the PCP. Pharmacist telephoned patients 2–4 days after the index discharge to reinforce the discharge plan by using a scripted interview. Pharmacist had access to the care plan and discharge summary and over several days made at least 3 attempts to reach each patient. Pharmacist asked patient to bring drugs to the phone, review them, and address any problems. Pharmacist communicated these issues to the PCP or discharge advocate. |
Patients who were emergency admissions to the medical teaching service and who were going to be discharged home | Readmission Patient satisfaction | Adequate sequence generation? Yes Allocation concealment? Yes Blinding? Yes Incomplete outcome data addressed? Yes Free of selective reporting? Unclear Baseline data? Yes |
|
| Kennedy et al, 1987 (31) N = 80 |
Discharge planning emphasized communication with the patient and family. A primary nurse assessed patients’ postdischarge needs. A comprehensive discharge planning protocol was developed that included an assessment of health status, orientation level, knowledge and perception of health status, pattern of resource use, functional status, skill level, motivation, and sociodemographic data. Implementation of the discharge plan by the primary nurse and other members of the health care team. Follow-up visit made to assess discharge placement. Control intervention: not described. |
Elderly acute care medical patients in a non-profit teaching hospital | Hospital LOS Readmission to hospital Discharge destination Health status |
Adequate sequence generation? Yes Allocation concealment? Yes Blinding? Yes Incomplete outcome data addressed? Yes Free of selective reporting? Unclear Baseline data? Yes |
Not clear when intervention implemented |
| Laramee et al, 2003 (32) N = 287 |
Early discharge planning and co-ordination of care and individualized and comprehensive patient and family education. Case manager assisted in the co-ordination of care by facilitating the discharge plan and obtaining needed consultations from social services, dietary services, and physical/occupation therapy. If needed, arrangements were made for additional services or support once the patient had returned home. Case manager also facilitated communication in the hospital among patient and family, attending physician, cardiology team, and other practitioners by participating in daily rounds, documenting patient needs in the medical record, submitting progress reports to the primary care physician, involving the patient and family in developing the plan of care, collaborating with the home health agencies, and providing informational and emotional support to the patient and family. 12 weeks of enhanced telephone follow-up and surveillance. Control intervention: social services evaluation (25% for usual care group), dietary consultation (15% usual care), physiotherapy/occupational therapy (17% usual care), drug and HF education by staff nurses and any other hospital services. Home care (44%). |
Patients admitted to an academic medical centre with confirmed HF who were at risk for early readmission | Readmissions Mortality Hospital bed days Resource use Patient satisfaction Follow-up at 3 months |
Adequate sequence generation? Unclear Allocation concealment? Unclear Blinding? Yes Incomplete outcome data addressed? Yes Free of selective reporting? Unclear Baseline data? Yes |
|
| Moher et al, 1992 (33) N = 267 |
A nurse employed as a team co-ordinator acted as a liaison between members of the medical team and collected patient information. The nurse facilitated discharge planning. Control intervention: standard medical care. |
Elderly medical patients admitted to a teaching hospital | Hospital LOS Readmission to hospital Discharge destination Patient satisfaction |
Adequate sequence generation? Yes Allocation concealment? Unclear Blinding? Yes Incomplete outcome data addressed? Yes Free of selective reporting? Unclear Baseline data? Yes |
Baseline data recorded only on age, sex, diagnosis Not clear when intervention implemented |
| Naji et al, 1999 (34) N = 343 |
Psychiatrist telephoned GP to discuss patient and make an appointment for the patient to see the GP within 1 week following discharge. A copy of the discharge summary was given to the patient to hand deliver to the GP. Control intervention: standard care. Patients advised to make an appointment to see their GP and were given a copy of the discharge summary to hand deliver to the GP. |
Acute psychiatric admissions | Readmission Mental health status Discharge process Follow-up at 1 month for patient assessed outcomes 6 months for readmissions |
Adequate sequence generation? Yes Allocation concealment? Yes Blinding? Yes Incomplete outcome data addressed? Unclear Free of selective reporting? Unclear Baseline data? Yes |
Psychiatric patients |
| Naughton et al, 1994 (35) N = 111 |
A geriatric evaluation and management team assessed the patient’s mental and physical health status and psychosocial condition to determine level of rehabilitation required and social needs. A geriatrician and social worker were the core team members. Team meetings with the team and nurse specialist and physical therapist took place twice a week to discuss patients’ medical condition, living situation, family and social supports and patient and family’s understanding of the patient’s condition. Social worker responsible for identifying and co-ordinating community resources and ensuring the posthospital treatment place was in place at the time of discharge and 2 weeks later. Nurse specialist co-ordinated the transfer to home health care. Patients who did not have a primary care provider received outpatient care at the hospital. Control intervention: received “usual care” by medical house staff and an attending physician. Social workers and discharge planners were available on request. |
Elderly medical patients admitted from ED in a non-profit academic medical centre | Hospital LOS Discharge destination |
Adequate sequence generation? Yes Allocation concealment? Yes Blinding? Yes Incomplete outcome data addressed? Yes Free of selective reporting? Unclear Baseline data? Yes |
Intervention implemented at time of admission |
| Naylor et al, 1994 (24) N = 276 |
Discharge plan included a comprehensive assessment of the needs of the elderly patient and their caregiver, an education component for the patient and family, and interdisciplinary communication regarding discharge status. Implemented by geriatric nurse specialist and extended from admission to 2 weeks postdischarge with ongoing evaluation of the effectiveness of the discharge plan. Control intervention: routine discharge planning available in the hospital. |
Elderly medical and cardiac surgery patients in an academic medical centre | Hospital LOS Readmission to hospital Health status |
Adequate sequence generation? Unclear Allocation concealment? Unclear Blinding? Yes Incomplete outcome data addressed? Yes Free of selective reporting? Unclear Baseline data? Yes |
Intervention implemented at time of admission |
| Nazareth et al, 2001 (36) N = 362 |
Hospital pharmacist assessed and rationalized the patients’ drug treatment, provided information, and liaised with caregiver and community professionals. Aim was to optimize communication between secondary and primary care professionals. Follow-up visit by community hospital 7–14 days after discharge to check drug and intervene if necessary. Subsequent visits arranged if appropriate. Copy of discharge plan given to the patient, caregiver, community pharmacist, and GP. Follow-up in the community by a pharmacist. Control intervention: discharge from hospital following standard procedures, which included a letter of discharge to the GP. Pharmacist did not provide a review of drugs or follow-up in the community. |
Elderly patients on ≥ 4 drugs who were discharged from 3 acute wards and 1 long-stay ward | Hospital readmission Mortality HRQOL Client satisfaction Knowledge and adherence to prescribed drugs Consultation with GP |
Adequate sequence generation? Yes Allocation concealment? Yes Blinding? Yes Incomplete outcome data addressed? Yes Free of selective reporting? Unclear Baseline data? Yes |
|
| Pardessus et al, 2002 (37) N = 60 |
All admitted patients during the trial period were screened for inclusion and exclusion criteria. 2-hour home visit by occupational therapist and a physical medicine/rehabilitation doctor to evaluate patient abilities in home environment. Enabled observation of patient in their living conditions.. Social supports addressed by social worker. Modification of home hazards and safety advice in home situation, adaptation of recommendations and prescriptions particularly for physical therapy, speedy evaluation of necessary technical aids and social supports. Telephone follow-up was conducted by an occupational therapist to check if the home modifications were completed and assist if necessary. Control intervention: received physical therapy and were informed of home safety and social assistance if required. No home visit. |
Patients aged ≥ 65 years who were hospitalized due to falls and able to return home | Functional status Falls Readmissions Mortality Residential care at 6 and 12 months |
Adequate sequence generation? Yes Allocation concealment? Unclear Blinding? Yes Incomplete outcome data addressed? Yes Free of selective reporting? Unclear Baseline data? Unclear |
|
| Parfrey et al, 1994 (38) N = 841 |
Developed a questionnaire to identify patients requiring discharge planning. Assessment based on the questionnaire that covered the patient’s social circumstances at home, if the admission was an emergency admission or a readmission, use of allied health and community services, mobility and activities of daily living, and medical or surgical condition. Referrals to allied health professionals following completion of the questionnaire for discharge planning. Control intervention: did not receive the questionnaire. Discharge planning occurred if the discharge planning nurses identified a patient or received a referral. |
Medical and surgical patients | Hospital LOS at 6 and 12 months | Adequate sequence generation? Unclear Allocation concealment? Yes Blinding? Yes Incomplete outcome data addressed? Yes Free of selective reporting? Unclear Baseline data? Yes |
Intervention implemented at time of admission |
| Preen et al, 2005 (39) N = 189 |
Discharge planning was based on the Australian Enhanced Primary Care Program and tailored to each patient. Discharge plan was developed 24–48 hours prior to discharge. Problems were identified from hospital notes and patient/caregiver consultation, goals were developed and agreed upon with the patient/caregiver based on personal circumstances and interventions, and community service providers who met patient needs and who were accessible and agreeable to the patient were identified. Discharge plan was faxed to the GP and consultation with the GP was scheduled within 7 days postdischarge. Copies faxed to all service providers identified on the care plan. Research nurse followed up if GP did not respond in 24 hours and the GP scheduled a consultation (within 7 days postdischarge) for patient review. Control intervention: patients were discharged under the hospitals’ existing processes following standard practice in Western Australia where all patients have a discharge summary completed, which was copied to their general practitioner. |
Patients with COPD, cardiovascular disease, or both in 2 tertiary hospitals | SF-12 Patient satisfaction and views of discharge process and GP views of the discharge planning process at 7 days postdischarge |
Adequate sequence generation? Unclear Allocation concealment? Yes Blinding? No Incomplete outcome data addressed? Yes Free of selective reporting? Unclear Baseline data? Yes |
|
| Rich et al, 1993 (40) N = 98 |
Intensive education about HF and its treatment during daily visits by cardiovascular research nurse to discuss diagnosis, symptoms, treatment, follow-up, and prognosis using a 15-page booklet. Dietary advice by dietician and study nurse. Assessment of medication with recommendations designed to improve compliance and reduce adverse effects. Drug card provided detailing the time, dose, and side effects of all drugs. Daily recording of weights emphasized and patients instructed to contact researchers for weight changes in excess of 3 to 5 pounds. Scales provided if needed. Early discharge planning. Patient seen by social worker and member of the home care team to facilitate discharge planning and ease the transition from the hospital to home. Economic, social, and transport problems identified and managed. Enhanced follow-up through home care and telephone contacts with additional assistance provided if needed. Patients visited at home within 48 hours of discharge and then 3 times in the first week and at regular intervals thereafter. At each visit, home care nurse reinforced the teaching materials, reviewed medications, diet and activity guidelines, physical assessment and cardiovascular examination plus assessed for additional problem areas. Study nurse contacted patients by phone and patients were encouraged to call researchers or personal physician with any new problems or questions. Control intervention: all conventional treatments as requested by the patient’s attending physician. These included social service evaluation, dietary and medical teaching, home care, and all other available hospital services. Received study education materials and formal assessment of drugs. |
Older people with HF in an academic medical centre | Hospital LOS Readmission to hospital Readmission days HRQOL |
Adequate sequence generation? Yes Allocation concealment? Unclear Blinding? Yes Incomplete outcome data addressed? Yes Free of selective reporting? Unclear Baseline data? Yes |
|
| Rich et al, 1995 (41) N = 282 |
Inpatient assessment included using a teaching booklet, individualized dietary assessment and instruction by dietician with reinforcement by the cardiovascular research nurse, consultation with social services, assessment of drugs by geriatric cardiologist, intensive follow-up after discharge through the hospital’s home care services plus individualized home visits and telephone contact with the study team. Control intervention: received all standard treatment and services ordered by their primary physicians. | Admitted to an academic medical centre with confirmed HF and at least one risk factor for readmission | Mortality Readmission to hospital HRQOL |
Adequate sequence generation? Yes Allocation concealment? Yes Blinding? Yes Incomplete outcome data addressed? Yes Free of selective reporting? Unclear Baseline data? Yes |
HRQOL data were collected from a subgroup of patients only (n = 126). |
| Shaw et al, 2000 (42) N = 97 |
Predischarge assessment with a pharmacy checklist that assessed patients’ knowledge and identified particular problems such as therapeutic drug monitoring, compliance aid requirements, and side effects. Pharmacy discharge plan supplied to the patients’ community pharmacist for the intervention group. Control intervention: not described. |
Patients discharged from a psychiatric hospital or care of the elderly ward | Readmission to hospital Readmission due to noncompliance Drug problems after discharge |
Adequate sequence generation? Yes Allocation concealment? Yes Blinding? No Incomplete outcome data addressed? Unclear Free of selective reporting? Unclear Baseline data? Yes |
Psychiatric patients |
| Sulch et al, 2000 (43) N = ? |
Rehabilitation and discharge planning with regular review of discharge plan. Senior nurse implemented and integrated care pathway. Multidisciplinary training preceded implementation of the pathway. Pathway piloted for 3 months prior to recruitment to the trial. Control intervention: to avoid contamination, the multidisciplinary process of care received by the control group was reviewed with a 3-month run-in period to ensure implementation. Both groups received comparable amounts of physiotherapy and occupational therapy. |
Patients recovering from stroke in a stroke rehabilitation unit at a teaching hospital | Hospital LOS Discharge destination Mortality at 26 weeks Mortality or institutionalization Activities of daily living HRQOL |
Adequate sequence generation? Yes Allocation concealment? Yes Blinding? No Incomplete outcome data addressed? Yes Free of selective reporting? Unclear Baseline data? Yes |
|
| Weinberger et al, 1996 (44) N = 1,396 |
3 days before discharge a primary nurse assessed the patient’s postdischarge needs. 2 days before discharge the primary care physician visited the patient and discussed patient’s discharge plan with the hospital physician and reviewed the patient. Primary nurse made an appointment for the patient to visit the primary care clinic within 1 week of discharge. Patient given educational materials and a card with the names and beeper numbers of the primary care nurse and physician. Primary care nurse telephoned the patient within 2 working days of discharge Primary care physician and primary nurse reviewed and updated the treatment plan at the first postdischarge appointment. Control intervention: did not have access to the primary care nurse and received no supplementary education or assessment of needs beyond usual care. |
Multicentre patients with diabetes, HF, and COPD. | Readmission to hospital Health status Patient satisfaction Intensity of primary care |
Discharge planning within 3 days of discharge 9 Veterans Administration hospitals participated in the trial |
Abbreviations: COPD, Chronic Obstructive Pulmonary Disease; ED, emergency department; EPOC, Effective Practice and Organization of Care Group; HF, heart failure; HRQOL, health-related quality of life; LOS, length of stay; PCP, primary care provider; RN, registered nurse.
Source: Shepperd et al, 2009. (4).
Table A3: Summary of Interventions Tested in Randomized Controlled Trials.
| Author, Year, Sample Size, Country | Population | Interventions | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predischarge Interventions | Postdischarge Interventions | Interventions Bridging the Transition | |||||||||||
| Patient Education | Discharge Planning | Medication Reconciliation | Appointment Scheduled Before Discharge | Timely PCP Communication | Timely Clinic Follow-up | Follow-up Telephone Call | Postdischarge Hotline | Home Visit | Transition Coach | Patient-Centred Discharge Instructions | Provider Continuity | ||
| Balaban et al, 2008 (12) N = 96 United States |
Community hospital | X | X | X | X | ||||||||
| Bolas et al, 2004 (28) N = 243 Ireland |
X | X | X | ||||||||||
| Evans et al, 1993 (17) N = 835 United States |
Veterans Affairs; high risk | X | |||||||||||
| Harrison et al, 2002 (29) N = 200 Canada |
X | X | X | X | |||||||||
| Hendriksen et al, 1989 (30) N = 273 Denmark |
X | X | X | X | |||||||||
| Jack et al, 2009 (20) N = 738 United States |
Medical/surgical ward | X | X | X | X | X | X | ||||||
| Kennedy et al, 1987 (31) N = 80 United States |
X | X | X | ||||||||||
| Laramee et al (32) 2003, N = 287 United States |
X | X | X | ||||||||||
| Moher et al, 1992 (33) N = 267 Canada |
X | ||||||||||||
| Naji et al, 1999 (34) N = 343 Scotland |
X | X | X | X | |||||||||
| Naughton et al, 1994 (35) N = 111 United States |
X | X | X | ||||||||||
| Naylor et al, 1994 (24) N = 142 United States |
Cardiac (medical/surgical), geriatric | X | X | X | X | X | X | ||||||
| Nazareth et al, 2001 (36) N = 362 United Kingdom |
X | X | X | X | |||||||||
| Pardessus et al, 2002 (37) N = 60 France |
X | X | X | ||||||||||
| Parfrey et al, 1994 (38) N = 841 Canada |
X | X | |||||||||||
| Preen et al, 2005 (39) N = 189 Australia |
X | X | X | X | |||||||||
| Rich et al, 1993 (40) N = 98 United States |
X | X | X | X | X | X | |||||||
| Rich et al, 1995 (41) N = 282 United States |
X | X | X | ||||||||||
| Shaw et al, 2000 (42) N = 97 Scotland |
X | X | |||||||||||
| Sulch et al, 2000 (43) N = 152 United Kingdom |
X | ||||||||||||
| Weinberger et al, 1996 (44) N = 1,396 United States |
X | X | X | X | X | X | |||||||
Abbreviations: PCP, primary care provider.
Source: Shepperd et al, 2009. (4)
Table A4: Randomized Controlled Trials.
| Author, Year, Country | N | Comprehensive Discharge Plan Plus Postdischarge Support | Duration of Follow-up (months) |
|---|---|---|---|
| Single Home Visit | |||
| Stewart et al, 1998 (45) Australia |
97 | Medication counselling and review by clinical pharmacist to promote medication adherence; home visit within 2 weeks of discharge | 6 |
| Stewart et al, 1999 (46) Australia |
200 | Medication review and counselling by clinical pharmacist to promote medication adherence; home visit within 2 weeks of discharge | 6 |
| Jaarsma et al, 1999 (19) Holland |
179 | Medication review and counselling; information card with advice about diet, sodium, and fluid restriction; psychosocial support; home visit within 10 days of discharge | 9 |
| Increased Clinic Follow-up and/or Frequent Telephone Contact | |||
| Cline et al, 1998 (47) Sweden |
190 | 7-day medication organizer; diary to record signs of worsening HF (e.g., body weight, ankle circumference, fatigue); diuretic adjustment; home visit within 2 weeks of discharge | 12 |
| Rainville, 1999 (26) United States |
34 | Medication review and counselling by clinical pharmacist; increased communication between providers; telephone follow-up | 12 |
| Oddone et al, 1999 (47) and Weinberger et al. 1996 (44;48) United States |
443 | Measurement of daily weights; diuretic adjustment, medication review; increased communication between providers; prescheduled clinic appointments in the 6 months after discharge | 6 |
| McDonald et al, 2002 (49) Ireland |
98 | Medication review and counselling; dietary counselling, salt restriction; measurement of daily weights; diuretic adjustment; telephone follow-up at 3 days, then weekly for 12 weeks after hospital discharge | 3 |
| Home Visits and/or Frequent Telephone Contact | |||
| Naylor et al, 1994 (24) United States |
142 | Geriatric discharge protocol; co-ordination of home care; increased communication between providers, telephone follow-up, home visits over 2 weeks after discharge | 3 |
| Naylor et al, 1999 (50) United States |
108 | Geriatric discharge protocol; co-ordination of home care; increased communication between providers, telephone follow-up home visits over 4 weeks after discharge | 6 |
| Serxner et al, 1998 (51) | 109 | Reinforcement of medication adherence; daily weights; dietary restrictions; increased communication between providers; additional mailing of educational materials; telephone follow-up for 3 months after discharge | 3 |
| United States | |||
| Blue et al, 2001 (52) England |
165 | Dietary counselling; optimization of medications; increased communication between providers; home visits; telephone follow-up | 12 |
| Riegel et al, 2002 (53) United States |
358 | Computerized assessment of patient and caregiver support; telephonic case management; monitoring of weight gain and dyspnea; increased communication between providers; multiple telephone calls for 6 months after discharge | 6 |
| Krumholz et al, 2002 (54) United States |
88 | Nurse-recommended follow-up based on patients’ reports of symptoms; telephone monitoring; follow-up for 12 months after discharge | 12 |
| Extended Home Care Services | |||
| Rich et al, 1993 (40) United States |
98 | Dietary and social service consultation; medication review by geriatric cardiologist; increased communication between providers; intensive follow-up for 3 months after discharge | 3 |
| Rich et al, 1995 (41) United States |
282 | Dietary and social service consultation; mediation review by geriatric cardiologist; increased communication between providers; intensive follow-up for 3 months after discharge | 12 |
| Harrison et al, 2002 (29) Canada |
192 | Management of medications, diet, exercise, and stress through community nurse visits; increased communication between providers; telephone follow-up; home care for 2 weeks after discharge | 3 |
| Laramee et al, 2003 (32) United States |
287 | Guidance with medications, diet, fluid intake, and daily weights (e.g., home scales, pill boxes); increased communication between providers; telephone follow-up; home care for 12 weeks after discharge | 3 |
| Day Hospital Services | |||
| Capomolla et al, 2002 (55) Italy |
234 | Exercise training; daily weight monitoring; fluid restriction; physical training; optimal medication regimen; increased communication between providers; available day hospital services for 12 months after discharge | 12 |
Abbreviations: HF, heart failure.
Source: Phillips et al, 2004. (11)
Table A5: Summary of Interventions Tested in Randomized Controlled Trials.
| Author, Year, Size, Country | Interventions | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predischarge Interventions | Postdischarge Interventions | Interventions Bridging the Transition | ||||||||||
| Patient Education | Discharge Planning | Medication Reconciliation | Appointment Scheduled Before Discharge | Timely PCP Communication | Timely Clinic Follow-up | Follow-up Telephone Call | Postdischarge Hotline | Home Visit | Transition Coach | Patient-Centred Discharge Instructions | Provider Continuity | |
| Blue et al, 2001 (52) N = 165 United Kingdom |
X | X | X | X | X | X | ||||||
| Capomolla et al, 2002 (55) N = 234 Italy |
X | X | X | X | X | |||||||
| Cline et al, 1998 (47) N = 190 Sweden |
X | X | X | X | ||||||||
| Harrison et al, 2002 (29) N = 200 Canada |
X | X | X | X | ||||||||
| Jaarsma et al, 1999 (19) N = 179 Holland |
X | X | X | X | X | |||||||
| Krumholz et al, 2002 (54) N = 88 United States |
X | X | X | |||||||||
| Laramee et al, 2003 (32) N = 287 United States |
X | X | X | X | X | |||||||
| McDonald et al, 2002 (49) N = 98 Ireland |
X | X | ||||||||||
| Naylor et al, 1994 (24) N = 142 United States |
X | X | X | X | X | X | ||||||
| Naylor et al, 1999 (50) N = 108 United States |
X | X | X | X | X | |||||||
| Oddone et al, 1999 (48)and Weinberger et al. (44) N = 443 United States |
X | X | X | X | X | X | ||||||
| Rainville, 1999 (26) N = 34 United States |
X | X | ||||||||||
| Rich et al, 1993 (40) N = 98 United States |
X | X | X | X | X | X | ||||||
| Rich et al, 1995 (41) N = 282 United States |
X | X | X | |||||||||
| Riegel et al, 2002 (53) N = 358 United States |
X | X | X | X | ||||||||
| Serxner et al, 1998 (51) N = 109 United States |
X | X | X | X | ||||||||
| Stewart et al, 1998 (45) N = 97 Australia |
X | X | X | |||||||||
| Stewart et al, 1999 (46) N = 200 Australia |
X | X | X | |||||||||
Abbreviations: PCP, primary care provider.
Source: Phillips et al, 2004 (11).
Appendix 3: GRADE Tables
Table A6: GRADE Evidence Profile for Comparison of Predischarge Planning Care and Usual Care.
| No. of Studies (Design) | Risk of Bias | Inconsistency | Indirectness | Imprecision | Publication Bias | Upgrade Considerations | Quality |
|---|---|---|---|---|---|---|---|
| Readmissions | |||||||
| 2 systematic reviews of RCTs | Some serious limitations (-1)a |
No serious limitationsb | No serious limitations | No serious limitations | Undetected | None | ⊕⊕⊕ Moderate |
| Length of Stay | |||||||
| 1 systematic review of RCTs | Some serious limitations (-1)c |
No serious limitationsd | No serious limitations | No serious limitations | Undetected | None | ⊕⊕⊕ Moderate |
| Mortality/Survival | |||||||
| 1 systematic review of RCTs | Some serious limitations (-1)e |
No serious limitationsf | No serious limitations | No serious limitations | Undetected | None | ⊕⊕⊕ Moderate |
| HRQOL | |||||||
| 1 systematic review of RCTs | Very serious limitations (-2)g |
Some serious limitations (-1)h |
No serious limitations | No serious limitations | Undetected | None | ⊕ Very Low |
| Patient Satisfaction | |||||||
| 1 systematic review of RCTs | Very serious limitations (-2)i |
Some serious limitations (-1)j |
No serious limitations | No serious limitations | Undetected | None | ⊕ Very Low |
Abbreviations: EPOC, Effective Practice and Organization of Care Group; No., number; RCT, randomized controlled trial
Average EPOC Risk of Bias score in studies included in systematic review by Hansen et al was 5 out of 9.
The systematic review by Shepperd et al focused on discharge planning and excluded RCTs evaluating interventions where discharge planning was not the main focus of a multifaceted package of care. It was not possible to assess how some components of the process compared between trials (e.g., inclusion of caregivers and the extent of their care). Adequate sequence generation and allocation concealment were reported in 14/21 and 12/21 trials respectively.
Shepperd et al found a significant difference in readmission favouring discharge planning versus usual care. Hansen et al did not conduct a meta-analysis due to heterogeneity among the included studies and could not make a conclusion as to which comprehensive discharge bundle/package was most effective compared with usual care.
The systematic review by Shepperd et al focused on discharge planning and excluded RCTs evaluating interventions where discharge planning was not the main focus of a multifaceted package of care. It was not possible to assess how some components of the process compared between trials (e.g., inclusion of caregivers and the extent of their care). Adequate sequence generation and allocation concealment were reported in 14/21 and 12/21 trials respectively.
Shepperd et al found a significant difference in hospital LOS favouring discharge planning. Phillips et al (11) did not find a significant difference in hospital LOS between the comprehensive discharge planning and postdischarge follow-up and usual care. Not all studies in the systematic reviews reported on hospital LOS.
The systematic review by Shepperd et al focused on discharge planning and excluded RCTs evaluating interventions where discharge planning was not the main focus of a multifaceted package of care. It was not possible to assess how some components of the process compared between trials (e.g., inclusion of caregivers and the extent of their care). Adequate sequence generation and allocation concealment were reported in 14/21 and 12/21 trials respectively.
Shepperd et al did not find a significant difference in mortality between study arms. No significant heterogeneity in summary statistic.
The systematic review by Shepperd et al focused on discharge planning and excluded RCTs evaluating interventions where discharge planning was not the main focus of a multifaceted package of care. It was not possible to assess how some components of the process compared between trials (e.g., inclusion of caregivers and the extent of their care). Adequate sequence generation and allocation concealment were reported in 14/21 and 12/21 trials respectively. HRQOL was a secondary endpoint in 3 studies that reported this outcome and measured using different scales in subgroups of patients.
A meta-analysis was not conducted by Shepperd et al for the HRQOL outcome due to the heterogeneity and diverse measurement techniques used by the 3 individual studies. One study reported no significant difference between the study arms. Another study only provided HRQOL data for baseline measurements. A third study showed a significant difference between study arms at 26 weeks follow-up in favour of the control group.
This outcome was reported in 3 studies in the systematic review by Shepperd et al and a meta-analysis was not conducted. Satisfaction was reported as a secondary outcome and performed on subgroups of patients using different measurement scales.
Two studies reported a significant difference between study arms, one study did not.
Table A7: GRADE Evidence Profile for Comparison of Predischarge Planning Plus Postdischarge Support and Usual Care.
| No. of Studies (Design) | Risk of Bias | Inconsistency | Indirectness | Imprecision | Publication Bias | Upgrade Considerations | Quality |
|---|---|---|---|---|---|---|---|
| Readmissions | |||||||
| 2 systematic reviews of RCTs 4 recent RCTs |
Some serious limitations (-1)a |
Some serious limitations (-1)b |
No serious limitations | No serious limitations | Undetected | None | ⊕⊕ Low |
| Length of Stay | |||||||
| 1 systematic review of RCTs | Some serious limitations (-1)c |
Some serious limitations (-1)d |
No serious limitations | No serious limitations | Undetected | None | ⊕⊕ Low |
| Mortality/Survival | |||||||
| 1 Systematic Review of RCTs 1 recent RCT |
Some serious limitations (-1)e |
Some serious limitations (-1)f |
No serious limitations | No serious limitations | Undetected | None | ⊕⊕ Low |
| HRQOL | |||||||
| 1 systematic review of RCTs 2 recent RCTs |
Very serious limitations (-2)g |
Some serious limitations (-1)h |
No serious limitations | No serious limitations | Undetected | None | ⊕ Very Low |
| Patient Satisfaction | |||||||
| 1 recent RCT | Very serious limitations (-2)i |
Some serious limitations (-1)j |
No serious limitations | No serious limitations | Undetected | None | ⊕ Very Low |
Abbreviations: EPOC, Effective Practice and Organization of Care Group; HF, heart failure; No., number; RCT, randomized controlled trial
Average EPOC Risk of Bias score in studies included in systematic review by Hansen et al was 5 out of 9.
The systematic review by Phillips et al (11) reported that 16/18 RCTs were assigned a Jadad score of 4 out of 5 and 2 studies reported a score of 3 out of 5. The overall summary estimate was significantly heterogeneous (P < 0.001). When a large study was removed from meta-analysis, heterogeneity was reduced but was still significant (P = 0.04)
Some significant differences in baseline characteristics between treatment arms in recent RCTs.
Phillips et al (11) found a significant difference in readmissions favouring comprehensive discharge planning with postdischarge support, however, there was significant statistical heterogeneity. Hansen et al did not conduct a meta-analysis due to heterogeneity among the included studies and could not make a conclusion as to which comprehensive discharge bundle/package was most effective compared with usual care. Of the 4 recent RCTs that were not included in the previous systematic reviews, 1 found a significant difference in readmissions favouring comprehensive pre- and postdischarge care.
The systematic review by Phillips et al (11) reported that 16/18 RCTs were assigned a Jadad score of 4 out of 5 and 2 studies reported a score of 3 out of 5. Hospital LOS was not reported in all studies included in the systematic reviews and of those that did, it was reported as a secondary outcome.
Phillips et al (11) did not find a significant difference in hospital LOS between the comprehensive discharge planning and postdischarge follow-up and usual care. Not all studies in the systematic reviews reported on hospital LOS. None of the 4 recent RCTs reported on hospital LOS.
The systematic review by Phillips et al (11) reported that 16/18 RCTs were assigned a Jadad score of 4 out of 5 and 2 studies reported a score of 3 out of 5. Mortality/survival was not reported in all studies included in the systematic reviews and of those that did, it was reported as a secondary outcome. One of the 4 recent RCTs reported a significant reduction in mortality for patients in the intervention group. (RCT incorporated an additional component to postdischarge follow-up [HF clinics]).
Phillips et al (11) did not find a significant difference in mortality between study arms. One of the 4 recent RCTs reported mortality and found a significant difference favouring comprehensive discharge planning and follow-up (Unlike the studies included in Phillips et al, this RCT also incorporated HF clinic visits as part of the intervention.)
The systematic review by Phillips et al reported that 16/18 RCTs were assigned a Jadad score of 4 out of 5 and 2 studies reported a score of 3 out of 5. HRQOL was not reported in all studies included in the systematic reviews and of those that did, it was assessed using different measurement tools and reported as a secondary outcome.
Two of the 4 recent RCTs reported HRQOL. One study had significant differences in baseline characteristics between study arms and the other RCT incorporated an additional component to postdischarge follow-up (HF clinics).
Phillips et al (11) meta-analyzed data for this outcome and reported that HRQOL scores of intervention patients improved significantly more than usual care patients. (Statistical heterogeneity was not reported.) One of the 4 recent RCTs reported a significant improvement in HRQOL for patients receiving comprehensive discharge planning (this study also incorporated HF clinic visits in the postdischarge follow-up). One RCT reported a significant improvement in HRQOL at one time point during follow-up (12 weeks). No significant difference was found at any other time point (2, 6, 26, and 52 weeks).
Significantly more patients with hypertension in the control group than the treatment group at baseline. This endpoint was a secondary outcome and performed on a subgroup of patients.
Satisfaction with care was greater in intervention patients at 2 and 6 weeks, however, no other time points were reported in a study that lasted 12 weeks.
Table A8: Risk of Bias Among Randomized Controlled Trials for the Comparison of Predischarge Planning Plus Postdischarge Support to Usual Care.
| Author, Year | Allocation Concealment | Blinding | Complete Accounting of Patients and Outcome Events | Selective Reporting Bias | Other Limitations |
|---|---|---|---|---|---|
| Atienza et al, 2004 (59) | No limitations | Limitationsa | No limitations | No limitations | No limitations |
| Naylor et al, 2004 (56) | No limitations | No limitations | No limitations | No limitations | Limitationsb |
| Kwok et al, 2008 (57) | No limitations | Limitationsc | Limitationsd | No limitations | Limitationse |
| Zhao et al, 2009 (58) | No limitations | Limitationsf | Limitationsg | No limitations | Limitationsh |
Blinding not discussed in paper.
Significant difference in baseline hypertension between study arms.
Patients knew their group assignment.
Intent-to-treat analysis not performed.
No statistical comparisons of baseline characteristics, yet differences noted. E.g., 47% (intervention) vs. 25% (control) on security assistance.
Not reported.
Intent-to-treat analysis not performed.
Instruments used to measure patient understanding, adherence and satisfaction not standardized or validated. Data regarding extent of coronary heart disease in patient arms not reported (severity).
Suggested Citation
This report should be cited as follows: McMartin K. Discharge planning in chronic conditions: an evidence-based analysis. Ont Health Technol Assess Ser [Internet]. 2013 September;13(4):1–72. Available from: http://www.hqontario.ca/en/documents/eds/2013/full-report-OCDM-discharge-planning.pdf.
Indexing
The Ontario Health Technology Assessment Series is currently indexed in MEDLINE/PubMed, Excerpta Medica/EMBASE, and the Centre for Reviews and Dissemination database.
Permission Requests
All inquiries regarding permission to reproduce any content in the Ontario Health Technology Assessment Series should be directed to: EvidenceInfo@hqontario.ca.
How to Obtain Issues in the Ontario Health Technology Assessment Series
All reports in the Ontario Health Technology Assessment Series are freely available in PDF format at the following URL: http://www.hqontario.ca/en/mas/mas_ohtas_mn.html.
Conflict of Interest Statement
All reports in the Ontario Health Technology Assessment Series are impartial. There are no competing interests or conflicts of interest to declare.
Peer Review
All reports in the Ontario Health Technology Assessment Series are subject to external expert peer review. Additionally, Health Quality Ontario posts draft reports and recommendations on its website for public comment prior to publication. For more information, please visit: http://www.hqontario.ca/en/mas/ohtac_public_engage_overview.html.
About Health Quality Ontario
Health Quality Ontario (HQO) is an arms-length agency of the Ontario government. It is a partner and leader in transforming Ontario’s health care system so that it can deliver a better experience of care, better outcomes for Ontarians and better value for money.
Health Quality Ontario strives to promote health care that is supported by the best available scientific evidence. HQO works with clinical experts, scientific collaborators and field evaluation partners to develop and publish research that evaluates the effectiveness and cost-effectiveness of health technologies and services in Ontario.
Based on the research conducted by HQO and its partners, the Ontario Health Technology Advisory Committee (OHTAC) — a standing advisory sub-committee of the HQO Board — makes recommendations about the uptake, diffusion, distribution or removal of health interventions to Ontario’s Ministry of Health and Long-Term Care, clinicians, health system leaders and policy-makers.
This research is published as part of Ontario Health Technology Assessment Series, which is indexed in CINAHL, EMBASE, MEDLINE, and the Centre for Reviews and Dissemination. Corresponding OHTAC recommendations and other associated reports are also published on the HQO website. Visit http://www.hqontario.ca for more information.
About the Ontario Health Technology Assessment Series
To conduct its comprehensive analyses, HQO and/or its research partners reviews the available scientific literature, making every effort to consider all relevant national and international research; collaborates with partners across relevant government branches; consults with clinical and other external experts and developers of new health technologies; and solicits any necessary supplemental information.
In addition, HQO collects and analyzes information about how a health intervention fits within current practice and existing treatment alternatives. Details about the diffusion of the intervention into current health care practices in Ontario add an important dimension to the review. Information concerning the health benefits; economic and human resources; and ethical, regulatory, social, and legal issues relating to the intervention assist in making timely and relevant decisions to optimize patient outcomes.
The public consultation process is available to individuals and organizations wishing to comment on reports and recommendations prior to publication. For more information, please visit: http://www.hqontario.ca/en/mas/ohtac_public_engage_overview.html.
Disclaimer
This report was prepared by HQO or one of its research partners for the Ontario Health Technology Advisory Committee and developed from analysis, interpretation, and comparison of scientific research. It also incorporates, when available, Ontario data and information provided by experts and applicants to HQO. It is possible that relevant scientific findings may have been reported since completion of the review. This report is current to the date of the literature review specified in the methods section, if available. This analysis may be superseded by an updated publication on the same topic. Please check the HQO website for a list of all publications: http://www.hqontario.ca/en/mas/mas_ohtas_mn.html.
Health Quality Ontario
130 Bloor Street West, 10th Floor
Toronto, Ontario
M5S 1N5
Tel: 416-323-6868
Toll Free: 1-866-623-6868
Fax: 416-323-9261
Email: EvidenceInfo@hqontario.ca
ISSN 1915-7398 (online)
ISBN 978-1-4606-1237-8 (PDF)
© Queen’s Printer for Ontario, 2013
List of Tables
| Table 1: Body of Evidence Examined According to Study Design |
| Table 2: Summary of Systematic Reviews |
| Table 3: Results of Two Meta-Analyses – Comparison of Individualized Discharge Planning Versus Usual Care and Comprehensive Discharge Planning With Postdischarge Support Versus Usual Care |
| Table 4: Summary of Interventions Tested in Randomized Controlled Trials Included in Systematic Review |
| Table 5: Results of Discharge Planning Compared with Usual Care |
| Table 6: Readmission Rates with Comprehensive Discharge Planning Plus Postdischarge Support Compared with Usual Care |
| Table 7: Summary of Recent Studies Not Included in Systematic Reviews |
| Table 8: Summary of Results |
| Table 9: Results of Discharge Planning Compared with Usual Care |
| Table 10: Results of Discharge Planning Compared with Usual Care |
| Table 11: Conclusions of Evidence-Based Review |
| Table A1: Quality (EPOC) of Randomized Controlled Trialsa |
| Table A2: Randomized Controlled Trials |
| Table A3: Summary of Interventions Tested in Randomized Controlled Trials |
| Table A4: Randomized Controlled Trials |
| Table A5: Summary of Interventions Tested in Randomized Controlled Trials |
| Table A6: GRADE Evidence Profile for Comparison of Predischarge Planning Care and Usual Care |
| Table A7: GRADE Evidence Profile for Comparison of Predischarge Planning Plus Postdischarge Support and Usual Care |
| Table A8: Risk of Bias Among Randomized Controlled Trials for the Comparison of Predischarge Planning Plus Postdischarge Support to Usual Care |
List of Figures
| Figure 1: Citation Flow Chart |
List of Abbreviations
- 6MWT
6-minute walking test
- APN
Advanced practice nurse
- CAD
Coronary artery disease
- CI
Confidence interval
- COPD
Chronic obstructive pulmonary disease
- EPOC
Effective Practice and Organization of Care Group
- HQO
Health Quality Ontario
- HRQOL
Health-related quality of life
- LOS
Length of stay
- RCT
Randomized controlled trial
- RR
Relative risk
- SD
Standard deviation
References
- 1.Naylor MD, Aiken LH, Kurtzman ET, Olds DM, Hirschman KB. The care span: the importance of transitional care in achieving health reform. 2011;30(4):746–54. doi: 10.1377/hlthaff.2011.0041. Health Aff. [DOI] [PubMed] [Google Scholar]
- 2.Holland DE, Harris MR. Discharge planning, transitional care, coordination of care and continuity of care: clarifying concepts and terms from the hospital perspective. 2007;26(4):3–19. doi: 10.1300/J027v26n04_02. Home Health Care Serv Q. [DOI] [PubMed] [Google Scholar]
- 3.Samuels-Kalow ME, Stack AM, Porter SC. Effective discharge communication in the emergency department. Forthcoming. 2012 doi: 10.1016/j.annemergmed.2011.10.023. Ann Emerg Med. [DOI] [PubMed] [Google Scholar]
- 4.Shepperd S, McClaran J, Phillips CO, Lannin NA, Clemson LM, McCluskey A, et al. Discharge planning from hospital to home. 2010 Mar;(1) doi: 10.1002/14651858.CD000313.pub3. Cochrane Database Sys Re. CD000313. [DOI] [PubMed] [Google Scholar]
- 5.Guyatt GH, Oxman AD, Shunemann HJ, Tugwell P, Knottnerus A. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. 2011;64(4):380–2. doi: 10.1016/j.jclinepi.2010.09.011. Clin Epidemiol. [DOI] [PubMed] [Google Scholar]
- 6.Goodman C. Literature searching and evidence interpretation for assessing health care practices. 81 p. SBU Report No. 119E. 1996 doi: 10.1017/s0266462300008321. Stockholm (SE): Swedish Council on Technology Assessment in Health Care. [DOI] [PubMed] [Google Scholar]
- 7.Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. 2011;155(8):520–8. doi: 10.7326/0003-4819-155-8-201110180-00008. Ann Intern Med. [DOI] [PubMed] [Google Scholar]
- 8.Scott IA. Preventing the rebound: improving care transition in hospital discharge processes. 2010;2010;34(4) doi: 10.1071/AH09777. Aust Health Rev. [DOI] [PubMed] [Google Scholar]
- 9.Kumar S, Grimmer-Somers K. A synthesis of the secondary literature on effectiveness of hospital avoidance and discharge programs. 2007;31(1):34–48. Aust Health Rev. [PubMed] [Google Scholar]
- 10.Mistiaen P, Francke AL, Poot E. Interventions aimed at reducing problems in adult patients discharged from hospital to home: a systematic meta-review. 2007 doi: 10.1186/1472-6963-7-47. BMC Health Serv Res. 7:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Phillips CO, Wright SM, Kern DE, Singa RM, Shepperd S, Rubin HR. Comprehensive discharge planning with postdischarge support for older patients with congestive heart failure: a meta-analysis. 2004;291(11):1358–67. doi: 10.1001/jama.291.11.1358. JAMA. [DOI] [PubMed] [Google Scholar]
- 12.Balaban RB, Weissman JS, Samuel PA, Woolhandler S. Redefining and redesigning hospital discharge to enhance patient care: a randomized controlled study. 2008;23(8):1228–33. doi: 10.1007/s11606-008-0618-9. Gen Intern Med. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Braun E, Baidusi A, Alroy G, Azzam ZS. Telephone follow-up improves patients satisfaction following hospital discharge. 2009 Mar;20(2):221–5. doi: 10.1016/j.ejim.2008.07.021. Eur Intern Med. [DOI] [PubMed] [Google Scholar]
- 14.Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. 2006;166(17):1822–8. doi: 10.1001/archinte.166.17.1822. Arch Intern Med. [DOI] [PubMed] [Google Scholar]
- 15.Dudas V, Bookwalter T, Kerr KM, Pantilat SZ. The impact of follow-up telephone calls to patients after hospitalization. 2001;111(9B):26S–30S. doi: 10.1016/s0002-9343(01)00966-4. Am J Med. [DOI] [PubMed] [Google Scholar]
- 16.Dunn RB, Lewis PA, Vetter NJ, Guy PM, Hardman CS, Jones RW. Health visitor intervention to reduce days of unplanned hospital readmission in patients recently discharged from geriatric wards: the results of a randomised controlled study. 1994;18(1):15–23. doi: 10.1016/0167-4943(94)90044-2. Arch Gerontol Geriatr. [DOI] [PubMed] [Google Scholar]
- 17.Evans RL, Hendricks RD. Evaluating hospital discharge planning: a randomized clinical trial. 1993;31(4):358–70. doi: 10.1097/00005650-199304000-00007. Med Care. [DOI] [PubMed] [Google Scholar]
- 18.Forster AJ, Clark HD, Menard A, Dupuis N, Chernish R, Chandok N, et al. Effect of a nurse team coordinator on outcomes for hospitalized medicine patients. 2005;118(10):1148–53. doi: 10.1016/j.amjmed.2005.04.019. Am J Med. [DOI] [PubMed] [Google Scholar]
- 19.Jaarsma T, Halfens R, Huijer Abu-Saad H, Dracup K, Gorgels T, van Ree J, et al. Effects of education and support on self-care and resource utilization in patients with heart failure. 1999;20(9):673–82. doi: 10.1053/euhj.1998.1341. Eur Heart J. [DOI] [PubMed] [Google Scholar]
- 20.Jack BW, Chetty VK, Anthony D, Greenwald JL, Sanchez GM, Johnson AE, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. 2009;150(3):178–87. doi: 10.7326/0003-4819-150-3-200902030-00007. Ann Intern Med. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Koehler BE, Richter KM, Youngblood L, Cohen BA, Prengler ID, Cheng D, et al. Reduction of 30-day postdischarge hospital readmission or emergency department (ED) visit rates in high-risk elderly medical patients through delivery of a targeted care bundle. 2009;4(4):211–8. doi: 10.1002/jhm.427. J Hosp Med. [DOI] [PubMed] [Google Scholar]
- 22.Kwok T, Lum CM, Chan HS, Ma HM, Lee D, Woo J. A randomized controlled trial of an intensive community nurse-supported discharge program in preventing hospital readmissions of older patients with chronic lung disease. 2004;52(8):1240–6. doi: 10.1111/j.1532-5415.2004.52351.x. Am Geriatr Soc. [DOI] [PubMed] [Google Scholar]
- 23.McDonald K, Ledwidge M, Cahill J, Kelly J, Quigley P, Maurer B, et al. Elimination of early rehospitalization in a randomized controlled trial of multidisciplinary care in a high-risk, elderly heart failure population: the potential contributions of specialist care, clinical stability and optimal angiotensin-converting enzyme inhibitor dose at discharge. 2001;3(2):209–15. doi: 10.1016/s1388-9842(00)00134-3. Eur Heart Fail. [DOI] [PubMed] [Google Scholar]
- 24.Naylor M, Brooten D, Jones R, Lavizzo-Mourey R, Mezey M, Pauly M. Comprehensive discharge planning for the hospitalized elderly: a randomized clinical trial. 1994;120(12):999–1006. doi: 10.7326/0003-4819-120-12-199406150-00005. Ann Intern Med. [DOI] [PubMed] [Google Scholar]
- 25.Parry C, Min SJ, Chugh A, Chalmers S, Coleman EA. Further application of the care transitions intervention: results of a randomized controlled trial conducted in a fee-for-service setting. 2009;(2-3):84–99. doi: 10.1080/01621420903155924. Home Health Care Serv Q. 28. [DOI] [PubMed] [Google Scholar]
- 26.Rainville EC. Impact of pharmacist interventions on hospital readmissions for heart failure. 1999;56(13):1339–42. Am Health Syst Pharm. [PubMed] [Google Scholar]
- 27.Wong FK, Chow S, Chung L, Chang K, Chan T, Lee WM, et al. Can home visits help reduce hospital readmissions? Randomized controlled trial. 2008;62(5):585–95. doi: 10.1111/j.1365-2648.2008.04631.x. J Adv Nurs. [DOI] [PubMed] [Google Scholar]
- 28.Bolas H, Brookes K, Scott M, McElnay J. Evaluation of a hospital-based community liaison pharmacy service in Northern Ireland. 2004;26(2):114–20. doi: 10.1023/b:phar.0000018601.11248.89. Pharm World Sci. [DOI] [PubMed] [Google Scholar]
- 29.Harrison MB, Browne GB, Roberts J, Tugwell P, Gafni A, Graham ID. Quality of life of individuals with heart failure: a randomized trial of the effectiveness of two models of hospital-to-home transition. 2002;40(4):271–82. doi: 10.1097/00005650-200204000-00003. Med Care. [DOI] [PubMed] [Google Scholar]
- 30.Hendriksen C, Stromgard E, Sorensen KH. Cooperation concerning admission to and discharge of elderly people from the hospital: the coordinated contributions of home care personnel. 1989;151(24):1531–4. Ugeskr Laeger. [PubMed] [Google Scholar]
- 31.Kennedy L, Neidlinger S, Scroggins K. Effective comprehensive discharge planning for hospitalized elderly. 1987;27(5):577–80. doi: 10.1093/geront/27.5.577. Gerontologist. [DOI] [PubMed] [Google Scholar]
- 32.Laramee AS, Levinsky SK, Sargent J, Ross R, Callas P. Case management in a heterogeneous congestive heart failure population: a randomized controlled trial. 2003;163(7):809–17. doi: 10.1001/archinte.163.7.809. Arch Intern Med. [DOI] [PubMed] [Google Scholar]
- 33.Moher D, Weinberg A, Hanlon R, Runnalls K. Effects of a medical team coordinator on length of hospital stay. 1992;146(4):511–5. CMAJ. [PMC free article] [PubMed] [Google Scholar]
- 34.Naji SA, Howie FL, Cameron IM, Walker SA, Andrew J, Eagles JM. Discharging psychiatric in-patients back to primary care: a pragmatic randomized controlled trial of a novel discharge. 1999;5(3):109–15. Primary Care Psychia. [Google Scholar]
- 35.Naughton BJ, Moran MB, Feinglass J, Falconer J, Williams ME. Reducing hospital costs for the geriatric patient admitted from the emergency department: a randomized trial. 1994;42(10):1045–9. doi: 10.1111/j.1532-5415.1994.tb06207.x. Am Geriatr Soc. [DOI] [PubMed] [Google Scholar]
- 36.Nazareth I, Burton A, Shulman S, Smith P, Haines A, Timberall H. A pharmacy discharge plan for hospitalized elderly patients: a randomized controlled trial. 2001;30(1):33–40. doi: 10.1093/ageing/30.1.33. Age Ageing. [DOI] [PubMed] [Google Scholar]
- 37.Pardessus V, Puisieux F, Di Pompeo C, Gaudefroy C, Thevenon A, Dewailly P. Benefits of home visits for falls and autonomy in the elderly: a randomized trial study. 2002;81(4):247–52. doi: 10.1097/00002060-200204000-00002. Am J Phys Med Rehabil. [DOI] [PubMed] [Google Scholar]
- 38.Parfrey PS, Gardner E, Vavasour H, Harnett JD, McManamon C, McDonald J, et al. The feasibility and efficacy of early discharge planning initiated by the admitting department in two acute care hospitals. 1994;17(2):88–96. Clin Invest Med. [PubMed] [Google Scholar]
- 39.Preen DB, Bailey BE, Wright A, Kendall P, Phillips M, Hung J, et al. Effects of a multidisciplinary, post-discharge continuance of care intervention on quality of life, discharge satisfaction, and hospital length of stay: a randomized controlled trial. 2005;17(1):43–51. doi: 10.1093/intqhc/mzi002. Int Qual Health Care. [DOI] [PubMed] [Google Scholar]
- 40.Rich MW, Vinson JM, Sperry JC, Shah AS, Spinner LR, Chung MK, et al. Prevention of readmission in elderly patients with congestive heart failure: results of a prospective, randomized pilot study. 1993;8(11):585–90. doi: 10.1007/BF02599709. Gen Intern Med. [DOI] [PubMed] [Google Scholar]
- 41.Rich MW, Beckham V, Wittenberg C, Leven CL, Freedland KE, Carney RM. A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure. 1995;333(18):1190–5. doi: 10.1056/NEJM199511023331806. N Engl Med. [DOI] [PubMed] [Google Scholar]
- 42.Shaw H, Mackie CA, Sharkie I. Evaluation of effect of pharmacy discharge planning on medication problems experienced by discharged acute admission mental health patients. 2000;8(2):144–53. Int J Pharm Prac. [Google Scholar]
- 43.Sulch D, Perez I, Melbourn A, Kalra L. Randomized controlled trial of integrated (managed) care pathway for stroke rehabilitation. 2000;31(8):1929–34. doi: 10.1161/01.str.31.8.1929. Stroke. [DOI] [PubMed] [Google Scholar]
- 44.Weinberger M, Oddone EZ, Henderson WG. Does increased access to primary care reduced hospital readmissions? 1996;334(22):1441–7. doi: 10.1056/NEJM199605303342206. N Engl Med. [DOI] [PubMed] [Google Scholar]
- 45.Stewart S, Pearson S, Horowitz JD. Effects of a home-based intervention among patients with congestive heart failure discharged from acute hospital care. 1998;158(10):1067–72. doi: 10.1001/archinte.158.10.1067. Arch Intern Med. [DOI] [PubMed] [Google Scholar]
- 46.Stewart S, Marley JE, Horowitz JD. Effects of a multidisciplinary home-based intervention on planned readmissions and survival among patients with chronic congestive heart failure: a randomised controlled study. 1999;354(9184):1077–83. doi: 10.1016/s0140-6736(99)03428-5. Lancet. [DOI] [PubMed] [Google Scholar]
- 47.Cline CM, Israelsson BY, Willenheimer RB, Broms K, Erhardt LR. Cost effective management programme for heart failure reduces hospitalisation. 1998;80(5):442–6. doi: 10.1136/hrt.80.5.442. Heart. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Oddone EZ, Weinberger M, Giobbie-Hurder A, Landsman P, Henderson W. Enhanced access to primary care for patients with congestive heart failure. 1999;2(5):201–9. Eff Clin Prac. [PubMed] [Google Scholar]
- 49.McDonald K, Ledwidge M, Cahill J, Quigley P, Maurer B, Travers B, et al. Heart failure management: multidisciplinary care has intrinsic benefit above the optimization of medical care. 2002;8(3):142–8. doi: 10.1054/jcaf.2002.124340. J Card Fail. [DOI] [PubMed] [Google Scholar]
- 50.Naylor MD, Brooten D, Campbell R, Jacobsen BS, Mezey MD, Pauly MV, et al. Comprehensive discharge planning and home followup of hospitalized elders: a randomized trial. 1999;281(7):613–20. doi: 10.1001/jama.281.7.613. JAMA. [DOI] [PubMed] [Google Scholar]
- 51.Serxner S, Miyaji M, Jeffords J. Congestive heart failure disease management study: a patient education intervention. 1998;4:23–8. Congestive Heart Fail. [Google Scholar]
- 52.Blue L, Lange E, McMurray JJV, Davie AP, McDonagh TA, Murdoch DR, et al. Randomised controlled trial of specialist nurse intervention in heart failure. 2001;323(7315):715–8. doi: 10.1136/bmj.323.7315.715. BMJ. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Riegel B, Carlson B, Kopp Z, LePetri B, Glaser D, Unger A. Effect of a standardized nurse case-management telephone intervention on resource use in patients with chronic heart failure. 2002;162(6):705–12. doi: 10.1001/archinte.162.6.705. Arch Intern Med. [DOI] [PubMed] [Google Scholar]
- 54.Krumholz HM, Amatruda J, Smith GL, Mattera JA, Roumanis SA, Radford MJ, et al. Randomized trial of an education and support intervention to prevent readmission of patients with heart failure. 2002;39(1):83–9. doi: 10.1016/s0735-1097(01)01699-0. J Am Coll Cardiol. [DOI] [PubMed] [Google Scholar]
- 55.Capomolla S, Febo O, Ceresa M, Caporotondi A, Guazzotti G, La Rovere M, et al. Cost/utility ratio in chronic heart failure: comparison between heart failure management program delivered by day-hospital and usual care. 2002;40(7):1259–66. doi: 10.1016/s0735-1097(02)02140-x. Am Coll Cardiol. [DOI] [PubMed] [Google Scholar]
- 56.Naylor MD, Brooten DA, Campbell RL, Maislin G, McCauley KM, Schwartz JS. Transitional care of older adults hospitalized with heart failure: a randomized controlled trial. 2004;52(5):675–84. doi: 10.1111/j.1532-5415.2004.52202.x. Am Geriatr Soc. [DOI] [PubMed] [Google Scholar]
- 57.Kwok T, Lee J, Woo J, Lee DT, Griffith S. A randomized controlled trial of a community nurse-supported hospital discharge programme in older patients with chronic heart failure. 2008;17(1):109–17. doi: 10.1111/j.1365-2702.2007.01978.x. Clin Nurs. [DOI] [PubMed] [Google Scholar]
- 58.Zhao Y, Wong FK. Effects of a postdischarge transitional care programme for patients with coronary heart disease in China: a randomised controlled trial. 2009;18(17):2444–55. doi: 10.1111/j.1365-2702.2009.02835.x. Clin Nurs. [DOI] [PubMed] [Google Scholar]
- 59.Atienza F, Anguita M, Martinez-Alzamora N, Osca J, Ojeda S, Almenar L, et al. Multicenter randomized trial of a comprehensive hospital discharge and outpatient heart failure management program. 2004;6(5):643–52. doi: 10.1016/j.ejheart.2003.11.023. Eur Heart Fail. [DOI] [PubMed] [Google Scholar]


