Abstract
Objective
We examined the leading causes of unintentional injury and suicide mortality in adults across the urban-rural continuum.
Methods
Injury mortality data were drawn from a representative cohort of 2,735,152 Canadians aged ≥25 years at baseline, who were followed for mortality from 1991 to 2001. We estimated hazard ratios and 95% confidence intervals for urban-rural continuum and cause-specific unintentional injury (i.e., motor vehicle, falls, poisoning, drowning, suffocation, and fire/burn) and suicide (i.e., hanging, poisoning, firearm, and jumping) mortality, adjusting for socioeconomic and demographic characteristics.
Results
Rates of unintentional injury mortality were elevated in less urbanized areas for both males and females. We found an urban-rural gradient for motor vehicle, drowning, and fire/burn deaths, but not for fall, poisoning, or suffocation deaths. Urban-rural differences in suicide risk were observed for males but not females. Declining urbanization was associated with higher risks of firearm suicides and lower risks of jumping suicides, but there was no apparent trend in hanging and poisoning suicides.
Conclusion
Urban-rural gradients in adults were more pronounced for unintentional motor vehicle, drowning, and fire/burn deaths, as well as for firearm and jumping suicide deaths than for other causes of injury mortality. These results suggest that the degree of urbanization may be an important consideration in guiding prevention efforts for many causes of injury fatality.
Injury is a leading cause of mortality in Canada, accounting for approximately 14,500 deaths each year.1 Although the majority of injury deaths are unintentional (29.5 deaths per 100,000 inhabitants), intentional deaths due to suicide (11.6 deaths per 100,000 inhabitants) are also common. Research shows that adults in rural areas are disproportionately affected by injury mortality.2–6 With populations of Western countries aging rapidly, particularly in rural areas,7 a better understanding of injury mortality in rural adults becomes increasingly important.
Only a limited number of studies have examined the relative contribution of different unintentional and intentional causes to urban-rural differences in injury mortality, despite the potential of cause-specific data to uncover possible underlying mechanisms and pathways for prevention.8,9 The few studies of unintentional injury that examined causes beyond motor vehicle collisions and falls were limited by dichotomous categorizations of urban and rural areas, which may decrease the ability to capture differences in injury mortality across the range of geographical areas typically present in Western countries. In fact, it has been proposed that a continuum-based approach of urban and rural areas better reflects social, economic, and geographic diversity and may enhance our understanding of health variation across areas.2,10
There is also very limited information on how method-specific suicide mortality varies across the urban-rural continuum. One study found elevated firearm suicide rates in less urbanized areas,11 but data do not exist for more common causes of suicide, such as hanging or poisoning. In light of the identified research gaps, we sought to determine the relationship between the urban-rural continuum and leading causes of unintentional injury and suicide mortality in Canadian adults.
METHODS
Data source
Data on injury mortality came from the 1991–2001 Canadian Census Mortality Follow-up Study, which tracked mortality for 10.6 years among respondents to the 1991 Census.12 The cohort represents a 15% sample of the Canadian noninstitutionalized population aged ≥25 years at baseline (n=2,735,152).
Variables
We used International Classification of Diseases (ICD) codes for principal cause of death (ICD Ninth Revision for 1991–1999 and ICD Tenth Revision for 2000–2001) to identify unintentional injury (E800–E869, E880–E929, V01–X59, and Y85–Y86) and suicide (E950–E959, E980–E989, X60–X84, Y87.0, Y10–Y34, Y87.2, and Y89.9) deaths.13,14 Cause-specific unintentional injuries included falls, motor vehicle collisions, poisoning, suffocation, fire/burns, and drowning. Cause-specific suicide deaths included hanging/strangulation/suffocation, poisoning, firearms, and jumping. Because suicides may be misclassified as “undetermined,”15 undetermined deaths were included as suicides.
We used municipality of residence at the time of cohort inception to determine urban-rural status, and we defined urban-rural continuum using an eight-category typology that differentiated urban areas on the basis of population size and rural areas according to degree of urban influence.10 Urban influence was based on percentage of residents commuting to, and distance from, urban cores. The categories, in declining order of urbanization, were defined as (1) very large urban areas with ≥1 million residents, (2) large urban areas with 500,000–999,999 residents, (3) medium urban areas with 100,000–499,999 residents, (4) small urban areas with 10,000–99,999 residents, (5) rural areas with a strong urban influence, (6) rural areas with a moderate urban influence, (7) rural areas with a weak urban influence, and (8) remote rural areas with no urban influence.
Covariates suggested by the literature included sex, age (10-year bands), marital status (legally married, common-law, never married, and separated/divorced/widowed), educational attainment (university degree, post-secondary diploma, high school diploma, and no high school diploma), income (ratio of family income to low-income cutoff,12 in quintiles), employment status (employed, unemployed, and not in the labor force), visible minority (no; yes—black/Asian/Arab/Pacific Islander/Latin American/multiple), immigrant status (immigrant ≤10 years, immigrant >10 years, and Canadian-born), provincial region (Atlantic, Québec, Ontario, Prairie, and British Columbia/territories), and neighborhood-level material deprivation quintile (composite score of census data on the proportion of people with no high school diploma, ratio of employment to population, and average income16).
Statistical analysis
We computed age-standardized mortality rates using the direct method, with the 1991 population as the reference. We estimated hazard ratios (HRs) and 95% confidence intervals (CIs) using Cox proportional hazards regression. Time of observation started on census day (June 4, 1991) and ended on day of injury death (event), death from another cause (censored), or December 31, 2001 (censored). The proportional hazard assumption was verified with log(-log Survival) curves. For causes of injury with sufficient numbers, we performed analyses for males and females separately, as previous research indicates that the relationship between urban-rural status and injury mortality can differ by sex.2,3,17
Initial models estimated age-adjusted hazards of all-cause and cause-specific unintentional injury and suicide death for the urban-rural continuum. Subsequent models additionally adjusted for all covariates. In sensitivity analyses, we ran final models excluding undetermined deaths, with a follow-up period ending in 1999 to ensure that the change in ICD coding in 2000 did not bias results, and using age as the underlying time.18,19 We accounted for clustering in neighborhood enumeration areas by using the robust sandwich estimator in select models. All analyses were performed using SAS® version 9.1.20
RESULTS
There were 260,820 deaths during the study period; 8,316 (3.0%) were due to unintentional injuries and 4,095 (1.6%) were due to suicides. For both causes of death, rates were higher in rural areas, although a clear gradient was not always present (Table 1). For both males and females, rates of unintentional injury and suicide mortality were higher for individuals who had lower socioeconomic status (i.e., education, income, employment, and neighborhood deprivation) and were separated/divorced/widowed or never married. Injury mortality rates were also greater for individuals born in Canada and, except for female unintentional injury, not of visible minority.
Table 1.
Age-standardized mortality rates per 100,000 person-years for males and females at risk for unintentional injury and suicide: Canadian Census Mortality Follow-up Study cohort, 1991–2001
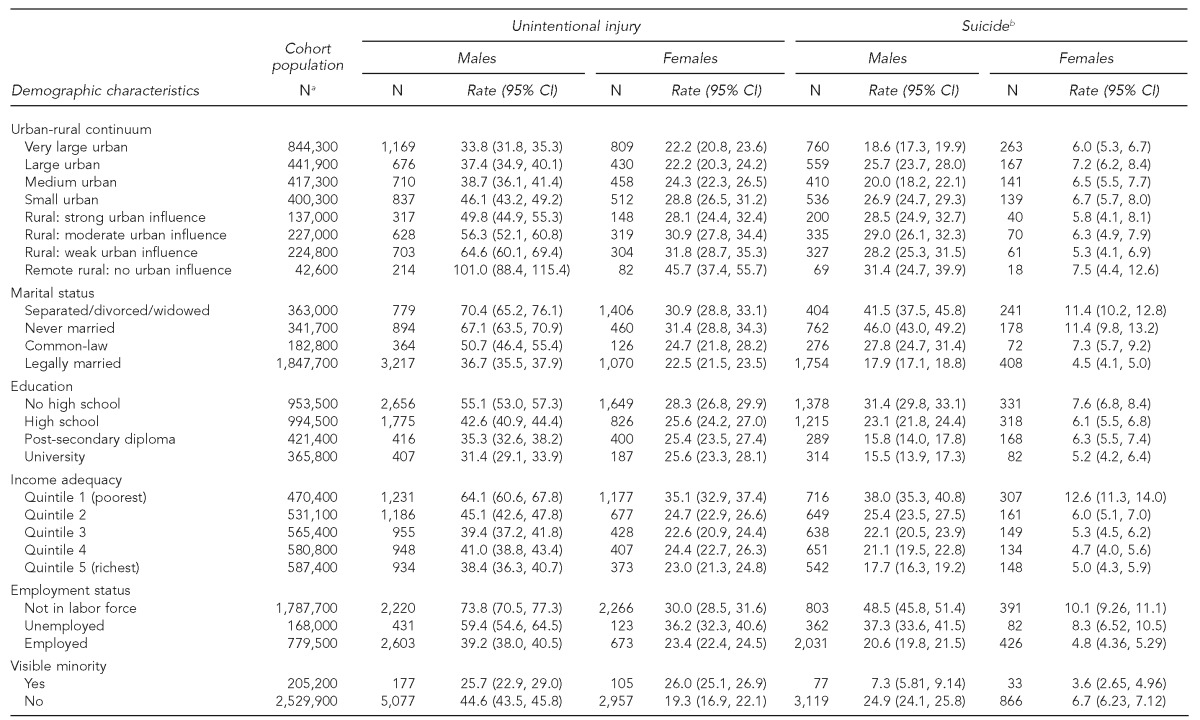
aCensus population counts rounded to nearest 100
bSuicides plus undetermined deaths
CI = confidence interval
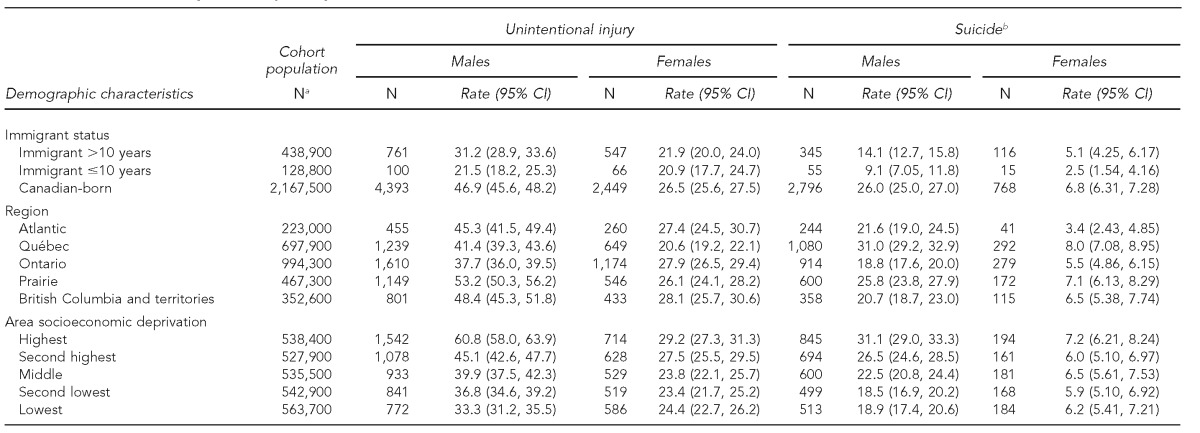
Less urbanized areas exhibited higher age-adjusted HRs for unintentional injuries in both males and females (Table 2). Risk of unintentional injury in remote rural areas was twice that of very large urban areas. HRs for suicide were elevated only among males in most areas relative to very large urban ones, but with little evidence of a gradient.
Table 2.
Associations between the urban-rural continuum and unintentional injury and suicide mortality: Canadian Census Mortality Follow-up Study cohort, 1991–2001
aSuicides plus undetermined deaths
bAdjusted for marital status, educational attainment, income, employment status, visible minority, immigrant status, provincial region, and area-level deprivation
HR = hazard ratio
CI = confidence interval
Ref. = reference group
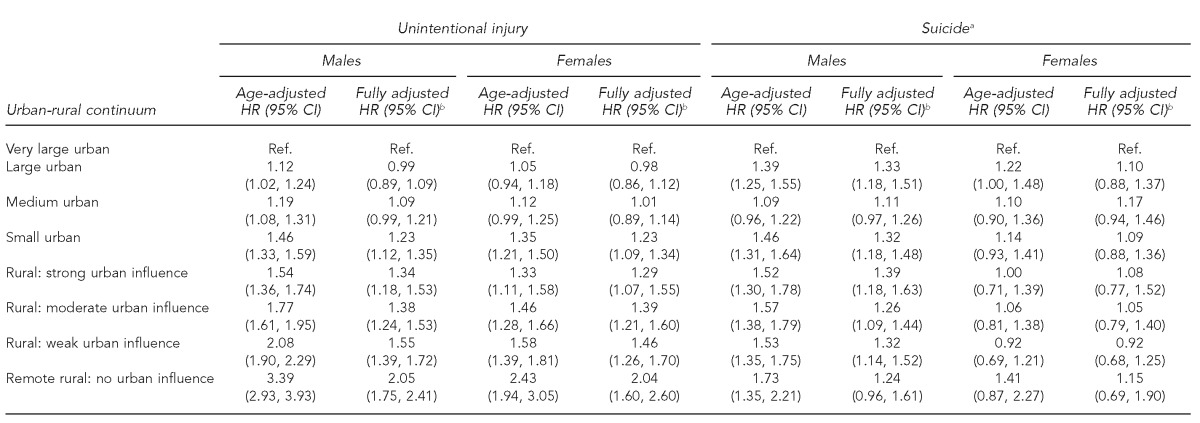
Associations between unintentional injury mortality and the urban-rural continuum differed by injury cause (Table 3). There was no association with falls, poisoning, or suffocation deaths. The risk of death in motor vehicle collisions in rural areas, however, was more than twice that of very large urban areas and was also elevated in small urban areas. Relative to very large urban areas, the risks of drowning and fire/burn deaths were also elevated in small urban and rural areas, especially remote rural areas with no urban influence (drowning HR=6.34, 95% CI 4.03, 9.98; fire/burn HR=4.03, 95% CI 2.18, 7.44).
Table 3.
Associations between the urban-rural continuum and cause-specific unintentional injury deaths: Canadian Census Mortality Follow-up Study cohort, 1991–2001
aAdjusted for marital status, educational attainment, income, employment status, visible minority, immigrant status, provincial region, and area-level deprivation
HR = hazard ratio
CI = confidence interval
Ref. = reference group
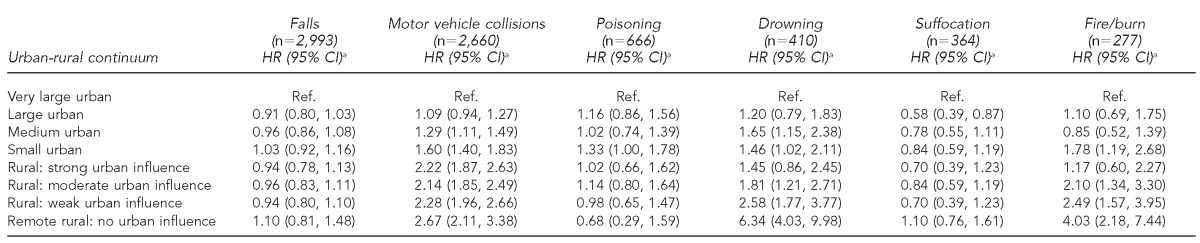
Associations with the urban-rural continuum for suicide also varied depending on the cause (Table 4). The risk of suicide by hanging was 48% higher in remote rural areas with no urban influence relative to very large urban areas, and there was a marginally higher risk in small urban areas. The pattern for poisoning suicides was unclear, but risks tended to be lower in rural areas. HRs for firearm suicides were higher in all other areas relative to very large urban areas, particularly remote rural areas (HR=3.43, 95% CI 2.35, 5.00). In contrast, HRs for jumping suicides were lower in all areas relative to very large urban ones, especially rural areas with a strong urban influence (HR=0.16, 95% CI 0.04, 0.68).
Table 4.
Associations between the urban-rural continuum and cause-specific suicide deaths:a Canadian Census Mortality Follow-up Study cohort, 1991–2001
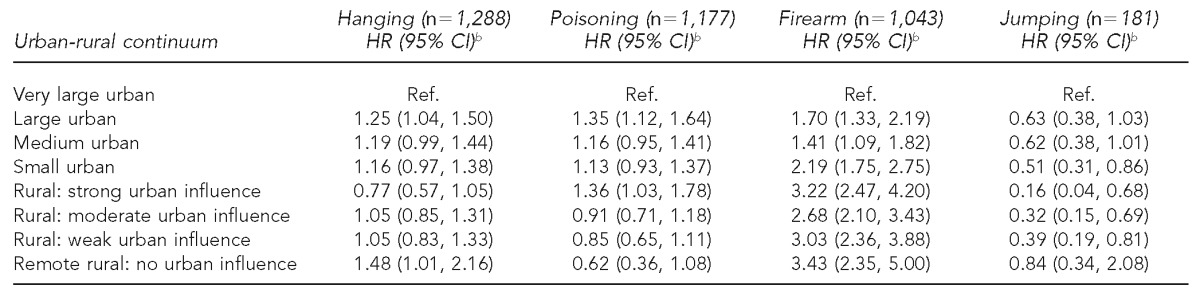
aSuicide plus undetermined deaths
bAdjusted for marital status, educational attainment, income, employment status, visible minority, immigrant status, provincial region, and area-level deprivation
HR = hazard ratio
CI = confidence interval
Ref. = reference group
Models excluding undetermined deaths, with follow-up ending in 1999, accounting for clustering, and using age as the underlying time, showed similar results (data not shown).
DISCUSSION
Our study used detailed census data linked with leading causes of injury mortality to investigate relationships with the urban-rural continuum for a large, nationally representative Canadian adult population.12 The risk of unintentional injury was significantly higher in small urban and rural areas compared with very large urban areas for both males and females. HRs for suicide in males were elevated for most areas relative to very large urban areas, but there was no difference across areas for females. Not all causes of injury were associated with urban-rural differences. Unintentional motor vehicle, drowning, and fire/burn deaths tended to increase as areas became less urbanized, but we observed no urban-rural differences for falls, poisoning, or suffocation deaths. Relative to very large urban areas, all areas had higher risks of firearm suicides, and most areas had lower risks of jumping suicides. There was little difference in hanging and poisoning suicides across areas.
Unintentional injury mortality
The doubling in risk of motor vehicle-related mortality in rural compared with very large urban areas is in line with several Canadian studies2,3,5 but much greater than the 7% and 88% higher rural rates reported in Australia9 and Ireland,8 respectively. The urban-rural dichotomy used in the latter studies might have attenuated associations, lending support for our use of an urban-rural continuum. The literature on urban-rural differences for drowning and fire/burn deaths is inconsistent and depends on setting. Higher rates of drowning in rural areas were reported in Ireland8 and China17 but not Australia.9 In contrast, rates of fire/burn deaths were higher in rural areas of Australia9 but not Ireland8 or China.17 The risks observed for rural relative to urban areas in these studies were again lower than the risks we observed.
One possible reason for greater injury mortality in rural areas is that rural residents have more exposure to injury risk in their environment than in urban areas. Motor vehicle crashes may be more frequent in rural areas because residents travel longer distances, often on narrow roads with poor lighting, or on steep, unprotected embankments.5,6,8,21 Although traffic volume is associated with injury and is greater in urban areas, speeds are higher in rural areas, with a greater likelihood of more serious injury. The elevated risk of drowning in rural areas in our study may reflect occupational risks (fishing), exposure to open bodies of water during recreational activities, or weaker regulation of pool enclosures.
There may also be differences in behavioral norms between urban and rural residents. Adults in rural areas use protective safety devices such as bicycle helmets,22 seatbelts,6 and smoke detectors23 less frequently than their urban counterparts. Rural residents may also be more likely to drive under the influence of alcohol and use high-risk recreational vehicles,6,8 whereas urban residents are more likely to rely on public transportation. There may be less efficient dissemination of safety messages, fewer programs to promote safety devices, or less stringent enforcement of safety devices in rural areas.24 Socioeconomic and demographic factors likely only partially account for urban-rural differences in adult injury mortality because HRs were only slightly attenuated in adjusted models, as was found in studies from the United Kingdom25 and New Zealand.26
Additionally, urban-rural differences in the quality and accessibility of emergency and medical care services can influence injury mortality. Delayed response times and long distances to health services are another probable explanation for the disproportionate injury mortality found in rural areas.27 However, our results indicate that urban-rural differences were present for some but not all causes, suggesting causal mechanisms beyond delayed care. This finding is supported by elevated nonfatal injury rates observed in rural areas,24,27 although rural hospitals with potentially greater bed availability may be more likely to admit patients for observation, especially if less imaging equipment is available to assess injury severity, or patients have long distances to drive after discharge.2,28
We found no urban-rural differences for fall, poisoning, or suffocation mortality. Similar results were reported by some studies for mortality by falls2,9 and poisoning,9 but higher rates in urban areas have also been reported.8,17 Two studies found higher rural rates of suffocation.9,17 Despite the absence of urban-rural differences for these injury causes in our study, circumstances may differ by geographic area. For example, falls in rural areas may be related to occupations such as forestry or mining, whereas falls in urban areas may involve stairs or icy sidewalks.
Suicide mortality
Our results for suicide align with a Canadian study in Québec province that found significant urban-rural differences for males only.2 A national-level study also reported a higher suicide risk in rural areas for males but a lower risk for females, relative to urban areas.5 Several early studies from other countries also showed lower rural rates, but these urban-rural differences largely disappeared in the mid- to late-1990s.25,26,29
The greater sex differential in rural areas may reflect occupational differences of males and females, as forestry and farming are associated with greater suicide risk among males.30 Also, males are more likely to commit suicide by firearms, a weapon commonly found in rural areas.31
Sociocultural and historical features of communities such as shared norms, traditions, values, and interests; networks of community support; social cohesion and social capital; and mobility into and out of communities26,32 have been proposed to explain urban-rural differences in suicide. Stigma attached to mental illness and help-seeking may be greater in rural areas, leading to underreporting of suicide and underestimation of urban-rural differences.29 Despite fewer physician consultations by rural than urban residents, there were no differences in reported unmet health-care needs between urban and rural residents in Québec.2 Other research has not found a link between rural residence and psychological distress; to the contrary, some studies of mental health show stress to be higher in urban areas.26 Furthermore, a Canadian study noted that rural residents had a stronger sense of community belonging,5 which is a protective factor for suicide.33,34 These findings may help explain why urban-rural differences were inconsistent for suicide in our study.
The urban-rural differences in cause-specific suicide may reflect differential access to means of suicide rather than contextual differences. Higher firearm suicide rates in more rural areas may be due to the greater number of firearms on farms and in the countryside.8 There is a strong link between firearm availability and suicide rates.29 Some Canadian researchers suggest that the decline in male firearm suicide rates in Québec toward the end of the 1990s was related to restrictive firearms regulations introduced in 1991 and 1995.35 These factors may have played a greater role in urban than in rural areas, particularly in very large urban areas such as Montréal.
In contrast, the risk of suicide by jumping was lower in the smallest urban and several rural areas relative to very large urban areas. This finding could be expected given the large number of high buildings and bridges in larger urban areas. However, Gunnell et al. argue that the quantity of available jumping sites is less important than their accessibility or popularity as a method.36 The construction of suicide barriers on bridges in several Canadian cities may have helped limit the accessibility of some jumping sites, but these preventive efforts may not be sufficiently widespread or have reduced the popularity of this method.37
In contrast to firearms and jumping, means to commit suicide by hanging or poisoning are likely to be equally available in urban and rural areas. We had no data on substances used in poisoning, but they may more frequently involve pesticides in rural areas and medications in urban areas.
Implications for research and prevention
Injury prevention strategies have generally been developed with urban areas in mind and may not be applicable to rural areas. For example, open bodies of water in rural areas cannot be easily fenced, and bicycle helmets are less effective in high-speed collisions on rural roads.21 Our results suggest that efforts to prevent unintentional motor vehicle, drowning, and fire/burn injury deaths need to target rural populations, particularly very remote areas. Improving rural road conditions and raising road safety awareness,5 implementing water safety programs in unsupervised rural settings,8 and promoting functional fire alarms in rural areas are warranted. On the other hand, prevention of fall, poisoning, and suffocation mortality should focus equally on urban and rural residents. Prevention strategies should consider that rural areas are increasingly composed of older adults.
Restricting access to lethal methods can be effective in preventing suicide.38 Most firearm-related suicides involve shotguns and rifles, as these firearms are most often found in homes, especially in rural areas.31 Despite evidence suggesting that restrictive firearms regulations in Canada contributed to a decrease in suicides,35,39,40 firearm registration remains a contentious issue. If urban-rural differences in firearm suicides increase following the recent abolishment of the long-gun registry, this increase would provide further evidence of the need to restrict access to these weapons. Physical barriers are effective in reducing suicides at particular jumping sites, although evidence regarding displacement of suicides to other sites remains inconclusive.41–44 Preventing access to the means of suicide does not, however, address individual psychological distress. Other interventions, such as depression screening and treatment, are likely to be important for reducing high suicide rates in urban and rural areas.35,38
Limitations
Our study was subject to several limitations. Although we considered several measures of individual- and -area-level socioeconomic status, we could not account for other possible determinants of urban-rural -differences, such as service availability, care-seeking behaviors, differences in exposure (e.g., distance driven or car ownership), road conditions, risk-taking, or the use of safety equipment.5,27 We were also unable to account for self-selection of individuals into areas—a problem common to most area-based studies. Furthermore, our samples were small in rural areas, particularly for some injury causes, leading to a lack of precision in estimates. Additionally, we only examined leading causes; other injuries that did not contribute enough to the total numbers could not be included. Categorization of undetermined deaths as suicides may have slightly overestimated suicide rates and underestimated unintentional deaths, but the extent is unknown and likely was nondifferential across the urban-rural continuum. Finally, we used place of residence at the beginning of the study period to specify urban-rural status, and available data suggest that up to 10% of the population migrated between urban and rural areas during the study period. However, misclassification of urban-rural status was likely nondifferential, thus attenuating the results toward the null and yielding conservative estimates.45,46
CONCLUSION
This study showed that less urbanized areas exhibited elevated risks of unintentional motor vehicle-related, drowning, and fire/burn deaths, as well as firearm suicides in Canadian adults. In contrast, jumping suicides were lower in rural areas. These results suggest that degree of urbanization may be an important consideration in guiding prevention efforts for several important causes of injury fatalities. In urban areas, attention should be paid to jumping suicides, whereas other causes of unintentional and intentional injury should be considered in rural areas.
Acknowledgments
The researchers thank the Health Analysis Division of Statistics Canada for facilitating access to the Canadian Mortality Database and Barry Pless for valuable comments on an earlier version of this article. Ethical approval for the follow-up study was obtained from the Statistics Canada Policy Committee and the Research Ethics Committee of the University of Toronto.
REFERENCES
- 1.Public Health Agency of Canada. Leading causes of death and hospitalization in Canada [cited 2012 Jul 16] Available from: URL: http://www.phac-aspc.gc.ca/publicat/lcd-pcd97/table1-eng.php.
- 2.Pampalon R, Martinez J, Hamel D. Does living in rural areas make a difference for health in Québec? Health Place. 2006;12:421–35. doi: 10.1016/j.healthplace.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 3.Pampalon R, Hamel D, Gamache P. Recent changes in the geography of social disparities in premature mortality in Québec. Soc Sci Med. 2008;67:1269–81. doi: 10.1016/j.socscimed.2008.06.010. [DOI] [PubMed] [Google Scholar]
- 4.Bell N, Simons RK, Lakha N, Hameed SM. Are we failing our rural communities? Motor vehicle injury in British Columbia, Canada, 2001–2007. Injury. 2012;43:1888–91. doi: 10.1016/j.injury.2011.07.018. [DOI] [PubMed] [Google Scholar]
- 5.Canadian Institute for Health Information. How healthy are rural Canadians? An assessment of their health status and health determinants. Ottawa (Ontario): Canadian Institute for Health Information; 2006. [Google Scholar]
- 6.Kmet L, Brasher P, Macarthur C. A small area study of motor vehicle crash fatalities in Alberta, Canada. Accid Anal Prev. 2003;35:177–82. doi: 10.1016/s0001-4575(01)00101-4. [DOI] [PubMed] [Google Scholar]
- 7.Statistics Canada. Profile of the Canadian population by age and sex: Canada ages. Ottawa (Ontario): Statistics Canada; 2002. [Google Scholar]
- 8.Boland M, Staines A, Fitzpatrick P, Scallan E. Urban-rural variation in mortality and hospital admission rates for unintentional injury in Ireland. Inj Prev. 2005;11:38–42. doi: 10.1136/ip.2004.005371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mitchell RJ, Chong S. Comparison of injury-related hospitalised morbidity and mortality in urban and rural areas in Australia. Rural Remote Health. 2010;10:1326. [PubMed] [Google Scholar]
- 10.Janes D, McNiven C, Puderer H. Census metropolitan area and census agglomeration influenced zones (MIZ): a description of the methodology. 2000 [cited 2012 May 20] Available from: URL: http://www5.statcan.gc.ca/bsolc/olc-cel/olc-cel?lang=eng&catno=92F0138MIE2000002.
- 11.Branas CC, Nance ML, Elliott MR, Richmond TS, Schwab CW. Urban-rural shifts in intentional firearm death: different causes, same results. Am J Public Health. 2004;94:1750–5. doi: 10.2105/ajph.94.10.1750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wilkins R, Tjepkema M, Mustard C, Choinière R. The Canadian census mortality follow-up study, 1991 through 2001. Health Rep. 2008;19:24–43. [PubMed] [Google Scholar]
- 13.World Health Organization. International classification of diseases, 9th revision. Geneva: WHO; 1977. [Google Scholar]
- 14.World Health Organization. ICD-10 classifications of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. Geneva: WHO; 1992. [Google Scholar]
- 15.Värnik P, Sisask M, Värnik A, Arensman E, Van Audenhove C, van der Feltz-Cornelis CM, et al. Validity of suicide statistics in Europe in relation to undetermined deaths: developing the 2–20 benchmark. Inj Prev. 2012;18:321–5. doi: 10.1136/injuryprev-2011-040070. [DOI] [PubMed] [Google Scholar]
- 16.Pampalon R, Hamel D, Gamache P, Raymond G. A deprivation index for health planning in Canada. Chronic Dis Can. 2009;29:178–91. [PubMed] [Google Scholar]
- 17.Hu G, Baker SP, Baker TD. Urban-rural disparities in injury mortality in China, 2006. J Rural Health. 2010;26:73–7. doi: 10.1111/j.1748-0361.2009.00255.x. [DOI] [PubMed] [Google Scholar]
- 18.Korn EL, Graubard BI, Midthune D. Time-to-event analysis of longitudinal follow-up of a survey: choice of the time-scale. Am J Epidemiol. 1997;145:72–80. doi: 10.1093/oxfordjournals.aje.a009034. [DOI] [PubMed] [Google Scholar]
- 19.Pencina MJ, Larson MG, D'Agostino RB. Choice of time scale and its effect on significance of predictors in longitudinal studies. Stat Med. 2007;26:1343–59. doi: 10.1002/sim.2699. [DOI] [PubMed] [Google Scholar]
- 20.SAS Institute, Inc. SAS®: Version 9.1. Cary (NC): SAS Institute, Inc.; 2004. [Google Scholar]
- 21.Hwang HC, Stallones L, Keefe TJ. Childhood injury deaths: rural and urban differences, Colorado 1980–8. Inj Prev. 1997;3:35–7. doi: 10.1136/ip.3.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harlos S, Warda L, Buchan N, Klassen TP, Koop VL, Moffatt ME. Urban and rural patterns of bicycle helmet use: factors predicting usage. Inj Prev. 1999;5:183–8. doi: 10.1136/ip.5.3.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harvey PA, Sacks JJ, Ryan GW, Bender PF. Residential smoke alarms and fire escape plans. Public Health Rep. 1998;113:459–64. [PMC free article] [PubMed] [Google Scholar]
- 24.Tiesman H, Zwerling C, Peek-Asa C, Sprince N, Cavanaugh JE. Non-fatal injuries among urban and rural residents: the National Health Interview Survey, 1997–2001. Inj Prev. 2007;13:115–9. doi: 10.1136/ip.2006.013201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Middleton N, Gunnell D, Frankel S, Whitley E, Dorling D. Urban-rural differences in suicide trends in young adults: England and Wales, 1981–1998. Soc Sci Med. 2003;57:1183–94. doi: 10.1016/s0277-9536(02)00496-3. [DOI] [PubMed] [Google Scholar]
- 26.Pearce J, Barnett R, Jones I. Have urban/rural inequalities in suicide in New Zealand grown during the period 1980–2001? Soc Sci Med. 2007;65:1807–19. doi: 10.1016/j.socscimed.2007.05.044. [DOI] [PubMed] [Google Scholar]
- 27.Jiang X, Li D, Boyce W, Pickett W. Variations in injury among Canadian adolescents by urban-rural geographic status. Chronic Dis Can. 2007;28:56–62. [PubMed] [Google Scholar]
- 28.Macpherson AK, To TM, Parkin PC, Moldofsky B, Wright JG, Chipman ML, et al. Urban/rural variation in children's bicycle-related injuries. Accid Anal Prev. 2004;36:649–54. doi: 10.1016/S0001-4575(03)00086-1. [DOI] [PubMed] [Google Scholar]
- 29.Singh GK, Siahpush M. Increasing rural-urban gradients in US suicide mortality, 1970–1997. Am J Public Health. 2002;92:1161–7. doi: 10.2105/ajph.92.7.1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mustard CA, Bielecky A, Etches J, Wilkins R, Tjepkema M, Amick BC, et al. Suicide mortality by occupation in Canada, 1991–2001. Can J Psychiatry. 2010;55:369–76. doi: 10.1177/070674371005500606. [DOI] [PubMed] [Google Scholar]
- 31.Coalition for Gun Control. Bill C-391 [cited 2012 Jul 12] Available from: URL: http://www.guncontrol.ca/English/Home/C391/C391.htm.
- 32.Macintyre S, Ellaway A, Cummins S. Place effects on health: how can we conceptualise, operationalise and measure them? Soc Sci Med. 2002;55:125–39. doi: 10.1016/s0277-9536(01)00214-3. [DOI] [PubMed] [Google Scholar]
- 33.Durkheim E. Suicide: a study in sociology. London: Routledge; 1951. [Google Scholar]
- 34.Evans J, Middleton N, Gunnell D. Social fragmentation, severe mental illness and suicide. Soc Psychiatry Psychiatr Epidemiol. 2004;39:165–70. doi: 10.1007/s00127-004-0733-9. [DOI] [PubMed] [Google Scholar]
- 35.Gagne M, Robitaille Y, Hamel D, St-Laurent D. Firearms regulation and declining rates of male suicide in Québec. Inj Prev. 2010;16:247–53. doi: 10.1136/ip.2009.022491. [DOI] [PubMed] [Google Scholar]
- 36.Gunnell D, Middleton N, Frankel S. Method availability and the prevention of suicide—a re-analysis of secular trends in England and Wales 1950–1975. Soc Psychiatry Psychiatr Epidemiol. 2000;35:437–43. doi: 10.1007/s001270050261. [DOI] [PubMed] [Google Scholar]
- 37.Sinyor M, Levitt AJ. Effect of a barrier at Bloor Street Viaduct on suicide rates in Toronto: natural experiment. BMJ. 2010;341:c2884. doi: 10.1136/bmj.c2884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mann JJ, Apter A, Bertolote J, Beautrais A, Currier D, Haas A, et al. Suicide prevention strategies: a systematic review. JAMA. 2005;294:2064–74. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- 39.Bridges FS. Gun control law (Bill C-17), suicide, and homicide in Canada. Psychol Rep. 2004;94(3 Pt 1):819–26. doi: 10.2466/pr0.94.3.819-826. [DOI] [PubMed] [Google Scholar]
- 40.Leenaars AA, Moksony F, Lester D, Wenckstern S. The impact of gun control (Bill C-51) on suicide in Canada. Death Stud. 2003;27:103–24. doi: 10.1080/07481180302890. [DOI] [PubMed] [Google Scholar]
- 41.Pelletier AR. Preventing suicide by jumping: the effect of a bridge safety fence. Inj Prev. 2007;13:57–9. doi: 10.1136/ip.2006.013748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Reisch T, Michel K. Securing a suicide hot spot: effects of a safety net at the Bern Muenster Terrace. Suicide Life Threat Behav. 2005;35:460–7. doi: 10.1521/suli.2005.35.4.460. [DOI] [PubMed] [Google Scholar]
- 43.Perron S, Burrows S, Fournier M, Perron PA, Quellet F. Installation of a bridge barrier as a suicide prevention strategy in Montréal, Québec, Canada. Am J Public Health. 2013;103:1235–9. doi: 10.2105/AJPH.2012.301089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bennewith O, Nowers M, Gunnell D. Effect of barriers on the Clifton suspension bridge, England, on local patterns of suicide: implications for prevention. Br J Psychiatry. 2007;190:266–7. doi: 10.1192/bjp.bp.106.027136. [DOI] [PubMed] [Google Scholar]
- 45.Audas R, McDonald T. Rural-urban migration in the 1990s. Ottawa: Statistics Canada; 2004. [Google Scholar]
- 46.Bollman RD, Marshall J, Rothwell N, Tremblay J. Recent migration patterns in rural and small town Canada. Ottawa (Ontario): Statistics Canada; 2002. [Google Scholar]


