Abstract
Objective
While limited access to care is associated with adverse health conditions, little research has investigated the association between barriers to care and having multiple health conditions (comorbidities). We compared the financial, structural, and cognitive barriers to care between Mexican-American border residents with and without comorbidities.
Methods
We conducted a stratified, two-stage, randomized, cross-sectional health survey in 2009–2010 among 1,002 Mexican-American households. Measures included demographic characteristics; financial, structural, and cognitive barriers to health care; and prevalence of health conditions.
Results
Comorbidities, most frequently cardiovascular and metabolic conditions, were reported by 37.7% of participants. Controlling for demographics, income, and health insurance, six financial barriers, including direct measures of inability to pay for medical costs, were associated with having comorbidities (odds ratios [ORs] ranged from 1.7 to 4.1, p<0.05). The structural barrier of transportation (OR=3.65, 95% confidence interval [CI] 1.91, 6.97, p<0.001) was also associated with higher odds of comorbidities, as were cognitive barriers of difficulty understanding medical information (OR=1.71, 95% CI 1.10, 2.66, p=0.017), being confused about arrangements (OR=1.82, 95% CI 1.04, 3.21, p=0.037), and not being treated with respect in medical settings (OR=1.63, 95% CI 1.05, 2.53, p=0.028). When restricting analyses to participants with at least one health condition (comparing one condition vs. having ≥2 comorbid conditions), associations were maintained for financial and transportation barriers but not for cognitive barriers.
Conclusion
A substantial proportion of adults reported comorbidities. Given the greater burden of barriers to medical care among people with comorbidities, interventions addressing these barriers present an important avenue for research and practice among Mexican-American border residents.
Limited access to health care has been associated with a wide range of adverse health consequences including premature mortality1,2 and increased risk for many common chronic conditions.3–5 Despite prior research documenting associations between sustained lack of access and many health conditions independently,6,7 very little research has described whether people with more than one health condition (i.e., comorbidities) experience greater barriers to obtaining health care.
Prior research based on information from the Medical Expenditure Panel Survey has further indicated that people with multiple chronic conditions incur far greater health-care costs (up to seven times as many) as patients with only one chronic condition.8 It is essential, therefore, to understand the barriers to care that are disproportionately faced by people with comorbidities who need ongoing care, particularly among populations at high risk for developing comorbidities.
Populations at high risk for having multiple health conditions include most minority populations in the U.S. and, in particular, Hispanic people, the largest and most rapidly growing minority group in the U.S.9 For example, the largest subgroup of Hispanic people, Mexican-Americans, has been found to have the highest incidence (an estimated 33.2%) of metabolic syndrome,10 a cluster of risk factors placing people at higher risk for heart disease, type 2 diabetes, and stroke.11 Although there is substantial variability among Hispanic subgroups, based on information from the National Health Interview Survey, Mexican-American populations have the poorest access to care and the lowest use of health services of all Hispanic subgroups.12,13 An estimated 32% of Hispanic people in the U.S. do not have health insurance compared with 15% of non-Hispanic white people.14 Besides economic limitations, Hispanic populations often face additional barriers to accessing health services. Factors that have been reported to impede Hispanic populations from obtaining medical care include, but are not limited to, language and literacy barriers,15–17 lack of transportation and geographic inaccessibility,15,17 the perception of being treated without respect in medical settings, and the perception that they would have received better quality care if they belonged to a difference racial/ethnic group.18
A valuable guiding framework for the current study that provides a comprehensive overview of modifiable factors associated with access to health care is the recently developed Health Care Access Barriers model, an evidence-based analytical framework developed by Carillo and colleagues.19 This model describes the assessment of three categories of barriers to health care (financial, structural, and cognitive) that have been shown to be associated with poor health outcomes.
Given the limited access to health care and high risk for comorbidities, gaining insight into which financial, structural, and cognitive barriers to care are associated with comorbidities among Mexican-Americans can provide valuable information for preventive efforts. Therefore, based on information from a randomized household survey conducted in a large city along the U.S.-Mexico border, the primary aim of the current study was to compare barriers to health care of participants with and without comorbidities. We hypothesized that people reporting comorbidities would be disproportionately affected by financial, cognitive, and structural barriers to care.
METHODS
Study setting
We conducted the study in El Paso, Texas, which is situated at the U.S.-Mexico border. In El Paso, approximately 80% of residents are Hispanic, with the overwhelming majority being of Mexican descent. The per capita income in 2008 was approximately $29,000, which is substantially below the state average. El Paso has one of the highest rates of uninsured residents of any major city in the United States, with one-third of the population lacking health insurance.20
Design and participants
A household survey was conducted from November 2009 to May 2010. Households were selected through a stratified two-stage probability sample based on geography and stratified by population density. Fifty strata were constructed from the city of El Paso using electronic Census tract data. Adjacent Census tracts were combined to reach approximately 13,000 residents per stratum. Twenty households were recruited from each stratum, resulting in a total of 1,002 households. We interviewed one randomly selected adult respondent in each household and used the sampling approach, which is described in detail elsewhere,21 to ensure population heterogeneity in terms of access, coverage, and health status.
Measures and instruments
Demographic information.
Demographic characteristics included each participant's age, sex, birthplace and number of years lived in the U.S., approximate annual household income, and health insurance status. Response options for household income included <$5,000, $5,000–$9,999, $10,000–$19,999, and $20,000–$30,000, increasing by increments of $10,000 until >$70,000. Income was then recoded into households with an annual income above or below $20,000. Health insurance status was dichotomized into those who were continuously insured during the past year and those who were not continuously insured during the past year. We assessed education by determining the highest level of education completed and dichotomized the results into those participants who completed high school vs. those who did not.
Health conditions and comorbidities.
The primary outcome variable included asking the participants, “Have you ever been told by a health-care provider (such as a doctor or a nurse) that you have or have had any of the following health problems? (Mark all that apply.)” The list of conditions included diabetes, high blood pressure, high cholesterol, heart attack or stroke, asthma, emphysema, hepatitis or cirrhosis, kidney disease, ulcer, colitis or chronic bowel disease, cancer, arthritis, tuberculosis, human immunodeficiency virus/acquired immunodeficiency syndrome, abuse/addiction, alcoholism, depression, anxiety, or other.
Access and barrier variables.
Access and barriers to health care were adapted from prior items developed by Heyman et al.22 We asked a series of questions to assess whether study participants had a provider or place they went for health care and if they had used health-care services in the past three years. Specifically, one yes/no question inquired if respondents had a health-care provider: “In general, when you become ill/want advice about your health, is there a person/place where you go most of the time?”
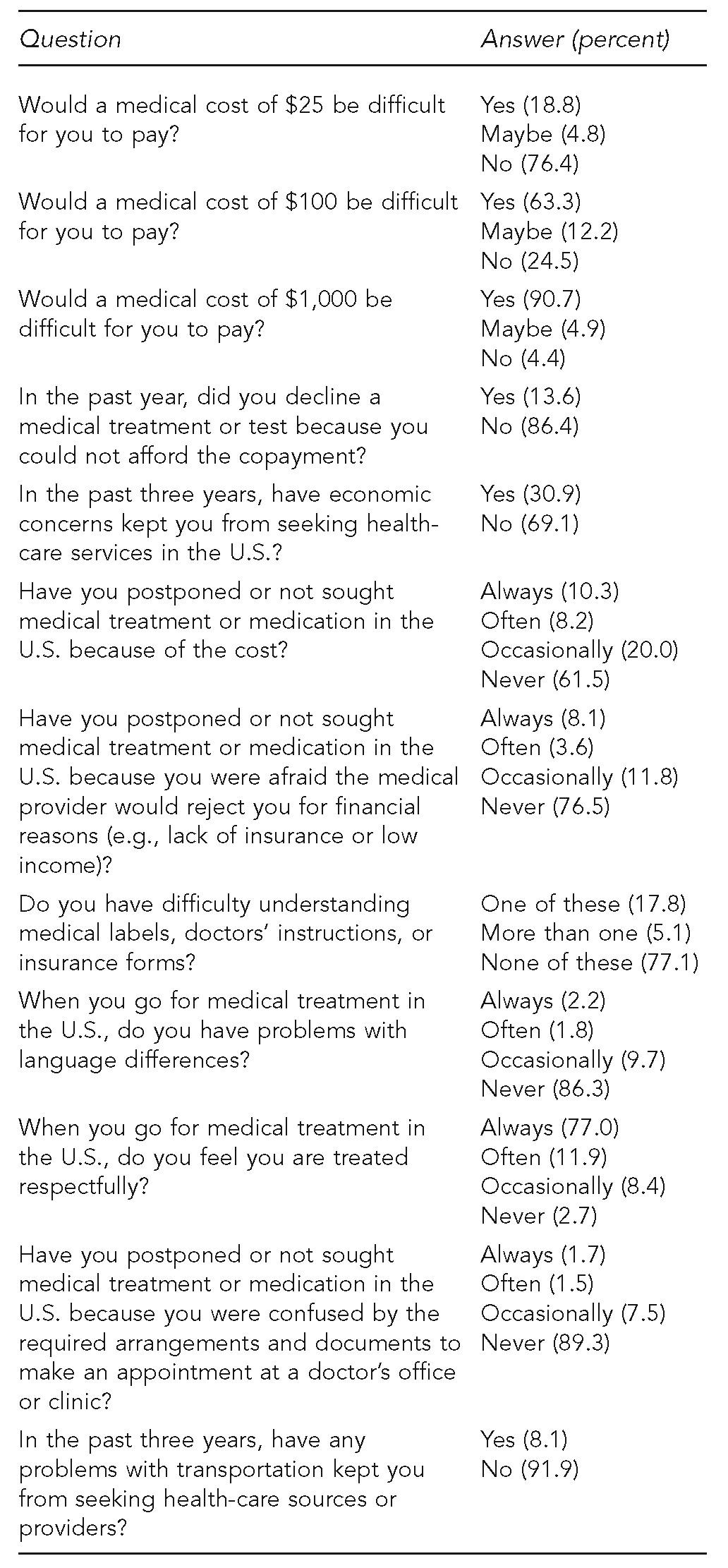
We assessed financial, cognitive, and structural barriers through 12 questions (Table 1). We assessed financial barriers to seeking care by asking seven questions. Cognitive barriers included four questions about not using health care or not receiving optimal health care as a result of barriers in language, barriers related to not being treated respectfully in health-care settings, and barriers related to a limited understanding about issues related to health care. Finally, we assessed the structural barrier of transportation by asking, “In the past three years, have any problems with transportation kept you from seeking health-care sources or providers?”
Table 1.
Household survey questions and responses regarding financial, cognitive, and structural barriers to care in a randomized household survey of Hispanic residents of El Paso, Texas: 2009–2010
Analyses
We used descriptive statistics (e.g., frequencies, means, and standard deviations [SDs]) to describe participant characteristics. We used independent sample t-tests to assess baseline differences between people with and without comorbidities. To assess the primary study question of whether different barriers to health-care variables were associated with having at least two health conditions (comorbidities), we conducted a series of logistic regression analyses. All logistic regressions included (1) demographic indicators such as age, sex, birthplace and years lived in the U.S., education, income, health insurance status, and whether the participant had a regular place to go for health care; and (2) one of the financial, structural, or cognitive barriers. Demographic indicators were included in all models regardless of whether they were significantly associated with the outcome variable. All analyses were conducted using SPSS® version 17.0.23
RESULTS
Self-reported comorbidities
In all, 37.1% of participants reported none of the health conditions listed and no other health condition, 25.2% of participants reported one condition, and 37.7% of participants reported two or more health conditions (comorbidities). The average number of health conditions reported was 1.5 (SD=1.7, range: 0–9). The conditions with the highest prevalence (i.e., >3% of participants) were high blood pressure (26.1%), high cholesterol (21.5%), diabetes (15.4%), arthritis (13.1%), depression (12.3%), anxiety (9.4%), asthma (8.1%), cancer (4.4%), colitis/chronic bowel disease (4.0%), ulcers (4.0%), and heart attack or stroke (3.9%). The most frequent comorbidities were hypertension and high cholesterol (12.9% of participants), hypertension and diabetes (9.7%), diabetes and high cholesterol (7.3%), and hypertension and arthritis (7.3%) (data not shown).
Demographics and barriers to health care of participants without comorbidities
As shown in Table 2, people without comorbidities were, on average, 39.5 years of age (SD=14.7) and most (62.3%) were female. On average, they have lived in the U.S. for 29.8 years or approximately three-quarters of their life. About 41.3% had an annual household income of <$20,000, 58.7% had no health insurance continuously for the past year, and more than one-third (35.3%) did not have a person or place to go for medical care. A total of 5.8% of participants reported never having had a medical checkup (data not shown).
Table 2.
Comparison of demographic variables and barriers to health care of Hispanic participants with and without comorbidities in a randomized household survey in El Paso, Texas: 2009–2010
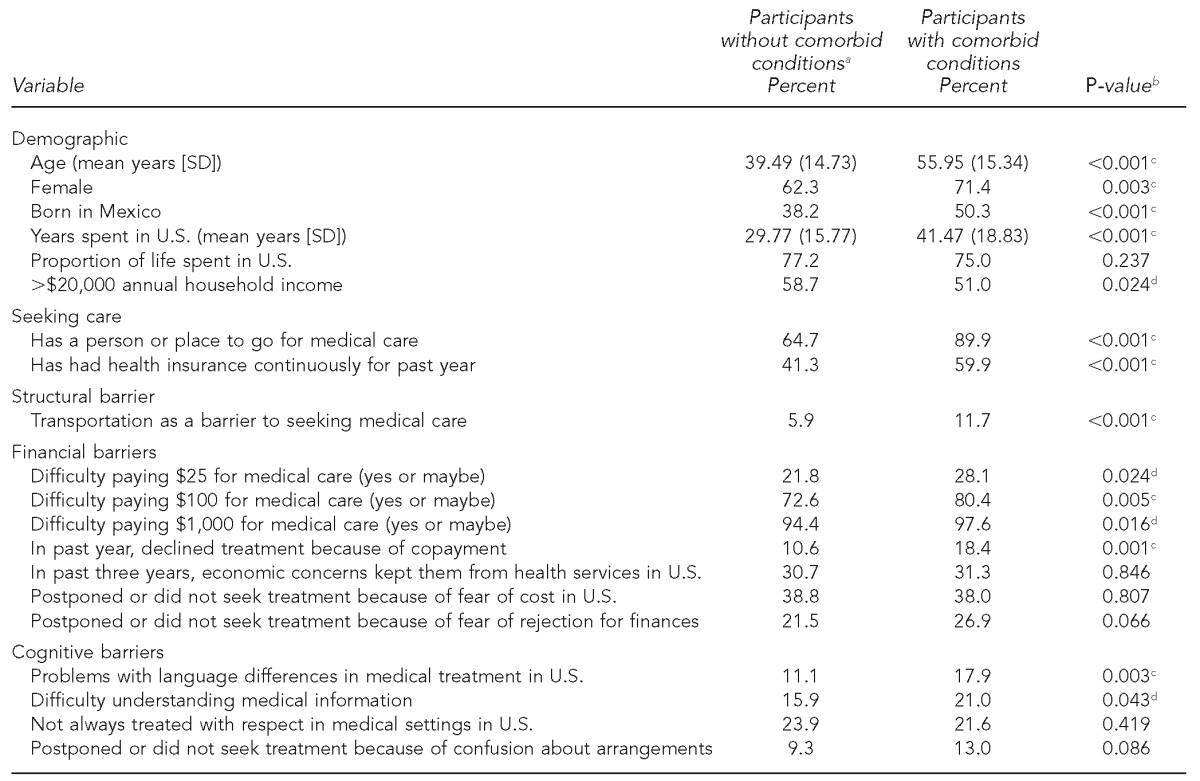
aComorbidities were defined as having at least two conditions of a list of 18 conditions and any other reported condition.
bP-value based on independent sample t-tests or Chi-square tests
cSignificant at p<0.01
dSignificant at p<0.05
Financial barriers to obtaining health care were the most commonly reported barriers for those without comorbidities. For example, 72.6% of participants reported that paying $100 for medical care would be difficult. Transportation barriers were mentioned least frequently among people without comorbidities (5.9%). Cognitive barriers were more common, ranging from 9.3% (confusion about the arrangements in medical settings) to 23.9% (not always treated with respect) (Table 2).
Demographics and barriers to care of participants with comorbidities
People with comorbidities (Table 2) were on average 56.0 years of age (SD=15.3), 71.4% were female, and about half (50.3%) were born in Mexico. Almost half (49.0%) had an annual income of <$20,000, but 59.9% reported having health insurance continuously for the past year, and 89.9% had a person or place to go for medical care.
In general, barriers to health care were reported more frequently among people with comorbidities than among people without comorbidities. Financial barriers were very common; for example, 80.4% of participants with comorbidities reported that it would be difficult for them to pay $100 for medical care. Transportation was a barrier for 11.7% of participants, whereas each of the cognitive barriers was reported by a range of 13.0%–21.6% of participants with comorbidities.
Comparing barriers to health care of participants with and without comorbidities
To assess whether barrier-to-care variables were significantly different among those with and without comorbidities, we conducted a series of multivariate logistic regression models. Demographic variables were included in all models and consisted of age, gender, birthplace, years lived in the U.S., education level, and income. In addition, access-to-care variables, including having health insurance and having a person or place to go for medical care, were included in every model. Secondly, each barrier (financial, cognitive, and structural) was entered separately to assess the unique impact of that particular barrier.
In the multivariate models (Table 3), people who reported comorbidities were older (OR=1.05, 95% CI 1.03, 1.07, p<0.001), more likely to be female (OR=1.54, 95% CI 1.07, 2.22, p=0.020), have at least a high school education (OR=1.60, 95% CI 1.05, 2.43, p=0.029), and have a person or place to go for medical care (OR=2.99, 95% CI 1.88, 4.74, p<0.001).
Table 3.
Logistic regression modelsa associating barriers to care with having comorbidities among Hispanic participants in a randomized household survey conducted in El Paso, Texas: 2009–2010
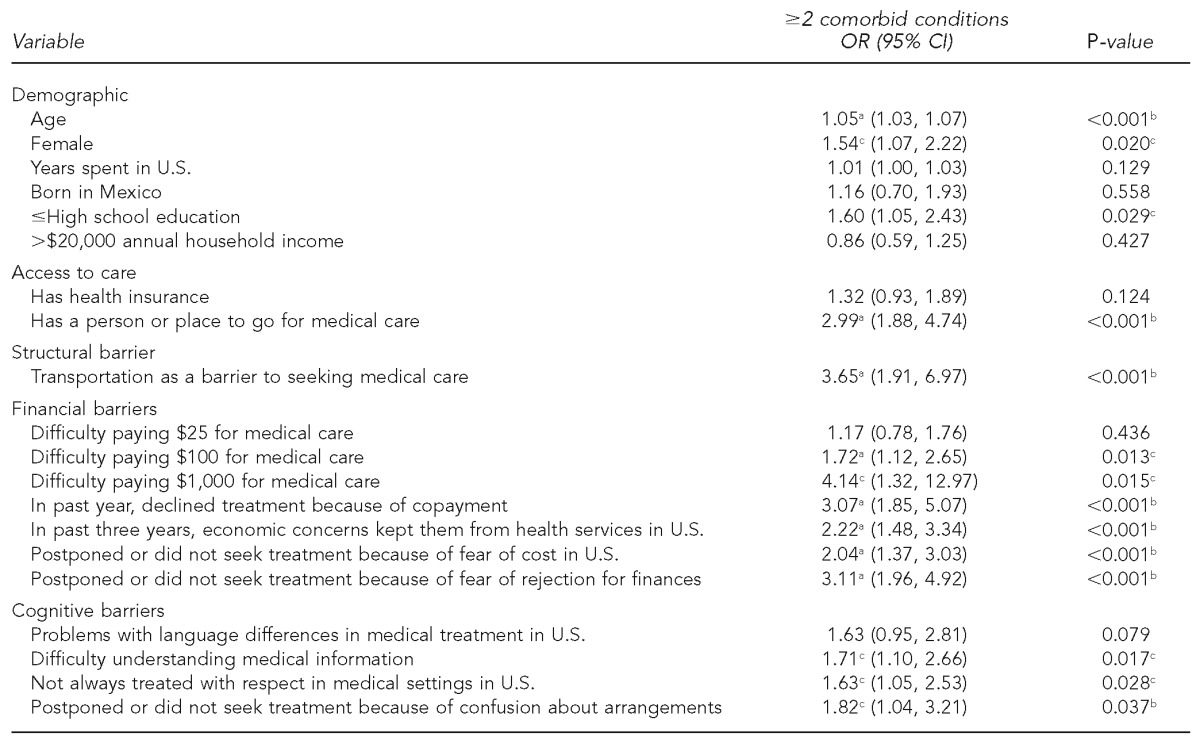
aAnalyses included logistic regression with each model including all demographic and access-to-care variables and one of the barriers.
bSignificant at p<0.01
cSignificant at p<0.05
OR = odds ratio
CI = confidence interval
People with comorbidities were more likely to report financial barriers across the board, with the exception of difficulty paying $25 out-of-pocket for medical expenses. Having comorbidities was associated with difficulty paying direct medical expenses including out-of-pocket medical expenses of $100 (OR=1.72, 95% CI 1.12, 2.65, p=0.013) and $1,000 (OR=4.14, 95% CI 1.32, 12.97, p=0.015), declining treatment in the past year because of the inability to afford a copayment (OR=3.07, 95% CI 1.85, 5.07, p<0.001), not seeking health-care services in the past three years in the U.S. because of economic concerns (OR=2.22, 95% CI 1.48, 3.34, p<0.001), or postponing and not seeking treatment because of fear of cost (OR=2.04, 95% CI 1.37, 3.03, p<0.001). Finally, postponing or not seeking medical treatment because of fear of rejection by the health-care provider for financial reasons was strongly associated with reporting comorbidities (OR=3.11, 95% CI 1.96, 4.92, p<0.001) (Table 3).
The structural barrier of transportation related to seeking medical care was strongly associated with having comorbidities (OR=3.65, 95% CI 1.91, 6.97, p<0.001). Three of the four cognitive barriers were also significantly associated with reporting comorbidities. Specifically, difficulty understanding medical information (OR=1.71, 95% CI 1.10, 2.66, p=0.017), the perception of not always being treated with respect in medical settings (OR=1.63, 95% CI 1.05, 2.53, p=0.028), and having postponed or not seeking treatment because of confusion about medical arrangements (OR=1.82, 95% CI 1.04, 3.21, p=0.037) were associated with reporting comorbidities. Having a language barrier in medical settings (OR=1.63, 95% CI 0.95, 2.81, p=0.079) was not significantly associated with comorbidities.
Subgroup analyses.
It could be assumed that participants who report no diagnosed health condition may have little reason to seek health care in the first place; therefore, they would be less likely to report barriers. When analyses compared participants with comorbidities only with people who had one chronic health condition, the financial and transportation barriers were still significantly associated with comorbidities (with similar ORs). Findings for the cognitive barriers were somewhat diminished in these new analyses. Only one cognitive barrier (having postponed or not seeking treatment because of confusion about arrangements in medical settings) was marginally associated with comorbidities (OR=1.90, 95% CI 0.95, 3.77, p=0.069), with an OR that was actually slightly higher than in the original analysis. The ORs for the other two previously significant variables were lower (the OR for not always being treated with respect in medical settings was 1.6, while in the new analysis it was 1.5 [95% CI 0.89, 2.46, p=0.134], and the OR for difficulty understanding medical information was 1.7, while in the new analysis it was 1.2 [95% CI 0.75, 2.03, p=0.407]) (data not shown).
DISCUSSION
We assessed which barriers to health-care services were associated with having comorbidities among Mexican-American adults living in a large metropolitan area along the U.S.-Mexico border. Notably, we found that barriers to care in all three categories (financial, structural, and cognitive) of the Health Care Access Barriers model19 were associated with comorbidities. In our health-care system, someone with multiple health conditions incurs far greater health-care costs than someone with a single chronic condition,24 and more than one-third of participants reported multiple health conditions. By far the most commonly reported comorbidities were diabetes, hypertension, and high cholesterol, all of which are risk factors for cardiovascular disease. Economic barriers were consistently associated with increased odds of reporting comorbidities, as were transportation barriers related to seeking medical care. Cognitive barriers, including difficulty understanding medical information or doctors' instructions, confusion about medical information, and the perception of not always being treated with respect, were all associated with comorbidities, although these associations were not significant when analyses excluded participants without any health conditions.
Financial and structural barriers
Most participants reported economic barriers to care, such as having difficulty paying out-of-pocket medical expenses, illustrating the limited capacity to access health care if direct expenses are required. People with comorbidities appeared to experience greater financial barriers. This finding is reason for concern, as research has provided evidence that out-of-pocket health-care spending increased 45% from 1996 to 2005, with the fastest growth among those with multiple chronic conditions.25 Furthermore, more recent evidence has indicated that out-of-pocket costs have accelerated in the last few years.26 If these trends continue, access to health care will become increasingly limited for people with comorbidities in underserved populations. Further, prior research (i.e., the Translating Research into Action for Diabetes study) has indicated that greater personal contribution for health care is associated with lower use of preventive services and poor clinical monitoring of disease, leading to poorer clinical outcomes, additional health complications, and potentially greater health-care costs in the long term.27
Transportation barriers to medical care were strongly associated with comorbidities. Prior studies have suggested that as many as 3.6 million Americans do not receive medical care every year due to limited access to non-emergency medical transportation. These barriers were found to be more common among older people, women, minority groups, the poor, and the less educated.28 It was further found that these 3.6 million Americans experience multiple conditions at a much higher rate than people who did not experience transportation barriers,28 which is consistent with the findings of the current study. In particular, foreign-born Mexican-American women have been reported to be much less likely to drive than non-Hispanic white women and, therefore, rely on family for transportation.29 Indeed, of the foreign-born women with comorbidities in the study, more than one in six reported transportation barriers compared with one in 16 Mexican-American U.S.-born women without comorbidities (data not shown).
Cognitive barriers
Participants with comorbidities may experience greater confusion and difficulty understanding medical information than all other participants (including those without any health conditions). However, when we restricted the analyses to compare participants who had comorbidities with people who had only one health condition, these findings were much more limited. Regardless of the significance of these differences, it is notable that among participants with comorbidities, almost half (45.2%) reported at least one cognitive barrier to receiving medical care. A total of 18.4% of participants with comorbidities reported two or more cognitive barriers, including barriers associated with literacy, language, and being treated with respect in medical settings. This finding is reason for concern, certainly in the context of prior research that has indicated an association between inadequate health literacy and a lower use of medical care and preventive services, as well as 1.5- to threefold increased odds for poor health outcomes.30 Recent research has provided further evidence that limited health literacy is associated with 3%–5% increased health-care costs, although individual-level estimates vary from an increased cost of $143 to as high as $7,798 annually per person.31 Finally, the perception of not being treated with dignity in medical settings has been associated with poor satisfaction, adherence, and preventive care.32
Limitations
This study was subject to several limitations. First, the study was cross-sectional and could only describe associations between barriers to health care and reported health outcomes. Financial limitations, for example, can either precede development of comorbidities or be a consequence of the health problems. It is further possible that barriers and comorbidities stem from a common set of causal factors not addressed in the current study, such as social or environmental circumstances. Second, the study was conducted in a large metropolitan border area among mostly Mexican-American women, and the findings may not be generalizable to Hispanic populations in other areas in the U.S. Finally, health conditions were self-reported, not clinically confirmed, and the proportion of disease estimates may underestimate actual disease prevalence due to the number of people with limited access to a health-care provider who may diagnose a disease.
CONCLUSIONS
Given the high proportion of participants with cardiovascular comorbidities in the current study and the reported barriers associated with these comorbidities, outreach approaches for Hispanic populations living within and outside the U.S. border region are warranted. These outreach approaches should use methods tailored to the needs of local immigrant populations who have higher rates of cardiovascular comorbidities.33,34 Given the low number of available health-care professionals in the El Paso area35 and other regions of the country, one way to address these barriers in the future is to increasingly use community resources.36 Recently, programs aimed at reducing the risk for cardiovascular and metabolic risk factors by using community health workers (promotoras) have been developed and evaluated in U.S.-Mexico border settings.37–39
In a medical context in which people with multiple chronic health conditions incur far greater health-care costs compared with people with a single chronic condition,8,24 addressing what may appear to be minor barriers to obtaining health care (e.g., being unable to afford copayments, find transportation to medical care, or understand medical information) could impact the risk for comorbidities or improve their treatment.
Intervention studies to address chronic conditions among Mexican-American border residents require the consideration of the greater burden of barriers to medical care prevalent among vulnerable border region populations. When implementing culturally relevant interventions by using community outreach strategies, it is imperative to consider the high proportion of Mexican-American border residents who have high rates of cardiovascular comorbidities.
Footnotes
This project was funded by the National Institutes of Health National Center on Minority Health and Health Disparities #1P20 MD002287-01. This study was approved by the Institutional Review Boards of the University of Texas at El Paso and the University of Texas Health Science Center–Houston, School of Public Health. The findings and conclusions in this article are those of the authors and do not represent the views of the finding agency.
REFERENCES
- 1.Institute of Medicine, Committee on Monitoring Access to Personal Health Care Services. Access to health care in America. Washington: National Academies Press; 1993. [Google Scholar]
- 2.Baker DW, Shapiro MF, Schur CL. Health insurance and access to care for symptomatic conditions. Arch Intern Med. 2000;160:1269–74. doi: 10.1001/archinte.160.9.1269. [DOI] [PubMed] [Google Scholar]
- 3.Wilper AP, Woolhandler S, Lasser KE, McCormick D, Bor DH, Himmelstein DU. Health insurance and mortality in US adults. Am J Public Health. 2009;99:2289–95. doi: 10.2105/AJPH.2008.157685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wilper AP, Woolhandler S, Lasser KE, McCormick D, Bor DH, Himmelstein DU. A national study of chronic disease prevalence and access to care in uninsured U.S. adults. Ann Intern Med. 2008;149:170–6. doi: 10.7326/0003-4819-149-3-200808050-00006. [DOI] [PubMed] [Google Scholar]
- 5.McWilliams JM. Health consequences of uninsurance among adults in the United States: recent evidence and implications. Milbank Q. 2009;87:443–94. doi: 10.1111/j.1468-0009.2009.00564.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ayanian JZ, Weissman MS, Schneider EC, Ginsburg JA, Zaslavsky AM. Unmet health needs of uninsured adults in the United States. JAMA. 2000;284:2061–9. doi: 10.1001/jama.284.16.2061. [DOI] [PubMed] [Google Scholar]
- 7.Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA. 2002;287:356–9. doi: 10.1001/jama.287.3.356. [DOI] [PubMed] [Google Scholar]
- 8.Stanton MW, Rutherford MK. The high concentration of U.S. health care expenditures. Rockville (MD): Agency for Healthcare Research and Quality (US); 2006. Research in Action Issue 19. AHRQ Pub. No. 06-0060. [Google Scholar]
- 9.Ennis SR, Rios-Vargas M, Albert NG. The Hispanic population: 2010. Washington: Census Bureau (US); 2011. Also available from: URL: http://www.census.gov/prod/cen2010/briefs/c2010br-04.pdf [cited 2013 Jun 12] [Google Scholar]
- 10.Mozumdar A, Liguori G. Persistent increase of prevalence of metabolic syndrome among U.S. adults: NHANES III to NHANES 1999–2006. Diabetes Care. 2011;34:216–9. doi: 10.2337/dc10-0879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wannamethee SG, Shaper AG, Lennon L, Morris RW. Metabolic syndrome vs Framingham Risk Score for prediction of coronary heart disease, stroke, and type 2 diabetes mellitus. Arch Intern Med. 2005;165:2644–50. doi: 10.1001/archinte.165.22.2644. [DOI] [PubMed] [Google Scholar]
- 12.Vargas Bustamante A, Fang H, Rizzo JA, Ortega AN. Understanding observed and unobserved health care access and utilization disparities among U.S. Latino adults. Med Care Res Rev. 2009;66:561–7. doi: 10.1177/1077558709338487. [DOI] [PubMed] [Google Scholar]
- 13.Perez VH, Fang H, Inkelas M, Kuo AA, Ortega AN. Access to and utilization of health care by subgroups of Latino children. Med Care. 2009;47:695–9. doi: 10.1097/MLR.0b013e318190d9e4. [DOI] [PubMed] [Google Scholar]
- 14.Livingston G, Minushkin S, Cohn D. Hispanics and health care in the United States: access, information and knowledge. Washington: Pew Hispanic Center; 2008. Also available from: URL: http://pewhispanic.org/files/reports/91.pdf [cited 2013 Jun 12] [Google Scholar]
- 15.Estrada AL, Trevino FM, Ray LA. Health care utilization barriers among Mexican Americans: evidence from HHANES 1982–84. Am J Public Health. 1990;80(Suppl):27–31. doi: 10.2105/ajph.80.suppl.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Timmins CL. The impact of language barriers on the health care of Latinos in the United States: a review of the literature and guidelines for practice. J Midwifery Womens Health. 2002;47:80–96. doi: 10.1016/s1526-9523(02)00218-0. [DOI] [PubMed] [Google Scholar]
- 17.DuBard CA, Gizlice Z. Language spoken and differences in health status, access to care, and receipt of preventive services among US Hispanics. Am J Public Health. 2008;98:2021–8. doi: 10.2105/AJPH.2007.119008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Johnson RL, Saha S, Arbelaez JJ, Beach MC, Cooper LA. Racial and ethnic differences in patient perceptions of bias and cultural competence in health care. J Gen Intern Med. 2004;19:101–10. doi: 10.1111/j.1525-1497.2004.30262.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Carillo JE, Carillo VA, Perez HR, Salas-Lopez D, Natale-Peirera A, Byron AT. Defining and targeting health care access barriers. J Health Care Poor Underserved. 2011;22:562–75. doi: 10.1353/hpu.2011.0037. [DOI] [PubMed] [Google Scholar]
- 20.Texas Department of State Health Services. Health currents system [cited 2013 Jun 12] Available from: URL: http://www.dshs.state.tx.us/chs/healthcurrents.
- 21.Lapeyrouse LM, Morera OF, Heyman JM, Amaya MA, Pingitore NE, Balcázar H. A profile of US-Mexico border mobility among a stratified random sample of Hispanics living in the El Paso-Juarez area. J Immigr Minor Health. 2012;14:264–71. doi: 10.1007/s10903-011-9453-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Heyman JM, Núñez GG, Talavera V. Health care access and barriers for unauthorized immigrants in El Paso County, Texas. Fam Community Health. 2009;32:4–21. doi: 10.1097/01.FCH.0000342813.42025.a3. [DOI] [PubMed] [Google Scholar]
- 23.SPSS Inc. SPSS®: Version 17.0 for Windows. Chicago: SPSS Inc.; 2008. [Google Scholar]
- 24.Boudreau DM, Malone DC, Raebel MA, Fishman PA, Nichols GA, Feldstein AC, et al. Health care utilization and costs by metabolic syndrome risk factors. Metab Syndr Relat Disord. 2009;7:305–14. doi: 10.1089/met.2008.0070. [DOI] [PubMed] [Google Scholar]
- 25.Paez KA, Zhao L, Hwang W. Rising out-of-pocket spending for chronic conditions: a ten-year trend. Health Aff (Millwood) 2009;28:15–25. doi: 10.1377/hlthaff.28.1.15. [DOI] [PubMed] [Google Scholar]
- 26.Hartman M, Martin AB, Benson J, Catlin A. National health spending in 2011: overall growth remains low, but some payers and services show signs of acceleration. Health Aff (Millwood) 2013;32:87–99. doi: 10.1377/hlthaff.2012.1206. [DOI] [PubMed] [Google Scholar]
- 27.Karter AJ, Stevens MR, Herman WH, Ettner S, Marrero DG, Safford MM, et al. Out-of-pocket costs and diabetes preventive services: the Translating Research into Action for Diabetes (TRIAD) study. Diabetes Care. 2003;26:2294–9. doi: 10.2337/diacare.26.8.2294. [DOI] [PubMed] [Google Scholar]
- 28.Wallace R, Hughes-Cromwick P, Mull H, Khasnabis S. Access to health care and nonemergency medical transportation: two missing links. Transport Res Rec. 2005;1924:76–84. [Google Scholar]
- 29.Angel JL, Angel RJ, McClellan JL, Markides KS. Nativity, declining health, and preferences in living arrangements among elderly Mexican Americans: implications for long-term care. Gerontologist. 1996;36:464–73. doi: 10.1093/geront/36.4.464. [DOI] [PubMed] [Google Scholar]
- 30.DeWalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and health outcomes: a systematic review of the literature. J Gen Intern Med. 2004;19:1228–39. doi: 10.1111/j.1525-1497.2004.40153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Eichler K, Wieser S, Brugger U. The costs of limited health literacy: a systematic review. Int J Public Health. 2009;54:313–24. doi: 10.1007/s00038-009-0058-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Beach MC, Sugarman J, Johnson RL, Arbelaez JJ, Duggan PS, Cooper LA. Do patients treated with dignity report higher satisfaction, adherence, and receipt of preventive care? Ann Fam Med. 2005;3:331–8. doi: 10.1370/afm.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Balcázar H, Wise S, Rosenthal EL, Ochoa C, Rodriguez J, Hastings D, et al. An ecological model using promotores de salud to prevent cardiovascular disease on the US-Mexico border: the HEART project. Prev Chronic Dis. 2012;9:110100. doi: 10.5888/pcd9.110100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Balcázar H, Alvarado M, Ortiz G. Salud Para Su Corazon (Health for Your Heart) community health worker model: community and clinical approaches for addressing cardiovascular disease risk reduction in Hispanics/Latinos. J Ambul Care Manag. 2011;34:362–72. doi: 10.1097/JAC.0b013e31822cbd0b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Texas Department of State Health Services, Health Professions Resource Center. Supply trends among licensed health professions: Texas, 1980–2011. 5th ed. Austin: Texas Department of State Health Services; 2012. [Google Scholar]
- 36.Nelson A. Unequal treatment: confronting racial and ethnic disparities in health care. J Natl Med Assoc. 2002;94:666–8. [PMC free article] [PubMed] [Google Scholar]
- 37.Balcázar H, Alvarado M, Hollen ML, Gonzalez-Cruz Y, Pedregon V. Evaluation of Salud Para Su Corazon (Health for your Heart)—National Council of La Raza Promotora Outreach Program. Prev Chronic Dis. 2005;2:A09. [PMC free article] [PubMed] [Google Scholar]
- 38.Balcázar H, Alvarado M, Cantu F, Pedregon V, Fulwood R. A promotora de salud model for addressing cardiovascular disease risk factors in the US-Mexico border region. Prev Chronic Dis. 2009;6:A02. [PMC free article] [PubMed] [Google Scholar]
- 39.Balcázar HG, de Heer H, Rosenthal L, Aguirre M, Flores L, Puentes FA, et al. A promotores de salud intervention to reduce cardiovascular disease risk in a high-risk Hispanic border population, 2005–2008. Prev Chronic Dis. 2010;7:A28. [PMC free article] [PubMed] [Google Scholar]


