Abstract
Objective
Vibrio is a naturally occurring waterborne pathogen with potential occupational, recreational, and commercial impacts. During the last 15 years in the U.S. and in Maryland, the incidence of vibriosis has increased. Due to the increase in cases in Maryland, warming water temperatures, and public concern about human health effects resulting from exposure to the Chesapeake Bay, we reviewed cases of vibriosis and evaluated the Vibrio surveillance system in Maryland for timeliness and data quality, attributes necessary for successful outbreak investigation and illness prevention.
Methods
The evaluation included (1) informal qualitative surveys of state and local personnel who report and manage Vibrio cases and (2) a review of Vibrio surveillance data from 2002 through 2008 for data quality and timeliness of the system.
Results
From 2002 to 2008, 188 laboratory-confirmed cases of vibriosis were reported in Maryland with an annual average of 27 cases. The species of Vibrio that were most frequently responsible for infection, regardless of clinical presentation, were V. parahaemolyticus (43.6%), V. vulnificus (23.9%), V. alginolyticus (9.6%), and non-toxigenic V. cholerae (9.0%). The case fatality rate fluctuated during the study period, but the number of cases increased.
Conclusions
The surveillance system in Maryland is flexible and captures cases of vibriosis where specimens were collected for testing; however, the system may not adequately capture mild, self-limiting infections. Better integration of data collection for clinical, laboratory, and environmental information and improved completion of variables for shellfish harvest or water exposure locations could improve the system. Quarterly meetings comprising surveillance, public health laboratory, and food-control personnel could direct and ensure the success of improvement efforts.
Maryland surrounds the Chesapeake Bay, the largest estuary in the United States, and is renowned for its blue crabs, oysters, and recreational opportunities. Unfortunately, Vibrio infections, which are generally acquired through recreational exposure to brackish water or consumption of shellfish, have occasionally sullied the state's reputation. The gram-negative, rod-shaped bacteria that cause these potentially severe infections are natural inhabitants of the Chesapeake Bay and other brackish coastal waters. As water temperatures rise seasonally, Vibrio species (spp.) accumulate in brackish water and within and on the surface of oysters, clams, crabs, and other shellfish, and the number of vibriosis cases associated with seafood consumption or water exposure rises.1,2 Oyster harvesting from natural harvest areas in Maryland is prohibited from March 30 to October 1 to allow for resource management. This restriction incidentally prevents oysters from being harvested when water temperatures and Vibrio concentrations are highest. Oyster harvesting from Maryland aquaculture facilities, where oysters are grown in surface waters instead of at the Bay bottom, is not similarly restricted. Surface temperatures are higher than at the Bay bottom and promote Vibrio congregation; thus, summer aquaculture harvests may result in infection.
Infection ranges from asymptomatic to severe and is characterized by persistent wounds, abdominal pain, diarrhea, and vomiting. Primary septicemia, septic shock, and blistering skin lesions may occur in severe cases.3,4 Consumption of raw or undercooked shellfish and cross-contamination during food preparation are sources of gastrointestinal vibriosis. Wound infections arise from exposure of skin lesions to, or injuries that occur in, marine or brackish waters. Liver disease, alcoholism, diabetes, cancer, hemochromatosis, and immunosuppression increase the risk for severe and systemic disease.5
During the last 15 years, the incidence of vibriosis has increased in the U.S. and in Maryland.6,7 Warming of coastal waters, which contributes to the growth and persistence of Vibrio, has been posited as a factor that contributes to increased incidence.6 The increase of vibriosis in Maryland, warming water temperatures, and public concern about human health effects associated with the Chesapeake Bay8 led to an evaluation of Maryland's Vibrio surveillance system. The assessment focused on a review of vibriosis cases and examination of timeliness and data quality, as outbreak control and prevention requires timely identification of the infection source.
MARYLAND'S VIBRIO SURVEILLANCE SYSTEM
Maryland law and regulations9,10 and Code of Maryland Regulations11 require health-care providers to report diagnoses of vibriosis to health departments and laboratories to submit clinical specimens to the Maryland Department of Health and Mental Hygiene (DHMH) Public Health Laboratory (PHL) for confirmatory testing. Results are reported to the submitter via the Laboratory Information Management System (hereafter, StarLIMS). DHMH and local health department (LHD) surveillance investigate and classify reports according to the Council of State and Territorial Epidemiologists' (CSTE's) case definitions for Vibrio cholerae (V. cholerae) and non-cholera vibriosis.4,12
The “Guidelines for the Epidemiological Investigation of Cholera and Other Vibrio Species Infections” provide the framework for Vibrio surveillance in Maryland.13 DHMH uses two surveillance systems to monitor vibriosis: the passive national Cholera and Other Vibrio Illness Surveillance System (COVIS)14 and the Foodborne Diseases Active Surveillance Network (FoodNet).15 The Centers for Disease Control and Prevention (CDC), the U.S. Food and Drug Administration (FDA), and the Gulf Coast states (Alabama, Florida, Louisiana, and Texas) initiated COVIS in 1988. By 1997, most states, including Maryland, were reporting cases via COVIS.16 The paper case report form (CRF) captures clinical details, underlying conditions, history of seafood consumption, and seawater exposure in the seven days prior to illness. Laboratory confirmation is required. Since 1996, the U.S. Department of Agriculture (USDA), FDA, CDC, and 10 state health departments, including Maryland, have used FoodNet to conduct active surveillance for cases otherwise missed by COVIS. FoodNet captures laboratory-confirmed vibriosis and other infections commonly transmitted through food to better understand foodborne disease epidemiology.
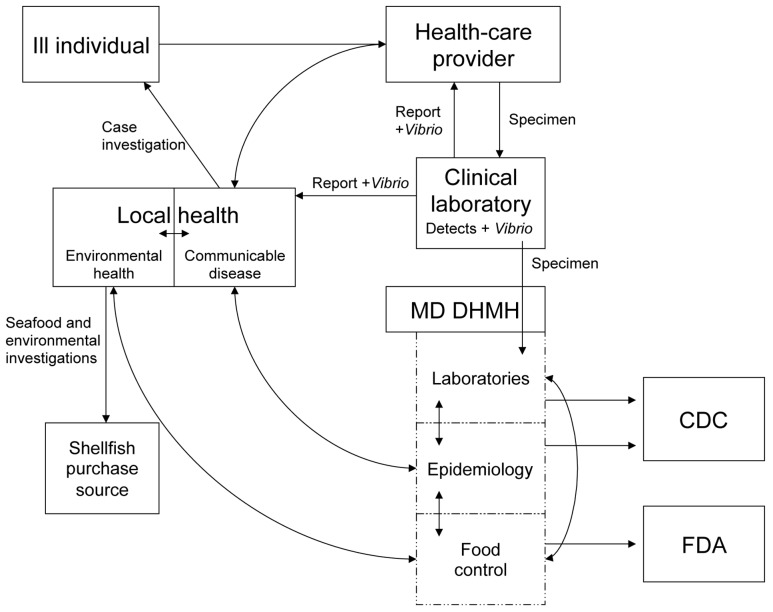
Surveillance case investigators at LHDs and DHMH gather information from patients, health-care providers, and clinical laboratories for each case (Figure 1) and record findings on the paper CRF and electronically in the National Electronic Disease Surveillance System (NEDSS). For patients with gastrointestinal illness, investigators also complete the paper gastroenteritis CRF that is specific to Maryland. LHD investigators fax the paper records to DHMH surveillance or DHMH food-control personnel (located in different physical locations) who oversee investigations and forward data to CDC. DHMH surveillance personnel maintain a spreadsheet to track the various components of the Vibrio investigations.
Figure 1.
The Vibrio surveillance system, Maryland, 2002–2008
MD DHMH = Maryland Department of Health and Mental Hygiene
CDC = Centers for Disease Control and Prevention
FDA = Food and Drug Administration
Additional programmatic activities are linked to the surveillance system and the sanitary control of shellfish. Maryland participates in the National Shellfish Sanitation Program (NSSP), which promotes consistency across states in the sanitation of oysters, mussels, clams, and scallops; risk assessment and risk management; growing area classification; dealer certification; and FDA evaluation of state program elements.17 When shellfish are implicated in an outbreak involving two or more people not from the same household, NSSP requires an epidemiologic investigation to determine an association between illness and shellfish. In Maryland, DHMH food-control personnel review the patient's food consumption history and the shellfish handling practices of the retailer to determine whether illness is related to a shellfish growing area or results from post-harvest contamination.18 If an association to shellfish is determined, LHD sanitarians inspect the purchase source within 24 hours for sanitation and food handling practices, collect environmental samples and any food still available, and retrieve oyster harvest tags. Federal regulations require oyster vendors and restaurants to retain harvest tags that include harvest date and location for at least 90 days after the product is gone.19 Environmental and sanitation controls are implemented to prohibit the sale of raw seafood until improvements are made.
The Maryland Department of the Environment protects shellfish harvest waters by identifying and eliminating sources of pollution and by routinely -collecting water samples and shell stock for bacterial and chemical toxicant testing. Locations that repeatedly exceed bacteriologic standards are restricted from harvesting until levels recede. The Maryland Department of Natural Resources posts and patrols restricted harvest waters and conducts the Maryland Beaches Program, which monitors public bathing beaches and closes beaches with poor water quality.
METHODS
The framework for this evaluation was based on CDC's “Updated Guidelines for Evaluating Public Health Surveillance Systems.”20 The evaluation included (1) informal qualitative interviews of state and local personnel who report and manage Vibrio cases to characterize the surveillance system, (2) description of 2002–2008 cases, and (3) review of Vibrio surveillance data from 2002 through 2008 for data quality and timeliness. Data were abstracted from NEDSS; for fields not captured electronically, data were abstracted from paper CRFs maintained by DHMH surveillance and DHMH food-control personnel. Cases were classified according to CSTE case definitions.
We reviewed variables including specimen source, signs and symptoms, evidence of a preexisting wound, exposure to brackish water, consumption of or exposure to raw seafood and seafood drippings, and occupational exposures and made a subjective determination as to whether the case was associated with seafood consumption or wound contamination. On occasion, there was not enough information to make a determination. We assessed data quality by reviewing the completeness of variables for occupation, exposure location (water location for wound infection cases and harvest location for seafood-associated cases), and important dates in the reporting continuum (date of onset, diagnosis, report to a public health agency, and seafood investigation completion). We assessed timeliness by measuring the elapsed time linking consecutive steps of the surveillance system.21
RESULTS
Interviews of system users allowed for an accurate description of the surveillance system (Figure 1). System users have adapted to multiple case definition changes (V. cholerae in 1990, 1995, and 1996 and non-cholera Vibrio in 2007) and implementation of electronic reporting of laboratory results.
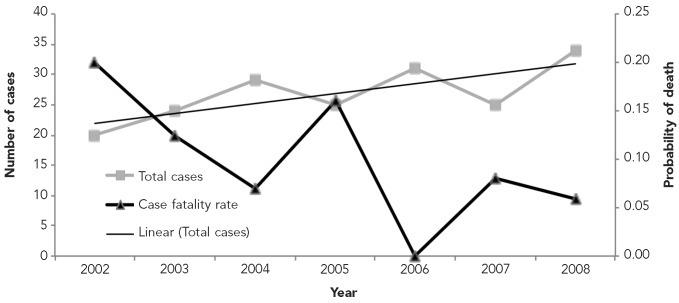
From 2002 to 2008, there were 188 laboratory-confirmed cases of vibriosis reported in Maryland (Figure 2), with an annual average of 27 cases. The Vibrio species most frequently identified, regardless of clinical presentation, were V. parahaemolyticus (43.6%), V. vulnificus (23.9%), V. alginolyticus (9.6%), and non-toxigenic V. cholerae (9.0%) (data not shown). While the number of cases of vibriosis increased, the case fatality rate (CFR) fluctuated during the study period (Figure 2) and the CFR paralleled the proportion of V. vulnificus cases.
Figure 2.
Laboratory-confirmed cases of Vibrio illness and probability of death from Vibrio species infection, Maryland, 2002–2008
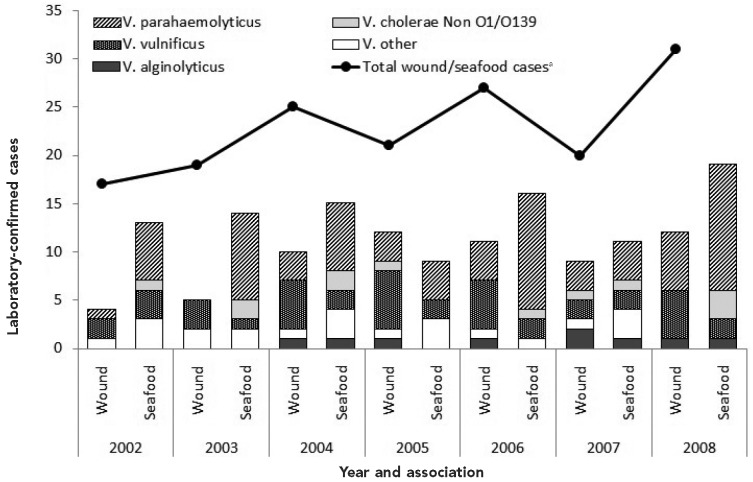
Sufficient information to subjectively determine a causative association of illness to water or seafood was available for 160 of 188 (85.1%) cases, 63 of which (39.4%) were water-associated wound infections and 97 of which (60.6%) were seafood-associated infections (Figure 3). The pathogen most frequently associated with both wound infections and seafood-associated cases was V. parahaemolyticus (12.5% of wound infections and 34.4% of seafood-associated cases). V. vulnificus was the second most frequent cause of infection (17.5% of wound infections and 8.8% of seafood-associated cases) (data not shown). The increase in the number of cases during the study period derives from increases in both water-associated wound infections and seafood-associated cases.
Figure 3.
Laboratory-confirmed cases of Vibrio illness, by species and association, Maryland, 2002–2008a
aCases of unknown association (n=28) are not shown.
We assessed the completeness of variables for occupation, exposure location, and important dates in the reporting continuum (Table). Occupation was collected for 173 (92.0%) cases. The most frequently reported occupation (n=9, 5.2%) was recreational or professional shellfish and crab harvesters. All nine -suffered water-associated wound infections from crabbing (data not shown). Exposure location was identified for 103 (54.7%) cases. Of the 63 water-associated wound infections, 46 (73.0%) reported a water location for their exposure, seven (11.1%) provided a land location proximal to the water exposure location, 10 (15.9%) did not report an exposure location, and eight (12.7%) provided enough detail to identify a specific water location (Table).
Table.
Completeness of selected variables for reported Vibrio illness in Maryland, 2002–2008
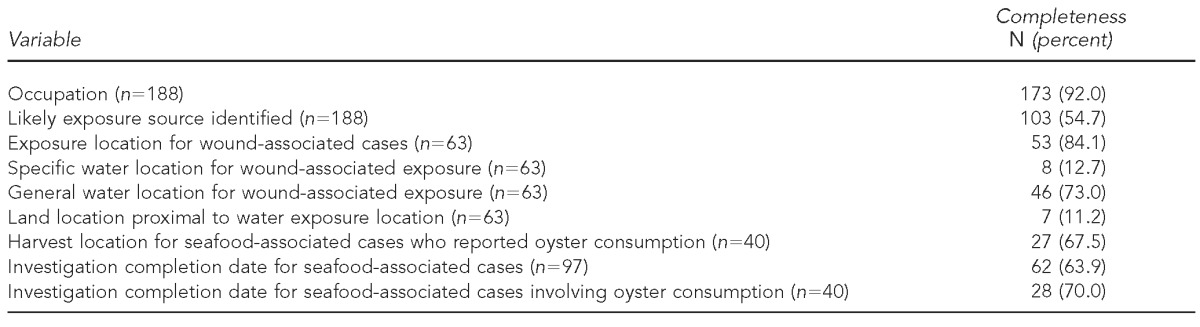
Seafood investigation information was most thoroughly captured on the paper CRF due to limitations in the variables captured in NEDSS. Of the 97 seafood-associated cases, 62 (63.9%) COVIS CRFs, maintained by either DHMH surveillance or DHMH food-control personnel, indicated a seafood investigation completion date (Table). Of the CRFs maintained by DHMH food-control personnel for the 40 seafood-associated cases with reported oyster consumption (which warrant a higher investigational priority), 27 (67.5%) identified an oyster harvest site. A review of CRFs maintained by DHMH surveillance personnel for the same 40 cases demonstrated that only 17 (42.5%) traceback investigations that identified an oyster harvest site were reported back to DHMH surveillance. Two-thirds of the cases were investigated and fewer than half of those investigated were communicated back to DHMH surveillance (data not shown).
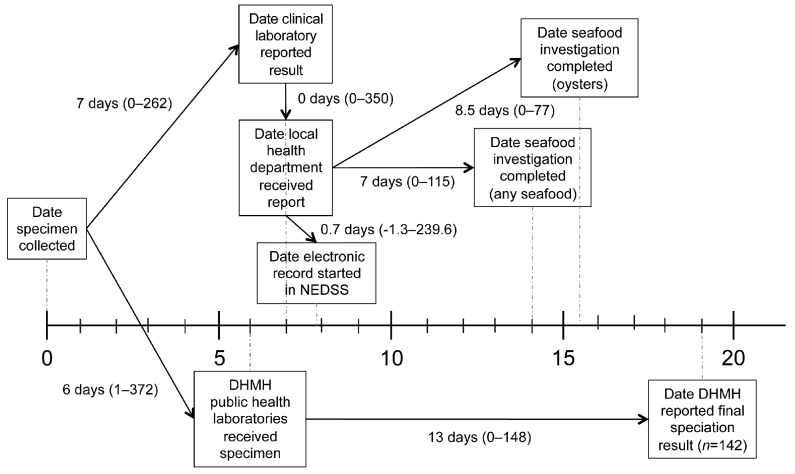
We assessed timeliness by measuring the elapsed time between consecutive steps of the surveillance system. The median number of days from specimen collection to when the laboratory reported a result to any public health agency was seven days (Figure 4), and LHDs typically started an electronic record in NEDSS the day they received a laboratory result. The median number of days from when the LHD received a laboratory report to the seafood investigation completion date for cases reporting oyster consumption was 8.5 days. The median number of days from when the DHMH PHL received the specimen to when DHMH reported the final speciation was 13 days. We examined outlying cases, where the median differed greatly from the mean, individually to determine the cause for such variance from the mean and found they were generally due to data entry errors and incomplete data.
Figure 4.
Timelinessa of the Vibrio surveillance system, Maryland, 2002–2008
aThe timeline reflects time in days, and results represent the median elapsed time linking any two consecutive steps of the surveillance system.
NEDSS = National Electronic Disease Surveillance System
MD DHMH = Maryland Department of Health and Mental Hygiene
DISCUSSION
The Vibrio surveillance system in Maryland successfully accomplishes its goals to identify opportunities for intervention and to monitor trends and patterns of vibriosis. The incidence of Vibrio cases in Maryland is similar to those identified nationally for the same time period,6 except that the contribution of V. parahaemolyticus in Maryland is higher than other states classified as inland states (50.6% in Maryland vs. 35.0% nationally), and Maryland's overall vibriosis incidence most closely resembles the higher incidence in coastal states, where consumption of shellfish and exposure to seawater would be expected to be most common.6,7 The system is representative for severe cases where diagnostic specimens were collected; however, mild, self-limiting infections may not be adequately represented. Patients with minor infections might be less likely to seek medical care, or if they do seek medical care, providers might treat them symptomatically. This limitation has also been recognized as a limitation of the national surveillance system.6
The system is flexible, as it has adapted to multiple case definition changes and transitions in data collection, including the implementation of electronic reporting of laboratory results. The flexibility is further underscored by the many contributors to the system and surveillance data users. Future changes to the system will require ongoing coordination among multiple agencies.
Despite its adaptability, the system is complex and cumbersome because it involves redundancy in data collection and cross-referencing of paper and electronic records. The NEDSS database does not capture all variables on the paper CRF, nor does it allow tracking of the components of an investigation. DHMH surveillance epidemiologists rely on a separate spreadsheet to ensure completion of the investigational components and rely on paper CRFs for seafood investigation and patient history details. The outcome of seafood investigations and the investigation completion date present in food-control records for seafood-associated cases were often not transmitted to the surveillance records, and explicit traceback findings were frequently missing altogether. Ideally, the NEDSS would mirror the CRF and contain investigation tracking fields, thereby eliminating paper CRFs and the additional tracking spreadsheet. Reducing redundancy could improve data integrity, completeness, and acceptability by users. Additional benefits would be improved coordination during investigations and swift, informed decision making to prevent further illness.
If some data are only available on paper, as is currently the case in Maryland, then a complete investigation record should be available in at least one central location for data integrity and for decision-making purposes. The evaluation identified numerous occasions in which data were not transferred from one group to the other at DHMH and a complete record was not available. While both DHMH food-control and DHMH surveillance personnel state that complete data sharing is the goal, the different physical locations of the two groups may hinder sharing; however, document scanning, e-mail, and fax transmission are readily available at each office.
Recreating and working in natural waters is not risk-free. Some disease-causing organisms occur naturally in brackish water while others are associated with the release of untreated sewage and animal waste into the water. The Maryland Beaches Program attempts to reduce this risk by monitoring the water quality of public bathing beaches for disease-causing organisms and posting and closing beaches with poor water quality. Improving public awareness of the symptoms of Vibrio infection and the potential risks of swimming with open wounds, especially for high-risk populations, may decrease the incidence of water-associated wound infections. Similarly, targeted educational messages aimed at professional and recreational crabbers on how to reduce risk and identify infections could increase awareness and prevent severe disease. In preparation for the summer recreation season and seafood harvesting, and to boost the number of cases with an identified water exposure location, LHD case investigation personnel would benefit from reviewing how Vibrio wound infections occur and the importance of capturing a water exposure location.
The absence of a standardized system to classify Vibrio cases as resulting from wound contamination or seafood exposure presented challenges when analyzing the surveillance data and could complicate the implementation of interventions. We attempted a systematic algorithm to determine the exposure; however, the distinction between water-associated wound infection and seafood-associated cases was not always clear, and we could not devise an algorithm that was comprehensive for all situations.
Improving the timeliness of any two steps in the surveillance system would potentially decrease the time to intervene when a source is implicated. Increased public awareness of the symptoms of and risk factors for vibriosis, and foodborne diseases in general, might motivate ill individuals to seek medical attention more promptly. Increasing health-care provider awareness, particularly of diagnostics and reporting requirements, could decrease the time between illness onset and when public health agencies are notified and more accurately capture the true burden of disease. The timeliness of seafood and environmental investigations could be improved with additional personnel and complete electronic data collection.
While it would be difficult to shorten the time it takes to confirm Vibrio by culture given current culture and speciation methodology, aspects of laboratory reporting could be improved specifically in Maryland. Surveillance epidemiologists do not receive real-time testing status from StarLIMS, as results are only reported to the original submitter. Automated alerts to DHMH surveillance epidemiologists regarding specimen submission and results would decrease the time needed to identify outbreaks. Modifications to StarLIMS, such as adding tracking information of the specimen testing status and data sharing regularly to DHMH surveillance epidemiologists, would improve the functionality of the Vibrio surveillance system.
Collaboration with additional partners in academia and federal agencies, such as the National Oceanic and Atmospheric Administration, CDC, FDA, and USDA, would allow all parties to better understand Vibrio ecology and infections. Further characterization of Vibrio and other health indicators in Maryland waters and investigation into climate change and Vibrio ecology would complement the public health surveillance system. Activities that have already been initiated include seasonal review of harvesting regulations, operations, and sanitation requirements (especially for aquaculture facilities during summer months); actions taken in response to these reviews could potentially reduce the impact of Vibrio infections in Maryland.
CONCLUSIONS
Vibrio is a naturally occurring waterborne pathogen with potential occupational, recreational, and commercial impacts. We have identified several areas for improvement to Maryland's surveillance system for Vibrio infections, including (1) better integration of data collection for clinical, laboratory, and environmental information; and (2) improved completion of variables for shellfish harvest or water exposure locations. Increased use of electronic health records and electronic laboratory reporting should help; however, greater coordination among quarterly training for all involved in Vibrio surveillance could have broader impact and aid in the implementation of improvement efforts. Key points to review include how to accurately capture exposure locations during patient interviews, pertinent regulations regarding the sale of oysters and shellfish, safe handling and sanitation procedures for prevention messaging, and quality assurance to ensure minimal data entry errors.
Footnotes
This study was supported in part by an appointment to the Applied Epidemiology Fellowship Program administered by the Council of State and Territorial Epidemiologists and funded by the Centers for Disease Control and Prevention Cooperative Agreement #1U38HM000414. The findings and conclusions in this article are those of the authors and do not necessarily reflect the views of the funding agencies.
Data are collected, managed, analyzed, and interpreted under public health surveillance authority and do not require human subject review or institutional review board approval.
REFERENCES
- 1.Davis JW, Sizemore RK. Incidence of Vibrio species associated with blue crabs (Callinectes sapidus) collected from Galveston Bay, Texas. Appl Environ Microbiol. 1982;43:1092–7. doi: 10.1128/aem.43.5.1092-1097.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (US), Center for Emerging and Zoonotic Infectious Diseases. Vibrio parahaemolyticus: general information [cited 2012 Jul 19] Available from: URL: http://www.cdc.gov/nczved/divisions/dfbmd/diseases/vibriop.
- 3.Centers for Disease Control and Prevention (US), Center for Emerging and Zoonotic Infectious Diseases. Vibrio vulnificus: general information [cited 2012 Jul 19] Available from: URL: http://www.cdc.gov/nczved/divisions/dfbmd/diseases/vibriov.
- 4.Centers for Disease Control and Prevention (US) Vibriosis (non-cholera Vibrio spp.): 2007 case definition [cited 2013 Jun 9] Available from: URL: http://wwwn.cdc.gov/NNDSS/script/casedef.aspx?CondYrID=891&DatePub=1/1/2007%2012:00:00%20AM.
- 5.Heymann DL, editor. Control of communicable diseases manual. 20th ed. Washington: American Public Health Association; 2009. [Google Scholar]
- 6.Newton A, Kendall M, Vugia DJ, Henao OL, Mahon BE. Increasing rates of vibriosis in the United States, 1996–2010: review of surveillance data from 2 systems. Clin Infect Dis. 2012;54(Suppl 5):S391–5. doi: 10.1093/cid/cis243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Preliminary FoodNet data on the incidence of infection with pathogens transmitted commonly through food—10 states, 2009. MMWR Morb Mortal Wkly Rep. 2010;59(14):418–22. [PubMed] [Google Scholar]
- 8.Chesapeake Bay Foundation. Bad water 2009: the impact on human health in the Chesapeake Bay region. Annapolis (MD): Chesapeake Bay Foundation; 2009. Also available from: URL: http://www.cbf.org/document.doc?id=328 [cited 2012 Nov 8] [Google Scholar]
- 9. Md. Code Ann. §18-201 (West 2012) [Google Scholar]
- 10. Md. Code Ann. §18-205 (West 2012) [Google Scholar]
- 11. COMAR 10.06.01. [Google Scholar]
- 12.Centers for Disease Control and Prevention (US) Cholera (Vibrio cholerae O1/O139): 1996 case definition [cited 2012 Aug 28] Available from: URL: http://wwwn.cdc.gov/NNDSS/beta/bcasedef.aspx?CondYrID=639&DatePub=1/1/1996%2012:00:00%20AM.
- 13.Maryland Department of Health and Mental Hygiene. Guidelines for the epidemiological investigation of cholera and other Vibrio species infections. 2004 [cited 2012 Jul 19] Available from: URL: http://ideha.dhmh.maryland.gov/IDEHASharedDocuments/guidelines/VibrioGuidelines_2004_final.pdf.
- 14.Centers for Disease Control and Prevention (US) Cholera and Other Vibrio Illness Surveillance System (COVIS) [cited 2012 Oct 11] Available from: URL: http://www.cdc.gov/nationalsurveillance/cholera_vibrio_surveillance.html.
- 15.Centers for Disease Control and Prevention (US) Foodborne Diseases Active Surveillance Network (FoodNet) [cited 2012 Oct 11] Available from: URL: http://www.cdc.gov/foodnet.
- 16.Centers for Disease Control and Prevention (US) Summary of human Vibrio cases reported to CDC, 2007 [cited 2012 Sep 12] Available from: URL: http://www.cdc.gov/nationalsurveillance/PDFs/CSTEVibrio2007.pdf.
- 17.Food and Drug Administration (US) National Shellfish Sanitation Program (NSSP) [cited 2013 Jun 9] Available from: URL: http://www.fda.gov/Food/GuidanceRegulation/FederalStateFood Programs/ucm2006754.htm.
- 18.Food and Drug Administration (US) National Shellfish Sanitation Program: guide for the control of molluscan shellfish, 2009 revision [cited 2013 Jun 9] Available from: URL: http://www.fda.gov/downloads/Food/GuidanceRegulation/FederalStateFood Programs/UCM350004.pdf.
- 19.Food and Drug Administration (US) National Shellfish Sanitation Program. 2009 NSSP guide for the control of molluscan shellfish: section IV: guidance documents; chapter III: harvesting, handling, processing, distribution;.04 shellstock tagging [cited 2013 Jun 9] Available from: URL: http://www.issc.org/client_ resources/2009%20nssp%20guide/section%20iv%20chapter%20 iii%20.04.pdf.
- 20.Updated guidelines for evaluating public health surveillance systems: recommendations from the Guidelines Working Group. MMWR Recomm Rep. 2001;50(RR13):1–35. [PubMed] [Google Scholar]
- 21.Jajosky RA, Groseclose SL. Evaluation of reporting timeliness of public health surveillance systems for infectious diseases. BMC Public Health. 2004;4:29. doi: 10.1186/1471-2458-4-29. [DOI] [PMC free article] [PubMed] [Google Scholar]