Abstract
Objective
To determine the prevalence of hypothyroidism in an adult female population in Puerto Rico and to determine the relationship between hypothyroidism, bone mineral density and vertebral and non-vertebral fractures in this population.
Methods
Data from the 400 subjects database of the Latin American Vertebral Osteoporosis Study (LAVOS), Puerto Rico site was reviewed. Patient’s medical history, anthropometric data, current medications, laboratories, and DXA results was extracted. Subjects with thyroid dysfunction were identified based on their previous medical history and levels of TSH. Bone Mineral Density was classified using the World Health Organization criteria. Crude prevalence of thyroid dysfunction were estimated with a confidence of 95% and weighted by the population distribution by age, according to the distribution by age group in the 2000 census. Bone mineral densities and prevalence of vertebral and non-vertebral fractures were compared among the groups.
Results
The weighted prevalence of hyperthyroidism in this population was 0.0043% (95% CI: −0.0021%, 0.0107%). The weighted prevalence of hypothyroidism was 24.2% (95% CI: 19.9%, 28.4%). Increased prevalence of hypothyroidism was found in participants 70 years or older. The mean BMD at spine, hip and femoral neck was similar among the groups. No difference in the proportion of participants with vertebral and non-vertebral fractures was found among the groups.
Conclusion
Our study found a high prevalence of hypothyroidism among adult postmenopausal females in Puerto Rico. No association between hypothyroidism and decreased bone mineral densities, vertebral or non-vertebral fractures was found in this population.
Keywords: hypothyroidism, TSH, BMD, Puerto Rico, LAVOS
Introduction
Diseases of the thyroid gland are common in adults. Thyroid dysfunction is diagnosed by measurement of the serum thyrotropin concentration, also known as the thyroid stimulating hormone (TSH). To date, serum TSH measurement is the best and most reliable test to diagnose problems with the thyroid gland (1–2). Thyroid dysfunction is defined according to clinical signs, symptoms, and the levels of TSH. Hypothyroidism is diagnosed by a TSH above the reference range and hyperthyroidism by TSH levels below the reference range. Epidemiological studies regarding the prevalence of thyroid dysfunction in Puerto Rico are lacking. Studies in special groups in Puerto Rico have shown a prevalence of 8.2% of hypothyroidism and 2.1% of hyperthyroidism in a group of overweight subjects ≥ 21 years old at a Weight Loss Clinic in Puerto Rico (3) and Molina et al. found that among patients with systemic lupus erythematous in Puerto Rico, the prevalence of hypothyroidism and hyperthytroidism were 19% and 0.3%, respectively (4).
According to the National Health and Nutrition Examination Survey (NHANES III) in which the general non-institutionalized population aged > 12 years old in the United States were evaluated, the prevalence of hypothyroidism and hyperthyroidism are 3.7% and 0.5%, respectively (5). Several studies have reported a variation in the levels of TSH and the prevalence of thyroid dysfunction by ethnicity, gender, and age (5–8). It has been shown that thyroid dysfunction is more common in females (1). In 1985, Nolan et al. found in a population of adult patients evaluated at Mount Auburn Hospital in Massachusetts, USA, an estimated incidence of hypothyroidism of 0.5% and hyperthyroidism of 0.2% in women (9). In another study, Vanderpump et al. found a prevalence of hypothyroidism of 9.3% and hyperthyroidism of 3.9% in women between 38 – 93 years of age (10). The majority of these studies have been conducted in non-hispanic populations (caucasians, blacks). Only few studies have reported the prevalence of thyroid dysfunction in the Hispanic population. In 2011, Marzouka et al. found an increased prevalence of hypothyroidism in patients with congestive heart failure among Hispanics > 18 years old (7). Similarly, Hinton et al. found an increased incidence of congenital hypothyroidism among Hispanic newborns when compared with non- Hispanics (11).
Thyroid dysfunction is associated with a broad range of metabolic disturbances and conditions such as: osteoporosis, hypercholesterolemia, obesity, and cardiovascular disease (12–18). There is a strong relationship between hyperthyroidism and decreased bone mineral density (BMD) and osteoporosis. Overt hyperthyroidism is associated with decreased BMD, and osteoporosis due to an accelerated bone remodeling (12–13). There is also an increased risk of fractures in these patients (19–20). Overt hypothyroidism has also been associated with an increased risk of fractures (21–22). A recent study also found an association between subclinical hypothyroidism and decreased bone structure and bone strength (23). On the other hand, there are studies that found no correlation between BMD and TSH levels (24). There are also studies suggesting that mild variations in thyroid hormone levels within the normal range could affect bone health as well, increasing the risk for vertebral and non-vertebral fractures (25–26). Another study from Korea, conducted in men, suggests an association between TSH concentration at the lower end of the reference range and low BMD (25). On the other hand, other studies failed to confirm these correlations (26–29). For this reason the relationship between TSH levels rather than thyroid hormone levels and decreased BMD remains controversial.
The aim of this study was to estimate the prevalence of thyroid dysfunction in a population-based sample of adult postmenopausal females ages 50 to 90 years in Puerto Rico and to determine the relationship between thyroid dysfunction, bone mineral density and vertebral and non-vertebral fractures in this population.
Methods
This retrospective study was conducted at the Endocrinology Clinics of the University Hospital in San Juan, Puerto Rico. Data from the 400 subjects’ database of the Latin American Vertebral Osteoporosis Study (LAVOS), Puerto Rico site were reviewed. LAVOS study is the first population-based study of vertebral fractures in Latin America (30). The objective of this study was to evaluate the prevalence of vertebral fractures in Latin American women. A random sample of 1,922 women 50 years and older from Argentina, Brazil, Colombia, Mexico and Puerto Rico were evaluated. In Puerto Rico, a random sample of households in San Juan was obtained using a probability cluster design with a total of 400 women 50 years and older selected (31). Evaluation consisted of a 30 minutes face to face interview to gather data on demographics, risk factors, and lifestyles. Imaging studies consisted of dual energy X-ray (DXA), lateral dorsolumbar X-rays and digital morphometry to determine vertebral deformities by Eastel criterion. Clinical parameters extracted for this study included: patient’s medical history, anthropometric data, current medications, laboratories, and DXA results. Patients who self-reported thyroid dysfunction and de novo patients with thyroid dysfunction were identified based on their levels of TSH. Thyroid dysfunction was classified (according to the reference range) as follows: hypothyroidism (TSH > 5.5 mIU/mL), normal function (TSH 0.35 – 5.5 mIU/mL) and hyperthyroidism (TSH < 0.35 mIU/mL). Patients with previous diagnosis of hypo- or hyperthyroidism who were on treatment at the moment of evaluation remained classified according to initial diagnosis. Bone Mineral Density was classified using the World Health Organization criteria (32).
This study was approved by the Institutional Review Board of the University of Puerto Rico, Medical Sciences Campus.
Statistical Analysis
Continuous variables were summarized using means and standard deviation; frequencies and percentages were used to summarize categorical variables.
Crude prevalence of thyroid dysfunction estimated was weighed by the population distribution by age, according to the distribution by age group in the 2000 census. Relationships between hypothyroidism and vertebral or non-vertebral fractures were evaluated using Chi-square test for independence. Independent sample t-tests were used to compare BMD among the groups. A p < 0.05 was considered statistically significant. Statistical analyses were performed using Stata software version 11.0 (StataCorp).
Results
The population consisted of 399 postmenopausal women between the ages 50 – 90 years old from San Juan, Puerto Rico who participated in the LAVOS study performed in 2003. One subject was eliminated due to age < 50 y/o. The mean age of this population was 67.6 ± 10.7 years and the age distribution was 111 participants (27.8%) in the 50 to 59 age group, 109 participants (27.3%) in the 60 to 69 age group, 112 participants (28.1%) in the 70 to 79 age group, and 67 participants (16.8%) in the 80 years and over age group (Table 1). One hundred fifty nine participants (39.8%) had a Body Mass Index (BMI) in the category of overweight (BMI 25.0 to 29.9) and 163 participants (40.9%) had a BMI in the category of obesity (BMI ≥ 30.0 Kg/m2) (Table 1). The weighted prevalence of hyperthyroidism (TSH levels < 0.35 mIU/mL) in this population was 0.0043% (95% CI: −0.0021%, 0.0107%) whereas the weighted prevalence of hypothyroidism (TSH > 5.5 mIU/mL) was 24.2% (95% CI: 19.9%, 28.4%). Among these participants, 14.5% had a previous history of hypothyroidism, and 9.7% were newly diagnosed. All patients with previous history of hypothyroidism were taking thyroid hormones. Twenty percent (20.7%) of these participants, who were taking replacement therapy with thyroid hormones, had increased TSH levels, 6.9% had decreased TSH levels, and 72.4% had TSH levels within the normal range (Table 2). Increased prevalence of hypothyroidism was found in participants 70 years or older. Among these participants, hypothyroidism was found in 27.7% and 35.8% in the 70–79 and 80+ years old age groups respectively (Fig 1).
Table 1.
Patient’s characteristics
| Characteristics | n | % |
|---|---|---|
| Age groups (years) | ||
| 50–59 | 111 | 27.8 |
| 60–69 | 109 | 27.3 |
| 70–79 | 112 | 28.1 |
| ≥ 80 | 67 | 16.8 |
| Total9 | 399 | 100 |
| BMI (Kg/m2) | ||
| < 18.5 | 7 | 1.8 |
| 18.5 – 24.9 | 70 | 17.5 |
| 25.0 – 29.9 | 159 | 39.8 |
| ≥ 30 | 163 | 40.9 |
| Total | 399 | 100 |
Table 2.
TSH levels of patients with previous history of hypothyroidism taking thyroid hormones (n=58)
| TSH levels | n | % |
|---|---|---|
| Decreased ( < 0.35 mIU/mL) | 4 | 6.9 |
| Normal (0.35 – 5.5 mIU/mL) | 42 | 72.4 |
| Increased ( > 5.5 mIU/mL) | 12 | 20.7 |
Figure 1.
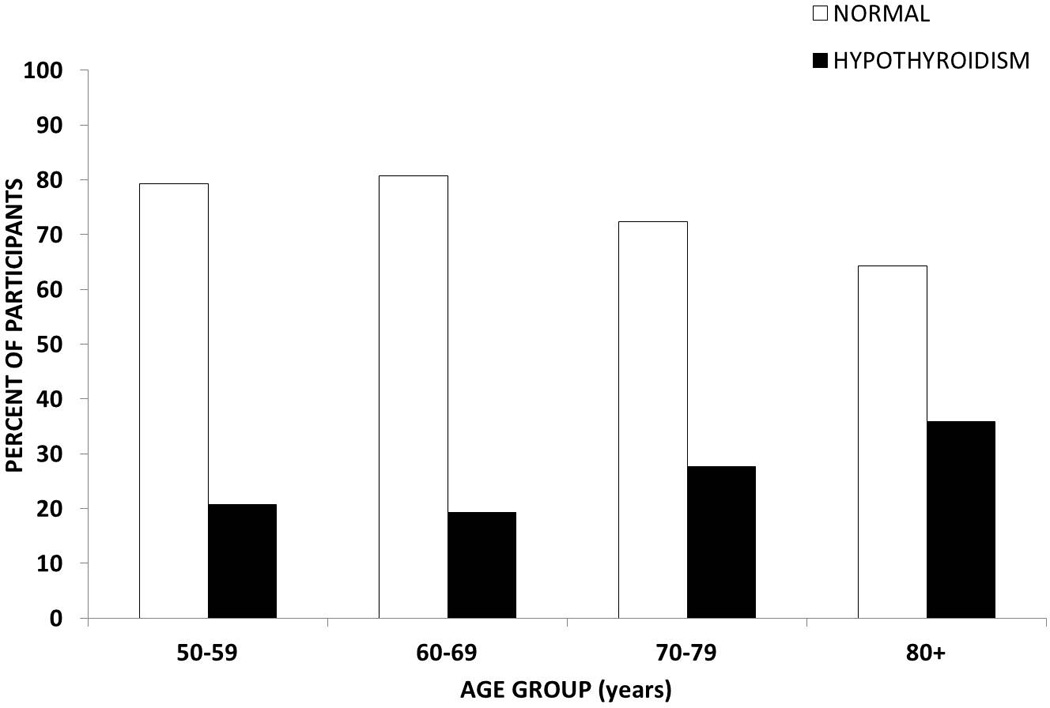
Distribution of hypothyroidism among different age groups in postmenopausal females ages 50 – 90 years who participated in LAVOS study- Puerto Rico site.
Participants with hypothyroidism had lower bone mineral densities at lumbar spine, hip, and femoral neck when compared to participants with normal TSH levels. However, this difference was not statistically significant (p > 0.05). The mean BMD for the participants with normal TSH levels were 0.90 ± 0.17 g/cm2 at lumbar spine, 0.84 ± 0.14 g/cm2 at total hip, and 0.70 ± 0.13 g/cm2 at femoral neck site. The mean BMD for the participants with elevated TSH levels were 0.88 ± 0.19 g/cm2 at lumbar spine, 0.82 ± 0.18 g/cm2 at total hip, and 0.68 ± 0.15 g/cm2 at femoral neck site (Fig 2). No association between hypothyroidism and decreased bone mineral densities at lumbar spine, hip, and femoral neck was found in the overall population. When the 4 subjects with decreased TSH were eliminated from the hypothyroid group, no statistically significant difference were found in the BMDs, as well as the comparison of participants on and off treatment (data not shown). Cases with hyperthyroidism (3 subjects) were excluded from the analysis due to inadequate sample size for comparison. Any test or comparison will lack the statistical sensitivity (power) needed to detect a true statistical significant difference between groups, thus, increasing the probability of committing a type II error and of yielding false-negative results.
Figure 2.
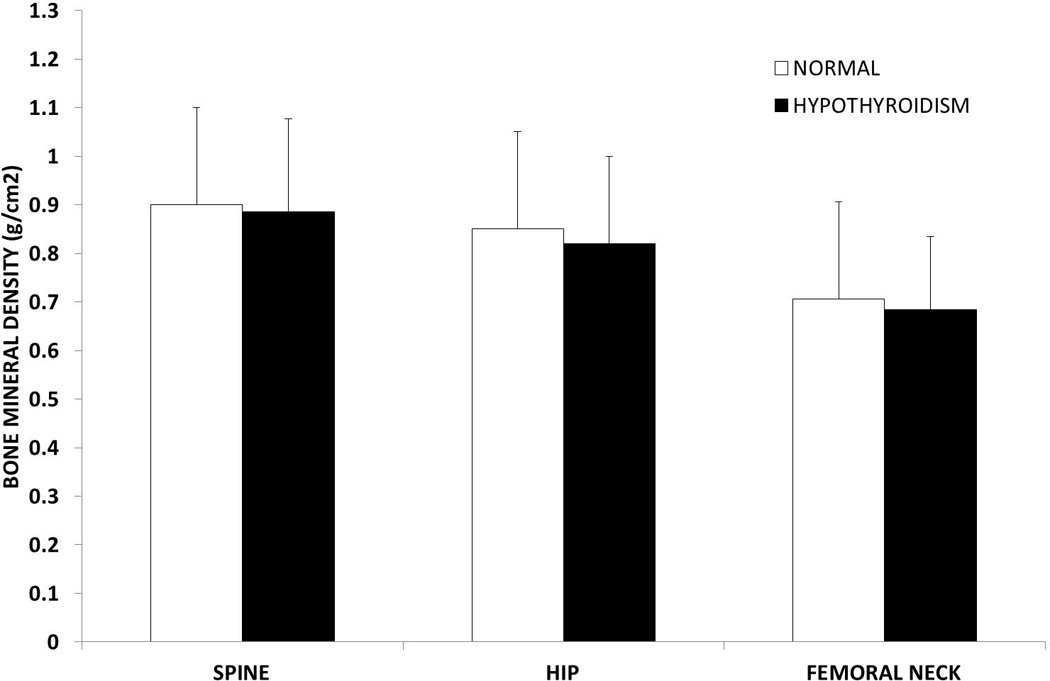
Bone mineral densities at different sites among postmenopausal females ages 50 – 90 years who participated in the LAVOS study – Puerto Rico site.
A total of 48 vertebral fractures were found in this population. The prevalence of vertebral fractures was 11.1% among participants with hypothyroidism and 12.3% among those without hypothyroidism. A total of 37 non-vertebral fractures were found in this population. The prevalence of non-vertebral fractures was 10.1% for the group with hypothyroidism and 9.0% for the group without hypothyroidism. No association between hypothyroidism and vertebral or non-vertebral fractures was found in this population.
Discussion
Information about thyroid dysfunction in the Hispanic population is scarce. Our study found that the prevalence of hypothyroidism in a sample of postmenopausal women 50 – 90 years old in Puerto Rico is 24.2%. Similar studies of other populations of women 42 years and older have found a prevalence of hypothyroidism ranging from 6.2% to 11.6% (Table 3). The higher prevalence found in our study is consistent with other studies that suggest ethnic variations in the prevalence of this condition, with increased prevalence among Hispanics (3,7,11). The proportion of subjects with hypothyroidism in our population increased with age (Fig 1), which is consistent with other studies (5,8,33). Almost 28% of participants with previous history of hypothyroidism who were on thyroid hormone replacement therapy had inadequate TSH levels with 6.9% having decreased levels and 20.7% still having elevated levels. This is also consistent with data from other studies that reported inadequate replacement of thyroid hormones in patients with hypothyroidism (5,8,34). This finding can be secondary to inadequate replacement therapy or poor medication compliance by the patients.
Table 3.
Prevalence of thyroid dysfunction among different populations
| Study reference |
Time | Population Age |
Study site |
n | Ethnicity | TSH levels (mIU/mL) |
Total prevalence |
|---|---|---|---|---|---|---|---|
| NHANES III (5) | 1999–2002 | General non-institutionalized > 12 yrs |
USA | 4392 | Multiethnic | > 4.5 < 0.1 |
3.7% 0.5% |
| Marzouka et al 2011 (7) | 2007–09 | Heart failure patients > 18 yrs |
USA | 194 | Hispanic and non-hispanic blacks | > 5.1 | 23% |
| Figueroa et al 2008 (3) | 2005 | adults > 21 yrs | PR | 575 | Hispanics | > 4.1 < 0.4 |
8.2% 2.1% |
| Parle et al. 1991 (34) | 1988–89 | > 60 yrs | UK | 1210 | Caucasians | > 5.0 < 0.5 |
F: 11.6% M: 2.9% F: 6.3% M: 5.5% |
| Sowers et al 2003 (42) | 1995–97 | Women 42 – 52 yrs |
USA | 3302 | Multiethnic | > 5.0 < 0.5 |
6.2% 3.2% |
| Benseñor et al 2011(43) | 2003–05 | Residents of economically deprived area ≥ 65 yrs |
Brazil | 1373 | Brazilian | > 5.0 < 0.4 |
F: 12.6% M: 11.5% F: 3.6% M: 2.3 % |
| Petersen et al 1991(44) | 1980–81 | Women 50 – 72 yrs |
Sweden | 1154 | Swedish | > 4.0 | 3.3% |
| Present study (LAVOS-PR site) | 2003 | women 50–90 yrs |
PR | 399 | Hispanics | > 5.5 < 0.35 |
24.2% 0.0043% |
It has been proposed that TSH by itself and its effect on the TSH receptors found on osteoblast and osteoclast precursors are associated with bone resorption and formation in mice (35,36). Several studies in humans have reported an association between low-normal serum TSH levels and decreased BMD (37–38). Other studies have suggested hypothyroidism to be a risk factor for fractures (21,39). In our study, no association between elevated levels of TSH and bone mineral density was found. We also found no association between hypothyroidism and vertebral and non-vertebral fractures in this population.
There are some limitations in our study. First, no information about time of diagnosis of hypothyroidism or symptoms associated to hypothyroidism was available. Second, free T3 and free T4 levels were not measured which limits the identification of overt hypothyroidism versus subclinical hypothyroidism. Third, information reference to concomitant medications or nutritional supplements that can affect the thyroid function in these participants was not available. This is particularly relevant since there are several factors that can affect the thyroid function in an individual such as iodine deficiency or excess, and drugs such as lithium, amiodarone, and interferon alfa, among others. It has been suggested that nutritional supplements and herbs such as ginseng, echinacea, and ginger can affect the thyroid function. Some of these supplements are frequently used in our community. However, since these supplements are not regulated by the Food and Drug Administration the exact pharmacological composition and effects are unknown. In 2008, Poon et al reported 3 patients found with factitious thyrotoxicosis secondary to herbal supplements for weight loss (40). On the other hand, there is limited information about these supplements and the possible effects in suppressing the thyroid function.
Screening for thyroid dysfunction has been controversial. Currently there is no consensus at what age screening for thyroid dysfunction should be started. According to the American Thyroid Association, which published a guideline for detection of thyroid dysfunction in 2000, screening is recommended in adults beginning at age 35 years and to be repeated every 5 years thereafter (1). Conversely, a statement published by the US Preventive Services Task Force in 2004 recommend against routine screening in adults (41). Currently, screening is performed in patients with risk factors or clinical symptoms for thyroid dysfunction such as goiter, previous history of radiotherapy or neck surgery, diabetes mellitus, vitiligo, medications like amiodarone or lithium, fatigue, and cold intolerance among others. Screening is also performed in pregnancy due to the deleterious effects and complications that untreated thyroid dysfunction can cause in the mother and the developing fetus. The variable screening practices may underestimate the true prevalence of thyroid disease in these populations.
In conclusion, our study found a high prevalence of hypothyroidism among adult postmenopausal females in Puerto Rico. No difference in BMDs nor prevalence of vertebral and non-vertebral fractures were found when compared to the non-hypothyroid group. Screening for thyroid disease is still controversial. Nonetheless, the higher prevalence of hypothyroidism in our population warrants further investigation.
Acknowledgements
This work has no funding source of support.
L.G. was supported by an educational grant from Lilly USA, LLC. This publication was possible by grants from the National Center for Research Resources (U54 RR 026139-01A1) and the National Institute on Minority Health and Health Disparities (8U54 MD 007587-03) from the National Institutes of Health.
Footnotes
The authors have no conflict of interest to disclose.
References
- 1.Ladenson PW, Singer PA, Ain KB, et al. American Thyroid Association guidelines for detection of thyroid dysfunction. Arch Intern Med. 2000;160(11):1573–1575. doi: 10.1001/archinte.160.11.1573. [DOI] [PubMed] [Google Scholar]
- 2.Baskin HJ, Cobin RH, Duick DS, et al. American Association of Clinical Endocrinologists American Association of Clinical Endocrinologists medical guidelines for clinical practice for the evaluation and treatment of hyperthyroidism and hypothyroidism. Endocr Pract. 2002;8(6):457–469. [PubMed] [Google Scholar]
- 3.Figueroa B, Vélez H, Irizarry-Ramírez M. Association of thyroid-stimulating hormone levels and body mass index in overweight Hispanics in Puerto Rico. Ethn Dis. 2008;18(2Supp2):S2151–S2154. [PubMed] [Google Scholar]
- 4.Molina MJ, Mayor AM, Franco AE, Morell CA, López MA, Vilá LM. Prevalence of systemic lupus erythematosus and associated comorbidities in Puerto Rico. J Clin Rheumatol. 2007;13(4):202–204. doi: 10.1097/RHU.0b013e318124a8af. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aoki Y, Belin RM, Clickner R, Jeffries R, Phillips L, Mahaffey KR. Serum TSH and total T4 in the United States population and their association with participant characteristics: National Health and Nutrition Examination Survey (NHANES 1999–2002) Thyroid. 2007;17(12):1211–1223. doi: 10.1089/thy.2006.0235. [DOI] [PubMed] [Google Scholar]
- 6.Schectman JM, Kallenberg GA, Hirsch RP, Shumacher RJ. Report of an association between race and Thyroid Stimulating Hormone level. Am J Public Health. 1991;81(4):505–506. doi: 10.2105/ajph.81.4.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marzouka G, Cortazar F, Alvarez JA, Dias A, Hebert K. Racial and sex differences in prevalence of hypothyroidism in patients with cardiomyopathies enrolled into a heart failure disease management program. Congest Heart Fail. 2011;17(3):133–139. doi: 10.1111/j.1751-7133.2011.00215.x. [DOI] [PubMed] [Google Scholar]
- 8.Canaris GJ, Manowitz NR, Mayor G, Ridgway EC. The Colorado Thyroid Disease Prevalence Study. Arch Intern Med. 2000;160(4):526–534. doi: 10.1001/archinte.160.4.526. [DOI] [PubMed] [Google Scholar]
- 9.Nolan JP, Tarsa NJ, DiBenedetto G. Case-finding for unsuspected thyroid disease: Cost and health benefits. Am J Clin Pathol. 1985;83(3):346–355. doi: 10.1093/ajcp/83.3.346. [DOI] [PubMed] [Google Scholar]
- 10.Vanderpump MP, Tunbridge WM, French JM, et al. The incidence of thyroid disorders in the community: a twenty-year follow-up of the Whickham Survey. Clin Endocrinol. 1995;43(1):55–68. doi: 10.1111/j.1365-2265.1995.tb01894.x. [DOI] [PubMed] [Google Scholar]
- 11.Hinton CF, Harris KB, Borgfeld L, et al. Trend in incidence rates of congenital hypothyroidism related to select demographic factors: data from the United Sates, California, Massachusetts, New York, and Texas. Pediatrics. 2010;125(Suppl2):S37–S47. doi: 10.1542/peds.2009-1975D. [DOI] [PubMed] [Google Scholar]
- 12.Linde J, Friis T. Osteoporosis in hyperthyroidism estimated by photon absorptiometry. Acta Endocrinol. 1979;91(3):437–448. doi: 10.1530/acta.0.0910437. [DOI] [PubMed] [Google Scholar]
- 13.Eriksen EF. Normal and pathological remodeling of human trabecular bone: three dimensional reconstruction of the remodeling sequence in normals and in metabolic bone disease. Endocr Rev. 1986;7(4):379–408. doi: 10.1210/edrv-7-4-379. [DOI] [PubMed] [Google Scholar]
- 14.Tagami T, Kimura H, Ohtani S, et al. Multi-center study on the prevalence of hypothyroidism in patients with hypercholesterolemia. 2011;58(6):449–457. doi: 10.1507/endocrj.k11e-012. [DOI] [PubMed] [Google Scholar]
- 15.Rotondi M, Magri F, Chiovato L. Thyroid and obesity: Not a one way-interaction. J Clin Endocrinol Metab. 2011;96(2):344–346. doi: 10.1210/jc.2010-2515. [DOI] [PubMed] [Google Scholar]
- 16.Walsh JP, Bremner AP, Bulsara MK, et al. Subclinical thyroid dysfunction as a risk factor for cardiovascular disease. Arch Intern Med. 2005;165(21):2467–2472. doi: 10.1001/archinte.165.21.2467. [DOI] [PubMed] [Google Scholar]
- 17.Razvi S, Weaver JU, Vanderpump MP, Pearce SH. The incidence of ischemic heart disease and mortality in people with subclinical hypothyroidism: reanalysis of the Whickham Survey cohort. J Clin Endocrinol Metab. 2010;95(4):1734–1740. doi: 10.1210/jc.2009-1749. [DOI] [PubMed] [Google Scholar]
- 18.Hak AE, Pols HA, Visser TJ, Drexhage HA, Hofman A, Witteman JC. Subclinical hypothyroidism is an independent risk factor for atherosclerosis and myocardial infarction in elderly women: the Rotterdam Study. Ann Intern Med. 2000;132(4):270–278. doi: 10.7326/0003-4819-132-4-200002150-00004. [DOI] [PubMed] [Google Scholar]
- 19.Wejda B, Hintze G, Katschinski B, Olbricht T, Benker G. Hip fractures and the thyroid: a case-control study. J Intern Med. 1995;237(3):241–247. doi: 10.1111/j.1365-2796.1995.tb01172.x. [DOI] [PubMed] [Google Scholar]
- 20.Cummings SR, Nevitt MC, Browner WS, et al. Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med. 1995;332(12):767–773. doi: 10.1056/NEJM199503233321202. [DOI] [PubMed] [Google Scholar]
- 21.Ahmed LA, Schirmer H, Berntsen GK, Fønnebø V, Joakimsen RM. Self-reported diseases and the risk of non-vertebral fractures: the Tromsø study. Osteoporos Int. 2006;17(1):46–53. doi: 10.1007/s00198-005-1892-6. [DOI] [PubMed] [Google Scholar]
- 22.Vestergaard P, Mosekilde L. Fractures in patients with hyperthyroidism and hypothyroidism: a nationwide follow-up study in 16,249 patients. Thyroid. 2002;12(5):411–419. doi: 10.1089/105072502760043503. [DOI] [PubMed] [Google Scholar]
- 23.Nagata M, Suzuki A, Sekiguchi S, et al. Subclinical hypothyroidism is related to lower heel QUS in postmenopausal women. Endocr J. 2007;54(4):625–630. doi: 10.1507/endocrj.k06-201. [DOI] [PubMed] [Google Scholar]
- 24.Marwaha RK, Garg MK, Tandon N, et al. Thyroid function and bone mineral density among Indian subjects. Indian J Endocrinol Metab. 2012;16(4):575–579. doi: 10.4103/2230-8210.98014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim BJ, Lee SH, Bae SJ, et al. The association between serum thyrotropin (TSH) levels and bone mineral density in healthy euthyroid men. Clin Endocrinol. 2010;73(3):396–403. doi: 10.1111/j.1365-2265.2010.03818.x. [DOI] [PubMed] [Google Scholar]
- 26.Grimnes G, Emaus N, Joakimsen RM, Figenschau Y, Jorde R. The relationship between serum TSH and bone mineral density in men and postmenopausal women: the Tromsø study. Thyroid. 2008;18(11):1147–1155. doi: 10.1089/thy.2008.0158. [DOI] [PubMed] [Google Scholar]
- 27.Svare A, Nilsen TI, Bjøro T, Forsmo S, Schei B, Langhammer A. Hyperthyroid levels of TSH correlate with low bone mineral density: the HUNT 2 study. Eur J Endocrinol. 2009;161(5):779–786. doi: 10.1530/EJE-09-0139. [DOI] [PubMed] [Google Scholar]
- 28.De Rosa G, Testa A, Maussier ML, Callà C, Astazi P, Albanese C. A slightly suppressive dose of L-thyroxine does not affect bone turnover and bone mineral density in pre- and postmenopausal women with nontoxic goitre. Horm Metab Res. 1995;27(11):503–507. doi: 10.1055/s-2007-980012. [DOI] [PubMed] [Google Scholar]
- 29.Bauer DC, Nevitt MC, Ettinger B, Stone K. Low thyrotropin levels are not associated with bone loss in older women: a prospective study. J Clin Endocrinol Metab. 1997;82(9):2931–2936. doi: 10.1210/jcem.82.9.4229. [DOI] [PubMed] [Google Scholar]
- 30.Clark P, Cons-Molina F, Deleze M, et al. The prevalence of radiographic vertebral fractures in Latin American countries: the Latin American Vertebral Osteoporosis Study (LAVOS) Osteoporos Int. 2009;20(2):275–282. doi: 10.1007/s00198-008-0657-4. [DOI] [PubMed] [Google Scholar]
- 31.Haddock L, Pérez CM, Marrero E, et al. The prevalence of vertebral fractures in San Juan, Puerto Rico: a population-based study among females aged 50 years and over. P R Health Sci J. 2010;29(4):377–384. [PubMed] [Google Scholar]
- 32.Kanis JA, Melton LJ, III, Christiansen C, Johnston CC, Khaltaev N. The diagnosis of osteoporosis. J Bone Miner Res. 1994;9(8):1137–1141. doi: 10.1002/jbmr.5650090802. [DOI] [PubMed] [Google Scholar]
- 33.Sawin CT, Castelli WP, Hershman JM, McNamara P, Bacharach P. The aging thyroid Thyroid deficiency in the Framingham Study. Arch Intern Med. 1985;145(8):1386–1388. [PubMed] [Google Scholar]
- 34.Parle JV, Franklyn JA, Cross KW, Jones SC, Sheppard MC. Prevalence and follow-up of abnormal thyrotrophin (TSH) concentrations in the elderly in the United Kingdom. Clin Endocrinol (Oxf) 1991;34(1):77–83. doi: 10.1111/j.1365-2265.1991.tb01739.x. [DOI] [PubMed] [Google Scholar]
- 35.Abe E, Marians RC, Yu W, et al. TSH is a negative regulator of skeletal remodeling. Cell. 2003;115(2):151–162. doi: 10.1016/s0092-8674(03)00771-2. [DOI] [PubMed] [Google Scholar]
- 36.Sendak RA, Sampath TK, McPherson JM. Newly reported roles of thyroid-stimulating hormone and follicle-stimulating hormone in bone remodelling. nt Orthop. 2007;31(6):753–757. doi: 10.1007/s00264-007-0417-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mazziotti G, Porcelli T, Patelli I, Vescovi PP, Giustina A. Serum TSH values and risk of vertebral fractures in euthyroid post-menopausal women with low bone mineral density. Bone. 2010;46(3):747–751. doi: 10.1016/j.bone.2009.10.031. [DOI] [PubMed] [Google Scholar]
- 38.Murphy E, Glüer CC, Reid DM, et al. Thyroid function within the upper normal range is associated with reduced bone mineral density and an increased risk of nonvertebral fractures in healthy euthyroid postmenopausal women. J Clin Endocrinol Metab. 2010;95(7):3173–3181. doi: 10.1210/jc.2009-2630. [DOI] [PubMed] [Google Scholar]
- 39.Vestergaard P, Rejnmark L, Mosekilde L. Influence of hyper- and hypothyroidism, and the effects of treatment with antithyroid drugs and levothyroxine on fracture risk. Calcif Tissue Int. 2005;77(3):139–144. doi: 10.1007/s00223-005-0068-x. [DOI] [PubMed] [Google Scholar]
- 40.Poon WT, Ng SW, Lai CK, Chan YW, Mak WL. Factitious thyrotoxicosis and herbal dietary supplement for weight reduction. Clin Toxicol. 2008;46(4):290–292. doi: 10.1080/15563650701381179. [DOI] [PubMed] [Google Scholar]
- 41.U.S. Preventive Services Task Force. Screening for thyroid disease: recommendation statement. Ann Intern Med. 2004;140(2):125–127. doi: 10.7326/0003-4819-140-2-200401200-00014. [DOI] [PubMed] [Google Scholar]
- 42.Sowers M, Luborsky J, Perdue C, Araujo KL, Goldman MB, Harlow SD;SWAN. Thyroid stimulating hormone (TSH) concentrations and menopausal status in women at the mid-life: SWAN. Clin Endocrinol (Oxf) 2003;58(3):340–347. doi: 10.1046/j.1365-2265.2003.01718.x. [DOI] [PubMed] [Google Scholar]
- 43.Benseñor IM, Goulart AC, Lotufo PA, Menezes PR, Scazufca M. Prevalence of thyroid disorders among older people: results from the São Paulo Ageing & Health Study. Cad Saude Publica. 2011;27(1):155–161. doi: 10.1590/s0102-311x2011000100016. [DOI] [PubMed] [Google Scholar]
- 44.Petersen K, Lindstedt G, Lundberg PA, Bengtsson C, Lapidus L, Nyström E. Thyroid disease in middle-aged and elderly Swedish women: thyroid-related hormones, thyroid dysfunction and goitre in relation to age and smoking. J Intern Med. 1991;229(5):407–413. doi: 10.1111/j.1365-2796.1991.tb00367.x. [DOI] [PubMed] [Google Scholar]


