Abstract
Background
The effect of language acculturation, socioeconomic status (SES), and immigrant generation on development of diabetes among Mexican Americans was evaluated in the Hispanic Established Population for the Epidemiologic Study of the Elderly (HEPESE).
Methods
HEPESE is a longitudinal cohort study of 3,050 non-institutionalized Mexican Americans aged 65 years at baseline (1993–1994) from 5 Southwestern states. Diabetes incidence was ascertained in 4 follow-up surveys to 2004–05 by respondent self-reported physician-diagnosis of diabetes, high blood glucose, or sugar in the urine. Language of interview, immigrant generation, gender, age, education, family history of diabetes, smoking status, alcohol use, health insurance type and self-reported height and weight were assessed. High socioeconomic status (SES) was defined by high school graduation and non-Medicaid insurance. Cox's proportional hazards models were fit to evaluate the effects of language acculturation, generation and SES on incident diabetes.
Results
845 of 3,050 (27.7%) Mexican Americans had diabetes at baseline and were younger, more educated, and more likely to have health insurance than those without diabetes. Risk of developing diabetes increased for Spanish-speaking respondents with low SES from 1st to 3rd generation (HR = 1.76, 95% CI = 1.02–3.03) and from 2nd to 3rd generation (HR = 2.15, 95% CI = 1.20–3.84). Among English-speaking, high SES participants, generation had a protective effect on developing diabetes: HR = 0.45 (95% CI = 0.22–0.91) when comparing 3rd versus 1st generation
Conclusion
The effect of language acculturation and immigrant generation on incident diabetes is moderated by SES status in HEPESE participants.
Keywords: acculturation, diabetes, Mexican Americans
Introduction
Diabetes is increasing in the US and in countries that are the biggest contributors of immigrants to the US such as Mexico (Villalpando S et al., 2010, Yang et al., 2010, Soria et al., 2009). Mexican immigrants to the US may provide a unique opportunity for studying the effect of immigration on incident diabetes especially considering their possible genetic predisposition (Gardner et al., 1984, Stern et al., 1991, Elbein, 2009, Haffner, 1998). Immigrants experience rapid change in exposures providing an efficient way to study the impact of migration and environmental change on the rate of diabetes. The foreign-born population in the US has increased at rate six times faster than the native population (Malone et al., 2003), and demographic projections indicate that 87% of the population growth to 2050 will be driven by immigrants and their children (Passel and Cohn, 2008).
It has been well documented that immigrants arrive in the US with a health advantage despite generally adverse social and economic factors. Although this observation was originally developed from studies of Latinos (Markides and Coreil, 1986), it has also been shown to apply to other immigrant groups (Singh and Siahpush, 2002). The most likely explanation for this immigrant health advantage is that immigrants may compose a selected group who are healthier than their counterparts who stay in the country of origin (Marmot et al., 1984). Another possible explanation is that the cultural orientation immigrants bring to the US is protective and provides a buffer from adverse health outcomes. It has been suggested that the protective culture of immigrants encourages healthy behaviors and strong social support systems, facilitates access to health information and health systems, and reinforces positive health norms (Cattell, 2001, Kawachi, 2000). For example, evidence suggests that the body mass index (BMI) of recent immigrants is lower, when compared to US natives (Antecol and Bedard, 2006, Oza-Frank and Cunningham) and other studies show higher fruit and vegetable intake (Ayala et al., 2008) and more frequent non-leisure time physical activity (Afable-Munsuz et al., 2010) among immigrants relative to US born. However, the predominant paradigm is that this initial health advantage is thought to erode over time and acculturation leads to adopting the unhealthy behaviors of the host country population leading to more chronic disease (Antecol and Bedard, 2006).
Mexico is the largest contributor of immigrants to the US (Grieco, 2009), and has recently experienced rapid increases in both obesity and doubling of diabetes rate (Aguilar-Salinas et al., 2003, Jimenez-Cruz and Bacardi-Gascon, 2004, Rivera et al., 2002). This pattern is common in middle-income countries undergoing rapid urbanization leading to more sedentary lifestyles and greater consumption of processed foods and higher total energy intake, a process that has been labeled the “nutrition transition” (Popkin, 2004, Rivera et al., 2004). In the US, it is well known that relative to non-Latino Whites, Latinos and those of Mexican-origin in particular, bear a disproportionate burden of diabetes (Hamman et al., 1989, Flegal et al., 1991, Harris et al., 1998, Cowie et al., 2010, Stern et al., 1983). There has been interest in understanding whether acculturation to US lifestyles contributes to the heightened diabetes risk experienced by Mexican Americans. The evidence on whether the risk of diabetes in Latino immigrant populations increases with greater time in the US or with increased acculturation, however, is equivocal (Afable-Munsuz A et al., 2012, Oza-Frank et al., 2009b, Ahmed et al., 2009, Hazuda et al., 1988, Kandula et al., 2008, Mainous et al., 2006).
We considered the theoretical model of segmented assimilation and postulated that divergent assimilation paths may manifest in different diabetes risks. Segmented assimilation theory views immigrant generation as a central variable conceptualized broadly as a time dimension reflecting increasing exposure to US social and cultural norms (Portes and Zhou, 1993). The length of residence in the US may lead to the progressive narrowing of socioeconomic differences with the native-born population, and gradual adoption of the traits of the host culture with a loss of those from their home country (Alba and Nee, 1997). However, segmented assimilation theory proposes more diverse paths of incorporation into US society with one path characterized by economic advancement with deliberate preservation of the immigrant community's values and traditions. An alternative path of downward assimilation leads to greater identification with a minority subculture and increasing poverty (Portes and Zhou, 1993). Thus the central concepts of segmented assimilation theory are: 1) that the assimilation pattern of immigrants is dependent on which segment of the society they adapt to; and 2) that assimilation involves both cultural change or what health researchers often refer to as acculturation as well as a process of social mobility (both upward, achieving greater affluence or downward, stagnating in poverty).
Following previous work and those of others (Afable-Munsuz et al., 2010, Finch et al., 2007, Nagasawa et al., 2001), we asked whether differences in language acculturation and socioeconomic status (SES) might lead to differential risks for diabetes from first to third generations. First, we aimed to describe patterns of diabetes risk across generations among immigrants who preserve their tradition, as indicated by Spanish language preference. We expected that diabetes risk is lower in second and third generations, relative to immigrants, an observation that would be consistent with the notion that immigrant culture is protective. Second, we examined whether SES confounds observed language acculturation patterns in diabetes risk from first to third generations. Third, if SES confounds observed patterns described above, we aimed to examine the interactive influences of SES, language preference and immigrant generation on diabetes risk. These questions are motivated in part by previous commentaries that have proposed that SES confounds the relationship between language measures of acculturation and health (Hunt et al., 2004). Given that segments of society are likely to have different lifestyle patterns we expect that health behaviors of poor immigrants will differ from those of more affluent immigrants because opportunities and norms for major risk factors for diabetes are likely to differ. We examined these hypotheses and questions using data from a large population-based cohort study representative of aging Mexican-origin adults living in the southwestern US.
Materials and Methods
The Hispanic Established Population for the Epidemiologic Study of the Elderly (HEPESE) is a longitudinal cohort study of 3,050 non-institutionalized Mexican Americans aged 65 years and older at baseline (1993–1994) from five Southwestern states: Texas, California, Colorado, New Mexico, and Arizona.(Markides et al., 1996) The HEPESE participants are representative of approximately 500,000 older Mexican Americans over these five states. The baseline sample was selected using an area probability sample design involving a list of counties in the Southwestern states that contained approximately 90% of Mexican Americans residing in these states (Markides et al., 1996). The first follow-up of the baseline data (1995–1996) followed 2,438 of the original 3,050 respondents and the second follow-up (1998–99) followed 1,980 of these respondents. The third follow-up (2000–2001) followed 1,682 of the original respondents and the fourth follow-up (2004–2005) followed 1,167 of these respondents. Interviews were conducted in English and Spanish, depending on the participants' preference.
Diabetes ascertainment
Respondents were coded as having diabetes if they reported one of three criteria: told by a physician that they had definite diabetes, that they had sugar in their urine, or that they had a test showing high blood glucose. If respondents reported having diabetes they were also probed for month and year of diagnosis. We also included participants who were told by a physician that they had borderline diabetes. At the time of the baseline survey diabetes was defined by fasting blood glucose of ≥140 mg/dl and this subsequently decreased to ≥126 mg/dl (Diabetes Care, 1997). Because all participants were 65 years of age or older, we assumed that all diabetes was type 2 and refer to all as diabetes. Participants, who did not report diabetes at baseline, were classified as having incident diabetes in follow-up or as being censored; time to diabetes/censorship was recorded as age (in years) of the participant at diabetes diagnosis.
Acculturation and immigrant generation
Given that language preference is a powerful component of ethnic identity (Giles and Johnson, 1987, Tong et al., 1999), language of interview (English vs. Spanish) was assessed as a measure of acculturation to US society. Generation was assessed based on information on the respondent's and respondent's parents nativity. A foreign-born respondent was classified as a first-generation immigrant; a US-born respondent with at least one foreign-born parent was classified as second-generation; if the respondent and both parents were born in the US, he/she was classified as third-generation (Afable-Munsuz et al., 2010).
Other Factors and Socioeconomic Status
Demographic variables included gender, age and marital status (married or not). Family history was assessed based on whether parents have/had diabetes (yes/no). Other measures at baseline were selected according to their potential association with acculturation and because they were thought to be potential confounders or mediators on the causal pathway between acculturation and diabetes risk (Baron and Kenny, 1986). These included Body Mass Index (BMI) calculated from self-reported weight and height and categorized as 25 or less, >25 to 30, and > 30 kg/m2; educational attainment categorized as no high school, high school graduate, and college or more; any current consumption of alcoholic beverages (yes/no); ever smoker of cigarettes (yes/no) (Baliunas et al., 2009, Willi et al., 2007); and type of health insurance (no insurance, private insurance, Medicare, and Medicaid).
We operationalized socioeconomic status (SES) using the educational attainment and health insurance variables as a proxy of income/wealth. Participants with high school graduation or more years of education and with private or Medicare insurance were considered of high SES. Persons who 1) did not graduate from high school, or 2) had no insurance, or 3) had Medicaid insurance (in combination with Medicare or not) were categorized as low SES.
Data Analysis
Descriptive statistics detailing demographics and diabetes were generated for the aggregate study population and for the diabetes and the non-diabetes group respectively at the baseline. Chi-square tests and t-tests were computed to assess differences in covariate distributions across groups. Data management and all SAS procedures for statistical analyses were performed with SAS 9.22.(SAS Institute, 2002–2003) Statistical significance throughout was defined p< 0.05. All analyses were adjusted for HEPESE complex survey design.
To examine our hypotheses, plots of diabetes survival functions, adjusted for covariates, were explored to visually provide information on the interactive effects of generation, language of interview and socioeconomic status. We divided the sample into low acculturation (Spanish language interview) vs. high acculturation (English language interview) and into low SES vs. high SES. We then plotted adjusted diabetes survival curves by immigrant generation for each of these four groups. We modeled time free from diabetes (survival) based on retaining Spanish language across generations (from 1st to 3rd). As a comparison, we also modeled time free from diabetes by generation among those who had an English language interview. To examine whether socioeconomic status moderates the relationship between language acculturation and diabetes risk across first to third generations, we stratified analyses by SES so that the effect of language and generation on incident diabetes was estimated within each SES stratum.
Because 19% of cases were missing responses for family history of diabetes, 20 multiply imputed datasets were generated for the analyses predicting incident diabetes. All potential predictor and outcome variables were included in the imputation model. To reflect the differences by language preference, separate imputations were performed and recombined into a single dataset after excluding the participants whose diabetes was diagnosed prior to the baseline survey. All parameter estimates, standard errors and significance tests were estimated by combining results across the imputed data sets (Allison, 2002).
To investigate the relation between generation, language acculturation, socioeconomic status and time to incident diabetes in the population, Cox's proportional hazards models were fit (Allison, 1996). After selecting the main effects, candidate interactions such as language of interview by generation, and socioeconomic status by generation, were investigated, and then tested using Wald chi-square tests. To account for the cases of interval censoring, the PHREG procedure was specified with exact method for tied event times (Klein and Moeschberger, 2003).
Results
At baseline the 3,050 participants had a mean age of 73 years, 57% were women, 89% had not graduated from high school and nearly 73% responded to the interview in Spanish. There were 690 persons with definite diabetes and 155 with borderline diabetes for total of 845 or 27.7% with diabetes at the baseline interview. The baseline characteristics of the sample stratified by diabetes prevalence are presented in Table 1. Persons with diagnosed diabetes were younger, had more education, were more likely to have health insurance, and were more likely to be second generation immigrants but less likely to be first or third generation immigrants in comparison with those who did not have diabetes at the baseline. Those who reported diabetes also had higher BMI (Mean BMI 28.8 vs. 27.5; p<0.01); were more likely to have a family history of diabetes (32.6 % vs. 12.1%; p<0.01) and were more likely to be not consuming any alcohol.
Table 1.
Characteristics of Baseline Sample by Diabetes Prevalence, Mexican Americans in Southwestern US, HEPESE, 1993–1994
| Total N=3050 | Diabetes N=845 | No Diabetes N=2205 | P valuea | |
|---|---|---|---|---|
|
| ||||
| Age | ||||
| 65–74 | 65.6 | 71.2 | 63.5 | |
| 75–84 | 27.3 | 23.9 | 28.6 | <.0001 |
| 85 or older | 7.1 | 4.9 | 7.9 | |
|
| ||||
| Gender | ||||
| Men | 42.4 | 43.1 | 42.1 | 0.620 |
| Women | 57.6 | 56.9 | 57.9 | |
|
| ||||
| State | ||||
| Arizona | 3.6 | 3.4 | 3.7 | |
| California | 27.2 | 26.8 | 27.3 | |
| Colorado | 2.3 | 2.1 | 2.4 | 0.210 |
| New Mexico | 3.6 | 2.4 | 4.0 | |
| Texas | 63.3 | 65.3 | 62.6 | |
|
| ||||
| Generation | ||||
| Third | 13.8 | 12.7 | 14.2 | |
| Second | 41.6 | 45.5 | 40.1 | 0.025 |
| First (Mexico born) | 44.6 | 41.8 | 45.7 | |
|
| ||||
| Language of interview | ||||
| English | 22.2 | 21.7 | 22.4 | 0.676 |
| Spanish | 77.8 | 78.3 | 77.6 | |
|
| ||||
| Education | ||||
| Less than high school | 90.0 | 89.4 | 90.3 | |
| High school graduate | 6.9 | 7.2 | 6.8 | 0.712 |
| Some college or more | 3.1 | 3.5 | 3.0 | |
|
| ||||
| Insurance | ||||
| No insurance | 7.7 | 5.7 | 8.5 | |
| Private & Medicare | 16.6 | 16.8 | 16.5 | 0.0003 |
| Medicare only | 40.7 | 37.2 | 42.0 | |
| Medicare & Medicaid | 35.1 | 40.4 | 33.0 | |
|
| ||||
| Ever Smoked at baseline | ||||
| Yes | 41.6 | 39.8 | 42.2 | 0.224 |
|
| ||||
| Used alcohol at baseline | ||||
| Yes | 15.6 | 9.3 | 18.0 | <0.0001 |
| No | 84.4 | 90.7 | 82.0 | |
|
| ||||
| Body mass Index (kg/m2) b | 0.002 | |||
| ≤25 | 37.2 | 33.5 | 38.6 | |
| <25 to ≤30 | 36.2 | 35.7 | 36.4 | |
| >30 | 26.6 | 30.8 | 25.0 | |
|
| ||||
| Family history of diabetes c | ||||
| Yes | 17.1 | 30.6 | 12.4 | <0.0001 |
| No | 82.9 | 69.4 | 87.6 | |
|
| ||||
| Total sample size (N) | 3050 | 845 | 2205 | |
chi-square test for categorical variables;
excludes 281 missing cases;
excludes 591 missing cases
Immigrant Generation and Language of Interview
Diabetes was most prevalent in second generation, followed by third and first generation Mexican Americans (30.3%, 26.4% and 24.9%; p <0.05). There was no significant difference in diabetes prevalence by language of interview. The educational levels increased with each generation, with third generation Mexican Americans being most likely to have a high school diploma or some level of college education, when compared with previous immigrant generations (5.4% vs. 12.7% vs. 16.1%, p<0.05). Those who preferred English as the language of interview had higher education levels in comparison to those who responded in Spanish (22.2% vs. 6.5%. p<0.05). First generation Mexican Americans and those who responded in Spanish as a language of interview were most likely to be uninsured, while third generation Mexican Americans and those who responded in English as a language for interview were more likely to have both private and Medicare health insurance. Use of Spanish as a language of interview decreased in each subsequent generation from first to third: 88.2%, 66.1%, and 40.6%, respectively (p<0.05).
Time Without Diabetes after Baseline
Table 2 shows the respondents in each of the four HEPESE follow-surveys with the new cases of definite and borderline diabetes by year of survey. Cumulative rate of diabetes increased with each follow-up survey, but the proportions responding in Spanish, and of low SES did not vary significantly.
Table 2.
Follow-up Surveys and Diabetes Status among Mexican Americans, HEPESE 1993–2005
| 1995–96 | 1998–99 | 2000–01 | 2004–05 | |
|---|---|---|---|---|
|
| ||||
| Total sample size (N) | 2438 | 1980 | 1682 | 1167 |
|
| ||||
| Gender | ||||
| Men (%) | 41.6 | 40.4 | 38.6 | 36.9 |
| Women (%) | 58.4 | 59.7 | 61.4 | 63.2 |
|
| ||||
| Language | ||||
| Spanish (%) | 78.7 | 78.7 | 78.0 | 79.7 |
| English (%) | 21.3 | 21.3 | 22.0 | 20.3 |
|
| ||||
| Generation | ||||
| 1st Generation (%) | 45.3 | 43.9 | 42.9 | 44.2 |
| 2nd Generation (%) | 40.9 | 42.6 | 44.2 | 44.5 |
| 3rd Generation (%) | 13.9 | 13.5 | 12.9 | 11.3 |
|
| ||||
| Socioeconomic status | ||||
| Low SES (%) | 39.6 | 38.7 | 38.4 | 38.1 |
| High SES (%) | 60.4 | 61.3 | 61.6 | 61.9 |
|
| ||||
| Diabetes status | ||||
| New DM (N) | 126 | 81 | 58 | 56 |
| New definitive diabetes (N) | 91 | 64 | 44 | 56 |
| New borderline diabetes (N) | 35 | 17 | 14 | n/a** |
Among 845 participants who diagnosed diabetes at the baseline, 155 is the number of borderline and 690 is the number of definite.
Have you ever been told by a doctor that you have diabetes, sugar in your urine, or high blood sugar? (no longer have a borderline category)
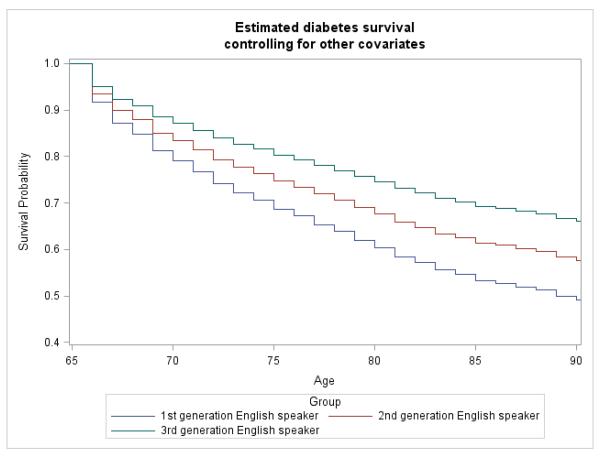
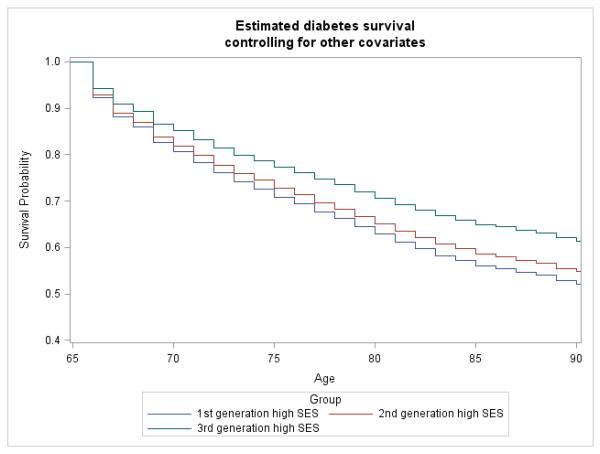
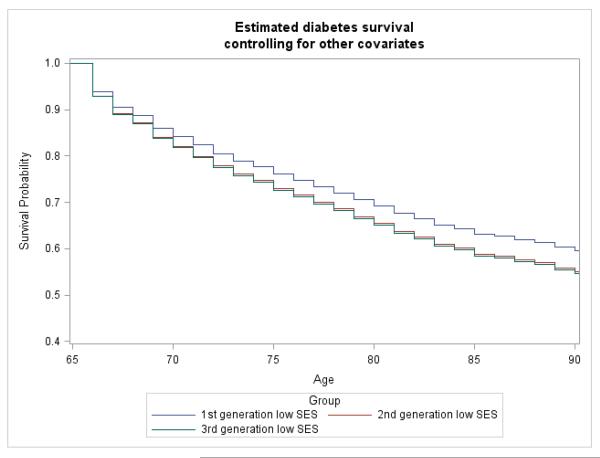
Plots of survival curve functions provided visual interpretation on the interactive effects of generation and SES or language of interview on the effect of time without diabetes in follow-up interviews. Figures 1a and 1b and 2a and 2b show the adjusted probability of being diabetes-free among four groups stratified by immigrant generation: low language acculturation, high language acculturation, higher SES and lower SES. In Figure 1a, for example, among respondents classified as low language acculturation (Spanish language interview), the probability of remaining diabetes-free decreases with increasing generation. In contrast, among the more acculturated respondents (English language interview), we observed an opposite trend where the probability of remaining diabetes-free increases from first to third generation (Figure 1b). Figures 2a and 2b assess potential confounding between language acculturation and SES, with plotted survival curves (time diabetes-free) among low vs. high SES respondents. We found a pattern among high SES respondents similar to that among high language acculturation respondents where time free from diabetes increases with increasing generation (Figure 2a). However, among low SES individuals, time free from diabetes is lower in 2nd and 3rd generations relative to 1st generation (Figure 2b).
Figure 1a.
Estimated Time without Diabetes (Survival) for 2,205 Mexican Americans through Three Follow-Up Surveys among those who Interviewed in Spanish by Immigrant Generation, HEPESE, 1993–2005
Figure 1b.
Estimated Time without Diabetes (Survival) for Mexican Americans through Three Follow-Up Surveys among those who Interviewed in English by Immigrant Generation, HEPESE, 1993–2005
Figure 2a.
Estimated Time without Diabetes (Survival) for Mexican Americans through Three Follow-Up Surveys among High Socioeconomic Status (SES) by Immigrant Generation, HEPESE, 1993–2005
Figure 2b.
Estimated Time without Diabetes (Survival) for Mexican Americans through Three Follow-Up Surveys among Low Socioeconomic Status (SES) by Immigrant Generation, HEPESE, 1993–2005
Predictors of Incident Diabetes
Table 3 shows the results of adjusted hazard ratios for developing new diabetes (definite plus borderline) during the follow-up period. Third generation immigrants who responded in English and had higher SES had lower risk of developing diabetes compared to their first-generation counterparts, and even comparison of second to first generations had borderline statistical significance (Table 3). Among English speaking lower SES respondents, the adjusted risk was also significantly lower for second compared to first generation immigrants, but not for other comparisons across generations. Maintaining Spanish as the primary language did not affect diabetes risk among higher SES respondents from first to third generations. However, among respondents who maintain Spanish and were of lower SES, there was a significantly higher risk of diabetes among third generation immigrants compared to second or first generation Mexican Americans. BMI greater than 30 kg/m2 and parental history of diabetes was significantly associated with developing diabetes as would be expected.
Table 3.
Risk of Developing Diabetes by Language Acculturation, Immigrant Generation and Socioeconomic Status in Follow-up Surveys, Mexican Americans HEPESE 1992–2005
| Hazard Ratio | 95% CI | P-value | |
|---|---|---|---|
|
| |||
| English and High SES | |||
| Generation: 2nd vs. 1st | 0.57 | 0.31–1.02 | 0.06 |
| Generation: 3rd vs. 1st | 0.45 | 0.22–0.91 | 0.03 |
| Generation: 3rd vs. 2nd | 0.79 | 0.42–1.51 | 0.48 |
|
| |||
| English and Low SES | |||
| Generation: 2nd vs. 1st | 0.47 | 0.23–0.96 | 0.04 |
| Generation: 3rd vs. 1st | 0.84 | 0.38–1.88 | 0.68 |
| Generation: 3rd vs. 2nd | 1.79 | 0.81–3.96 | 0.15 |
|
| |||
| Spanish and High SES | |||
| Generation: 2nd vs. 1st | 0.99 | 0.72–1.36 | 0.95 |
| Generation: 3rd vs. 2nd | 0.94 | 0.56–1.59 | 0.82 |
| Generation: 3rd vs. 2nd | 0.95 | 0.56–1.61 | 0.85 |
|
| |||
| Spanish and Low SES | |||
| Generation: 2nd vs. 1st | 0.82 | 0.53–1.27 | 0.37 |
| Generation: 3rd vs. 1st | 1.76 | 1.02–3.03 | 0.04 |
| Generation: 3rd vs. 2nd | 2.15 | 1.20–3.84 | 0.01 |
|
| |||
| Body Mass Index ≥ 30 kg/m2 | 1.68 | 1.30–2.16 | <0.001 |
|
| |||
| Parental History of Diabetes | 1.39 | 1.02–1.90 | 0.04 |
High SES defined by being a high school graduate and having Medicare or private health insurance
All models adjusted for gender, age, BMI, smoking history, alcohol use and family history of diabetes.
Discussion
The immigrant health advantage is predicted to attenuate or disappear with increasing time living in the US. There is empirical evidence that acculturation has adverse health effects behavioral risk factors such as cigarette smoking and obesity (Oza-Frank et al., 2009a, Antecol and Bedard, 2006) (Pérez-Stable EJ et al., 2001); (Kaplan MS et al., 2004) as well as increased risk of diabetes (Oza-Frank et al, 2012). Our findings highlight the importance of consideration of socioeconomic status when interpreting the relationships between language acculturation, immigrant generation and incident diabetes risk. Our findings provide empirical support for the idea that the effects of acculturation on health outcomes are dependent on the segment of society to which the immigrant group adapts, a key theme of segmented assimilation theory. The idea that assimilation's association with health might be moderated or influenced by socioeconomic status has been studied previously with regard to obesity.(Sanchez-Vaznaugh et al., 2008, Kaushal, 2009) This is one of the only studies that have evaluated inter-related influences of SES, language acculturation and immigrant generation on the development of a major health outcome: incident diabetes in a high-risk population.
In this study, we do not find evidence that preservation on immigrant culture, measured by Spanish language preference, was protective against developing diabetes. On the contrary, we observed a tendency to increasing diabetes risk from first to third generation among participants interviewed in Spanish that was only statistically significant among participants of lower SES. This would potentially imply that behavioral or environmental exposures among less acculturated second and third generation Mexican immigrants increase risk of developing diabetes. Furthermore, we observed that among those who responded in English to the interview, there was a lower subsequent risk of incident diabetes in the second and third generation HEPESE participants. This protective effect from diabetes among English responding, higher SES participants, however, was absent in English interviewed participants of lower SES. Overall evidence on the divergent relationships between language acculturation and immigrant generation and diabetes risk is consistent with past studies on obesity, which have found a higher obesity risk in adults with increasing years in the US and low SES but no association among higher SES individuals by years in the US (Sanchez-Vaznaugh et al., 2008, Kaushal, 2009). These data provide some support for the “unhealthy assimilation” perspective for those with low levels of language acculturation and lower levels of SES and these findings are consistent with past studies on immigrant generation and diabetes risk (Ahmed et al., 2009, Oza-Frank et al., 2009b).
Despite the known higher risk of diabetes among Mexican Americans, the HEPESE offered an opportunity to expand on this knowledge by identifying possible contributions of SES, immigrant generation and language acculturation in the development of incident diabetes in this population in a prospective cohort. Previous studies of diabetes in HEPESE participants have focused on cross-sectional analyses and incidence of cardiovascular complications among those identified as having diabetes, but none had evaluated risk factors for developing incident diabetes (Beard HA et al., 2009); (Black SA et al., 1999).
Our study has important limitations. First, we do not have laboratory measures to further define diabetes risk among those without reported diabetes at baseline. In our study, diabetes is based on self-report only so it is possible that this study under-estimated prevalence at baseline and incidence in subsequent surveys (Margolis et al., 2008). Over this time period awareness and detection of pre-diabetes and diabetes has increased and thus differential use of health services by language preference and immigrant generation may lead to differences in undiagnosed diabetes rates. By including persons with self-reported “borderline” diabetes we do partially address the under-diagnosis problem. Second, because we have a cross-section of different immigrant generations in our study, each generation may come from a different migration cohort, and thus have a different migration experience (Antecol and Bedard, 2006). Third, first generation immigrants compared to US-born participants in our study may come from different ancestral and regional groups in Mexico, who are diverse in genetic admixture (Gonzalez Burchard et al., 2005, Martinez-Marignac et al., 2007) and social characteristics, and as a result, potentially vary in diabetes risk (Barquera et al., 2003). Family inter-generational studies and prospective cohort studies of new immigrants followed at regular intervals would allow us to control for heterogeneity by place of origin and to study adaptation over time (Jasso et al., 2000). Fourth, our measure of acculturation was a one-item proxy language of interview that performed as well as the longer language-based scale included in HEPESE. Although acculturation is a complex process, it remains unclear whether more extensive measures add explanatory power over the shorter scales or even one-item language proxies in health studies (Alegria, 2009). Finally, HEPESE did not collect complete physical activity or dietary measures. Thus, we were unable to examine the potential role these factors played in the relationship between acculturation, generation, SES and development of diabetes.
Relationships between assimilation, acculturation and health are complex (Markides, 2001) and both negative and positive associations between assimilation, acculturation indicators and diabetes and its risk factors have been observed. (Mainous et al., 2006, Ahmed et al., 2009, Ayala et al., 2008, Oza-Frank et al., 2009b, Lara et al., 2005, Afable-Munsuz et al., 2010, Hazuda et al., 1988, Kandula et al., 2008, Antecol and Bedard, 2006). This is not surprising given the heterogeneity of acculturation and assimilation processes in US immigrants as described by scholars of migration (Portes and Zhou, 1993). Our study suggests that the effects of acculturation on health are not uniform among Mexican Americans and are modified by SES and possibly explained by assimilation pattern. We found divergent associations between immigrant generation and diabetes risk. On the one hand, we add to the evidence that increased exposure to the US environment leads to higher risk of diabetes in immigrants to the US who remain predominantly Spanish speaking and are of lower SES background. But the study also demonstrates that this pattern does not apply to all segments of the population studied and that higher SES individuals may benefit from increased exposure to the US to the point of having a decreased risk of developing diabetes. Thus in these data increased acculturation as measured by language preference was protective from developing incident diabetes among higher SES Mexican Americans. This would be evidence that increased acculturation may actually be good for health in selected situations.
Our findings suggest the need to examine more closely the causal mechanisms linking acculturation to health and suggest that such examinations would benefit when considering the socioeconomic changes occurring as immigrants assimilate to US society. Because upward social mobility affords wider access and range of opportunities for different lifestyle options we also argue that need to examine more closely the environmental and lifestyle changes occurring among immigrants.
These findings can be applied to advance the health of older Mexican Americans by intensifying efforts to increase access to education for all immigrants given that more education can facilitate upward social mobility and better health. Public health education also needs to be directed at Spanish speaking Latinos with low levels of education so they eat healthier food, increase leisure time physical activity and do not gain excess weight. Overall, we need to intensify prevention efforts among Latinos of low SES especially in second and subsequent generations in the US.
Table 4.
Risk of Developing Diabetes by Language Acculturation, Immigrant Generation and Socioeconomic Status in Follow-up Surveys, Mexican Americans HEPESE 1992–2005
| Hazard Ratio | 95% CI | P-value | |
|---|---|---|---|
|
| |||
| English and High SES | |||
| Generation: 2nd vs. 1st | 0.57 | 0.31–1.02 | 0.06 |
| Generation: 3rd vs. 1st | 0.45 | 0.22–0.91 | 0.03 |
| Generation: 3rd vs. 2nd | 0.79 | 0.42–1.51 | 0.48 |
|
| |||
| English and Low SES | |||
| Generation: 2nd vs 1st | 0.47 | 0.23–0.96 | 0.04 |
| Generation: 3rd vs 1st | 0.84 | 0.38–1.88 | 0.68 |
| Generation: 3rd vs. 2nd | 1.79 | 0.81–3.96 | 0.15 |
|
| |||
| Spanish and High SES | |||
| Generation: 2nd vs 1st | 0.99 | 0.72–1.36 | 0.95 |
| Generation: 3rd vs. 2nd | 0.94 | 0.56–1.59 | 0.82 |
| Generation: 3rd vs. 2nd | 0.95 | 0.56–1.61 | 0.85 |
|
| |||
| Spanish and Low SES | |||
| Generation: 2nd vs 1st | 0.82 | 0.53–1.27 | 0.37 |
| Generation: 3rd vs 1st | 1.76 | 1.02–3.03 | 0.04 |
| Generation: 3rd vs 2nd | 2.15 | 1.20–3.84 | 0.01 |
|
| |||
| Body Mass Index ≥ 30 kg/m2 | 1.68 | 1.30–2.16 | <0.001 |
|
| |||
| Parental History of Diabetes | 1.39 | 1.02–1.90 | 0.04 |
High SES defined by being a high school graduate or having Medicare or private health insurance
Acknowledgements
This study was supported by Grant P30-AG15272 under the Resource Centers for Minority Aging Research program by the National Institute on Aging, National Institutes of Health. Dr. Afable-Munsuz received a Diversity Supplement to this grant. We thank Juliette Hong, MS for conducting data analyses.
References
- Centers for Disease Control and Prevention, National Center for Health Statistics, Division of Health Interview Statistics, data from the National Health Interview Survey Statistical analysis by the Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Division of Diabetes Translation. Accessed on Nov. 5, 2010. http://www.cdc.gov/diabetes/statistics/prev/national/figage.htm. [Online]
- AFABLE-MUNSUZ A, MAYEDA ER, PÉREZ-STABLE EJ, MN H. Immigrant generation and diabetes risk among Mexican Americans: Evidence from SALSA (Sacramento Area Latino Study on Aging) American Journal of Public Health. 2013;103:e45–e52. doi: 10.2105/AJPH.2012.300969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- AFABLE-MUNSUZ A, PONCE N, PEREZ-STABLE E, RODRIGUEZ M. Immigrant generation and physical activity among Mexican, Chinese and Filipino adults in the U.S. Soc Sci Med. 2010;70:1997–2005. doi: 10.1016/j.socscimed.2010.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- AGUILAR-SALINAS CA, VELAZQUEZ MONROY O, GOMEZ-PEREZ FJ, GONZALEZ CHAVEZ A, ESQUEDA AL, MOLINA CUEVAS V, RULL-RODRIGO JA, TAPIA CONYER R. Characteristics of patients with type 2 diabetes in Mexico: Results from a large population-based nationwide survey. Diabetes Care. 2003;26:2021–6. doi: 10.2337/diacare.26.7.2021. [DOI] [PubMed] [Google Scholar]
- AHMED AT, QUINN VP, CAAN B, STERNFELD B, HAQUE R, VAN DEN EEDEN SK. Generational status and duration of residence predict diabetes prevalence among Latinos: the California Men's Health Study. BMC Public Health. 2009;9:392. doi: 10.1186/1471-2458-9-392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ALBA R, NEE V. Rethinking assimilation theory for a new era of immigration. Int Migr Rev. 1997;31:826–74. [PubMed] [Google Scholar]
- ALEGRIA M. The challenge of acculturation measures: what are we missing? A commentary on Thomson & Hoffman-Goetz. Soc Sci Med. 2009;69:996–8. doi: 10.1016/j.socscimed.2009.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ALLISON A. Missing Data. Sage; Thousand Oaks, CA: 2002. [Google Scholar]
- ALLISON P. Survival Analysis Using SAS®: A Practical Guide. SAS Institute Inc.; Cary, NC: 1996. [Google Scholar]
- ANTECOL H, BEDARD K. Unhealthy assimilation: Do immigrants converge to American health status levels? Demography. 2006;43:337–360. doi: 10.1353/dem.2006.0011. [DOI] [PubMed] [Google Scholar]
- AYALA GX, BAQUERO B, KLINGER S. A systematic review of the relationship between acculturation and diet among Latinos in the United States: implications for future research. J Am Diet Assoc. 2008;108:1330–44. doi: 10.1016/j.jada.2008.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BALIUNAS DO, TAYLOR BJ, IRVING H, ROERECKE M, PATRA J, MOHAPATRA S, REHM J. Alcohol as a risk factor for type 2 diabetes: A systematic review and meta-analysis. Diabetes Care. 2009;32:2123–32. doi: 10.2337/dc09-0227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BARON RM, KENNY DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–82. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- BARQUERA S, TOVAR-GUZMAN V, CAMPOS-NONATO I, GONZALEZ-VILLALPANDO C, RIVERA-DOMMARCO J. Geography of diabetes mellitus mortality in Mexico: an epidemiologic transition analysis. Arch Med Res. 2003;34:407–14. doi: 10.1016/S0188-4409(03)00075-4. [DOI] [PubMed] [Google Scholar]
- BEARD HA, ALGHATRIF M, SAMPER-TERNENT R, GERST K, KS M. Trends in diabetes prevalence and diabetes-related complications in older Mexican Americans from 1993–1994 to 2004–2005. Diabetes Care. 2009;32:2212–2217. doi: 10.2337/dc09-0938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BLACK SA, RAY LA, MARKIDES KS. The prevalence and health burden of self-reported diabetes in the older Mexican Americans: Findings from the Hispanic EPESE. American Journal of Public Health. 1999;89:546–552. doi: 10.2105/ajph.89.4.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CARLTON J. Hispanics surge in California. Wall Street Journal. 2011 http://online.wsj.com/article/SB10001424052748703662804576189031330152462html?KEYWORDS=JIM+CARLTON. Accessed on March 11, 2011.
- CATTELL V. Poor people, poor places, and poor health: the mediating role of social networks and social capital. Soc Sci Med. 2001;52:1501–16. doi: 10.1016/s0277-9536(00)00259-8. [DOI] [PubMed] [Google Scholar]
- COWIE CC, RUST KF, BYRD-HOLT DD, GREGG EW, FORD ES, GEISS LS, BAINBRIDGE KE, FRADKIN JE. Prevalence of diabetes and high risk for diabetes using A1C criteria in the U.S. population in 1988–2006. Diabetes Care. 2010;33:562–8. doi: 10.2337/dc09-1524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DIABETES CARE. Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 1997;20:1183–1197. doi: 10.2337/diacare.20.7.1183. [DOI] [PubMed] [Google Scholar]
- ELBEIN SC. Genetics factors contributing to type 2 diabetes across ethnicities. J Diabetes Sci Technol. 2009;3:685–9. doi: 10.1177/193229680900300412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FINCH B, LIM N, PEREZ W, PUONG DO D. Toward a population health model of segmented assimilation: The Case of low birth-weight in Los Angeles. Sociological Perspectives. 2007;50:445–468. [Google Scholar]
- FLEGAL KM, EZZATI TM, HARRIS MI, HAYNES SG, JUAREZ RZ, KNOWLER WC, PEREZ-STABLE EJ, STERN MP. Prevalence of diabetes in Mexican Americans, Cubans, and Puerto Ricans from the Hispanic Health and Nutrition Examination Survey, 1982–1984. Diabetes Care. 1991;14:628–38. doi: 10.2337/diacare.14.7.628. [DOI] [PubMed] [Google Scholar]
- GARDNER LI, JR., STERN MP, HAFFNER SM, GASKILL SP, HAZUDA HP, RELETHFORD JH, EIFLER CW. Prevalence of diabetes in Mexican Americans. Relationship to percent of gene pool derived from native American sources. Diabetes. 1984;33:86–92. doi: 10.2337/diab.33.1.86. [DOI] [PubMed] [Google Scholar]
- GILES H, JOHNSON P. Ethnolinguistic identity theory: A social psychological approach to language maintenance. Int J Soc Language. 1987;68:69–100. [Google Scholar]
- GONZALEZ BURCHARD E, BORRELL LN, CHOUDHRY S, NAQVI M, TSAI HJ, RODRIGUEZ-SANTANA JR, CHAPELA R, ROGERS SD, MEI R, RODRIGUEZ-CINTRON W, ARENA JF, KITTLES R, PEREZ-STABLE EJ, ZIV E, RISCH N. Latino populations: a unique opportunity for the study of race, genetics, and social environment in epidemiological research. Am J Public Health. 2005;95:2161–8. doi: 10.2105/AJPH.2005.068668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GRIECO P. American Community Survey Reports, ACS-11. U.S. Census Bureau; Washington, DC: 2009. Race and Hispanic Origin of the Foreign-Born Population in the United States: 2007. [Google Scholar]
- HAFFNER SM. Epidemiology of type 2 diabetes: risk factors. Diabetes Care. 1998;21(Suppl 3):C3–6. doi: 10.2337/diacare.21.3.c3. [DOI] [PubMed] [Google Scholar]
- HAMMAN RF, MARSHALL JA, BAXTER J, KAHN LB, MAYER EJ, ORLEANS M, MURPHY JR, LEZOTTE DC. Methods and prevalence of non-insulin-dependent diabetes mellitus in a biethnic Colorado population. The San Luis Valley Diabetes Study. Am J Epidemiol. 1989;129:295–311. doi: 10.1093/oxfordjournals.aje.a115134. [DOI] [PubMed] [Google Scholar]
- HARRIS MI, FLEGAL KM, COWIE CC, EBERHARDT MS, GOLDSTEIN DE, LITTLE RR, WIEDMEYER HM, BYRD-HOLT DD. Prevalence of diabetes, impaired fasting glucose, and impaired glucose tolerance in U.S. adults. The Third National Health and Nutrition Examination Survey, 1988–1994. Diabetes Care. 1998;21:518–24. doi: 10.2337/diacare.21.4.518. [DOI] [PubMed] [Google Scholar]
- HAZUDA HP, HAFFNER SM, STERN MP, EIFLER CW. Effects of acculturation and socioeconomic status on obesity and diabetes in Mexican Americans. The San Antonio Heart Study. Am J Epidemiol. 1988;128:1289–301. doi: 10.1093/oxfordjournals.aje.a115082. [DOI] [PubMed] [Google Scholar]
- HUNT L, SCHNEIDER S, COMER B. Should “acculturation” be a variable in health research? A critical review of research on US Hispanics. Social Science & Medicine. 2004;59:973–986. doi: 10.1016/j.socscimed.2003.12.009. [DOI] [PubMed] [Google Scholar]
- JASSO G, MASSEY DS, ROSENZWEIG MR, SMITH JP. The New Immigrant Survey Pilot (NIS-P): overview and new findings about U.S. legal immigrants at admission. Demography. 2000;37:127–38. [PubMed] [Google Scholar]
- JIMENEZ-CRUZ A, BACARDI-GASCON M. The fattening burden of type 2 diabetes on Mexicans: projections from early growth to adulthood. Diabetes Care. 2004;27:1213–5. doi: 10.2337/diacare.27.5.1213. [DOI] [PubMed] [Google Scholar]
- KANDULA NR, DIEZ-ROUX AV, CHAN C, DAVIGLUS ML, JACKSON SA, NI H, SCHREINER PJ. Association of acculturation levels and prevalence of diabetes in the multi-ethnic study of atherosclerosis (MESA) Diabetes Care. 2008;31:1621–8. doi: 10.2337/dc07-2182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KAPLAN MS, HUGUET N, NEWSOM JT, BH M. The association between length of residence and obesity among Hispanic immigrants. Am J Prev Med. 2004;27:323–326. doi: 10.1016/j.amepre.2004.07.005. [DOI] [PubMed] [Google Scholar]
- KAUSHAL N. Adversities of acculturation? Prevalence of obesity among immigrants. Health Econ. 2009;18:291–303. doi: 10.1002/hec.1368. [DOI] [PubMed] [Google Scholar]
- KAWACHI I, BERKMAN L. Social Cohesion, Social Capital, and Health. In: BERKMAN L, KAWACHI I, editors. Social Epidemiology. Oxford University Press; Oxford: 2000. [Google Scholar]
- KLEIN J, MOESCHBERGER M. Survival Analysis: Techniques for Censored and Truncated Data. Springer Science+Business Media, Inc.; New York, NY: 2003. [Google Scholar]
- LARA M, GAMBOA C, KAHRAMANIAN M, MORALES L, BAUTISTA D. Acculturation and Latino Health in the Unites States: A Review of the Literature and its Sociopolitical Context. Annu Rev Public Health. 2005;26:367–397. doi: 10.1146/annurev.publhealth.26.021304.144615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MAINOUS AG, 3RD, MAJEED A, KOOPMAN RJ, BAKER R, EVERETT CJ, TILLEY BC, DIAZ VA. Acculturation and diabetes among Hispanics: evidence from the 1999–2002 National Health and Nutrition Examination Survey. Public Health Rep. 2006;121:60–6. doi: 10.1177/003335490612100112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MALONE N, BALUJA K, COSTANZO J, DAVIS C. Census 2000 Brief. U.S. Census Bureau; 2003. The Foreign-Born Population: 2000. [Google Scholar]
- MARGOLIS KL, LIHONG Q, BRZYSKI R, BONDS DE, HOWARD BV, KEMPAINEN S, SIMIN L, ROBINSON JG, SAFFORD MM, TINKER LT, PHILLIPS LS. Validity of diabetes self-reports in the Women's Health Initiative: comparison with medication inventories and fasting glucose measurements. Clin Trials. 2008;5:240–7. doi: 10.1177/1740774508091749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MARKIDES KS. Migration and Health. In: SMELSER MPBANJ, editor. International Encyclopedia of the Social and Behavioral Sciences. Elsevier; New York and Amsterdam: 2001. [Google Scholar]
- MARKIDES KS, COREIL J. The health of Hispanics in the southwestern United States: an epidemiologic paradox. Public Health Rep. 1986;101:253–65. [PMC free article] [PubMed] [Google Scholar]
- MARKIDES KS, STROUP-BENHAM CA, GOODWIN JS, PERKOWSKI LC, LICHTENSTEIN M, RAY LA. The effect of medical conditions on the functional limitations of Mexican-American elderly. Ann Epidemiol. 1996;6:386–91. doi: 10.1016/s1047-2797(96)00061-0. [DOI] [PubMed] [Google Scholar]
- MARMOT MG, ADELSTEIN AM, BULUSU L. Lessons from the study of immigrant mortality. Lancet. 1984;1:1455–7. doi: 10.1016/s0140-6736(84)91943-3. [DOI] [PubMed] [Google Scholar]
- MARTINEZ-MARIGNAC VL, VALLADARES A, CAMERON E, CHAN A, PERERA A, GLOBUS-GOLDBERG R, WACHER N, KUMATE J, MCKEIGUE P, O'DONNELL D, SHRIVER MD, CRUZ M, PARRA EJ. Admixture in Mexico City: implications for admixture mapping of type 2 diabetes genetic risk factors. Hum Genet. 2007;120:807–19. doi: 10.1007/s00439-006-0273-3. [DOI] [PubMed] [Google Scholar]
- NAGASAWA R, QIAN Z, WONG P. Theory of segmented assimilation and the adoption of marijuana use and delinquent behavior by Asian Pacific youth. The Sociological Quarterly. 2001;42:351–372. [Google Scholar]
- OZA-FRANK R, ALI MK, VACCARINO V, NARAYAN KM. Asian Americans: diabetes prevalence across U.S. and World Health Organization weight classifications. Diabetes Care. 2009a;32:1644–6. doi: 10.2337/dc09-0573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OZA-FRANK R, CUNNINGHAM SA. The weight of US residence among immigrants: a systematic review. Obes Rev. 11:271–80. doi: 10.1111/j.1467-789X.2009.00610.x. [DOI] [PubMed] [Google Scholar]
- OZA-FRANK R, STEPHENSON R, VENKAT NARAYAN KM. Diabetes Prevalence by Length of Residence Among US Immigrants. J Immigr Minor Health. 2009b doi: 10.1007/s10903-009-9283-2. [DOI] [PubMed] [Google Scholar]
- OZA-FRANK R, CHAN C, LIU K, BURKE G, KANAYA AM. Incidence of type 2 diabetes by place of birth in the Multi-Ethnic Study of Atherosclerosis. Journal of Immigrant and Minority Health. doi: 10.1007/s10903-012-9683-6. Epub 2012 July 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PASSEL JS, COHN D. U.S. Population Projections: 2005–2050. In: CENTER PR, editor. Social & Demographic Trends. Washington, DC.: 2008. [Google Scholar]
- PÉREZ-STABLE EJ, RAMIREZ A, VILLAREAL R, TALAVERA GA, TRAPIDO E, SUAREZ L MJ, A M. Cigarette smoking behavior among US Latino men and women from different countries of origin. Am J Public Health. 2001;91:1424–1430. doi: 10.2105/ajph.91.9.1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- POPKIN BM. The nutrition transition: an overview of world patterns of change. Nutr Rev. 2004;62:S140–3. doi: 10.1111/j.1753-4887.2004.tb00084.x. [DOI] [PubMed] [Google Scholar]
- PORTES A. The New Second Generation. Russell Sage Foundation; New York: 1996. [Google Scholar]
- PORTES A, ZHOU M. The New Second Generation: Segmented Assimilation and Its Variants. The Annals of the American Academy. 1993;530 [Google Scholar]
- RIVERA JA, BARQUERA S, CAMPIRANO F, CAMPOS I, SAFDIE M, TOVAR V. Epidemiological and nutritional transition in Mexico: rapid increase of non-communicable chronic diseases and obesity. Public Health Nutr. 2002;5:113–22. doi: 10.1079/PHN2001282. [DOI] [PubMed] [Google Scholar]
- RIVERA JA, BARQUERA S, GONZALEZ-COSSIO T, OLAIZ G, SEPULVEDA J. Nutrition transition in Mexico and in other Latin American countries. Nutr Rev. 2004;62:S149–57. doi: 10.1111/j.1753-4887.2004.tb00086.x. [DOI] [PubMed] [Google Scholar]
- SANCHEZ-VAZNAUGH EV, KAWACHI I, SUBRAMANIAN SV, SANCHEZ BN, ACEVEDO-GARCIA D. Differential effect of birthplace and length of residence on body mass index (BMI) by education, gender and race/ethnicity. Soc Sci Med. 2008;67:1300–10. doi: 10.1016/j.socscimed.2008.06.015. [DOI] [PubMed] [Google Scholar]
- SAS INSTITUTE, I . SAS. 9.1.3 ed. SAS Institute; Cary, NC: 2002–2003. [Google Scholar]
- SINGH GK, SIAHPUSH M. Ethnic-immigrant differentials in health behaviors, morbidity, and cause-specific mortality in the United States: an analysis of two national data bases. Hum Biol. 2002;74:83–109. doi: 10.1353/hub.2002.0011. [DOI] [PubMed] [Google Scholar]
- SORIA ML, SY RG, VEGA BS, TY-WILLING T, ABENIR-GALLARDO A, VELANDRIA F, PUNZALAN FE. The incidence of type 2 diabetes mellitus in the Philippines: a 9-year cohort study. Diabetes Res Clin Pract. 2009;86:130–3. doi: 10.1016/j.diabres.2009.07.014. [DOI] [PubMed] [Google Scholar]
- STERN MP, GASKILL SP, HAZUDA HP, GARDNER LI, HAFFNER SM. Does obesity explain excess prevalence of diabetes among Mexican Americans? Results of the San Antonio Heart Study. Diabetologia. 1983;24:272–7. doi: 10.1007/BF00282712. [DOI] [PubMed] [Google Scholar]
- STERN MP, KNAPP JA, HAZUDA HP, HAFFNER SM, PATTERSON JK, MITCHELL BD. Genetic and environmental determinants of type II diabetes in Mexican Americans. Is there a “descending limb” to the modernization/diabetes relationship? Diabetes Care. 1991;14:649–54. doi: 10.2337/diacare.14.7.649. [DOI] [PubMed] [Google Scholar]
- TONG Y, HONG Y, LEE S, AL E. Language use as a carrier of social identity. Int J Intercultural Relations. 1999;23:281–96. [Google Scholar]
- VILLALPANDO S, ROJAS R, SHAMAH-LEVY T, ÁVILA MA, GAONA B, DE LA CRUZ V, REBOLLAR R, L. HN. Prevalence and distribution of type 2 Diabetes mellitus in Mexican adult population.A probabilistic survey. Salud Publica Mex. 2010;52:S19–S26. doi: 10.1590/s0036-36342010000700005. [DOI] [PubMed] [Google Scholar]
- WILLI C, BODENMANN P, GHALI WA, FARIS PD, CORNUZ J. Active smoking and the risk of type 2 diabetes: a systematic review and meta-analysis. JAMA. 2007;298:2654–64. doi: 10.1001/jama.298.22.2654. [DOI] [PubMed] [Google Scholar]
- YANG SH, DOU KF, SONG WJ. Prevalence of diabetes among men and women in China. N Engl J Med. 2010;362:2425–6. author reply 2426. [PubMed] [Google Scholar]