Abstract
The purpose of the current study was to determine if volunteerism is prospectively associated with hypertension risk among older adults. Participants provided data during the 2006 and 2010 waves of the Health and Retirement Study, a longitudinal panel survey utilizing a nationally representative sample of community-dwelling older adults (age >50). Volunteerism and blood pressure were measured at baseline and again four years later. Analyses exclude individuals hypertensive at baseline and control for age, race, sex, education, baseline systolic/diastolic blood pressure, and major chronic illnesses. Those who had volunteered at least 200 hours in the 12 months prior to baseline were less likely to develop hypertension (OR=0.60; 95% CI: 0.40–0.90) than non-volunteers. There was no association between volunteerism and hypertension risk at lower levels of volunteer participation. Volunteering at least 200 hours was also associated with greater increases in psychological well-being (B=0.99; β=0.05; p=.006) and physical activity (B=0.21; β=0.05; p=.04) compared to non-volunteers; however, these factors did not explain the association of volunteerism with hypertension risk.
Keywords: volunteerism, older adults, hypertension, blood pressure, Health and Retirement Study
Epidemiological studies have consistently linked volunteerism to lower all-cause mortality among older adults (Musick, Herzog, & House, 1999; Oman, Thoresen, & McMahon, 1999). However, despite the fact that cardiovascular disease is the leading cause of death among older adults, few studies have focused specifically on how volunteering might be associated with cardiovascular outcomes. Here we examine the association between volunteerism and incidence of hypertension, a risk factor for cardiovascular disease, cardiovascular mortality and stroke, in a sample of the United States population of adults 51 and older.
Participation in volunteer activities can provide older adults with distinct role identities that have positive ramifications for psychological well-being (Thoits, 1983). In the extant literature, volunteerism among older adults has been linked to greater life satisfaction (Thoits & Hewitt, 2001; van Willigen, 2000), more purpose in life (Greenfield & Marks, 2004; Weinstein, Xie, & Cleanthous, 1995), greater self-esteem (Thoits & Hewitt, 2001), increased personal control (Thoits & Hewitt, 2001), and fewer depressive symptoms (Morrow-Howell, Hinterlong, Rozario, & Tang, 2003; Musick & Wilson, 2003). Further, markers of well-being have been associated with blood pressure and hypertension risk in both general and medical populations over 50 (Hawkley, Thisted, Masi, & Cacioppo, 2010; Ostir, Berges, Markides, & Ottenbacher, K.J., 2006; Roepke et al., 2008).
Volunteerism may also be linked to reduced hypertension risk through its effects on physical activity. Fried and colleagues (2004) suggested that volunteer activities may benefit older adults by providing alternative sites for physical activity outside of the home. Many forms of volunteer work require moderate physical exertion (e.g. planting trees, gardening, running/walking with children). Further, the simple act of walking to and from a volunteer site may promote increased activity among otherwise sedentary individuals. In fact, there is increasing evidence that older adults who do volunteer work are more physically active than non-volunteers (Fried et al., 2004; Tan et al., 2009; Tan, Xue, Li, Carlson, & Fried, 2006). Increased physical activity may directly improve cardiovascular function, or it may operate indirectly by delaying the onset of functional limitations that predict psychological distress among older adults (Schieman & Plickert, 2007; Zeiss, Lewinsohn, Rohde, & Seeley, 1996). This reduced psychological distress may, in turn, decrease hypertension risk (Levenstein et al., 2001; Steptoe 2000; Yan et al., 2003).
Burr, Tavares, and Mutchler (2011) have reported an association between volunteerism and hypertension in older adults; however, these analyses had some limitations. First, they relied on longitudinal data that measured hypertension at only one point in time. As a result, it is unclear from their data if volunteerism is associated with prevalent hypertension or the new onset of hypertension. Further, the analyses did not control for chronic illnesses (e.g. history of stroke, heart disease, diabetes) that are associated with elevated blood pressure but also often involve health limitations that may preclude participation in volunteer work. Our analyses build upon the extant literature by prospectively evaluating these associations among older adults, controlling for major chronic illnesses, and excluding individuals with prevalent hypertension at baseline.
We were particularly interested in how the amount of time committed to volunteer work might be important. Existing studies of volunteerism are inconsistent in identifying what level of commitment is beneficial. For example, Luoh and colleagues (2002) found that men and women aged ≥ 70 years who engaged in moderate volunteer work (at least 100 hours in the past year) had lesser mortality risk, fewer functional limitations, and better self-rated health than non-volunteers; however, volunteering at greater levels did not confer any additional benefits in bivariate analyses. In contrast, in their longitudinal analyses, Burr and colleagues (2011) observed lesser hypertension risk among those who volunteered 1–99 hours (compared to non-volunteers); however, greater levels of volunteer work were only marginally related to less hypertension. The relationship between hours volunteering and risk for hypertension could take a number of forms. Some examples include: (1) hypertension risk may decrease in a graded fashion as volunteers’ levels of time commitment increase; (2) there may be a time commitment threshold that one must meet before a benefit is accrued; (3) increased time commitment may be beneficial at first, but there may be a point at which further hours volunteering have equivalent but no additional beneficial effect; and (4) increased time commitment may be beneficial at first but at some point begin to have a negative effect by creating demand overload or interfering with conduct of primary social roles.
We also explore factors that might link volunteerism to reduced hypertension risk. Potential mediators we examine include increases in psychological well-being and physical activity, and decreases in functional limitations. These factors have all been previously associated with both volunteerism and hypertension risk. Further we explore the extent to which demographic variables (e.g. age, sex, race/ethnicity, marital status, education, and employment status) interact with volunteerism in predicting hypertension.
Finally, we were interested in whether or not volunteerism predicts hypertension risk above and beyond personality characteristics, as we expect that personality might select individuals into volunteerism and also be linked to decreased hypertension risk. Agreeableness and extraversion have been previously associated with both greater volunteer participation (Burke & Hall, 1986; Carlo, Okun, Knight & de Guzman, 2005; Smith & Nelson, 1975) and better cardiovascular function (Miller, Cohen, Rabin, Skoner, & Doyle, 1999). Consequently, we evaluate the association between volunteerism and hypertension controlling for these characteristics.
Methods
Participants
Study participants came from the 2006 and 2010 waves of the Health and Retirement Study (HRS), a longitudinal panel study including a nationally representative sample of community-dwelling adults over the age of 50 (Heeringa & Connor, 1995). A total of 6,734 individuals provided volunteerism and blood pressure information at baseline (2006 wave). We first excluded participants who were hypertensive at baseline. That is, they either reported use of antihypertensive medications (3,226 participants), or had average blood pressure readings in the hypertensive range (resting systolic blood pressure ≥ 140 mmHg, or average resting diastolic blood pressure ≥90 mmHg; 1256 participants). We also excluded 26 individuals who were missing data on at least one of the control variables, 170 individuals who died during the follow-up period, and 394 individuals who were lost to follow-up. Our final sample included 1654 participants who were 59.7% female and ages 51–91 years at baseline (mean age 64.2; SD 8.9). The sample included 1381 Non-Hispanic whites, 122 Non-Hispanic Blacks, 119 Hispanics, and 32 participants of other racial/ethnic backgrounds (Table 1).
Table 1.
Descriptive statistics of the study sample
| Variable | |
|---|---|
| Age, mean years (SD) | 64.2 (8.9) |
| Sex | |
| Female, n (%) | 988(59.7) |
| Male, n (%) | 666 (40.3) |
| Race/Ethnicity | |
| Non-Hispanic White, n (%) | 1381 (83.5) |
| Non-Hispanic Black, n (%) | 122 (7.4) |
| Hispanic, n (%) | 119 (7.2) |
| Non-Hispanic Other, n (%) | 32 (1.9) |
| Education | |
| Less than high school, n (%) | 198 (12.0) |
| GED, n (%) | 75 (4.5) |
| High school graduate, n (%) | 476 (28.8) |
| Some college, n (%) | 423 (25.6) |
| College and above (n, %) | 482 (29.1) |
| Marital Status | |
| Married, n (%) | 1169 (70.7) |
| Annulled, n (%) | 0 (0.0) |
| Never married, n (%) | 60 (3.6) |
| Separated, n (%) | 19 (1.1) |
| Divorced, n (%) | 192 (11.6) |
| Widowed, n (%) | 214 (12.9) |
| Employment Status | |
| Employed, n (%) | 866 (52.4) |
| Not Employed, n (%) | 788 (47.6) |
Procedures
The HRS sampling methods and study design have been described previously (Heeringa, & Connor, 1995; Juster & Suzman, 1995). In 2006, in addition to the HRS core interview, 50% of the sample was randomly selected to participate in enhanced face-to-face interviews that included collection of physical measures/biomarker data (including blood pressure) and completion of a self-administered psychosocial questionnaire. Similar follow-up interviews were completed among these individuals in 2010. We compared our sample to the overall sample of individuals who were selected for the enhanced face-to-face interview but excluded from our study. Excluded individuals tended to be older and less educated, less likely to be married, and more likely to be unemployed and to be non-Hispanic white than those in the analyzed sample. Most of these factors have been associated with risk for hypertension (Chobanian, Bakris, Black, Cushman, Green, Izzo, et al., 2003; Detection, 1977; Rose, Newman, Tyroler, Szklo, Arnett, & Srivastava, 1999); hence these differences primarily reflect the exclusion of hypertensives at baseline.
Volunteerism Measure
Volunteerism was measured during the core HRS interview. At baseline (2006), all HRS participants were asked “Have you spent any time in the past 12 months doing volunteer work for religious, educational, health-related or other charitable organizations?” Volunteers were further probed to quantify the number of hours they had spent volunteering in the past 12 months using the following questions: “Altogether, would you say the time amounted to less than 100 hours, more than 100 hours or what?” “Would it be less than 200 hours, more than 200 hours or what?” “Would it be less than 50 hours, more than 50 hours or what?” Based on responses to these questions, we quantified participants’ volunteer hours into the following five categories: none, 1–49 hours, 50–99 hours, 100–199 hours, 200 hours or more.
Outcome Measure
Systolic and diastolic blood pressure were measured in both 2006 and 2010. Three blood pressure measurements, 45 seconds apart, were taken on the respondent’s left arm using an Omron HEM-780 Intellisense automated blood pressure monitor with ComFit cuff (Crimmins, Guyer, Langa, Ofstedal, Wallace, & Weir, 2008). Resting blood pressure values were based on the average of the 3 blood pressure measurements. Individuals were considered to have hypertension at the four-year follow-up examination in 2010 based on the following definition: self-reported use of antihypertensive medications, or average resting systolic blood pressure ≥ 140 mmHg, or average resting diastolic blood pressure ≥90 mmHg.
Standard Control Variables
All analyses controlled for the following variables measured at baseline: average systolic blood pressure (continuous), average diastolic blood pressure (continuous), age (continuous), sex, self-reported race (Non-Hispanic White, Non-Hispanic Black, Hispanic, Non-Hispanic Other), education (less than high school, General Equivalency Diploma [GED], high school diploma, some college, college and above), marital status (married, annulled, never married, divorced, separated, widowed), employment status (employed/not employed), and self-reported history of diabetes (yes/no), cancer (yes/no), heart problems (yes/no), stroke (yes/no), or lung problems (yes/no).
Potential Mediating Variables
We used two variables to assess functional limitations at baseline and 4-year follow-up (Fonda & Herzog, 2004): number of difficulties with activities of daily living (ADLs) and number of difficulties with independent activities of daily living (IADLs). For both variables, we created composite scores by summing the number of difficulties reported in each domain. ADLs included any self-reported difficulty with dressing, walking across a room, bathing/showering, eating, getting in/out of bed, and using the toilet (Katz, Ford, Moskowitz, Jackson, & Jaffe, 1963). IADLs included difficulty preparing hot meals, shopping for groceries, using the telephone, taking medications, managing money, and using a map (Lawton and Brody, 1969).
We used nine variables to assess psychological well-being at baseline and four-year follow-up: personal control, purpose in life, life satisfaction, positive affect, optimism, loneliness, hopelessness, negative affect, and pessimism. These variables were measured in both the 2006 and 2010 HRS waves using standard scales (Table 2). Scores on each measure were determined by averaging the scores across the individual items. Scores were set to missing if more than 50% of individual items for each respective measure had missing values. Correlations between the nine psychological constructs are provided in Table 3. To maintain comparability between waves where there were differences in measurement of the various psychological constructs, the average scores for all of the psychological variables were standardized. A principal components factor analysis of these nine variables at both baseline and follow-up yielded one factor (factor loading of 0.5 or higher). Consequently, we created a composite index of psychological well-being by reverse coding the variables with negative factor loadings, standardizing the average scores for each variable, and summing the standardized scores.
Table 2.
Measures Used to Evaluate Psychological Well-Being in the 2006 and 2010 Waves of the Health and Retirement Study.
| Construct | Measure |
|---|---|
| Hopelessness |
2006: Beck Hopelessness Scale (2 items; Beck, Weissman, Lester, & Trexler, 1974) 2010: Selected hopelessness items (Everson, Kaplan, Goldberg, Salonen, & Salonen, 1997) |
| Life Satisfaction | Satisfaction with Life Scale (5 items; Diener, Emmons, Larsen, & Griffin, 1985) |
| Loneliness |
2006: UCLA Loneliness Scale (3 items; Hughes, Waite, Hawkley, & Cacioppo, 2004) 2010: UCLA Loneliness Scale (11 items; Hughes, Waite, Hawkley, & Cacioppo, 2004) |
| Negative Affect |
2006: Negative Affect Scale from the Midlife in the United States study (MIDUS; 6 items; Mroczek & Kolarz, 1998) 2010: Positive and Negative Affect Schedule-Expanded Form (PANAS-X; 12 items; Watson & Clark, 1994) |
| Optimism | Revised Life Orientation Test (LOT-R; 3 items; Scheier, Carver, & Bridges, 1994) |
| Personal Control | Sense of Control Scales of the Midlife Developmental Inventory (5 items; Lachman & Weaver, 1998a; Lachman & Weaver, 1998b) |
| Pessimism | Revised Life Orientation Test (LOT-R; 3 items; Scheier, Carver, & Bridges, 1994) |
| Positive Affect | Positive Affect Scale from the Midlife in the United States study (MIDUS; 6 items; Mroczek & Kolarz, 1998) |
| Purpose in Life | Purpose Scale of Ryff Measures of Psychological Well-Being (7 items; Ryff 1995; Keyes, Shmotkin, & Ryff, 2002) |
Note. To maintain comparability between waves where there were differences in measurement of the various psychological constructs, the average scores for all of the psychological variables were standardized.
Table 3.
Correlations between nine psychological constructs measured at baseline.
| Personal Control | Purpose in Life | Life Satisfaction | Positive Affect | Optimism | Loneliness | Hopelessness | Negative Affect | Pessimism | |
|---|---|---|---|---|---|---|---|---|---|
| Personal Control | 1 | .327** | .318** | .345** | .355** | −.228 | −.324** | −.350** | −.267** |
| Purpose in Life | .327** | 1 | .320** | .438** | .357** | −.374** | −.419** | −.413** | −.350** |
| Life Satisfaction | .318** | .320** | 1 | .472** | .344** | −.429** | −.403** | −.403** | −.305** |
| Positive Affect | .345** | .438** | .472** | 1 | .397** | −.517** | −.433** | −.561** | −.332** |
| Optimism | .355** | .357** | .344** | .397** | 1 | −.252** | −.345** | −.289** | −.318** |
| Loneliness | −.228 | −.374** | −.429** | −.517** | −.252** | 1 | −.450** | .537** | .375** |
| Hopelessness | −.324** | −.419** | −.403** | −.433** | −.345** | .450** | 1 | .524** | .803** |
| Negative Affect | −.350** | −.413** | −.403** | −.561** | −.289** | .537** | .524** | 1 | .440** |
| Pessimism | −.267** | −.350** | −.305** | −.332** | −.318** | .375** | .703** | .440** | 1 |
p<.01
Physical activity was measured at baseline and four-year follow-up by assessing self-reported participation in vigorous or moderate sports or activities. Examples of vigorous activities included running, jogging, swimming, cycling, aerobics, a gym workout, tennis, or digging with a spade or shovel. Moderate activities included the following examples: gardening, cleaning the car, walking at a moderate pace, dancing, or floor or stretching exercises. Participants were asked to indicate how often they performed each type of activity (vigorous or moderate) using the following categories: more than once a week, once a week, one to three times a month, or hardly ever/never. We used a summary physical activity variable previously used in the English Longitudinal Study of Aging (McMunn, Hyde, Janevic, & Kumari, 2004) to organize vigorous and moderate physical activity into 5 ordinal categories ranging from 0 (sedentary) to 4 (active).
Personality as an Alternative Explanation
Extraversion and agreeableness were assessed by self-report questionnaire using 10 adjectives (5 for each personality characteristic) from the Midlife Development Inventory (MIDI) personality scales (Lachman & Weaver, 1997).
Statistical Analyses
Logistic regression was used to evaluate the relationship between volunteerism and hypertension, adjusting for the standard controls. Categorical variables were dummy coded. We compared volunteers to non-volunteers (reference group) based on their self-reported number of volunteer hours in the past 12 months using the following 4 dummy-coded categories: 1–49 hours, 50–99 hours, 100–199 hours, 200 hours or more. Odds ratios and 95% confidence intervals were used to estimate the ratio of risk at varying levels of volunteering relative to non-volunteers.
To test our expectation that changes in psychological well-being, physical activity, and/or functional limitations would mediate the association between volunteerism and hypertension, we first evaluated associations between volunteerism and changes in the respective mediating variables from baseline to follow-up. We used multiple linear regression to evaluate the extent to which volunteerism (measured at baseline) predicted each potential mediating variable at follow-up. Covariates included our standard controls plus baseline levels of the respective mediating variables. Then in cases where volunteerism predicted changes in our potential mediating variable, we added each variable (measured at both baseline and follow-up) to the regression equation predicting hypertension in separate models. Mediation was supported if the addition of these covariates substantially reduced the association of volunteerism with hypertension risk (Sobel, 1982).
To determine if any of the covariates interacted with volunteerism in predicting hypertension, we used first-order cross product terms for volunteer hours and each of these variables. Interaction terms were entered into individual regression equations with standard controls and the corresponding main effects.
Results
Six hundred sixty-eight (40.4%) of 1654 study participants reported some volunteer work in the 12 months prior to the baseline interview. Among the 668 study participants who reported some volunteer work in the past year, 226 (33.8%) volunteered 1–49 hours, 166 (24.9%) volunteered 50–99 hours, 105 (15.7%) volunteered 100–199 hours, and 171(25.6%) volunteered 200 or more hours. Volunteers were more likely than non-volunteers to be married, Non-Hispanic White, college-educated and not employed (Table 4).
Table 4.
Association Between Standard Controls (Covariates) and Volunteerism in Bivariate Analyses
| Hours of Volunteerism | p value | |||||
|---|---|---|---|---|---|---|
| None | 1–49 Hours | 50–99 Hours | 100–199 Hours | 200 Hours or More | ||
| Mean Age | 64.47 | 64.35 | 62.33 | 63.22 | 64.34 | 0.05 |
| % Female | 57.9 | 63.3 | 65.7 | 63.8 | 57.3 | 0.19 |
| % Non-Hispanic White | 81.1 | 82.7 | 87.3 | 90.5 | 90.1 | 0.005 |
| % Non-Hispanic Black | 7.6 | 8.4 | 9.8 | 3.8 | 5.3 | 0.38 |
| % Hispanic | 9.0 | 8.0 | 1.8 | 2.9 | 3.5 | 0.001 |
| % Non-Hispanic Other | 2.2 | 0.9 | 1.8 | 2.9 | 1.2 | 0.60 |
| Education | <0.0001 | |||||
| % Less than High School | 16.9 | 7.5 | 3.6 | 4.8 | 1.8 | |
| % GED | 5.4 | 3.1 | 3.6 | 2.9 | 3.5 | |
| % High school graduate | 29.6 | 31.9 | 28.9 | 26.7 | 21.1 | |
| % Some college | 24.5 | 31.0 | 23.5 | 20.0 | 29.8 | |
| %College and above | 23.5 | 26.5 | 40.4 | 29.8 | 43.9 | |
| Marital Status | ||||||
| % Married | 66.7 | 70.8 | 74.7 | 81.9 | 82.5 | <0.0001 |
| %Never married | 4.1 | 2.2 | 3.0 | 3.8 | 3.5 | 0.73 |
| %Separated | 1.3 | 1.8 | 0.6 | 0.0 | 0.6 | 0.53 |
| %Divorced | 13.7 | 9.7 | 12.0 | 8.6 | 3.5 | 0.002 |
| %Widowed | 14.2 | 15.5 | 9.6 | 5.7 | 9.9 | 0.03 |
| % Employed | 49.0 | 58.0 | 65.7 | 59.0 | 47.4 | <0.0001 |
| Mean Baseline Average Systolic Blood Pressure | 118.73 | 117.74 | 117.34 | 118.04 | 117.77 | 0.51 |
| Mean Baseline Average Diastolic Blood Pressure | 74.20 | 73.71 | 74.85 | 74.72 | 74.43 | 0.65 |
| % With History of Diabetes | 10.4 | 11.1 | 5.4 | 7.6 | 7.6 | 0.20 |
| % With History of Cancer | 14.3 | 14.6 | 10.8 | 10.5 | 7.6 | 0.11 |
| % With History of Heart Disease | 17.3 | 15.5 | 11.4 | 11.4 | 17.5 | 0.22 |
| % With History of Stroke | 3.8 | 2.2 | 2.4 | 1.9 | 1.8 | 0.43 |
| % With History of Lung Problems | 8.9 | 8.4 | 6.6 | 5.7 | 5.3 | 0.40 |
Of the 1654 study participants included in our analyses, 501 (30.3%) were hypertensive at follow-up. Of the 501 participants who developed hypertension during the 4-year follow-up period, 276 individuals had elevated average resting blood pressure only (systolic blood pressure >140 mmHg or diastolic blood pressure >90), 163 had normal blood pressure but reported use of antihypertensive medications, and 62 individuals had elevated average resting blood pressure AND reported use of antihypertensive medications.
When entered into the logistic regression model together, the following standard control variables were related to increased hypertension risk (Table 5): older age: (B=.03, p=.002), Hispanic ethnicity (compared to Non-Hispanic Whites; B=0.63; p=.004), self-reported history of diabetes (B=0.46; p=.01), average baseline systolic blood pressure (B=0.04; p<.0001), and average baseline diastolic blood pressure (B=0.02; p=.02). The other covariates were not related to hypertension risk. Further, none of the covariates interacted with volunteerism in predicting hypertension.
Table 5.
Logistic Regression Model for the Association of the Standard Controls (Covariates) with Four-Year Incident Hypertension
| Variable | B | Standard Error | P value |
|---|---|---|---|
| Age (Continuous) | 0.03 | 0.009 | 0.001 |
| Sex (Reference: Male) | |||
| Female | 0.05 | 0.14 | 0.75 |
| Race/Ethnicity (Reference: Non-Hispanic White) | |||
| Hispanic | 0.77 | 0.24 | 0.001 |
| Non-Hispanic Black | 0.47 | 0.24 | 0.05 |
| Non-Hispanic Other | −0.25 | 0.46 | 0.59 |
| Education (Reference: college and above) | |||
| Less than High School | 0.05 | 0.22 | 0.83 |
| General Equivalency Diploma (GED) | −0.69 | 0.34 | 0.04 |
| High School Diploma | −0.15 | 0.17 | 0.37 |
| Some College | −0.06 | 0.17 | 0.73 |
| Marital Status (Reference: Never Married) | |||
| Married | 0.03 | 0.31 | 0.91 |
| Divorced | −0.14 | 0.35 | 0.70 |
| Separated | −0.55 | 0.62 | 0.38 |
| Widowed | −0.02 | 0.35 | 0.97 |
| Employment Status (Reference: Not employed) | |||
| Employed | −0.02 | 0.13 | 0.88 |
| Baseline Systolic Blood Pressure (Continuous) | 0.04 | 0.007 | <0.0001 |
| Baseline Diastolic Blood Pressure (Continuous) | 0.02 | 0.01 | 0.02 |
| History of Diabetes | 0.46 | 0.19 | 0.01 |
| History of Cancer | −0.19 | 0.18 | 0.28 |
| History of Heart Problems | 0.27 | 0.16 | 0.09 |
| History of Stroke | 0.16 | 0.32 | 0.62 |
| History of Lung Problems | 0.17 | 0.21 | 0.42 |
In a regression including the covariates, hours of volunteer work were related to hypertension risk (Figure 1). Those who had volunteered at least 200 hours in the past 12 months were less likely to develop hypertension than non-volunteers (OR=0.60; 95% CI: 0.40–0.90). There was also a decrease in hypertension risk among those who volunteered 100–199 hours; however, this estimate was not statistically reliable (OR=0.78; 95% CI=0.48–1.27). Those who volunteered 1–49 and 50–99 hours had hypertension risk similar to that of non-volunteers (OR=0.95; 95% CI: 0.68–1.33 and OR=0.96; 95% CI: 0.65–1.41, respectively).
Figure 1.
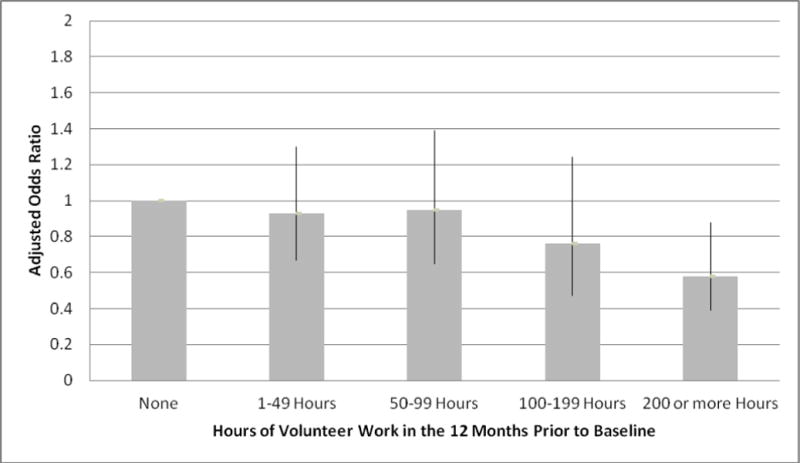
Odds ratios and 95% confidence intervals for 4-year incident hypertension by hours of volunteer work in the 12 months prior to baseline, adjusted for age, race/ethnicity, sex, employment status, marital status, education, baseline systolic blood pressure, baseline diastolic blood pressure, and self-reported history of diabetes, cancer, heart problems, lung problems, or stroke.
The number of hours of volunteer work was associated with increases in psychological well-being (Figure 2). Individuals who engaged in 1–49, 100–199, and 200 or more hours of volunteer work in the 12 months prior to baseline had greater psychological well-being than non-volunteers. There was no difference in levels of well-being between those who volunteered 50–99 hours and non-volunteers (B=−.35; p=0.35). Hours of volunteer work were also associated with increases in physical activity. Individuals who volunteered at least 200 hours in the 12 months prior to baseline reported greater increases in physical activity than nonvolunteers (B=0.21; β=0.05;p=.04). Hours of volunteer work were not associated with changes in ADLs or IADLs.
Figure 2.
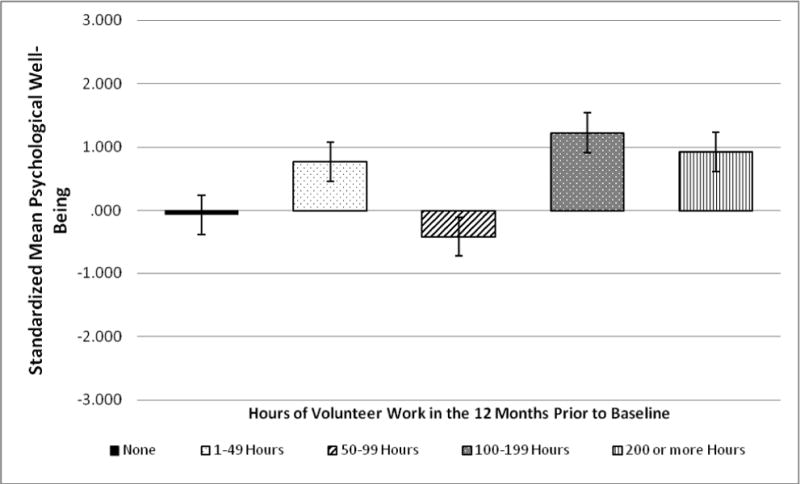
Estimated standardized marginal means (standard error of mean) of psychological well-being at four-year follow-up by hours of volunteer work in the 12 months prior to baseline, adjusted for baseline well-being, age, race/ethnicity, sex, employment status, marital status, education, baseline systolic blood pressure, baseline diastolic blood pressure, and self-reported history of diabetes, cancer, heart problems, lung problems, or stroke.
Although psychological well-being and physical activity were prospectively associated with hours of volunteer work, neither of them altered the association between hours of volunteer work and hypertension when added to the equation in separate regression models (Table 6; regression with well-being: OR 0.56; 95%: CI 0.36–0.90; regression with physical activity: OR 0.60; 95% CI: 0.40–0.91). Given that the composite measure of psychological well-being did not explain the relationship between volunteerism and hypertension, we fit a series of individual regression models to determine whether any of the individual constituent variables reduced the effect; however, none did. We also fit a regression entering extraversion and agreeableness as additional covariates to the original model. Adding these variables to the equation similarly did not reduce the effect size observed between hours of volunteer work and hypertension (Table 6; with the additional covariates OR=0.59; 95% CI: 0.38–0.91).
Table 6.
Logistic Regression for Association of Volunteer Work with Hypertension
| Variable | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 |
|---|---|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Hours of Volunteer Work | ||||||
| None (Reference) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 1–49 | 0.95 (0.68–1.33) | 0.96 (0.68–1.35) | 0.95 (0.68–1.34) | 1.00 (0.69–1.46) | 0.95 (0.68–1.33) | 0.95 (0.68–1.33) |
| 50–99 | 0.96 (0.65–1.41) | 0.91 (0.61–1.36) | 0.98 (0.67–1.45) | 1.00 (0.66–1.54) | 0.97 (0.66–1.42) | 0.95 (0.65–1.40) |
| 100–199 | 0.78 (0.48–1.27) | 0.82 (0.50–1.34) | 0.81 (0.50–1.32) | 0.90 (0.54–1.50) | 0.77 (0.48–1.26) | 0.79 (0.49–1.28) |
| 200 or more | 0.60 (0.40–0.90) | 0.59 (0.38–0.91) | 0.60 (0.40–0.90) | 0.57 (0.36–0.90) | 0.59 (0.39–0.89) | 0.59 (0.39–0.90) |
| Extraversion | 0.81 (0.61–1.06) | |||||
| Agreeableness | 1.42 (1.02–1.96) | |||||
| Physical Activity (Measured at Baseline) | 0.90 (0.82–0.99) | |||||
| Physical Activity (Measured at Follow-up) | 1.04 (0.95–1.14) | |||||
| Psychological Well-Being (Measured at Baseline) | 1.01 (0.98–1.04) | |||||
| Psychological Well-Being (Measured at Follow-up) | 0.99 (0.96–1.02) | |||||
| Number of Difficulties with ADLs (Measured at Baseline) | 1.21 (0.96–1.52) | |||||
| Number of Difficulties with ADLs (Measured at Follow-up) | 0.87 (0.73–1.04) | |||||
| Number of Difficulties with IADLs (Measured at Baseline) | 0.84 (0.69–1.03) | |||||
| Number of Difficulties with IADLs (Measured at Follow-up) | 1.12 (0.96–1.29) |
IADLs: Independent Activities of Daily Living; ADLs: Activities of Daily Living
All models adjust for age, race/ethnicity, sex, employment status, marital status, education, baseline systolic blood pressure, baseline diastolic blood pressure, and self-reported history of diabetes, cancer, heart problems, lung problems, or stroke.
Discussion
We found that those who volunteer 200 hours or more per year (roughly 4 hours per week) were 40% less likely to develop hypertension over a four-year follow-up of a sample of community-dwelling older adults. This association was independent of age, race/ethnicity, baseline health status, education, sex, marital status, employment status, baseline systolic/diastolic blood pressure, extraversion and agreeableness. Importantly, the association persisted even after controlling for chronic illnesses measured at baseline, such as history of diabetes, cancer, stroke, lung problems, or heart problems. This is important because these illnesses could be associated with lesser volunteer participation and also with greater hypertension risk. Our findings are consistent with other literature linking volunteerism to physical health outcomes, including better self-rated health, (Luoh & Herzog, 2002; Morrow-Howell, 2003; Tang, 2009) and lesser mortality risk (Harris & Thoreson, 2005; Luoh & Herzog, 2002; Musick, 1999).
Existing studies of volunteerism and health have been inconsistent in identifying what level of commitment is beneficial. For example, several studies suggest that the health benefits of volunteerism are achieved with 100 or more hours of commitment (Lum & Lightfoot, 2005; Luoh & Herzog, 2002). This difference is likely due to the fact that these studies drew no distinctions between those who volunteered 100–199 hours versus 200+ hours; rather, both groups were collapsed into one category. Here, we treated the two as separate categories in order to more precisely identify the level of commitment most protective with respect to hypertension risk. While we observed a nonsignificant trend toward reduced hypertension risk for those who volunteered at least 100 hours; significant risk reduction was observed only for those who volunteered at least 200 hours.
We found no statistical interactions between volunteerism and sex, age, marital status, employment status, education, race/ethnicity, or baseline systolic/diastolic blood pressure in predicting hypertension. This suggests that the effects of volunteerism on hypertension are equal across various demographic control factors. Further, it indicates that volunteerism is not just protective for those who are nearly hypertensive at baseline. We also found no psychological or behavioral explanations for why volunteer hours were associated with lesser hypertension risk. Volunteerism was associated with increases in both psychological well-being and physical activity. This is consistent with the extant literature which suggests that volunteerism is linked to both physical activity (Fried et al., 2004; Tan et al., 2009; Tan, Xue, Li, Carlson, & Fried, 2006) and markers of well-being(Moen, Dempster-McClain, & Williams, 1992; Morrow-Howell, Hinterlong, Rozario, & Tang, 2003; Musick, Herzog, & House, 1999; Oman et al., 1999; Thoits, 2001; Van Willigen, 2000). Neither of these variables, however, accounted for the association of volunteer hours with hypertension. It is possible that our measure of physical activity was not sensitive enough to capture activity levels among the participants. Self-report measures of moderate and vigorous activity may not adequately reflect levels of physical activity among elderly individuals, as most physical activity performed by older adults involves walking in the context of regular daily activities rather than a formal exercise regimen (Walsh, Rogot, Pressman, Cauley, & Browner, 2004). More sensitive, objectives measures of physical activity (e.g. accelerometry) might be more useful in this population. It is also possible that volunteerism is linked to hypertension through mechanisms not measured here. (Collins, Glei, & Goldman, 2009; Siahpush, Spittal, & Singh, 2008). For example, volunteerism may boost self-esteem and feelings of self-worth in this population. It may also protect individuals from social isolation, as participation in volunteer activities may replenish social ties that may be lost due to social transitions such as retirement, divorce, bereavement, and departure of children from the home. Strong social ties and social network diversity (having multiple social roles) have both been linked to positive health outcomes among older adults (Seeman, Kaplan, Knudsen, Cohen, & Guralnik, 1987; Seeman, Lusignolo, Albert, & Berkman, 2001).
Volunteerism may also function to alter the psychological or biological stress response among older adults. Performing volunteer work may give individuals perspective on their own life struggles, promoting more positive coping strategies in the face of potentially stressful situations. Brown and colleagues (2008) suggest that helping others may release stress-buffering and restorative hormones that decrease activity in the hypothalamic pituitary adrenal (HPA) axis by regulating the cortisol stress response. There is experimental evidence that engaging in prosocial behaviors activates areas of the brain associated with reward and with the release of oxytocin and vasopressin, neurohormones implicated in HPA regulation (Moll, 1996). Dysregulation of the HPA axis has been previously linked to hypertension in experimental studies (Kelly, Mangos, Williamson, & Whitworth, 2007; Wirtz, von Känel, Emini, Ruedisueli, Groessbauer, Maercker, & Ehlert, 2007).
We evaluated how the amount of time committed to volunteer work might be related to hypertension risk. We found a significant association between volunteerism and hypertension risk only when contrasting the highest levels of commitment to nonvolunteers. However, commitment was assessed in rather large increments, insensitive to smaller changes, and there were increasing odds ratios starting at about 100 hours suggesting the possibility of a more linear association.
This study has several strengths. Although its correlational nature does not allow us to make explicit causal inferences, our use of a prospective design and control for chronic illnesses help to decrease the possibility that observed effects are attributable to selection effects, as it is plausible that healthier individuals may be more likely to engage in volunteer work in the first place. Further, we controlled for a range of demographic and personality variables that could have potentially confounded our findings.
This study has broad implications. Hypertension is an important, modifiable risk factor for cardiovascular disease and mortality among older adults. This is the first study to prospectively evaluate the association of volunteerism with hypertension risk. Our findings suggest that volunteerism may be an effective, non-pharmacological intervention for reducing hypertension risk. Future research should more precisely explore possible biological and psychological mechanisms linking volunteerism to hypertension, such as neurohormonal changes that may result from the initiation of volunteer activities or changes in psychological stress, social connectedness or self-esteem that may decrease disease risk. It may also be necessary to evaluate the differential effects of various types of volunteer work. Finally, experimental studies are needed in order to causally link volunteerism to hypertension.
Acknowledgments
These analyses use data from the Health and Retirement Study, (HRS 2006 Core [Final V2.0)]; HRS 2010 Core [Final V1.0]) sponsored by the National Institute on Aging (grant number NIA U01AG009740) and conducted by the University of Michigan. Ms. Sneed’s participation in this work was partly supported by a grant from the National Institutes of Health’s National Center for Complementary and Alternative Medicine (AT006694).
Ms. Sneed’s participation in this research was partly supported by a grant from the National Institutes of Health’s National Center for Complementary and Alternative Medicine (AT006694).
References
- Beck AT, Weissman A, Lester D, Trexler L. The measurement of pessimism: The hopelessness scale. Journal of Consulting and Clinical Psychology. 1974;42(6):861–865. doi: 10.1037/h0037562. [DOI] [PubMed] [Google Scholar]
- Brown SL, Brown RM, House JS, Smith DM. Coping with spousal loss: Potential buffering effects of self-reported helping behavior. Personality and Social Psychology Bulletin. 2008;34:849–861. doi: 10.1177/0146167208314972. [DOI] [PubMed] [Google Scholar]
- Burke DM, Hall M. Personality characteristics of volunteers in a Companion for Children program. Psychological Reports. 1986;59:819–825. [Google Scholar]
- Burr JA, Tavares J, Mutchler JE. Volunteering and Hypertension Risk in Later life. Journal of Aging and Health. 2011;23:24–51. doi: 10.1177/0898264310388272. [DOI] [PubMed] [Google Scholar]
- Carlo G, Okun MA, Knight GP, de Guzman MRT. The interplay of traits and motives on volunteering: Agreeableness, extraversion and prosocial value motivation. Personality and Individual Differences. 2005;38:1293–1305. [Google Scholar]
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Rocella EJ. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. Journal of the American Medical Association. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- Crimmins EM, Guyer H, Langa KM, Ofstedal MB, Wallace RB, Weir DR. Documentation of Physical Measures, Anthropometrics and Blood Pressure in the Health and Retirement Study. 2008 Retrieved from http://hrsonline.isr.umich.edu/sitedocs/userg/dr-011.pdf.
- Detection H. Race, Education, and Prevalence of Hypertension, 2. American Journal of Epidemiology. 1977;106:351–361. [PubMed] [Google Scholar]
- Diener E, Emmons RA, Larsen RJ, Griffin S. The satisfaction with life scale. Journal of Personality Assessment. 1985;49:71–75. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- Everson SA, Kaplan GA, Goldberg DE, Salonen R, Salonen JT. Hopelessness and 4-year progression of carotid atherosclerosis: The Kuopio Ischemic Heart Disease Risk Factor Study. Arteriosclerosis, Thrombosis, and Vascular Biology. 1997;17:1490–1495. doi: 10.1161/01.atv.17.8.1490. [DOI] [PubMed] [Google Scholar]
- Fonda S, Herzog AR. HRS/AHEAD Documentation Report: Documentation of Physical Functioning Measured in the Heath and Retirement Study and the Asset and Health Dynamics among the Oldest Old Study. Ann Arbor, MI: Survey Research Center, University of Michigan; 2004. Retrieved from http://hrsonline.isr.umich.edu/sitedocs/userg/dr-008.pdf. [Google Scholar]
- Fried LP, Carlson MC, Freedman M, Frick KD, Glass TA, Hill J, McGill S, Rebok GW, Seeman T, Tielsch J, et al. A social model for health promotion for an aging population: Initial evidence on the Experience Corps model. Journal of Urban Health. 2004;81:64–78. doi: 10.1093/jurban/jth094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield EA, Marks NF. Formal Volunteering as a Protective Factor for Older Adults’ Psychological Well-Being. The Journals of Gerontology, Series B. 2004;59:S258–S264. doi: 10.1093/geronb/59.5.s258. [DOI] [PubMed] [Google Scholar]
- Harris AHS, Thorensen CE. Volunteering is Associated with Delayed Mortality in Older People: Analysis of the Longitudinal Study of Aging. Journal of Health Psychology. 2005;10:739–752. doi: 10.1177/1359105305057310. [DOI] [PubMed] [Google Scholar]
- Hawkley LC, Thisted RA, Masi CM, Cacioppo JT. Loneliness predicts increased blood pressure: 5-year cross-lagged analyses in middle-aged and older adults. Psychology and Aging. 2010;25:132–141. doi: 10.1037/a0017805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heeringa SG, Connor J. Technical Description of the Health and Retirement Study Sample Design. 1995 Retrieved from http://hrsonline.isr.umich.edu/sitedocs/userg/HRSSAMP.pdf.
- Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A short scale for measuring loneliness in large surveys: results from two population-based studies. Research on Aging. 2004:655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juster FT, Suzman R. An overview of the Health and Retirement Study. Journal of Human Resources. 1995;30:S7–S56. [Google Scholar]
- Katz S, Ford A, Moskowitz R, Jackson B, Jaffe M. Studies of illness in the aged. The index of ADL: A standardized measure of biological and psychosocial function. Journal of the American Medical Association. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- Kelly JJ, Mangos G, Williamson PM, Whitworth JA. Cortisol and hypertension. Clinical and Experimental Pharmacology and Physiology. 2007;25(S1):S51–S56. doi: 10.1111/j.1440-1681.1998.tb02301.x. [DOI] [PubMed] [Google Scholar]
- Keyes CLM, Shmotkin D, Ryff CD. Optimizing well-being: The empirical encounter of two traditions. Journal of Personality and Social Psychology. 2002;82:1007–1022. [PubMed] [Google Scholar]
- Lachman ME, Weaver SL. Unpublished Technical Report. Brandeis University; 1997. Midlife Development Inventory (MIDI) personality scales: Scale construction and scoring. Retrieved from http://www.brandeis.edu/projects/lifespan/scales.html. [Google Scholar]
- Lachman ME, Weaver SL. Sociodemographic variations in the sense of control by domain: Findings from the MacArthur studies of midlife. Psychology and Aging. 1998a;13:556–562. doi: 10.1037//0882-7974.13.4.553. [DOI] [PubMed] [Google Scholar]
- Lachman ME, Weaver SL. The sense of control as a moderator of social class differences in health and well-being. Journal of Personality and Social Psychology. 1998b;74(3):763–773. doi: 10.1037//0022-3514.74.3.763. [DOI] [PubMed] [Google Scholar]
- Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–86. [PubMed] [Google Scholar]
- Levenstein S, Smith MW, Kaplan GA. Psychosocial Predictors of Hypertension in Men and Women. Archives of Internal Medicine. 2001;161:1341–1346. doi: 10.1001/archinte.161.10.1341. [DOI] [PubMed] [Google Scholar]
- Lum TY, Lightfoot E. The Effects of Volunteering on the Physical and Mental Health of Older People. Research on Aging. 2005;27:31–55. [Google Scholar]
- Luoh M, Herzog AR. Individual Consequences of Volunteer and Paid Work in Old Age: Health and Mortality. Journal of Health and Social Behavior. 2002;43:490–509. [PubMed] [Google Scholar]
- McMunn A, Hyde M, Janevic M, Kumari M. Health (Chapter 6) In: Marmot M, Banks J, Blundell R, Lessof C, Nazroo J, editors. Health, Wealth and Lifestyles of the Older Population: The 2002 English Longitudinal Study of Ageing. London: Institute for Fiscal Studies; 2003. pp. 207–230. Retrieved from http://www.ifs.org.uk/ELSA/reportWave1. [Google Scholar]
- Miller GE, Cohen S, Rabin BS, Skoner DP, Doyle WJ. Personality and Tonic Cardiovascular, Neuroendocrine, and Immune Parameters. Brain, Behavior, and Immunity. 1999;13:109–123. doi: 10.1006/brbi.1998.0545. [DOI] [PubMed] [Google Scholar]
- Moen P, Dempster-McClain D, Williams RM., Jr Successful aging: A life course perspective on women’s multiple roles and health. American Journal of Sociology. 1992;97:1612–1638. [Google Scholar]
- Moll J, Krueger F, Zahn R, Pardini M, de Oliveira-Souza R, Grafman J. Huan fronto-mesolimbic networks guide decisions about charitable donation. Proceedings of National Academy of Sciences of the United States of America. 2006;103:15623–15628. doi: 10.1073/pnas.0604475103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrow-Howell N, Hinterlong J, Rozario PA, Tang F. Effects of Volunteering on the Well-Being of Older Adults. Journals of Gerontology: Series B. 2003;58:S137–S145. doi: 10.1093/geronb/58.3.s137. [DOI] [PubMed] [Google Scholar]
- Mroczek DK, Kolarz CM. The effect of age on positive and negative affect: a developmental perspective on happiness. Journal of Personality and Social Psychology. 1998;75:1333–1349. doi: 10.1037//0022-3514.75.5.1333. [DOI] [PubMed] [Google Scholar]
- Musick MA, Herzog AR, House JS. Volunteering and Mortality Among Older Adults: Findings From a National Sample. Journals of Gerontology: Series B. 1999;54B:S173–S180. doi: 10.1093/geronb/54b.3.s173. [DOI] [PubMed] [Google Scholar]
- Musick MA, Johnson W. Volunteerism and Depression: The Role of Psychological and Social Resources in Different Age Groups. Social Science and Medicine. 2003;56:259–69. doi: 10.1016/s0277-9536(02)00025-4. [DOI] [PubMed] [Google Scholar]
- Oman D, Thoresen CE, McMahon K. Volunteerism and mortality among the community dwelling elderly. Journal of Health Psychology. 1999;4:301–316. doi: 10.1177/135910539900400301. [DOI] [PubMed] [Google Scholar]
- Ostir GV, Berges IM, Markides KS, Ottenbacher KJ. Hypertension in Older Adults and the Role of Positive Emotions. Psychosomatic Medicine. 2006;68:727–733. doi: 10.1097/01.psy.0000234028.93346.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roepke SK, Mausbach BT, Aschbacher MS, Ziegler MG, Dimsdale JE, Mills PJ, …Grant I. Personal Mastery is Associated with Reduced Sympathetic Arousal in Stressed Alzheimer Caregivers. American Journal of Geriatric Psychiatry. 2008;16:310–317. doi: 10.1097/JGP.0b013e3181662a80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose KM, Newman B, Tyroler HA, Szklo M, Arnett D, Srivastava N. Women, employment status, and hypertension: cross-sectional and prospective findings from the Atherosclerosis Risk in Communities (ARIC) Study. Annals of epidemiology. 1999;9:374–82. doi: 10.1016/s1047-2797(99)00015-0. [DOI] [PubMed] [Google Scholar]
- Rutledge T, Hogan BE. A Quantitative Review of Prospective Evidence Linking Psychological Factors With Hypertension Development. Psychosomatic Medicine. 2002;64:758–766. doi: 10.1097/01.psy.0000031578.42041.1c. [DOI] [PubMed] [Google Scholar]
- Ryff CD, Keyes CLM. The structure of psychological well-being revisited. Journal of Personality and Social Psychology. 1995;69:719–727. doi: 10.1037//0022-3514.69.4.719. [DOI] [PubMed] [Google Scholar]
- Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A reevaluation of the Life Orientation Test. Journal of Personality and Social Psychology. 1994;67:1063–1078. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- Schieman S, Plickert G. Functional Limitations and Changes in Levels of Depression Among Older Adults: A Multiple-Hierarchy Stratification Perspective. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2007;62:S36–S42. doi: 10.1093/geronb/62.1.s36. [DOI] [PubMed] [Google Scholar]
- Seeman TE, Kaplan GA, Knudsen L, Cohen R, Guralnik J. Social network ties and mortality among tile elderly in the ALAMEDA County Study. American journal of epidemiology. 1987;126(4):714–723. doi: 10.1093/oxfordjournals.aje.a114711. [DOI] [PubMed] [Google Scholar]
- Seeman TE, Lusignolo TM, Albert M, Berkman L. Social relationships, social support, and patterns of cognitive aging in healthy, high-functioning older adults: MacArthur studies of successful aging. Health Psychology; Health Psychology. 2001;20(4):243. doi: 10.1037//0278-6133.20.4.243. [DOI] [PubMed] [Google Scholar]
- Smith BMM, Nelson LD. Personality Correlates of Helping Behavior. Psychological Reports. 1975;37:307–310. doi: 10.2466/pr0.1975.37.1.307. [DOI] [PubMed] [Google Scholar]
- Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. Sociological Methodology. 1982;13:290–312. [Google Scholar]
- Steptoe A. Psychosocial factors in the development of hypertension. Annals of Medicine. 2000;32:371–375. doi: 10.3109/07853890008995940. [DOI] [PubMed] [Google Scholar]
- Tan E, Xue QL, Li T, Carlson M, Fried L. Volunteering: A Physical Activity Intervention for Older Adults—The Experience Corps Program in Baltimore. Journal of Urban Health. 2006;83:954–969. doi: 10.1007/s11524-006-9060-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan EJ, Rebok GW, Yu Q, Frangakis CE, Carlson MC, Wang T, Ricks M, Tanner EK, McGill S, Fried LP. The Long-Term Relationship Between High-Intensity Volunteering and Physical Activity in Older African American Women. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2009;64B:304–311. doi: 10.1093/geronb/gbn023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang F. Late-Life Volunteering and Trajectories of Physical Health. Journal of Applied Gerontology. 2009;28:524–533. [Google Scholar]
- Thoits PA. Multiple Identities and Psychological Well-Being: A Reformulation and Test of the Social Isolation Hypothesis. American Sociological Review. 1983;48:174–87. [PubMed] [Google Scholar]
- Thoits P, Hewitt L. Volunteer work and well-being. Journal of Health and Social Behavior. 2001;42:115–131. [PubMed] [Google Scholar]
- Van Willigen M. Differential benefits of volunteering across the life course. Journal of Gerontology: Social Sciences. 2000;55B:308–318. doi: 10.1093/geronb/55.5.s308. [DOI] [PubMed] [Google Scholar]
- Walsh JM, Rogot Pressman A, Cauley JA, Browner WS. Predictors of Physical Activity in Community-dwelling Elderly White Women. Journal of General Internal Medicine. 2004;16:721–727. doi: 10.1111/j.1525-1497.2001.00506.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark LA. The PANAS-X: Manual for the Positive and Negative Affect Schedule – Expanded Form. 1994 Retrieved from http://www.psychology.uiowa.edu/faculty/clark/panas-x.pdf.
- Weinstein L, Xie X, Cleanthous CC. Purpose in life, boredom, and volunteerism in a group of retirees. Psychological Reports. 1995;76:482. doi: 10.2466/pr0.1995.76.2.482. [DOI] [PubMed] [Google Scholar]
- Wirtz PH, von Känel R, Emini L, Ruedisueli K, Groessbauer S, Maercker A, Ehlert U. Evidence for altered hypothalamus-pituitary-adrenal axis functioning in systemic hypertension: Blunted cortisol response to awakening and lower negative feedback sensitivity. Psychoneuroendocrinology. 2007;32:430–436. doi: 10.1016/j.psyneuen.2007.02.006. [DOI] [PubMed] [Google Scholar]
- Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J, Lisheng L INTERHEART Study Investigators. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART Study): a case-control study. Lancet. 2004;364:937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- Zeiss AM, Lewinsohn PM, Rohde P, Seeley JR. Relationship of physical disease and functional impairment to depression in older people. Psychology & Aging. 1996;11:572–581. doi: 10.1037//0882-7974.11.4.572. [DOI] [PubMed] [Google Scholar]


