Abstract
Black women in the United States are disproportionately affected by obesity, with almost two-thirds considered obese based on body mass index. Obesity has been directly linked to cardiovascular morbidity and mortality in black women. Therefore, understanding contributors to the genesis of obesity in black women is imperative. While biologic differences likely result in varying obesity prevalence across racial/ethnic groups, behaviors such as post-partum weight retention and limited leisure-time physical activity, may especially contribute to obesity in black women. Black women also appear to be particularly susceptible to cultural, psychosocial, and environmental factors that can promote weight gain. Therapeutic interventions are being tailored to specifically address these social determinants of health and to foster lifestyle modification; however, more work is needed to understand barriers to behavior change for black women. Knowledge gaps also remain in identifying mechanisms by which pharmacologic and surgical treatments for obesity modify cardiovascular risk in black women.
Keywords: obesity, Black women, genetics, behavior, cultural norms, psychosocial stress, environmental factors, lifestyle modification, therapeutics
Introduction
The global epidemic of obesity is rising, but the prevalence of obesity is disparate among racial and ethnic groups. In the United States, black women have the highest rates of obesity compared to other racial/ethnic groups [1]. Approximately 60% of black women are considered obese based on a body mass index (BMI) ≥ 30 kg/m2, and black women are 70% more likely to be obese as compared to Non-Hispanic white women [1, 2]. The disparities in obesity prevalence are linked to disproportionate rates of hypertension, diabetes mellitus, and cardiovascular disease (CVD) among black women [3, 4]. Obesity has also been directly associated with 30-day mortality following a myocardial infarction [5••], death from cardiovascular (CV) events, and all-cause mortality in black women [6••].
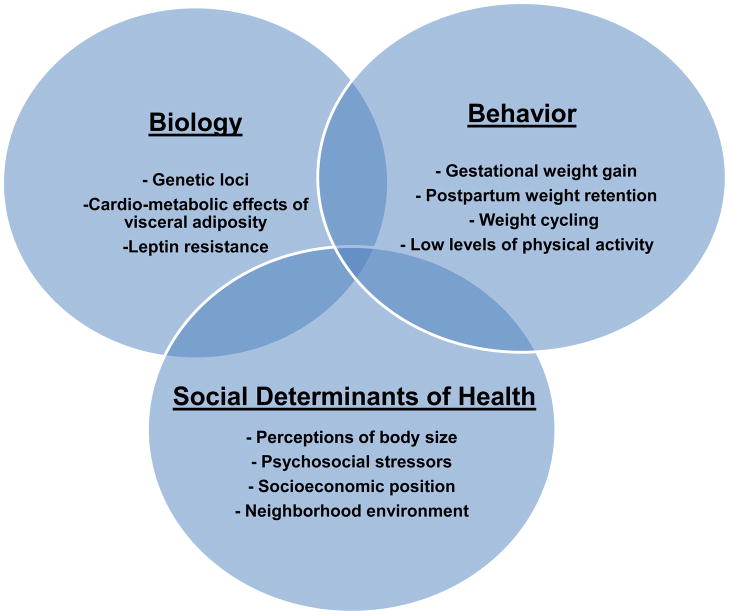
Data from the National Health and Nutrition Examination Survey (NHANES) indicate a significant increase in obesity prevalence from 1999 through 2010 among Non-Hispanic black women, without a significant increase in prevalence for women of all race/ethnic groups [2]. If obesity trends continue as projected, there will be parallel increases in obesity-related CV morbidity and mortality among black women [7–9]. Consequently, obesity is a complex public health issue that must be addressed to improve the CV health of black women. Understanding the genesis of obesity in black women from a biologic, behavioral, and social perspective can aid in the development of targeted, effective treatment to ameliorate the obesity epidemic (Figure). Additionally, evaluating current therapeutic approaches that target obesity among black women can identify existing mechanisms for intervention and areas for future research.
Figure 1.
Figure Factors contributing to the genesis of obesity and increased cardiovascular risk in black women
The Genesis of Obesity among Black Women
Genes and Metabolism
Recent studies have explored heritable traits linked to obesity in blacks [10, 11]; however, obesity-related genetic studies in black women are scarce. In a population-based cohort of women in the southeastern U.S., single nucleotide polymorphisms (SNPs) in adiponectin-related genes were evaluated in black and white women. SNP rs17366568 in the ADIPOQ gene was significantly correlated with adiponectin levels in white women. However, this relationship was not observed among black women in the study [12]. Lower levels of adiponectin have been previously shown among women as compared to men and among blacks as compared to whites [13, 14]; lower adiponectin has also been associated with greater adiposity, metabolic syndrome [15], and atherosclerosis [16]. The authors acknowledged that racial/ethnic differences in the relationship between SNP rs17366568 and adiponectin levels may have been partially due to the greater number of allele frequency variations displayed in persons of African descent as compared to those of European descent [12]. The genetic diversity and complexity of gene frequencies within the genome of individuals of African descent may lead to difficulties in elucidating genetic factors associated with obesity among black women.
Recent data also suggest that black women may be more susceptible to the cardio-metabolic effects of visceral adipose tissue and provide further evidence of racial/ethnic differences in adipokine levels among women. In the Jackson Heart Study, a population-based cohort of over 5,300 African Americans, visceral adipose tissue was a significant predictor of lower adiponectin levels in African American women, but not in African American men [17•]. In addition, African American women in the Study of Women’s Health Across the Nation (SWAN) cohort had significantly lower total adiponectin levels compared to Caucasian women after controlling for overall or central adiposity. African American women in SWAN also had significantly higher levels of leptin and lower levels of soluble leptin receptor (sOB-R) than Caucasian, Japanese, and Chinese women, independent of adiposity [18]. These findings suggest greater resistance to the satiety-promoting effects of leptin among black women as compared to other racial and ethnic groups [19]. Greater leptin resistance may place black women at higher risk of cardio-metabolic diseases, even at lower levels of adiposity.
Behavioral Factors Influencing Weight Loss and Weight Maintenance in Black Women
Excessive gestational weight gain and postpartum weight retention likely contribute to the development of overweight and obesity in black women. Although black women are more likely to have inadequate gestational weight gain than white women, over 40% of black women have excessive gestational weight gain based on recent data [20]. Black women are also more prone to postpartum weight retention than white women when they gain weight during pregnancy [20]. Two studies in low-income, pregnant African American women found that most women perceived gestational weight gain to be essential for their babies’ health and were comfortable with gestational weight gain as long as it did not negatively impact their physical appearance or interfere with their activities. These perceptions were often reinforced through encouragement from members of their social support network to increase their dietary intake during pregnancy [21, 22].
Irrespective of pregnancy-related weight gain, obese black women may disproportionately struggle with weight cycling. Weight cycling is defined as repeated loss and regain of body weight [23]. The proposed consequences of weight cycling on CVD risk are not well-understood [24, 25], but weight cycling has been associated with hypertension [26], central/truncal fat distribution [27], and all-cause and CV mortality [28, 29] in Caucasian populations. However, there are a limited number of studies about weight cycling in blacks. Among 167 overweight and obese black women evaluated prior to recruitment into a weight management program, 63% of them were found to be weight cyclers, reporting weight loss and regain of 20 pounds or more unrelated to illness [30 ]. Black women characterized as weight cyclers had a significantly higher BMI and peak weight, a higher incidence of binge/disordered eating, and greater desire for thinness as compared to non-cyclers [30]. The results of this study are less generalizable because the cohort only included black women seeking treatment for their weight; nonetheless, this study is one of very few to explore weight cycling in black women. More data are needed to understand the prevalence of weight cycling among black women and the biologic pathways by which weight cycling potentially contributes to obesity and CV morbidity and mortality in black women.
Differences in dietary intake may also lead to greater obesity prevalence among black women. Recent data demonstrate lower intake of fruits, vegetables, and whole grains and greater intake of added sugars, sodium, and calories from fat in overweight/obese black women as compared to women of other racial/ethnic groups, particularly Hispanic women [31]. Another important disparity in health behaviors among women of different racial and ethnic groups is levels of physical activity. A significantly larger proportion of black women do not engage in leisure-time physical activity as compared with black men, and men and women of other races/ethnicities [32]. Hair care practices are increasingly recognized as a potential barrier to physical activity among black women. In a study of female African American dermatology patients aged 21–60, fifty percent of the women adjusted their hairstyle to accommodate exercise, a third exercised less frequently because of their hair, and approximately forty percent completely avoided exercise because of hair issues [33••]. Additionally, physical activity was reported to have worsened scalp conditions in up to one-third of the population. The investigators recognized the limited generalizability of this study due to potential oversampling of African American women with hair and scalp conditions, and geographic/regional differences in African American women’s hair care practices [33]. Given the contribution of limited physical activity to decreased CV health among black women [3, 34–36], future interventions that promote physical activity in Black women likely need to address hair-related issues.
Cultural Norms, Psychosocial and Environmental Factors Related to Obesity in Black Women
Perceptions of Body Size
Compared to women of other racial/ethnic groups, overweight and obese black women exhibit acceptance of a larger body size [37•, 38] (Table). Body size misperception, or the desire to maintain or gain weight when one is already obese, appears to be disproportionately more prevalent in racial/ethnic minorities and has been associated with overly-optimistic perceptions of CV risk and unhealthy behaviors, including inadequate physical activity, in African Americans [39, 40]. NHANES data from 2003–2006 demonstrated that among overweight and obese U.S. adults, black women who misperceived their body weight were more likely to be sedentary and less likely to meet recommendations for physical activity as compared to women of other racial/ethnic groups [41]. In addition, data suggest black women have accurate knowledge of the health risks of obesity [42]; however, these health considerations are often trumped by black women’s belief that a larger body size is embraced in their culture [21, 22, 37, 42]. This notion is supported by qualitative data from focus groups of African American women involved in weight control programs where they describe social pressures “not to lose too much weight” [43]. Thus, body size perceptions likely influence weight control, physical activity and, ultimately CV risk in black women.
Table.
Studies that highlight cultural norms, psychosocial & environmental factors that contribute to obesity in black women
| Study Title | Characteristics of Study or Population | Focus of Study | Relevant Findings |
|---|---|---|---|
| Cultural Norms | |||
| Body Image and Modifiable Weight Control Behaviors Among Black Females: A Review of the Literature (Robinson et al., 2011 [37•]) | Literature review of 31 articles | Body image satisfaction and weight loss behaviors | Body image and culture influence dietary, physical activity, and smoking behaviors among black women. |
| Racial differences in perception of healthy body weight in midlife women: Results from the Do Stage Transition Result in Detectable Effects Study (Thomas et al., 2013 [38]) | N= 689 black and white women aged 40 to 65 years | Weight perception | Among women with higher body mass index, black women are more accepting of their weight compared to white women. |
| Does perception equal reality? Weight misperception in relation to weight-related attitude and behaviors among overweight and obese US adults (Duncan et al., 2011 [41]) | N=up to 5401 overweight/obese adults aged ≥ 20 from 2003–2006 NHANES | Weight misperception | Weight misperception in overweight and obese adults is associated with decreased interest or fewer attempts at weight loss and physical activity. |
| Psychosocial Stress | |||
| The contribution of stress to the social patterning of clinical and subclinical CVD risk factors in African Americans: The Jackson Heart Study (Gebreab et al., 2012 [44•]) | N= 4404 African American adults residing in Jackson, MS | Perceived stress and negative life events | High psychosocial stress mediates the relationship between income and obesity, and income and diabetes for African American women. |
| Changes in Waist Circumference and Body Mass Index in the US CARDIA Cohort: Fixed effects associations with self-reported Experiences of racial/ethnic discrimination (Cunningham et al., 2012 [45•]) | N=3,193 black and white adults ages 18–30 years | Racial/ ethnic discrimination | Self-reported experiences of racial/ethnic discrimination is associated with longitudinal weight gain and increases in waist circumference in black women. |
| Environmental Factors | |||
| Lifecourse educational status in relation to weight gain in African American women (Coogan et al., 2012 [46•]) | N=21,457 women in the Black Women’s Health Study | Parental and current educational status | Low parental education status and achieved education below college level are associated with increased likelihood of adult obesity. |
| Racial and Ethnic Residential Segregation, the Neighborhood Socioeconomic Environment, and Obesity Among Blacks and Mexican Americans (Kershaw et al., 2012 [51•]) | N= 5271 adults from NHANES 1999–200 | Racial/ethnic residential segregation | High metropolitan level racial/ethnic residential segregation is associated with obesity in black women. |
| Residential segregation, health behavior and overweight/obesity among a national sample of African American adults (Corral et al., 2012 [52]) | N=11,142 African Americans in the year 2000 Behavioral Risk Factor Surveillance System | Racial/ethnic residential segregation | Metropolitan level racial/ethnic residential segregation is associated with overweight/obesity in blacks. |
Psychosocial Stress
Black women may be particularly vulnerable to obesity and higher CV risk due to psychosocial stress. In the Jackson Heart Study cohort, overall psychosocial stress served a mediating factor in the inverse association between income and prevalent obesity and in the relationship between income and prevalent diabetes for black women [44•]. Among black men in the cohort, this relationship was not seen. While the mediating effect of psychosocial stress on obesity among black women in this study was not statistically significant, the generalized measure of psychosocial stress used in the study may not have reflected the specific types of stressors most relevant to the development of obesity. Racial/ethnic discrimination may be a particular psychosocial stressor that plays a role in weight gain among black women. In the Coronary Artery Risk and Development in Young Adults (CARDIA) cohort, black women who reported greater racial/ethnic discrimination over an eight-year period had significant increases in waist circumference and BMI over time. In contrast, there was no association between increased racial/ethnic discrimination and change in adiposity among black men and white men and women [45•]. Future work should delineate how the specific types and the chronicity of psychosocial stressors, particularly racial/ethnic discrimination, relate to longitudinal weight change in black women.
Socioeconomic and Physical Environment
Socioeconomic status as measured by educational exposure across the life-course likely places black women at risk for weight gain and the development of obesity. Those in the Black Women’s Health Study with the lowest parental education and achieved education levels were found to be more likely to gain weight and become obese in adulthood [46]. For black women who graduated from college, there was no longer a relationship between parental education and risk of obesity, suggesting that a college education may overcome the adverse impact of limited childhood resources on obesity. Additionally, neighborhood-level socioeconomic environment appears to play a causal role in the development of obesity in black women [47, 48••]. The Moving to Opportunities study provided unique, randomized trial-based evidence that moving to a neighborhood of higher socioeconomic level could lessen the prevalence of morbid obesity and diabetes among low-income women. Over 60% of the study cohort was black women although race-stratified outcomes were outside the scope of the study.
Prevalent obesity in the U.S. has been shown to be inversely associated with neighborhood built environment characteristics, such as density of food venues and recreation facilities [49]. More data are emerging that highlight the relationship between neighborhood built environment, obesity and cardio-metabolic risk in black women [50, 51•]. Metropolitan-level racial or ethnic segregation may serve as a surrogate for neighborhood built environment resources. Neighborhoods of higher metropolitan-level segregation are areas of concentrated poverty and disadvantage, and black women are more likely to reside in these neighborhoods with limited resources for healthy nutrition and physical activity [52]. Using NHANES (1999–2006) data, Kershaw and colleagues found greater prevalent obesity among black women living in neighborhoods with higher racial/ethnic residential segregation versus those living in low segregation areas; however, this relationship did not exist for black men [51•]. Therefore, black men and women may have differential responses in coping with the chronic stress associated with neighborhood racial/ethnic segregation. One pathway by which neighborhood built environment may relate to prevalent obesity is through psychosocial stress, as measured by perceptions of neighborhood environment. More unfavorable perceptions of neighborhood environment, especially perceptions related to neighborhood aesthetics and available resources, have been associated with prevalent obesity [53]. However, longitudinal studies are needed to differentiate the mechanisms by which neighborhood built environment may lead to weight gain specifically in Black women.
Therapeutic Approaches Targeting Obesity in Black Women
Lifestyle Modification
Despite recommendations for improved nutrition and increased physical activity as the first line of treatment for obesity [54], physicians appear to provide suboptimal counseling for lifestyle modification to overweight and obese patients, particularly among black women [55–57]. In a sample of over 2,000 obese black and white patients of whom 60% were women, black physicians were up to 66% less likely to counsel black patients on weight reduction as compared to white patients [56]. Additionally, black patients seeing white physicians had a 46% lower likelihood of receiving counseling as compared to white patients seen by white physicians. In data from the Dallas Heart Study, obese African Americans without CV risk factors were less likely to receive lifestyle counseling by clinicians as compared to obese African Americans with CV risk factors, suggesting that obesity itself may not serve as a catalyst for lifestyle modification counseling by health care providers as opposed to the presence of CV risk factors [57]. Physicians may also demonstrate lower emotional rapport, including empathy, with overweight and obese patients, which can potentially impact patients’ weight-related attitudes and behaviors [58, 59]. Although there is evidence suggesting overall racial/ethnic disparities in primary care provider counseling on weight reduction, diet/nutrition, and exercise to obese patients, more data is needed to understand the disparities in lifestyle modification counseling specific to Black women.
Racial/ethnic minority populations and black women in particular, have been disproportionately underrepresented in clinical trials for behavioral weight loss interventions despite the high prevalence of obesity and associated CV risk factors among black women [60]. Specifically, few interventions targeting obesity in black women have occurred in the primary care setting. The Shape Program, a community health center-based intervention, targets overweight and Class I obese African American women in rural North Carolina [61•]. This novel intervention is tailored for a socioeconomically disadvantaged population with elevated CV risk. This study will provide insight into whether behavior change among black women may be achieved by focusing on weight gain prevention to maintain one’s “shape”, thus complying with cultural norms within the black community regarding body size.
In a review of weight loss among African American women in behavioral weight loss interventions published from 1990 to 2010, Fitzgibbon et al. demonstrated that African American women lost significantly less weight as compared to men or women of other racial/ethnic groups. While many of these prior interventions focused on individual-level behavior change, future interventions targeting black women may need to focus on existing social networks or neighborhood-level socioeconomic and built environment factors that limit availability of healthful foods and areas for physical activity [62].
Community-based participatory research (CBPR) approaches to addressing obesity among black women may be a method to leverage existing social networks and modify behavior using environmental changes. Community-based interventions appear to be effective at facilitating health behavior change and improving CV risk factors in black women. A pilot, community-based intervention focused on nutrition and physical activity for a population of African American women in Boston, MA and demonstrated significant reductions in systolic blood pressure, BMI, body weight, and waist circumference in the population [63]. A church-based intervention in over 1,200 overweight and obese African Americans from 74 churches in South Carolina leveraged the availability and accessibility of resources for healthy lifestyle choices and existing social support networks within the church to improve physical activity levels and nutrition [64]. The intervention led to significant improvements in leisure-time moderate to vigorous intensity physical activity with no differences in fruit and vegetable consumption between intervention and control groups. However, only 25% of the study population was African American women, limiting the generalizability of study findings to black women. Finally, Zoellner and colleagues reported significant reductions in blood pressure in a two-phased CBPR-based walking intervention in a cohort predominantly of African American women [65]. Thus, the current literature suggests that successful community-based interventions focused on obesity in black women should engage faith-based organizations [66], community organizations advocating for black women’s health issues [63, 67], and community advisory boards [68] to design interventions promoting social support and environmental changes for lifestyle modification.
Pharmacotherapy for Obesity
Black women have been underrepresented in study populations of recent clinical trials for long-term obesity pharmacotherapy. There are currently three medications approved by the Food and Drug Administration (FDA) for long-term obesity treatment, with lorcaserin and phentermine-topiramate approved in 2012. The multicenter, one-year BLOSSOM trial randomized 4,008 non-diabetic, overweight and obese individuals, of whom 80% were women, to lorcaserin twice daily, once daily or placebo [69]. In the EQUIP trial evaluating phentermine-topiramate in Class II and Class III obesity, 83% of the cohort were women, and the authors claimed that blacks were substantially represented in the study [70]. However, in both trials, blacks only made up approximately 20% of the cohort. Like many studies of pharmacologic approaches for treatment of obesity, these two studies did not stratify results by sex-race/ethnicity groups, which could be helpful in evaluating potential outcomes specific to black women. Although lorcaserin and phentermine-topiramate appear to be effective at inducing clinically significant weight loss when used in conjunction with diet and exercise [69–71], long-term CV safety studies are still required [72]. Furthermore, differences in the distribution of metabolically active adipose tissue among different racial/ethnic groups may affect the efficacy of obesity pharmacotherapy [73]. However, to date, there is no available data to elucidate differences in drug efficacy or CV safety across racial and ethnic groups or specific to black women.
Bariatric Surgery
18% of black women in the U.S. have Class III obesity (BMI ≥ 40 kg/m2) as compared to only 8% of the overall population [2]. However, black women have seldom been a target population for studies of bariatric surgery, one of the most effective therapies for the treatment of diabetes and the reduction of CV risk for individuals with Class III obesity or obesity-related CV risk factors [74–77]. Cohorts in large outcomes studies of bariatric surgery have been entirely [74] or predominantly white [74, 78], limiting the generalizability of findings related to CV risk reduction to black women. Prior data from surgical registries also suggest a lower frequency of bariatric surgery among obese black women. In a nationally representative sample of obese patients hospitalized between 2002 and 2008, over 80% of those who underwent laproscopic gastric bypass were women, but only 12% were African American. African American women were less likely to have undergone laparoscopic gastric bypass as compared to Hispanic and white women [79]. Further studies are needed to elucidate psychosocial, cultural, or socioeconomic factors that may serve as barriers to the use of bariatric surgery among black women.
In a meta-analysis of studies comparing racial/ethnic differences in outcomes after bariatric surgery, patients of African descent who underwent surgery had less weight loss as compared to white patients, regardless of the type of surgery [80•]. However, despite differences in excess weight lost, there were no differences in diabetes remission between the racial/ethnic groups. More outcomes data are needed to determine if individuals of African descent and black women in particular confer similar benefits from bariatric surgery in CV morbidity and mortality as compared to whites.
Conclusion
Given the disproportionate prevalence of obesity among black women in the United States and its impact on CV risk, more work must be done to elucidate mechanisms for the development of obesity in black women. Genetic, behavioral, and social determinants likely contribute in a multifactorial and inter-connected manner to the genesis of obesity in black women (Figure). Black women appear to be highly susceptible to the impact of unfavorable neighborhood environments in the development of obesity. Given the sensitivity of the epigenome to environmental changes, future studies should evaluate epigenetic variability associated with adipokine levels or obesity in black women across different environmental conditions. In addition to epigenomic analyses, other gene-environment interactions should be investigated to elucidate genetic traits that place black women at greater risk for obesity or weight gain in adverse conditions. Moreover, longitudinal data are also needed to determine causal pathways between the duration of psychosocial stressors, such as racial/ethnic discrimination, and the risk of cardio-metabolic diseases in black women. Finally, data on the prevalence of weight cycling, psychosocial and environmental factors related to its development, and its adverse CV effects among obese black women may shed light on an important behavioral factor leading to increased CV risk.
Therapeutic approaches to the treatment of obesity also need to incorporate behavioral, cultural and environmental factors specific to obesity in black women. More recent interventions are beginning to leverage cultural norms related to body size and existing social networks in the black community, particularly through community-based interventions to increase physical activity and improve dietary habits. In addition, interventions targeting excessive gestational weight gain and post-partum weight retention in black women may be effective at reducing future CV risk for this population. Although recent advances have been made in obesity pharmacotherapy and bariatric surgery, black women, who suffer from the highest rates of Class III obesity, have been underrepresented in clinical trials of these new treatments. More work is needed to evaluate the impact of pharmacotherapy and bariatric surgery on CV risk factors and CV outcomes in black women. Concerted efforts to address the epidemic of obesity in black women in the U.S. can reduce racial and ethnic disparities in CVD and ultimately improve the CV health of the U.S. population.
Acknowledgments
Funding Sources: Ms. Agyemang and Dr. Powell-Wiley are supported by the Division of Intramural Research of the National Heart, Lung, and Blood Institute (NHLBI).
Footnotes
Conflict of Interest
Priscilla Agyemang and Tiffany M. Powell-Wiley declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Contributor Information
Priscilla Agyemang, Email: pagyeman169@gmail.com.
Tiffany M. Powell-Wiley, Email: tiffany.powell@nih.gov.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1.National Center for Health Statistics. Health. United States, 2011: With Special Feature on Socioeconomic Status and Health. Hyattsville, MD: 2012. [PubMed] [Google Scholar]
- 2.Flegal KM, Carroll MD, Kit BK, et al. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307:491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 3.Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics--2013 update: a report from the American Heart Association. Circulation. 2013;127:e6–e245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Warren TY, Wilcox S, Dowda M, et al. Independent association of waist circumference with hypertension and diabetes in African American women, South Carolina, 2007–2009. Prev Chron Dis. 2012;9:e105. doi: 10.5888/pcd9.110170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5••.Das SR, Alexander KP, Chen AY, et al. Impact of body weight and extreme obesity on the presentation, treatment, and in-hospital outcomes of 50,149 patients with ST-Segment elevation myocardial infarction results from the NCDR (National Cardiovascular Data Registry) J Am Coll Cardiol. 2011;58:2642–50. doi: 10.1016/j.jacc.2011.09.030. This study examined the impact of morbid obesity on treatment patterns and 30-day in- hospital mortality in patients following ST-segment elevation myocardial infarction. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6••.Boggs DA, Rosenberg L, Cozier YC, et al. General and abdominal obesity and risk of death among black women. N Engl J Med. 2011;365:901–908. doi: 10.1056/NEJMoa1104119. This prospective study of a population-based cohort demonstrated the direct relationship between obesity and all-cause mortality among women in the Black Women’s Health Study. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang YC, McPherson K, Marsh T, et al. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet. 2011;378:815–825. doi: 10.1016/S0140-6736(11)60814-3. [DOI] [PubMed] [Google Scholar]
- 8.Stewart ST, Cutler DM, Rosen AB, et al. Forecasting the effects of obesity and smoking on U.S. life expectancy. N Engl J Med. 2009;361:2252–2260. doi: 10.1056/NEJMsa0900459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bibbins-Domingo K, Coxson P, Pletcher MJ, et al. Adolescent overweight and future adult coronary heart disease. N Engl J Med. 2007;357:2371–2379. doi: 10.1056/NEJMsa073166. [DOI] [PubMed] [Google Scholar]
- 10.Zhao W, Wineinger NE, Tiwari HK, et al. Copy number variations associated with obesity-related traits in African Americans: a joint analysis between GENOA and HyperGEN. Obesity. 2012;20:2431–2437. doi: 10.1038/oby.2012.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Monda KL, Chen GK, Taylor KC, et al. A meta-analysis identifies new loci associated with body mass index in individuals of African ancestry. Nat Genet. 2013 doi: 10.1038/ng.2608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cohen SS, Gammon MD, North KE, et al. ADIPOQ, ADIPOR1, and ADIPOR2 polymorphisms in relation to serum adiponectin levels and BMI in black and white women. Obesity. 2011;19:2053–2062. doi: 10.1038/oby.2010.346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Duncan BB, Schmidt MI, Pankow JS, et al. Adiponectin and the development of type 2 diabetes: the atherosclerosis risk in communities study. Diabetes. 2004;53:2473–8. doi: 10.2337/diabetes.53.9.2473. [DOI] [PubMed] [Google Scholar]
- 14.Heid IM, Wagner SA, Gohlke H, et al. Genetic architecture of the APM1 gene and its influence on adiponectin plasma levels and parameters of the metabolic syndrome in 1,727 healthy Caucasians. Diabetes. 2006;55:375–84. doi: 10.2337/diabetes.55.02.06.db05-0747. [DOI] [PubMed] [Google Scholar]
- 15.Matsuzawa Y, Funahashi T, Nakamura T. The concept of metabolic syndrome: contribution of visceral fat accumulation and its molecular mechanism. J Atheroscler Thromb. 2011;18:629–639. doi: 10.5551/jat.7922. [DOI] [PubMed] [Google Scholar]
- 16.Maahs DM, Ogden LG, Kinney GL, et al. Low plasma adiponectin levels predict progression of coronary artery calcification. Circulation. 2005;111:747–753. doi: 10.1161/01.CIR.0000155251.03724.A5. [DOI] [PubMed] [Google Scholar]
- 17•.Bidulescu A, Liu J, Hickson DA, et al. Gender differences in the association of visceral and subcutaneous adiposity with adiponectin in African Americans: the Jackson Heart Study. BMC Cardiovasc Disord. 2013;13:9. doi: 10.1186/1471-2261-13-9. This study evaluated gender-specific associations between adiposity and adiponectin among African Americans in the Jackson Heart Study cohort. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khan UI, Wang D, Sowers MR, et al. Race-ethnic differences in adipokine levels: the Study of Women’s Health Across the Nation (SWAN) Metabolism. 2012;61:1261–1269. doi: 10.1016/j.metabol.2012.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mattu HS, Randeva HS. Role of adipokines in cardiovascular disease. J Endocrinol. 2013;216:T17–36. doi: 10.1530/JOE-12-0232. [DOI] [PubMed] [Google Scholar]
- 20.Headen IE, Davis EM, Mujahid MS, et al. Racial-ethnic differences in pregnancy-related weight. Adv Nutr. 2012;3:83–94. doi: 10.3945/an.111.000984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Groth SW, Morrison-Beedy D, Meng Y. How pregnant African American women view pregnancy weight gain. J Obstet Ggynecol Neonatal Nurs. 2012;41:798–808. doi: 10.1111/j.1552-6909.2012.01391.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Herring SJ, Henry TQ, Klotz AA, et al. Perceptions of low-income African-American mothers about excessive gestational weight gain. Matern Child Health J. 2012;16:1837–1843. doi: 10.1007/s10995-011-0930-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health. Weight Cycling. Bethesda, MD: Weight Control Information Network; 2008. [Google Scholar]
- 24.Montani JP, Viecelli AK, Prevot A, et al. Weight cycling during growth and beyond as a risk factor for later cardiovascular diseases: the ‘repeated overshoot’ theory. Int J Obes. 2006;30 (Suppl 4):S58–66. doi: 10.1038/sj.ijo.0803520. [DOI] [PubMed] [Google Scholar]
- 25.Jeffery RW, Wing RR, French SA. Weight cycling and cardiovascular risk factors in obese men and women. Am J Clin Nutr. 1992;55:641–644. doi: 10.1093/ajcn/55.3.641. [DOI] [PubMed] [Google Scholar]
- 26.Schulz M, Liese AD, Boeing H, et al. Associations of short-term weight changes and weight cycling with incidence of essential hypertension in the EPIC-Potsdam Study. J Hum Hypertens. 2005;19:61–67. doi: 10.1038/sj.jhh.1001776. [DOI] [PubMed] [Google Scholar]
- 27.Wallner SJ, Luschnigg N, Schnedl WJ, et al. Body fat distribution of overweight females with a history of weight cycling. Int J Obes Relat Metab Disord. 2004;28:1143–1148. doi: 10.1038/sj.ijo.0802736. [DOI] [PubMed] [Google Scholar]
- 28.Blair SN, Shaten J, Brownnell K, et al. Body weight change, all-cause mortality, and cause-specific mortality in the Multiple Risk Factor Intervention Trial. Ann Intern Med. 1993;119:749–757. doi: 10.7326/0003-4819-119-7_part_2-199310011-00024. [DOI] [PubMed] [Google Scholar]
- 29.Rzehak P, Meisinger C, Woelke G, et al. Weight change, weight cycling and mortality in the ERFORT Male Cohort Study. Eur J Epidemiol. 2007;22:665–673. doi: 10.1007/s10654-007-9167-5. [DOI] [PubMed] [Google Scholar]
- 30•.Osborn RL, Forys KL, Psota TL, et al. Yo-yo dieting in African American women: weight cycling and health. Ethn Dis. 2011;21:274–280. Despite data on the adverse cardiovascular risks associated with weight cycling, this study is among the first to examine weight cycling in African American women. [PMC free article] [PubMed] [Google Scholar]
- 31.Kong A, Odoms-Young AM, Schiffer LA, et al. Racial/ethnic differences in dietary intake among WIC families prior to food package revisions. J Nutr Educ Behav. 2013;45:39–46. doi: 10.1016/j.jneb.2012.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.National Center for Chronic Disease Prevention and Health Promotion, Division of Adult and Community Health. Adults Who Report No Liesure Time Physical Activity During Preceding Month: REACH, U.S. 2009. Atlanta, GA: 2011. [Google Scholar]
- ••33.Hall RR, Francis S, Whitt-Glover M, et al. Hair Care Practices as a Barrier to Physical Activity in African American Women. Arch Dermatol. 2012:1–6. doi: 10.1001/jamadermatol.2013.1946. This cross-sectional study highlights a growing area of interest for targeting health behaviors related to hair care practices among black women. [DOI] [PubMed] [Google Scholar]
- 34.Chomistek AK, Manson JE, Stefanick ML, et al. The Relationship of Sedentary Behavior and Physical Activity to Incident Cardiovascular Disease: Results from the Women’s Health Initiative. J Am Coll Cardiol. 2013 doi: 10.1016/j.jacc.2013.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Manson JE, Greenland P, LaCroix AZ, et al. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med. 2002;347:716–725. doi: 10.1056/NEJMoa021067. [DOI] [PubMed] [Google Scholar]
- 36.Mathieu RA, Powell-Wiley TM, Ayers CR, et al. Physical activity participation, health perceptions, and cardiovascular disease mortality in a multiethnic population: the Dallas Heart Study. Am Heart J. 2012;163:1037–1040. doi: 10.1016/j.ahj.2012.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37•.Robinson SA, Webb JB, Butler-Ajibade PT. Body image and modifiable weight control behaviors among black females: a review of the literature. Obesity. 2012;20:241–252. doi: 10.1038/oby.2011.54. This review article examines 31 studies pertaining to body image satisfaction and weight loss behaviors in black women. [DOI] [PubMed] [Google Scholar]
- 38.Thomas S, Ness S, Thurston RC, et al. Racial differences in perception of healthy body weight in midlife women: results from the Do Stage Transitions Result in Detectable Effects study. Menopause. 2013;20:269–273. doi: 10.1097/GME.0b013e31826e7574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Powell TM, de Lemos JA, Banks K, et al. Body size misperception: a novel determinant in the obesity epidemic. Arch Intern Med. 2010;170:1695–1697. doi: 10.1001/archinternmed.2010.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mastin T, Campo S, Askelson NM. African American women and weight loss: disregarding environmental challenges. J Transcult Nurs. 2012;23:38–45. doi: 10.1177/1043659611414140. [DOI] [PubMed] [Google Scholar]
- 41.Duncan DT, Wolin KY, Scharoun-Lee M, et al. Does perception equal reality? Weight misperception in relation to weight-related attitudes and behaviors among overweight and obese US adults. Intern J Behav Nutr Phys Act. 2011;8:20. doi: 10.1186/1479-5868-8-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.James DC, Pobee JW, Oxidine D, et al. Using the health belief model to develop culturally appropriate weight-management materials for African-American women. J Acad Nutr Diet. 2012;112:664–670. doi: 10.1016/j.jand.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 43.Barnes AS, Kimbro RT. Descriptive study of educated African American women successful at weight-loss maintenance through lifestyle changes. J Gen Intern Med. 2012;27:1272–1279. doi: 10.1007/s11606-012-2060-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44•.Gebreab SY, Diez-Roux AV, Hickson DA, et al. The contribution of stress to the social patterning of clinical and subclinical CVD risk factors in African Americans: the Jackson Heart Study. Soc Sci Med. 2012;75:1697–1707. doi: 10.1016/j.socscimed.2012.06.003. This cross-sectional study explores the impact of perceived stress and negative life events on cardiovascular risk factors in the Jackson Heart Study cohort. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45•.Cunningham TJ, Berkman LF, Kawachi I, et al. Changes in waist circumference and body mass index in the US CARDIA cohort: fixed-effects associations with self-reported experiences of racial/ethnic discrimination. J Biosoc Sci. 2013;45:267–278. doi: 10.1017/S0021932012000429. Using data from the CARDIA cohort, this longitudinal study investigates changes in waist circumference and body mass index associated with racial/ethnic discrimination. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Coogan PE, Wise LA, Cozier YC, et al. Lifecourse educational status in relation to weight gain in African American women. Ethn Dis. 2012;22:198–206. [PMC free article] [PubMed] [Google Scholar]
- 47.Coogan PF, Cozier YC, Krishnan S, et al. Neighborhood socioeconomic status in relation to 10-year weight gain in the Black Women’s Health Study. Obesity. 2010;18:2064–2065. doi: 10.1038/oby.2010.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48••.Ludwig J, Sanbonmatsu L, Gennetian L, et al. Neighborhoods, obesity, and diabetes--a randomized social experiment. N Engl J Med. 2011;365:1509–1519. doi: 10.1056/NEJMsa1103216. This is one of the first randomized trials to assess the effects of changes in neighborhood socioeconomic level with moving on obesity and diabetes prevalance in U.S. populations. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jilcott Pitts SB, Edwards M, Moore JB, et al. Obesity is Inversely Associated with Natural Amenities and Recreation Facilities Per Capita. J Phys Act Health. 2012:23. doi: 10.1123/jpah.10.7.1032. [DOI] [PubMed] [Google Scholar]
- 50.Lee RE, Mama SK, Adamus-Leach HJ. Neighborhood street scale elements, sedentary time and cardiometabolic risk factors in inactive ethnic minority women. PloS one. 2012;7:e51081. doi: 10.1371/journal.pone.0051081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51•.Kershaw KN, Albrecht SS, Carnethon MR. Racial and ethnic residential segregation, the neighborhood socioeconomic environment, and obesity among Blacks and Mexican Americans. Am J Epidemiol. 2013;177:299–309. doi: 10.1093/aje/kws372. This cross-sectional study of a national sample of African American adults provides insight about the association between metropolitan level racial/ ethnic neighborhood segregation and obesity among ethnic minorities. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Corral I, Landrine H, Hao Y, et al. Residential segregation, health behavior and overweight/obesity among a national sample of African American adults. J Health Psychol. 2012;17:371–378. doi: 10.1177/1359105311417191. [DOI] [PubMed] [Google Scholar]
- 53.Powell-Wiley TM, Ayers CR, de Lemos JA, et al. Relationship between perceptions about neighborhood environment and prevalent obesity: data from the Dallas Heart Study. Obesity. 2013;21:e14–21. doi: 10.1002/oby.20012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Moyer VA. Screening for and management of obesity in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2012;157:373–378. doi: 10.7326/0003-4819-157-5-201209040-00475. [DOI] [PubMed] [Google Scholar]
- 55.Alexander SC, Cox ME, Turer B, et al. Do the Five A’s Work When Physicians Counsel About Weight Loss? Family Medicine. 2011;43:179–184. [PMC free article] [PubMed] [Google Scholar]
- 56.Bleich SN, Simon AE, Cooper LA. Impact of patient-doctor race concordance on rates of weight-related counseling in visits by black and white obese individuals. Obesity. 2012;20:562–570. doi: 10.1038/oby.2010.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Powell-Wiley TM, Ayers CR, Banks-Richard K, et al. Disparities in counseling for lifestyle modification among obese adults: insights from the Dallas Heart Study. Obesity. 2012;20:849–855. doi: 10.1038/oby.2011.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cox ME, Yancy WS, Jr, Coffman CJ, et al. Effects of counseling techniques on patients’ weight-related attitudes and behaviors in a primary care clinic. Patient Educ Couns. 2011;85:363–368. doi: 10.1016/j.pec.2011.01.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gudzune KA, Catherine Beach M, Roter DL, et al. Physicians build less rapport with obese patients. Obesity. 2013 doi: 10.1002/oby.20384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bennett GG, Warner ET, Glasgow RE, et al. Obesity treatment for socioeconomically disadvantaged patients in primary care practice. Arch Intern Med. 2012;172:565–574. doi: 10.1001/archinternmed.2012.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61•.Foley P, Levine E, Askew S, et al. Weight gain prevention among black women in the rural community health center setting: the Shape Program. BMC Public Health. 2012;12:305. doi: 10.1186/1471-2458-12-305. This study highlights the potential of a community- based intervention to target obesity in socioeconomically disadvantaged populations. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Fitzgibbon ML, Tussing-Humphreys LM, Porter JS, et al. Weight loss and African-American women: a systematic review of the behavioural weight loss intervention literature. Obesity Rev. 2012;13:193–213. doi: 10.1111/j.1467-789X.2011.00945.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rodriguez F, Christopher L, Johnson CE, et al. Love your heart: a pilot community-based intervention to improve the cardiovascular health of African American women. Ethn Dis. 2012;22:416–421. [PubMed] [Google Scholar]
- 64.Wilcox S, Parrott A, Baruth M, et al. The faith, activity, and nutrition program: a randomized controlled trial in african-american churches. Am J Prev Med. 2013;44:122–131. doi: 10.1016/j.amepre.2012.09.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zoellner JM, Connell CC, Madison MB, et al. H.U.B city steps: methods and early findings from a community-based participatory research trial to reduce blood pressure among African Americans. Int J Behav Nutr Phys Act. 2011;8:59. doi: 10.1186/1479-5868-8-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Whitt-Glover MC, Goldmon MV, Karanja N, et al. Learning and Developing Individual Exercise Skills (L.A.D.I.E.S.) for a better life: a physical activity intervention for black women. Contemp Clin Trials. 2012;33:1159–1171. doi: 10.1016/j.cct.2012.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Yoong SL, Carey M, Sanson-Fischer R, et al. A systematic review of behavioural weight-loss interventions involving primary-care physicians in overweight and obese primary-care patients (1999–2011) Public Health Nutr. 2012:1–17. doi: 10.1017/S1368980012004375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wilcox S, Sharpe PA, Parra-Medina D, et al. A randomized trial of a diet and exercise intervention for overweight and obese women from economically disadvantaged neighborhoods: Sisters Taking Action for Real Success (STARS) Contemp Clin Trials. 2011;32:931–945. doi: 10.1016/j.cct.2011.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Fidler MC, Sanchez M, Raether B, et al. A one-year randomized trial of lorcaserin for weight loss in obese and overweight adults: the BLOSSOM trial. J Clin Endocrin Metab. 2011;96:3067–3077. doi: 10.1210/jc.2011-1256. [DOI] [PubMed] [Google Scholar]
- 70.Allison DB, Gadde KM, Garvey WT, et al. Controlled-release phentermine/topiramate in severely obese adults: a randomized controlled trial (EQUIP) Obesity. 2012;20:330–342. doi: 10.1038/oby.2011.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gadde KM, Allison DB, Ryan DH, et al. Effects of low-dose, controlled-release, phentermine plus topiramate combination on weight and associated comorbidities in overweight and obese adults (CONQUER): a randomised, placebo-controlled, phase 3 trial. Lancet. 2011;377:1341–1352. doi: 10.1016/S0140-6736(11)60205-5. [DOI] [PubMed] [Google Scholar]
- 72.Colman E, Golden J, Roberts M, et al. The FDA’s assessment of two drugs for chronic weight management. N Engl J Med. 2012;367:1577–1579. doi: 10.1056/NEJMp1211277. [DOI] [PubMed] [Google Scholar]
- 73.Carter R, Mouralidarane A, Ray S, et al. Recent advancements in drug treatment of obesity. Clin Med. 2012;12:456–460. doi: 10.7861/clinmedicine.12-5-456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Adams TD, Davidson LE, Litwin SE, et al. Health benefits of gastric bypass surgery after 6 years. JAMA. 2012;308:1122–1131. doi: 10.1001/2012.jama.11164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hallersund P, Sjostrom L, Olber T, et al. Gastric bypass surgery is followed by lowered blood pressure and increased diuresis - long term results from the Swedish Obese Subjects (SOS) study. PloS one. 2012;7:e49696. doi: 10.1371/journal.pone.0049696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sjostrom L, Peltonen M, Jacobson P, et al. Bariatric surgery and long-term cardiovascular events. JAMA. 2012;307:56–65. doi: 10.1001/jama.2011.1914. [DOI] [PubMed] [Google Scholar]
- 77.Vest AR, Heneghan HM, Agarwal S, et al. Bariatric surgery and cardiovascular outcomes: a systematic review. Heart. 2012;98:1763–1777. doi: 10.1136/heartjnl-2012-301778. [DOI] [PubMed] [Google Scholar]
- 78.Mackey RH, Belle SH, Courcoulas AP, et al. Distribution of 10-year and lifetime predicted risk for cardiovascular disease prior to surgery in the longitudinal assessment of bariatric surgery-2 study. Am J Cardiol. 2012;110:1130–1137. doi: 10.1016/j.amjcard.2012.05.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Worni M, Guller U, Maciejewski ML, et al. Racial differences among patients undergoing laparoscopic gastric bypass surgery: a population-based trend analysis from 2002 to 2008. Obes Surg. 2013;23:226–233. doi: 10.1007/s11695-012-0832-8. [DOI] [PubMed] [Google Scholar]
- 80•.Admiraal WM, Celik F, Gerdes VE, et al. Ethnic differences in weight loss and diabetes remission after bariatric surgery: a meta-analysis. Diabetes Care. 2012;35:1951–1958. doi: 10.2337/dc12-0260. This meta- analysis examines differences in weight loss outcomes and diabetes mellitus remission in Caucasians and African Americans after bariatric surgery. [DOI] [PMC free article] [PubMed] [Google Scholar]