Abstract
Objectives
To examine and compare the effects of massage and matrix rhythm therapy in young women on the peripheral blood circulation.
Design
Randomized, double-blind, controlled trial.
Setting
Pamukkale University in Denizli, Turkey.
Patients
Fifteen healthy women age 19–23 years.
Intervention
Matrix rhythm therapy was applied to the left lower extremity for a single 30-minute session. At least 1 week later, massage was applied to the left lower extremity for 30 minutes in a single session. The same physiotherapist applied both sessions.
Outcome measures
The blood velocity (cm/s), artery diameter (mm), and blood flow (ml/min) of the popliteal and the posterior tibial arteries were measured with color Doppler ultrasonography. All images were evaluated by the same radiologist.
Results
After matrix rhythm therapy and massage application, blood velocity, artery diameter, and blood flow in arteries increased. However, matrix rhythm therapy caused a more prominent increase in the amount of blood flow in the popliteal and in the posterior tibial artery than did massage. After matrix rhythm therapy application, the average increases in the blood flow rates in the popliteal and the posterior tibial arteries were 25.29%±16.55% and 34.33%±15.66%, respectively; after the massage, the increases were 17.84%±17.23% and 16.07%±10.28%, respectively.
Conclusion
Matrix rhythm therapy and massage increased peripheral blood flow in young women. Matrix rhythm therapy method resulted in more prominent increases.
Introduction
In patients with musculoskeletal problems, anaerobic metabolism is activated because of the reduction of the blood circulation and microcirculation.1,2 The impaired regulation of microcirculation in the muscle is thought to result in nociceptive pain.3 Circulation has an essential role in tissue healing.4 The increased blood circulation facilitates the delivery of protein, nutrients, and oxygen, which in turn results in better tissue healing.5 Numerous recent studies have compared the effects of different conservative treatment approaches on the bloodstream to determine their effectiveness.1,4,6,7
Massage is a physiotherapeutic approach widely used to improve blood circulation.8 Massage therapy is defined as soft tissue manipulation, applied for therapeutic purposes, by a trained therapist.9 Some sports medicine staff believe that massage has benefits, such as increasing blood circulation, reducing muscle tension and neural excitability, and even increasing feeling.10 However, opinions about the effects of massage on circulation differ. In the literature, some authors suggest that massage improves blood circulation,11–14 whereas others claim that it has no effect.15–18
The types of massage application include effleurage, pétrissage, tapotement, friction, and vibration.8 Vibration massage is used to improve the circulation and to facilitate muscle relaxation.19 With mechanical devices, vibration treatment can be applied safely and in a more localized manner.8 Vibration devices with edited speed and frequency can be used for different indications.19 Certain vibration devices are used in beauty salons for fat burning, hand-held vibration devices are used for musculoskeletal pain,12 and whole-body vibration devices are used as an exercise modality.20 Although hand-held devices have a strong placebo effect, especially over the short term, low-magnitude mechanical vibration is thought to increase local blood flow.8,21–23
Matrix rhythm therapy (MRT) is a new application of vibromassage used in special education and rehabilitation centers; sports clubs; and neurologic, orthopedic, physical therapy, and rehabilitation centers. A few studies and clinical experience indicate the effectiveness of MRT.24–26 However, the level of evidence of these studies is low. To explain the therapeutic effectiveness of MRT, its effect on the peripheral circulation should be investigated.
Because MRT is a new method of vibromassage, no studies have evaluated its effect on the circulation. Moreover, the literature reports conflicting results regarding the effect of massage on the peripheral circulation. No device is required for massage. However, MRT is a vibromassage method applied with a device. If the results of the current study show that massage and MRT increase the peripheral blood circulation to the same extent, the findings would suggest that massage may be preferable to MRT. An earlier study observed that the therapists prefer to use manual hand massage instead of hand-held devices.27 For this reason, instead of comparing the MRT application with placebo, the current study compared the effects of MRT with those of conventional massage on the peripheral blood circulation.
This study sought to examine and compare the acute effects of conventional massage and MRT application on the peripheral blood circulation of the triceps surae muscle in healthy young women. The study hypotheses were as follows: (1) Massage and MRT increase the peripheral blood circulation, and (2) MRT increases the peripheral blood circulation more than conventional massage does.
Materials and Methods
Participants
Fifteen healthy young women age 19–23 years were included in the study. Table 1 lists the demographic characteristics. The inclusion criteria were age 18–24 years, no medical treatment (including drugs that affect the peripheral circulation), no acute or chronic pain anywhere in the body, no other disease-related symptoms, no orthopedic or neurologic problems (joint, muscle, bone, or nerve-related), no circulatory problems, no prior surgery of the lower extremity associated with muscles or joints, no skin problems, and body mass index less than 28 kg/m2. Women were excluded if they were active athletes or smokers. All participants were volunteers and gave informed consent to participate in the study. The Denizli Clinical Research Ethics Board approved the study.
Table 1.
Demographic Characteristics
| Variable | Minimum–maximum | Mean±standard deviation |
|---|---|---|
| Age (y) | 19–23 | 21.47±1.06 |
| Height (cm) | 158–172 | 164.87±4.70 |
| Weight (kg) | 50–65 | 55.20±5.06 |
| Body mass index (kg/m2) | 17,65–22,49 | 20.29±1.45 |
Measurements
At least 12 hours before the first measurement, the participants were asked not to drink beverages such as tea, coffee, and alcohol, which can affect the blood circulation. In addition, the participants rested in bed for 15 minutes before the first measurement. The participants' hemodynamic responses before and after the application were evaluated with color Doppler ultrasound using the linear probe (also called the transducer). This is a popular configuration for peripheral vascular scanning.28 The measurements were performed by the same radiologist using the same device in a dark, quiet room, with a constant humidity and temperature. The location where the vessel was best displayed during the first measurement was marked with an indelible pencil, and the second measurement was repeated at the same point. The second measurement was performed immediately after the application.15,29,30
Two arteries—the popliteal artery and the proximal portion of the posterior tibial artery—were evaluated. The diameter of the artery was measured in the anteroposterior cross-section (Fig. 1). To determine the velocity of blood flow through the artery, the peak systolic maximum velocity (Vmax) was measured. The Doppler insonation angle was kept below 60 degrees during the velocity measurements. The average speed (Vmean) was calculated as the mean of the three consecutive measurements of Vmax (Fig. 2).
FIG 1.
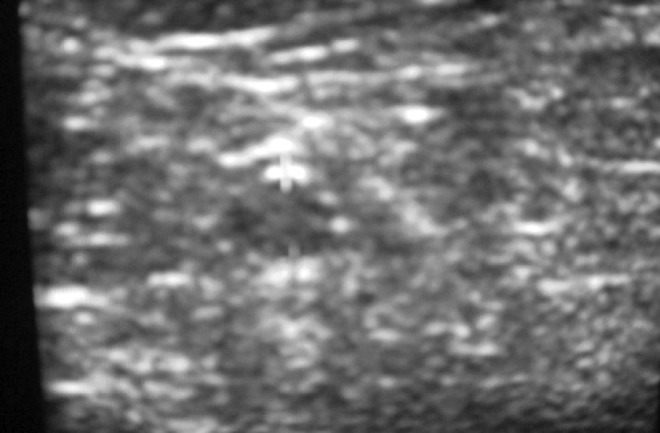
Measurement of arterial diameter.
FIG 2.
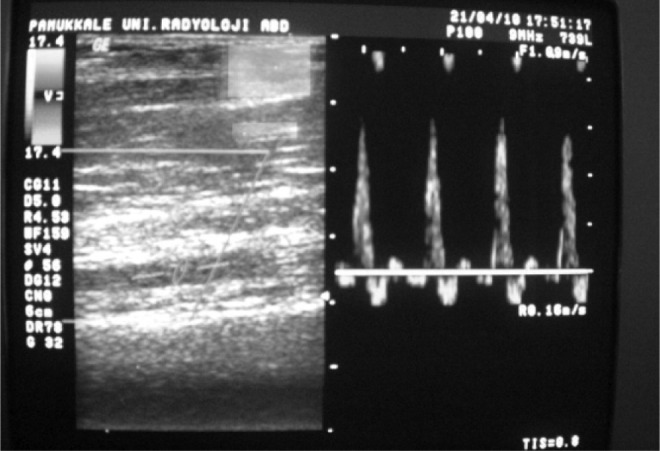
Measurement of blood flow velocity.
The radius and the cross-sectional area of the vessel were determined (the vessel was assumed to be circular). The amount of blood flow through the vessel (ml/min) was calculated by using the following formula:
 |
where mean blood velocity (cm/sec) was the average of three consecutive Vmax values, π is the constant value of 3.14, and r is the radius of the cross-sectional area of the vessel in mm.31
Interventions
During the treatment, the participants were in the prone position, with the body and lower limbs flat. Both methods were applied for 30 minutes to the hamstrings and triceps surae muscle groups in the left lower limbs. The left side was preferred because of the location of the Doppler ultrasound device in the room. In both methods, the application was performed from the proximal to the distal. The MRT technique was applied parallel to the fibers of muscle groups. With massage, stroking and kneading were used.16
Statistical analysis
For the statistical analysis, SPSS software, version 15.0, was used (SPSS Inc., Chicago, Illinois). The descriptive data are expressed as minimum–maximum and mean±standard deviation. The Wilcoxon signed-rank test was used to determine the effectiveness of the methods used in this study. For the analysis of the differences before and after applications of the two different methods, the Mann-Whitney U test was used. After the treatments, the percentage increase in blood flow in arteries depending on the level of resting was calculated, and the average values of percentage increase in arterial blood flow were obtained.
Results
Before application of MRT and conventional massage, vessel diameter and blood flow velocity were measured, and blood flow in the vessel was calculated. The preliminary data obtained from the measurements were compared statistically, and the difference was statistically insignificant (p>0.05) (Table 2).
Table 2.
First Comparison of Values Obtained Before Applications
| |
Matrix rhythm therapy |
Massage therapy |
|
||
|---|---|---|---|---|---|
| Outcome | Minimum–maximum | Mean±SD | Minimum–maximum | Mean±SD | p-Value* |
| Posterior tibial artery | |||||
| Vmean (cm/s) | 17.33–76.20 | 38.36±16.33 | 22.90–67 | 41.07±14.09 | 0.539. |
| R (mm) | 3.1–4.2 | 3.69±0.32 | 3.5–4.9 | 3.94±0.36 | 0.098 |
| BF (ml/min) | 164.46–612.79 | 402.22±142.52 | 273.42–1222 | 47 525.58±283.04 | 0.305 |
| Popliteal artery | |||||
| Vmean (cm/s) | 29–88.33 | 54.90±19.61 | 31.40–66 | 47.26±9.80 | 0.345 |
| R (mm) | 4.3–5.5 | 4.88±0.37 | 4–5.8 | 4.96±0.45 | 0.624 |
| BF (ml/min) | 438.78–1514.05 | 1038.58±384.34 | 394.38–1400.94 | 931.90±2644.47 | 0.389 |
Mann-Whitney U test.
BF, blood amount flowing in the artery; R, radius of the cross-sectional area of the artery; SD, standard deviation; Vmean, average value of three successive measurements; Vmax, peak systolic maximum velocity.
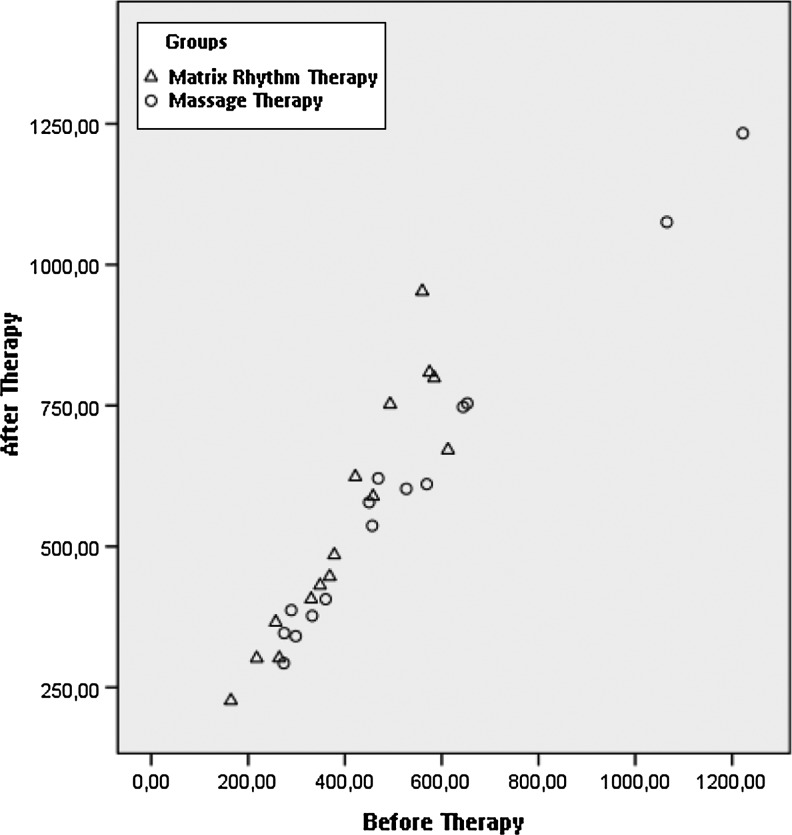
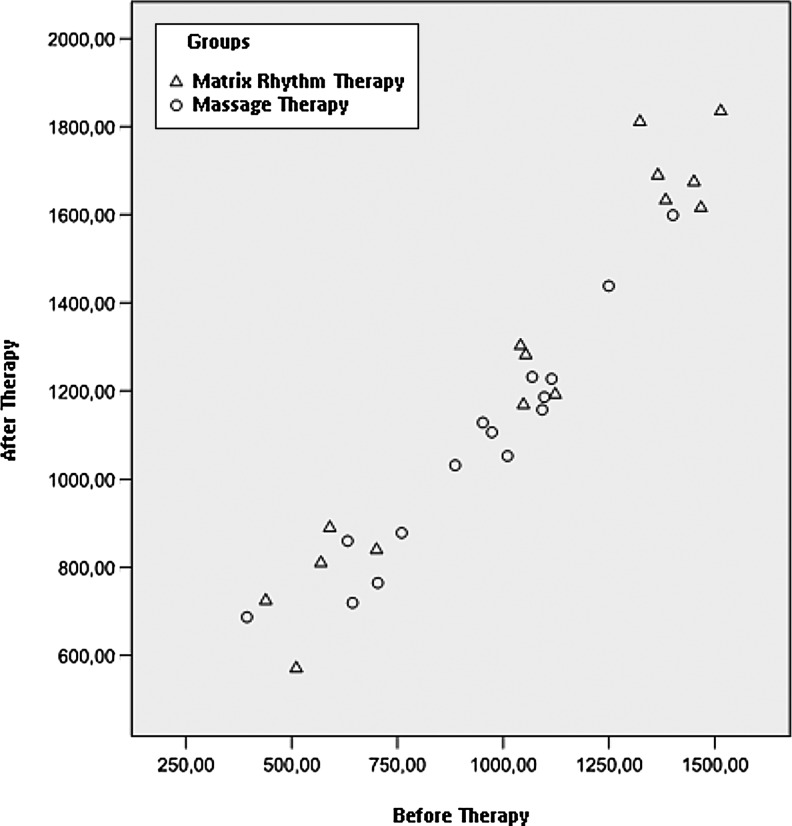
After the application of MRT, the velocity, diameter, and blood flow in the posterior tibial artery and popliteal artery were increased compared with the values before the application. The difference between the measured hemodynamic parameters before and after the application was highly significant (p≤0.001) (Table 3). After application of massage, the velocity, diameter, and blood flow in the posterior tibial artery and popliteal artery were also increased compared with the values before the application. The difference between the measured hemodynamic parameters before and after the application was very significant. Namely, p-values of hemodynamic parameters of the posterior tibial artery and popliteal artery ranged from 0.001 to 0.008 (Table 3). Figure 3 and Figure 4 show scatter plots of blood flow results in the posterior tibial and popliteal arteries.
Table 3.
Comparison of Hemodynamic Parameters of Matrix Rhythm Therapy and Conventional Massage Before and After Application
| |
Before therapy |
After therapy |
|
||
|---|---|---|---|---|---|
| Variable | Minimum–Maximum | Mean±SD | Minimum–Maximum | Mean±SD | p-Value |
| Matrix rhythm therapy (n=15) | |||||
| Posterior tibial artery | |||||
| Vmean (cm/s) | 17.33–76.20 | 38.36±16.33 | 22.86–79.50 | 44.60±17.20 | 0.001* |
| R (mm) | 3.1–4.2 | 3.69±0.32 | 3.2–4.6 | 3.93±0.32 | 0.001* |
| BF (ml/min) | 164.46–612.79 | 402.22±142.52 | 226.36–952.78 | 544.05±217.92 | 0.001* |
| Popliteal artery | |||||
| Vmean (cm/s) | 29–88.33 | 54.90±19.61 | 30.26–89.86 | 60.89±18.42 | 0.001* |
| R (mm) | 4.3–5.5 | 4.88±0.37 | 4.4–6.1 | 5.13±0.46 | 0.001* |
| BF (ml/min) | 438.78–1514.05 | 1038.58±384.34 | 570.34–1834.75 | 1269.13±426.73 | 0.001* |
| Massage therapy (n=15) | |||||
| Posterior tibial artery | |||||
| Vmean (cm/s) | 22.90–67 | 41.07±14.09 | 24.53–67.66 | 44.11±13.70 | 0.001* |
| R (mm) | 3.5–4.9 | 41.07±14.09 | 3.7–4.9 | 4.06±0.30 | 0.003* |
| BF (ml/min) | 273.42–1222.47 | 525.58±283.04 | 292.88–1233.21 | 593.93±271.95 | 0.001* |
| Popliteal artery | |||||
| Vmean (cm/s) | 31.40–66 | 394.38–1400.94 | 38.96–67.33 | 51.59±9.28 | 0.008* |
| R (mm) | 4–5.8 | 4.96±0.45 | 4.3–5.9 | 5.1±0.41 | 0.008* |
| BF (ml/min) | 394.38–1400.94 | 931.90±2644.47 | 686.98–1598.84 | 1071.18±258.85 | 0.004* |
Mann-Whitney U test.
FIG 3.
Scatter plot showing blood flow data of posterior tibial artery.
FIG 4.
Scatter plot showing blood flow data of popliteal artery.
To assess the effectiveness of MRT and conventional massage, the study compared the hemodynamic parameters before and after both applications. The application of MRT caused more increases in blood flow rate in the posterior tibial artery compared with conventional massage (p≤0.05).
The two methods were compared in terms of the blood flow velocity in the popliteal artery; although blood flow velocity after the application of MRT was greater than that of conventional massage, the difference was not statistically significant (p>0.05). Regarding the effect on diameter of the posterior tibial artery, the increase after MRT was significantly greater than that after conventional massage (p≤0.05). However, although the increase in the diameter of the popliteal artery favored MRT, the difference between the two methods was statistically insignificant (p>0.05)
As to the effect of the two methods on blood flow per minute in the popliteal and posterior tibial arteries, MRT caused a greater increase in blood flow compared with conventional massage (p≤0.05) (Table 4). The percentage increase in blood flow observed after the implementation of each method was calculated. After the application of MRT and conventional massage, the average increase in blood flow rates in the popliteal and the posterior tibial arteries were 25.29%±16.55% and 34.33%±15.66% and 17.84%±17.23% and 16.07%±10.28%, respectively, depending on the level of resting (Table 5).
Table 4.
The Difference between Hemodynamic Parameters Before and After Implementation
| Variable | Difference in matrix rhythm therapy group (n=15) | Difference in massage therapy group (n=15) | p-Value |
|---|---|---|---|
| Posterior tibial artery | |||
| Vmean (cm/s) | 6.24±4.05 | 3.04±2.92 | 0.008* |
| R (mm) | 0.24±0.15 | 3.04±2.92 | 0.05* |
| BF (ml/min) | 141.82±98.57 | 68.34±42.60 | 0.016* |
| Popliteal artery | |||
| Vmean (cm/s) | 5.98±5.82 | 4.32±4.37 | 0.486 |
| R (mm) | 0.24±0.15 | 0.14±0.1 | 0.056 |
| BF (ml/min) | 230.55±111.74 | 139.28±69.63 | 0.015* |
Values are expressed as the mean±standard deviation.
Mann-Whitney U test.
Table 5.
Percentage Average Increase in Blood Flow Levels After Application, Depending on Level of Resting
| Variable | Matrix rhythm therapy group (n=15) (%) | Massage therapy group (n=15) (%) |
|---|---|---|
| Popliteal artery | 25.29±16.55 | 17.84±17.23 |
| Posterior tibial artery | 34.33±15.66 | 16.07±10.28 |
Values are expressed as the mean±standard deviation.
Discussion
This study have evaluated and compared the acute effects of MRT, which is used in physical therapy and rehabilitation clinics, and of conventional massage therapy, which is a traditional physical therapy approach, on the peripheral blood circulation of the triceps surae muscle group in healthy young women. This study found that MRT improves the peripheral circulation more than conventional massage does.
Wright and Sluka reported that massage can improve tissue healing, pain modulation, and mood because of different physiologic effects.32 The authors have pointed out a study showing the beneficial effects of massage on the arterial and the venous blood circulation and edema.12 The current results showed that massage leads to acute hemodynamic changes in the peripheral blood vessels, with an increase of 17.84%±17.23% in the popliteal artery and 16.07%±10.28% in the posterior tibial artery.
In a study on the effects of therapeutic massage applied to the neck and the shoulders on the peripheral bloodstream was examined using a dynamic infrared thermography, massage led to an increase in temperature.14 This result is consistent with the current findings. Conventional massage is thought to affect the blood circulation through mechanical and reflex stimulation.13 Sefton et al. showed an increase in temperature in the region where the massage was applied, as well as in the adjacent region.14 The temperature increase in the adjacent region reveals the effect of reflex stimulation. Other studies indicate that massage does not improve the peripheral blood circulation.15–18 In a study describing the effect of different types of massage while resting, Shoemaker has applied effleurage, pétrissage, and tapotement massages each for 5 minutes, with a 5-minute rest period between the applications, followed by exercise. That study found that massage does not increase the blood circulation, but exercise does.16 In that study, the total application time for massage was 15 minutes, with a rest period of 5 minutes between applications. In the current study, massage was applied for a longer period without any disruption. These differences in methods may have led to contradictory results. Some other studies that evaluated the efficacy of massage after exercise16–18 found that massage did not improve blood flow. Therefore, the results of these studies show that massage after exercise does not increase blood circulation.
The results of the current study reveal that MRT improves the blood circulation more than conventional massage does. In MRT, the therapist applies longitudinal strokings by pushing the probe of the device towards the soft tissues. Compared with that of massage, the compression effect created by the application of MRT can cause more soft tissue mobilization and more afferent stimuli by the effect of the vibration. Callaghan has suggested that the major effect of mechanical vibration massage is to increase the blood circulation and that the tonic vibration reflex in mechanical vibration leads to the active contraction of the muscles.13 The muscle contraction may have caused an increase in blood flow. In addition, we think that MRT is an application similar to connective tissue massage (CTM), which is a soft tissue manual therapy approach.33 In CTM, the therapist applies soft tissue mobilization using his or her fingers. In MRT, a similar procedure is performed with the probe of the device. The experimental observations show that CTM can also improve the blood circulation through its effects on the autonomic system, independent of physiologic effects.33,34 Therefore, MRT can cause more mechanical and reflex stimulation than conventional massage.
The vibration frequency created by the MRT device is thought to be compatible with the natural vibration frequency of the muscle, which is considered to contribute to the therapeutic effectiveness of MRT.35 However, this idea lacks scientific support. No previous study has compared MRT and any other vibration devices. The current study found that MRT increases the blood circulation by 35%. In previous studies, following the application of different mechanical vibratory devices, Zhang et al., Button, and Stewart have reported an increased blood flow at a rate of 20%, 26%, and 46%, respectively.21–23 The increase in the blood circulation due to the use of MRT in this study is similar to that of other mechanical devices. Because of its effect on the blood circulation, MRT can be suggested as an alternative method for treating musculoskeletal problems. There are a limited number studies with a low level of evidence about the effects of MRT on musculoskeletal problems. Jager et al. have assessed the effect of MRT on pain level, sleep patterns, and flexibility of the spine in patients with low back pain. The results of that study, involving 80 patients, demonstrate that the application of MRT, compared with conservative therapy (including application of warmth, electrotherapy, and exercise), is more effective in reducing pain and in increasing sleep duration and flexibility of the spine.26 Randoll and Hennig applied MRT in 65 patients with low back pain over six sessions within a week, and they reported a significant improvement in pain.24
This study has some limitations. The study population is small. Neither method of massage was compared with a placebo. Button et al. compared the effect of a mechanical vibration device with a (nonvibratory) placebo device on the local peripheral blood circulation in healthy individuals. Depending on the level of resting, after the application of vibration, the average increase in the blood flow was 26%±49%, whereas the same value after the application of placebo was 12±39%.23 In addition, the current study focused on the early (immediate) effect MRT and conventional massage but did not assess duration of effect and the timing of maximum increase. Sefton et al. found that the temperature rise caused by massage continues 60 minutes after the application.14 Button reported that the application of mechanical vibration level causes an increase in the bloodstream at peak level after 22 minutes.23 In the current study, the participants felt a greater temperature increase in the lower extremities after MRT application and reported that the feeling of warmth lasted longer. However, this information is a subjective description.
Conclusion
This study observed that the application of MRT and conventional massage increases the peripheral blood circulation in healthy young women. The MRT method was more effective on the peripheral blood circulation compared with conventional massage. Still, certain issues require further investigation. The small increase noted in the blood circulation after conventional massage is a remarkable result. To evaluate the effect of MRT and conventional massage on the bloodstream, placebo-controlled studies are needed. This study was not placebo controlled because the MRT method was compared with conventional massage, which manual therapists in daily practice usually prefer. In addition, further studies are necessary to determine and compare the peak level of the peripheral blood circulation after the application of MRT and other vibration devices. Furthermore, investigation of the effect of MRT on the blood circulation in individuals with musculoskeletal problems will highlight the need for clinical studies. Despite all these issues, the current findings suggest that MRT is an approach that can be selected to improve the blood circulation in healthy people.
Acknowledgment
This study was supported by the Pamukkale University Scientific Research Commission (grant no. 2009SBE014).
Disclosure Statement
No competing financial interests exist.
References
- 1.Sakai Y. Matsuyama Y. Ishiguro N. Intramuscular oxygenation of exercising trunk muscle in elderly persons. J Lumbar Spine Disorders. 2005;11:148–56. [Google Scholar]
- 2.Oskarsson E. Gustafsson BE. Pettersson K. Piehl Aulin K. Decreased intramuscular blood flow in patients with lateral epicondylitis. Scand J Med Sci Sports. 2007;17:211–215. doi: 10.1111/j.1600-0838.2006.00567.x. [DOI] [PubMed] [Google Scholar]
- 3.Larsson R. Oberg PA. Larsson SE. Changes of trapezius muscle blood flow and electromyography in chronic neck pain due to trapezius myalgia. Pain. 1999;79:45–50. doi: 10.1016/S0304-3959(98)00144-4. [DOI] [PubMed] [Google Scholar]
- 4.Lohman EB., 3rd Bains GS. Lohman T. DeLeon M. Petrofsky JS. A comparison of the effect of a variety of thermal and vibratory modalities on skin temperature and blood flow in healthy volunteers. Med Sci Monitor. 2011;17:72–81. doi: 10.12659/MSM.881921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cameron MH. Thermal agents: physical principles, cold and superficial heat. Physical Agents in Rehabilitation: From Research to Practice. In: Cameron MH, editor. Philadelphia: Saunders; 1999. pp. 149–175. [Google Scholar]
- 6.Kelly R. Beehn C. Hansford A. Westphal KA. Halle JS. Greathouse DG. Effect of fluidotherapy on superficial radial nerve conduction and skin temperature. J Orthop Sports Phys Ther. 2004;34:377–384. doi: 10.2519/jospt.2005.35.1.16. [DOI] [PubMed] [Google Scholar]
- 7.Sandberg ML. Sandberg MK. Dahl J. Blood flow changes in the trapezius muscle and overlying skin following transcutaneous electrical nerve stimulation. Phys Ther. 2007;87:1047–1055. doi: 10.2522/ptj.20060178. [DOI] [PubMed] [Google Scholar]
- 8.Goats G. Massage—the scientific basis of an ancient art: part 1. The techniques. Br J Sports Med. 1994;28:149–152. doi: 10.1136/bjsm.28.3.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Field TM. Massage therapy effects. Am Psychol. 1998;53:1270–1281. doi: 10.1037//0003-066x.53.12.1270. [DOI] [PubMed] [Google Scholar]
- 10.Weerapong P. Hume PA. Kolt GS. The mechanisms of massage and effects on performance, muscle recovery and injury prevention. Sports Med. 2005;35:235–256. doi: 10.2165/00007256-200535030-00004. [DOI] [PubMed] [Google Scholar]
- 11.Tappan FM. East Norwalk, CT: Appelton & Lange; 1988. Effects of massage. In: Tappan's Handbook of Healing Massage Techniques: Classic, Holistic and Emerging Methods; pp. 21–34. [Google Scholar]
- 12.Goats G. Massage—the scientific basis of an ancient art: part 2. Physiological and therapeutic effects. Br J Sports Med. 1994;28:153–156. doi: 10.1136/bjsm.28.3.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Callaghan MJ. The role of massage in the management of the athlete: a review. Br J Sports Med. 1993;27:28–33. doi: 10.1136/bjsm.27.1.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sefton JM. Yarar C. Berry JW. Pascoe DD. Therapeutic massage of the neck and shoulders produces changes in peripheral blood flow when assessed with dynamic infrared thermography. J Altern Complement Med. 2010;16:723–732. doi: 10.1089/acm.2009.0441. [DOI] [PubMed] [Google Scholar]
- 15.Tiidus PM. Shoemarker JK. Effleurage massage, muscle blood flow and long-term post-exercise strength recovery. Int J Sports Med. 1995;16:478–483. doi: 10.1055/s-2007-973041. [DOI] [PubMed] [Google Scholar]
- 16.Shoemaker J. Tiidus P. Mader R. Failure of manual massage to alter limb blood flow: measures by Doppler ultrasound. Med Sci SportsExercise. 1997;29:610–614. doi: 10.1097/00005768-199705000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Hinds T. McEwan I. Perkes J. Dawson E. Ball D. George K. Effects of massage on limb and skin blood flow after quadriceps exercise. Med Sci Sports Exercise. 2004;36:1308–1313. doi: 10.1249/01.mss.0000135789.47716.db. [DOI] [PubMed] [Google Scholar]
- 18.Wiltshire EV. Poitras V. Pak M. Hong T. Rayner J. Tschakovsky ME. Massage impairs postexercise muscle blood flow and "lactic acid" removal. Med Sci Sports Exercise. 2010;42:1062–1071. doi: 10.1249/MSS.0b013e3181c9214f. [DOI] [PubMed] [Google Scholar]
- 19.Benjamin PJ. Lamp SP. Champaign, IL: Human Kinetics; 2005. Understanding Sports Massage; pp. 2–9. [Google Scholar]
- 20.Rittweger J. Beller G. Felsenberg D. Acute physiological effects of exhaustive whole-body vibration exercise in man. Clin Physiol. 2000;20:134–142. doi: 10.1046/j.1365-2281.2000.00238.x. [DOI] [PubMed] [Google Scholar]
- 21.Zhang Q. Ericson K. Styf J. Blood flow in the tibialis anterior muscle by photoplethysmography during foot-transmitted vibration. Eur J Appl Physiol. 2003;90:464–469. doi: 10.1007/s00421-003-0904-5. [DOI] [PubMed] [Google Scholar]
- 22.Stewart JM. Karman C. Montgomery LD. McLeod KJ. Plantar vibration improves leg fluid flow in perimenopausal women. Am J Physiol. 2005;288:R623–R629. doi: 10.1152/ajpregu.00513.2004. [DOI] [PubMed] [Google Scholar]
- 23.Button C. Anderson N. Bradford C. Cotter JD. Ainslie PN. The effect of multidirectional mechanical vibration on peripheral circulation of humans. Clin Physiol Functional Imaging. 2007;27:211–216. doi: 10.1111/j.1475-097X.2007.00739.x. [DOI] [PubMed] [Google Scholar]
- 24.Randoll UG. Hennig FF. A new approach for the treatment of low back pain, matrix-rhythm-therapy. Osteologie. 2001;(Suppl):66. [Google Scholar]
- 25.Randoll UG. Hennig FF. Preoperative and postoperative matrix-rhythm-therapy to optimize hip surgery. Osteologie. 2001;(Suppl):149. [Google Scholar]
- 26.Jager PA. Chan D. Muderrisoglu HF. Matrix rhythm therapy application to patient with back pain. Turk J Phys Ther Rehabil. 2008;19:217. [Google Scholar]
- 27.McDonagh D. Wilson L. Haslamand C. Weightman D. Good vibrations: do electrical therapeutic massagers work? Ergonomics. 2005;48:680–691. doi: 10.1080/00140130500070988. [DOI] [PubMed] [Google Scholar]
- 28.Ultrasound – Technology Information Portal. Transducer types [homepage on the Internet] www.us-tip.com/serv1.php?type=db1&dbs=Transducer+Types. [Apr 7;2010 ]. www.us-tip.com/serv1.php?type=db1&dbs=Transducer+Types
- 29.Casey DP. Joyner MJ. Skeletal muscle blood flow responses to hypoperfusion at rest and during rhythmic exercise in humans. J Applied Physiol. 2009;107:429–437. doi: 10.1152/japplphysiol.00331.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Osada T. Radegran G. Femoral artery blood flow and its relationship to spontaneous fluctuations in rhythmic thigh muscle workload. Clin PhysiolFunct Imaging. 2009;29:277–292. doi: 10.1111/j.1475-097X.2009.00868.x. [DOI] [PubMed] [Google Scholar]
- 31.Merritt CRB. Doppler color flow imaging. J Clin Ultrasound. 1987;15:591–597. doi: 10.1002/jcu.1870150904. [DOI] [PubMed] [Google Scholar]
- 32.Wright A. Sluka KA. Nonpharmacological treatments for musculoskeletal pain. Clin J Pain. 2001;17:33–46. doi: 10.1097/00002508-200103000-00006. [DOI] [PubMed] [Google Scholar]
- 33.Goats GC. Keir KI. Connective tissue massage. Br J Sports Med. 1991;25:131–133. doi: 10.1136/bjsm.25.3.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Holey LA. Dixon J. Selfe J. An Exploratoryt hermographic investigation of the effects of connective tissue massage on autonomic function. J Manip Physiol Ther. 2011;34:457–462. doi: 10.1016/j.jmpt.2011.05.012. [DOI] [PubMed] [Google Scholar]
- 35.Matrix Rhythmus Therapie [home page on the Internet] www.marhythe.in/index.php/about-marhyther/the-therapy. [Apr 14;2010 ]. www.marhythe.in/index.php/about-marhyther/the-therapy