Abstract
Objective:
To determine the effectiveness of the use of the SIP score and the quality of life impairment in patients with ileal conduit and orthotropic ileal derivations by Hautmann and AbolEnein/Ghoneim.
Methods:
Prospectively evaluated 146 patients in different age groups. In 66 patients ileal conduit derivation was performed, in 20 patients orthotropic derivation using Hautman technique was recorded and in 20 of them AbolEnein/Ghoneim was used. Prior to examining patients with urinary diversions, 40 patients with minor urological symptoms not requiring any active treatment, were surveyed in order to validate SIP score. Six months after the operation, all patients with urinary diversions filled the SIP score questionnaire.
Results:
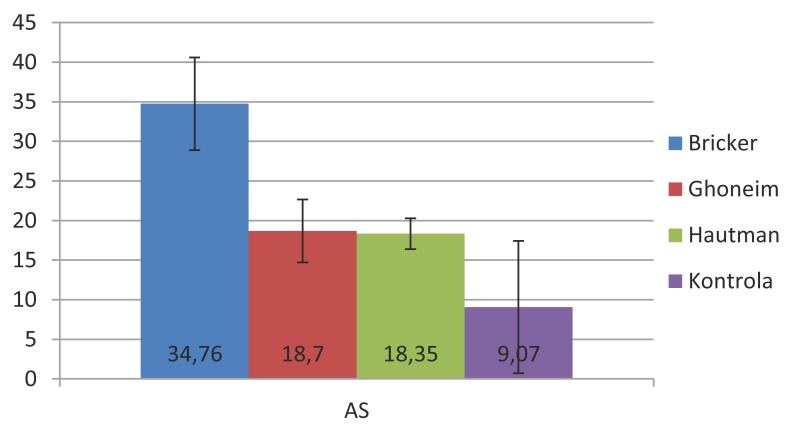
Using Crombach’s Alpha equation the high reliability of SIP questionnaire was proven. Average scale value was 0,93. Using descriptive statistics mean values of all categories and dimensions of the SIP questionnaire of examined patients were determined, calculated according to the questionnaire manual being converted to percentage. Total value of SIP score for the ileal conduit group was 34,76% and in orthotropic derivation 18,52% respectively. For Hautmann procedure total SIP score was 18,35% and for AbolEnein/Ghoneim 18,7%. In the control group total SIP score was 9%. The most influential dimensions on the total score of ileal conduit were physical and psycho-social, while independent dimension did not significantly influent total SIP score.
Conclusion:
Taking into consideration the lack of questionnaires on quality of life for urinary derivations, SIP score as a general disease influence to the quality of life questionnaire represents a reliable alternative for objectification and quantification of the quality of life upon urinary derivation. According to this instrument, orthotropic derivations provide significantly better quality of life compared to ileal conduit.
Key words: Ileal urinary diversions, Quality of life, Sickness impact Profile (SIP) score.
1. INTRODUCTION
Although the post-operative morbidity analysis is simple for evaluation measuring the quality of life still represents an issue. Quality of life was a subject of medical research for over twenty years and now numerous authorities agree that measuring quality of life is the key measuring in clinical research. The main problem for all researchers within this field is the lack of universal accordance regarding definition of the quality of life term. The WHO concept defines the quality of life of an individual as individual perception of their position in life in the context of the culture and assessment of the system in which they live and in relations towards their goals, expectation, standards and worries. It’s a generally leveled concept deeply influenced by physical health of the person, his psychological status, the level of independence, social relations and their relation towards main characteristics of their environment (1). Quality of life describes and measures influence of a different conditions of everyday life and activities, taking in consideration emotional and social functions, as well as purely physical (2). In urologic surgery, urinary reconstructive surgery should be focused both on morbidity and quality of life of selected patients. The fact is that certain dilemmas exist regarding better quality of life in patients with orthotropic urinary derivation (3, 4), compared to ileal conduit or urinary derivation forms requiring urinary receptaculum and vice versa (5). The purpose of quality of life questionnaire is a supplement to objectification and quantification of clinical or biological disease measuring, evaluation of treatment quality, the need for healthcare intervention effectiveness and the patients’ contentment with the performed treatment. Nowadays there are numerous general quality of life questionnaires used as well as questionnaires related to a specific disease. Some are general (commonly used for urinary derivations), and the others are targeted for specific types of diseases(SF 36, Nottingham Health Profile, Health Assessment Questionnaire, Missoula-VITAS Quality of Life Index (MVQOLI), QLQ C30...) (6). In the lack of validated questionnaire which would be used for urinary derivations a question of comprehensiveness of such instrument is posed, which would consider all the problems influencing the quality of life in patients with urinary derivations. Sickness impact profile (SIP) questionnaire is designed to measure patients dysfunction through his everyday behavior, and generally related to disease. Since it measures general health status, it is appropriate in large number of disease. Each item has its value as well as total values of categories and dimensions. The general score of SIP categories or dimensions is multiplied by hundred obtaining the result in percentages, where 0% represents completely healthy patients, and 100% represents very difficult patients with a 100% dysfunction, completely dependent on another person in all aspects of life. It was developed in University of Washington in Seattle, USA. Nowadays it is used by numerous institutions in the world and it is the official quality of life questionnaire on Johns Hopkins University in Baltimore. Questionnaire consists of 136 YES/NO questions which represent specific activities divided in twelve general categories.
2. MATERIAL AND METHODS
In this prospective, clinical, analytical and comparative trial 106 patients were evaluated suffering from bladder invasive cancer who were separated into three groups and one more group consisted of 40 urological patients with minor symptoms used as control group for testing the comprehension of SIP score and to validate values of SIP score. In the bladder cancer group all patients were suffering from transitional cell cancer without distant metastasis or local recurrence. Research was conducted at the Urological Clinic of the Clinical Center University in Sarajevo in the period 2006 – 2012 in 106 patients aging from forty to eighty suffering from bladder invasive cancer, to which a radical cystectomy was indicated with one examined types of urine derivation. Patients were divided into three groups, with another control group of forty patients with minor chronic urological diseases.
Ileal conduit group
This group consisted of 66 patients, with diagnosed bladder cancer, and radical cystectomy and supravesical derivation with ileal conduit was performed.
Ghoneim/AbolEnein group
This group consisted of 20 patients suffering from invasive bladder antyreflux tunnel, upon radical cystectomy.
Hautmann group
This group consists of 20 patients suffering from invasive bladder cancer. These patients were treated with orthotopic derivation byHautmann, using 40 cm of terminal ileum, with uretherileal anastomosis by chimney. In order to simplify the interpretation of the results which were very similar, the Ghoneim/AbolEnein and cancer. These patients were treated with orthotopic derivation by AbolEnein and Ghoneim with serosa Hautmann-group was indicated as group A and Ileal conduit group as group B.
Control
This group consisted of 41 urological patients. These patients suffered from minor chronic conditions, which do not require any urological treatment (micro-lithiasis, cysts of epydidimis smaller than 1 cm, varicocele with regular spermatogram and without pain, chronic prostatitis and benign prostate hyperplasia with IPSS score under 8, kidney cysts under 2 cm…). This group was used only to test comprehension of the SIP score translation and as a control group to compare values of SIP score.
3. RESULTS
Cronbach Alpha indicates the level of internal reliability of the questionnaire. It is commonly used in the case of multiple questions which form the scale in order to determine reliability of the scale. Maximum coefficient value is 1, and any value above 0, 8 is considered highly reliable scale. Average value of this scale is 0, 938.
Average body care value in group B is 48,9, in group A 21,97 (Hautmann 20,93, Ghoneim 23,10), while in control group this value is 2,085. Value of mobility in group B is 30,026, in group A 10,97 (Ghoneim 23,010, Hautmann 20,93), control group 0,00.Value of walking in group B is 16,98, in group A 10,97 (Ghoneim 8,055, Hautmann 7,42), while in control group this item was not impaired at all, nor was the mobility. The total value of physical dimension of SIP score in group B was 95,79 in group A 40,68 (Ghoneim 42,25, Hautmann 39,11), while the value of physical dimension of SIP score in control group was 2,09. (Table 1, 2, 3).
Table 1.
Categories and dimensions of SIP score
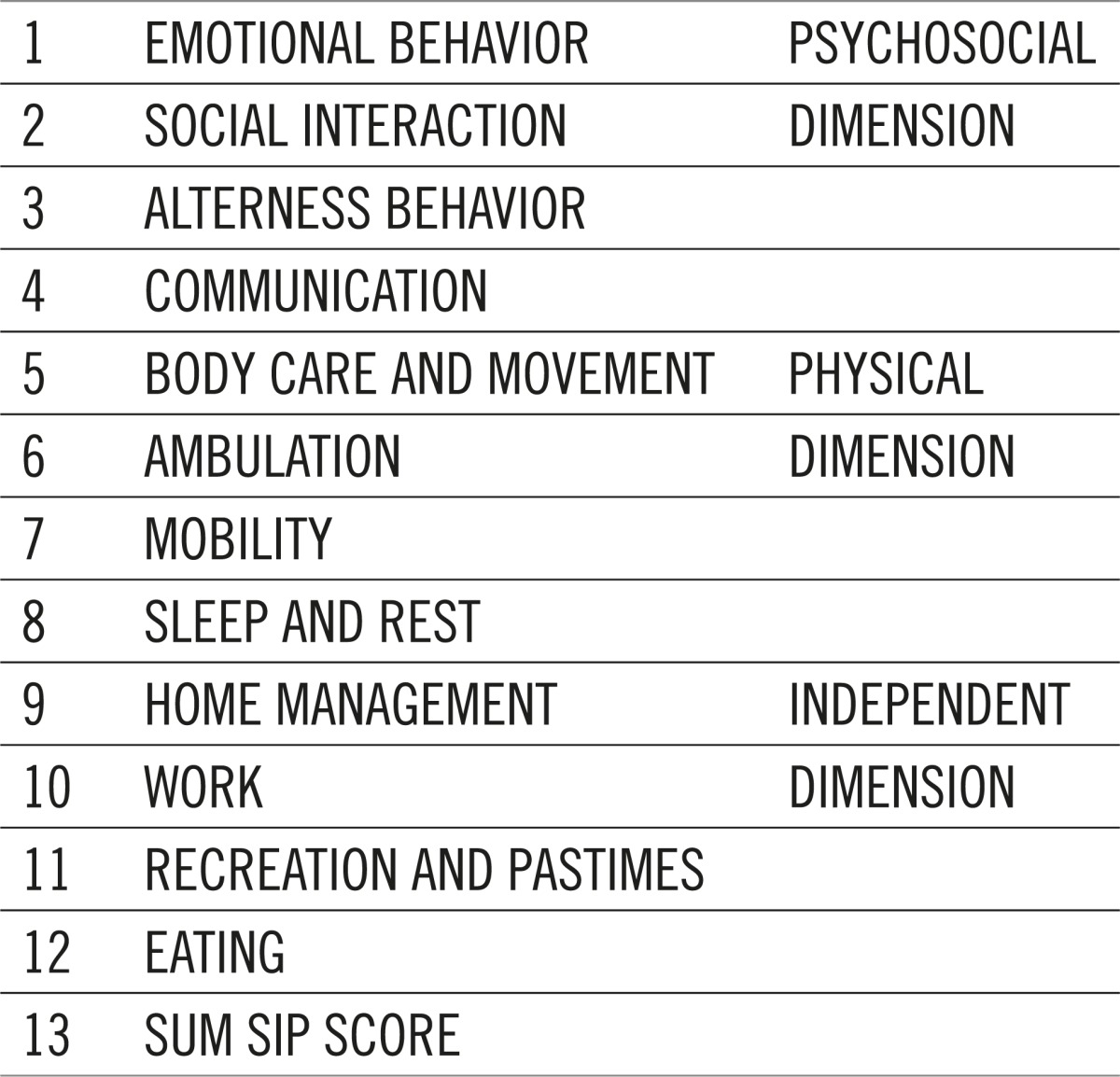 |
Table 2.
Questionnaire reliability
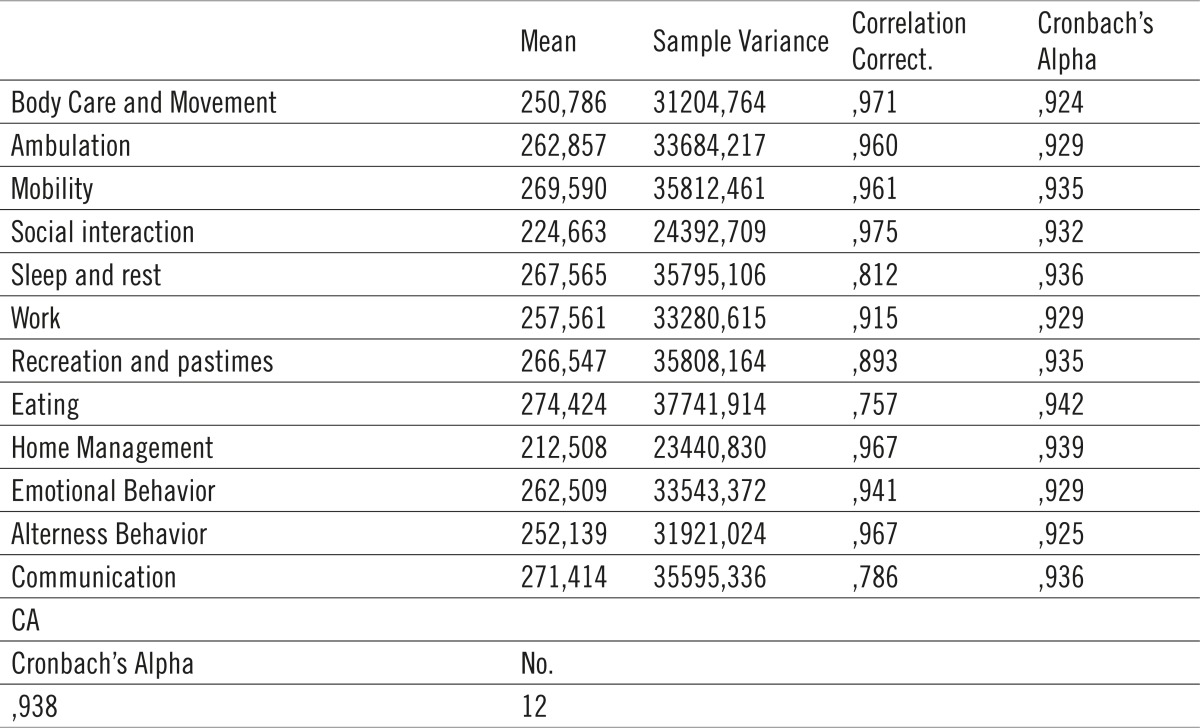 |
Table 3.
Values of all dimension and categories for urinary derivations
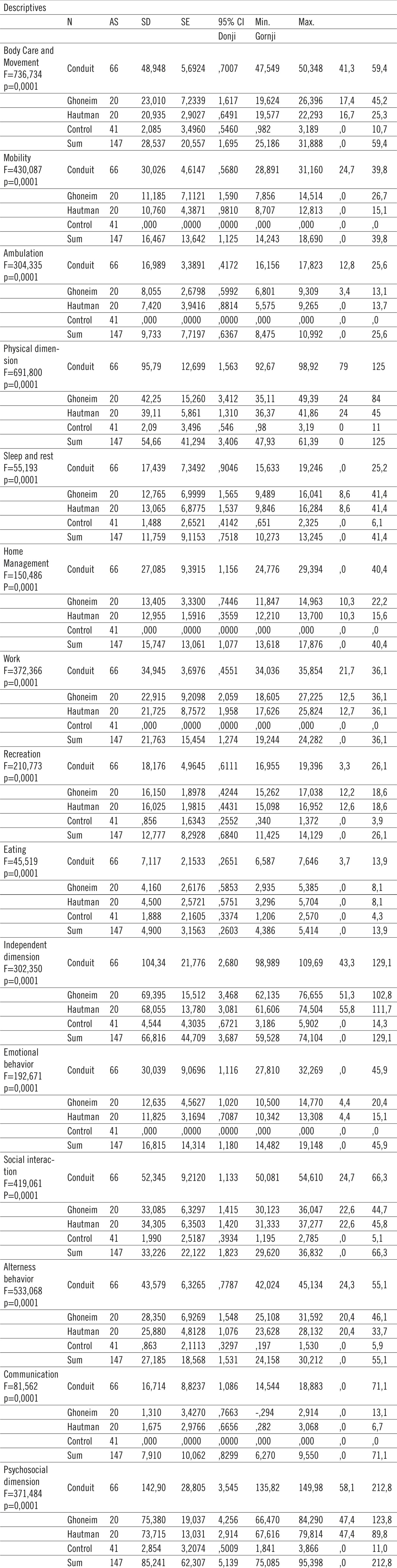 |
If independent dimension is taken into consideration and categories within it, we observed that mean value of relaxation sleep for group B is 17,43 while for group A is 12,91 (Ghoneim 12,76, Hautmann 13,065), control group 1,48. Mean value of domestic activities category for group B is 27,08, while for group A 13,18 (Ghoneim 12,95, Hautmann 13,405), control group 0. Mean value of the work category for group B is 34,94, for group A 22,3 (Ghoneim 22,19, Hautmann 21,72), the control group was not affected. Mean value of recreation category for group B is 18,76, for group A 16,088 (Ghoneim 16,150, Hautmann 16,025), in the control group recreation was practically not affected being 0,85. Mean value for food in group B is 7,11, while in group A is 4,33 (Ghoneim 4,1, Hautmann 4,5), control group mean value of this category is 1,88. Total value of independent dimension of SIP score is 104,342 for group B, while this value in group A is 68,72 (Ghoneim 69,39, Hautmann 68,055), for control group 4,54. Given psycho-social dimension examination, in the emotional behavior category mean value for group B is 30,039, in group A 12,230 (Ghoneim 12,635, Hautmann 11,285), control group 0. In social interaction category mean value for group B is 52,345, while for group A is 33,69 (Ghoneim 33,085, Hautmann 34,305). Control group 0,199. For behavior disorder category in group B mean value is 43,57, in group A 27,115 (Ghoneim 28,35, Hautmann 25,800), control mean value in this category is 0, 86. In communication category mean value for group B is 16,71, for group A is 1,49 (Ghoneim 1,31, Hautmann 1,67), in control group this value is 0. Total value for psyco-social dimension for conduit group is 142,903, for orthotropic derivation group is 74,54 (Ghoneim 75, 38, Hautmann 73,715), control group 2,85. (Graph 1).
Graph 1.
Total mean values of SIP score for urinary derivations presented percentages.
Multiplying mean values by 100 it can be obtain values of total SIP score in percentage, and for ileal conduit group 34,76%, for orthotropic derivation group 18, 4%, for control group 9,07%. Mean value by the type of operation at Ghoneim is 18,7% and at Hautmann 18,3% respectively.
4. DISCUSSION
During the last decade there has been a significant raise of interest for the quality of life in certain urological diseases. This phenomenon is especially considered in assessing the quality of life in patients with certain form of urinary derivation that was performed. Nowadays examination of the life quality becomes one of the most important factors in selecting the type of urinary derivation. Even today, the question related to the best solution for urinary derivation after radical cystectomy remains unclear. In current literature there is a notable advantage of orthotopic derivation compared to forms of cutaneous derivations. On the other hand, these “complicated” forms of derivation also have some weak points in a general assessment of the quality of life. Continent diversions demand more technical skills and longer operational time. Postoperatively, patients are discharged with permanent urinary catheter demanding longer recovery. Upon catheter extraction, patients will face incontinence and all of them will have to acquire techniques for adequate care of the new formed bladder reservoir. This education is essential whether or not this incontinence remains constant or temporary. Furthermore, patients with orthotopic derivation through longer period of time may face problems due to bowel dysfunction (diarrhea, vitamin B12 mal absorptive). In order to measure quality of life of those patients numerous trails were conducted. Those trails were limited because a randomized trail comparing quality of life of patients with conduit and those with orthotopic derivation was never performed.
In this questionary every question carries certain number of points. Since the questionnaire is validated certain questions carrie more points, meaning that these answers represent higher level of dysfunction. For instance answer “I tried to commit suicide” is more important than the answer “I indulge less in social activities”. In our examinees mean values of 12 general categories of SIP score divided by groups and operations are shown. Most commonly the answers related to body care category in ileal conduit group are “I stand only for short periods of time”, “I have trouble getting shoes, socks or stockings on”, “I do not have control of my bladder”, “I dress myself, but do so very slowly”, while the answer “I do not control of my bladder” was present in 20% of cases in orthotopic derivation group and is a direct consequence of derivation. This category depends entirely on disease stage and derivation in conduit group. The fact that they cannot control urinating was pointed out in 100% cases, which is a direct consequence of urinary derivation, while in 20% of cases the patients answered that they cannot control defecation. This answer directly reflects the extent of radical operation and the stage of disease. The question of incontinence has the biggest percentage of dysfunction for this category. Mobility category was not affected in control group. The most common answers in this category given by the patients from conduit group were “I am staying in bad most of the time”, “I stay home most of the time”, “I am going to places with restrooms nearby”, “I stay away from home only for brief periods of time”, “I am not using public transportation” while in orthotopic derivation group the most common answer was “I am not using public transportation”. Changes in conduit category could be related to disease and to age as well. Average age in conduit group is for ten years more than in orhotopic derivation group, so the majority of the patients from this group are retired or do not leave home on every day basis. The answer describing that they visit places with restrooms and stay longer in bad, most probably represents direct influence of disease stage and type of derivation. The most common answers in ambulation category given by the patients with ileal conduit were “I walk shorter distances or stop to rest often”, “I go up and down stairs more slowly” and “I walk more slowly”. In orthotopic derivation group the most common answers were “I walk more slowly” and “I go up and down stairs more slowly, for example, one step at a time, stop often” are probably related to the disease, and the one “I go up and down stairs more slowly, for example, one step at a time, stop often” is probably related to age of the patients from this group, although disease impact can not be excluded. According to physical dimension results, we can deduct that life impairment in group ileal conduit is bigger than life impairment in other two groups mostly because of the problems with body care. In independent dimension, the most common answer in rest (sleep) category for conduit group were “I sit around half-asleep”, “I spend much of the day lying down in order to rest” which could correlate to stage and derivation, but also to patients age, while in orhotopic derivation group the most common answer was “I sit during much of the day”, probably related to derivation.
The most common answers in home management category, given by the patients from the conduit group were “I do work around the house only for short periods of time or rest often”, “I am doing less of the regular daily work around the house that I would usually do”, “I am not doing any of the house cleaning that I would usually do”, which is again related to type of derivation, and could be related with psychological dimension in terms of patient indifference. In orthotopic derivation group most common answer was “I am doing less of the regular daily work around the house that I would usually do”, probably related to derivation. Control group did not answer this question.
The most common answers in work category regarding conduit group were “I am not accomplishing as much as usual at work”, “I am working shorter hours”,“I do not do my job as carefully and accurately as usual”. We would like to point out that majority of examinees from this group are retired, and these answers are related only to younger age out of this group, which is again related to derivation. It is interesting that the group with orthotopic derivation performed gave answers like “I am working shorter hours”, “I am working at my usual job but with some changes”. Although these patients have significantly lower SIP score it is still evident that they are aware of diagnoses, and for those with this derivation we tried to provide life as normal as possible. Most of the patients from this group are employed, so due to differences in ages of these patients being very important in this group, results should be taken into consideration with a certain dose of reserve. Patients in group of ileal conduit show that they are not contentious, probably aware that they can not function without the help of colleagues from work, but at home their nervousness comes to the fore.
In recreation and pastimes category in conduit group the most common answers were “I do my hobbies and recreation for shorter periods of time”, “I am going out for entertainment less often”, “I am doing more inactive pastimes in place of my usual activities”, “I am cutting down on some of my usual physical recreation or activities”, which is probably related to type of the derivation but to age as well. In orthotopic derivation group, the most common answers were “I am cutting down on some of my usual physical recreation or activities”, which is obviously related to type of derivation. This category has to be taken into consideration with reserve because of the patients’ age. It remains unclear was shorter recreation and pastime activities were present before the operation. Most common answers in eating category in ileal conduit group were “I am eating much less than usual”, “I am eating special or different food”, while the most common answers in orthotopic bladder group were “I am eating special or different food”. Those answers are directly related to operation and derivation, one due to bowel resection, and second due to type of disease. Upon being acknowledged that they suffer from cancer, the patients tend to eat healthy food in order to improve they condition. According to independent dimension results, it can be deducted that quality of life in group B is better than in group A primarily on the basis of work that they perform at home or in office.
The most common answers in emotional behavior category related to psychosocial dimension for ileal conduit group were “I say how bad or useless I am”, “I act nervous or restless”.. This is a direct consequence of derivation reminding patient with conduit on his diagnoses permanently. There is also very powerful orthotopic derivation patients’ answers like “I talk about the future in a hopeless way”, which is obviously related to diagnoses. Control group does not face this kind of problems.
In social interaction category, the most common answers for conduit group were “I am going out less to visit people”, “I show less interest in other people’s problems”, “I often act irritable toward those around me”, “I am doing fewer social activities with groups of people”, “My sexual activities is decreased”, “I often express concern over what might be happening to my health”, “I make many demands”, “I have frequent outbursts of anger at family members”, “I am not joking with family members as I usually do”. This category is completely related to derivation.
Due to unpleasant smell of urine or the thought that they disperse unpleasant smell, the patients avoid social interaction. This is one of the additional factors to develop depression at this type of patients. In orthotopic derivation group the most common answers were “My sexual activitiy is decreased”, “I’m not joking with family members as I usually do”. Thus, we can say that their derivation does not influence much on social interaction. Even is interesting that reduced sexual activity is more important than incontinence in this group.
The most common answers in alterness behavior category from the conduit group patients were “I am confused and start several actions at one time”, “I react slowly to things that are said or done”, “I make more mistakes than usual”, “I have difficulty doing activities involving concentration and thinking”. These statements are directly related to derivation, depression and loss of concentration and loss of interest for anything other than disease. In orthotopic derivation group, one most common answer were “I have difficulty doing activities involving concentration and thinking”. Therefore in orhotopic derivation group, the thought of disease has certain influence to higher SIP score. In communication category in ileal conduit group, the most common answers were “I carry on conversation only when very close to the other person or looking at him/her”, “I do not speak clearly when I am under stress”, which is again consequence of psychological impact of derivation and disease on the patients status. In orthotopic derivation group the only answer which was occasionally noted was “I carry on a conversation only when very close to the other person or looking him”.
Since the mean value of this dimension in conduit group is almost two times bigger compared to orthotopic derivation group, we may come to the conclusion that total quality of life in this type of derivation (conduit) is closely related to all categories of psych-social dimension. Similar results were found by McGuire and associates. They used validated questionnaire in 2000 patients to evaluate influence of certain forms of urinary diversions and general quality of life in loco regional patients treated for bladder cancer. Physical score was not different compared to population norm, but the mental score significantly decreased compared to published mental norms. Authors concluded that patients with ileal conduit have significantly low total mental quality of life while patients with continent forms do not. Furthermore they suggested that whenever is possible and when there is no medical contraindications, any form of orhotopic derivation should be performed (8).
General quality of life score is mostly influenced by body care, social interaction and behavior disorder, continuous unpleasant smell of urine from receptaculum which has a direct influence on social interaction. This is at the same time consequence of patients’ depression, which leads to loss of concentration and behavior disorder. This research proved that sexual indifference in ileal conduit group six months post operatively did not influence significantly general SIP score as much as urinary leak problem. The reason for this is the fact that six months after the surgery patients spent more time thinking about their disease than about sexual problem with receptaculum as a constant reminder. It is interesting that in orthotopic derivation group the problem of postoperative incontinence did not influence the SIP score at all, which proves that outer body appearance of the patient dominantly affects quality of life. From the SIP score results by categories and dimensions it is notable that ileal conduit group patients have lower quality of life compared to orhotopic derivation group.
5. CONCLUSION
Although extensive, SIP score with its 12 categories and three dimensions, provides us with comprehensive review and analysis of psychological and physical state of patient. By entering into details of everyday life having particular importance to SIP score, sometimes neglected by the patient, a comprehensive picture of the change of everyday behavior depending on patients’ disease is given. In this trail it is proven that orthotopic derivations are significantly comfortable for patients compared to those with ileal conduit. In lack of quality of life for urinary derivation questionnaire SIP score as a general questionnaire of disease impact on quality of life represents reliable alternative for objectification and quantification of quality of life after urinary derivation.
Conflict of interest
None declared.
REFERENCES
- 1.Carr AJ, Higginson IJ. Are quality of life measures patient centred? BMJ. 2001;322:1357–1360. doi: 10.1136/bmj.322.7298.1357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lee KT, Li MK, et al. The impact of a modified ileal neobladder on the lifestyle and voiding patterns in Asian patients. BJU. 1998;81:705–708. doi: 10.1046/j.1464-410x.1998.00586.x. [DOI] [PubMed] [Google Scholar]
- 3.Yoneda T, Igawa M, et al. Postoperative morbidity, functional results and quality of life of patients following orthotopic neobladder reconstruction. International Journal of Urology. 2003;10:119–125. doi: 10.1046/j.1442-2042.2003.00591.x. [DOI] [PubMed] [Google Scholar]
- 4.Hara I, Miyake S, et al. Health-related quality of life after radical cystectomy for bladder cancer: a comparasation of ileal conduit and orthotopic bladder replacement. BJU International. 2002;89:10–13. doi: 10.1046/j.1464-4096.2001.01475.x. [DOI] [PubMed] [Google Scholar]
- 5.Donald A. What are health-related quality of life analyses. What is Quality of life. 2003;1(9):1–4. [Google Scholar]
- 6.Short TG, Rowbottom MY, et al. Translation and calibration of a Chinese version of the Sickness Impact Profile for use in Hong Kong. HKMJ. 1998;4(4):375–381. [PubMed] [Google Scholar]
- 7.Bowling A. Measuring Health: A Review of Quality of Life Measurment Scales. Buckingham: Open University Press; 1997. [Google Scholar]
- 8.McGuire MS, Grimaldi G, Grotas J, Russo P. The type of urinary diversion after radical cystectomy significantly impacts on the patient’s quality of life. Ann Surg Oncol. 2000;7:4. doi: 10.1007/s10434-000-0004-2. [DOI] [PubMed] [Google Scholar]