Abstract
Introduction:
Studies indicate that using interventions including education may improve medical record documentation and decrease incomplete files. Since physicians play a crucial role in medical record documentation, the researchers intend to examine the effect of educational intervention on physicians’ performance and knowledge about principles of medical diagnosis recording among residents in Hormozgan University of Medical Sciences(HUMS).
Methods:
This quasi-experimental study was conducted in 2010 on 40 specialty residents (from internal medicine, obstetrics and gynecology, pediatrics, anesthesiology and surgery specialties) in Hormozgan University of Medical Sciences. During a workshop, guidelines for recording diagnostic information related to given specialty were taught. Before and after the intervention, five medical records from each resident were selected to assess physician performance about chart documentation. Using a questionnaire, physicians’ knowledge was investigated before and after intervention. Data were analyzed through one-way ANOVA test.
Results:
Change in physicians’ knowledge before and after education was not statistically significant (p = 0.15). Residents’ behavior did not have statistically significant changes during three phases of the study.
Conclusion:
Diversity of related factors which contributes to the quality of documentation compels portfolio of strategies to enhance medical charting. Employing combination of best practice efforts including educating physicians from the beginning of internship and applying targeted strategy focus on problematic areas and existing gap may enhance physicians’ behavior about chart documentation.
Key words: diagnosis writing, medical record, medical records departments, documentation, education, residency training, performance change.
1. INTRODUCTION
The medical record works as a primary tool in providing high quality patient care, preventing disease, hospital revenue and reimbursement, legal aspects and medical research and education (1). Therefore, all caregivers that contribute in patient care must document their services in medical record to support broad spectrum of medical record usages (2). Huffman believes that “Information is life blood of health care organization” (3). In this context, diagnostic information accounts for the main part of medical record and documents in form of medical diagnosis (4). Medical diagnosis intend to describe patient care and its outcome, and physicians take the primary responsibility to record it in medical record (5, 6). Therefore, undertaking actions to improve physician behavior regarding medical record documentation has been emphasized in numerous studies (7-10).
Most methods to enhance physician behaviors regarding medical record documentation highlighted on knowledge, beliefs, attitudes, skills, and social norms (11, 12). These methods include continuing medical education (13) in term of formal credits, academic detailing (13), guidelines (14), chart audit and feedback (15). Education is one of the most effective mechanisms to enhance chart documentation among physicians (7, 8). American Health Information Management Association (AHIMA) believes that education of health care practitioners can improve clinical documentation practices (9). Studies conducted in Iran indicated that medical record suffers from various problems in form of inaccuracy, incompleteness and illegibility (17-20). Mashofee believed that physician documentation was poor in Ardebil (21). Moghaddasi revealed that lack of physician’s knowledge resulted in inaccurate medical diagnosis and chart documentation (22). To fill this knowledge gap, the current study sought to evaluate the effect of educational intervention on knowledge and performance of residents of Hormozgan University of Medical Sciences (HUMS) medical chart documentation.
2. METHODS
We conducted a quasi-experimental study in HUMS in south of Iran. Total residents who were accepted at HUMS in 2010 participated in this study. There were 40 residents in different subspecialties including Internal (7), pediatrics (8), pathology (5), obstetrics (8), surgery (8) and anesthesiology (4).
The study included three parts: a retrospective review about physicians’ chart documentation and physicians’ knowledge, an educational intervention, and a prospective analysis of physician behaviors and knowledge following the intervention after one month and three months.
In retrospective phase, the residents’ knowledge and behavior about medical records documentation were assessed. In pretest phase, up to five medical records from each physician were randomly selected and reviewed by two reviewers who were blinded to the physician identification and intervention. A checklist was employed to collect information about medical record documentation. Physicians’ knowledge about medical record documentation was investigated through the self-administered questionnaire in pretest phase.
In intervention phase, a multidisciplinary team including physicians and health information management professionals were launched. The team members found charts problematic areas related to recording diagnostic information. Educational content and objective were formulated based on International Classification of Diseases (ICD) recording principals of medical diagnosis.
The final phase of the research project was conducted one month after the educational session to determine the physicians’ knowledge and behavior about medical record documentation. The same process was directed in prospective phase to assess impact of educational intervention on physicians’ knowledge and behavior about chart documentation. This process continued three months later to verify if the behavior changes had been sustained. Collected data were analyzed through one-way ANOVA by using SPSS software.
3. RESULTS
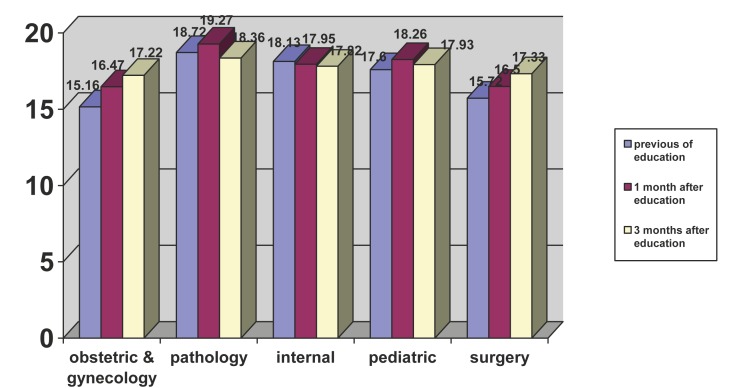
Figure 1 indicates that chart documentation was high before and after educational intervention in pathology residents in comparison with other specialties. Compliance in charting for internal medicine was similar before and after educational intervention. Gynecology residents had the lowest level of chart documentation before and after educational intervention.
Figure 1.
Residents’ behavior of chart documentation.
Residents’ behavior did not have statistically significant changes during three phases of the study (p = 0.15).
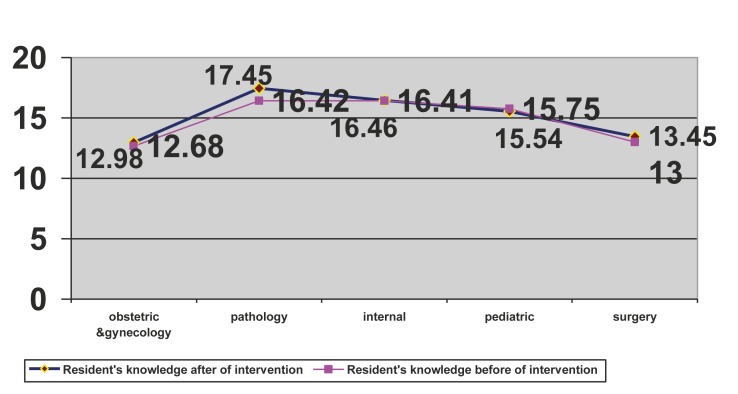
Figure 2 reveals that pathology residents had the highest level of knowledge about chart documentation before and after educational intervention. Gynecology residents had the minimum level of knowledge before and after intervention. Altogether, change in physicians’ knowledge before and after education was not statistically significant (p= 0.15).
Figure 2.
Resident’s Knowledge before and after eductational intervention.
4. DISCUSSION
The current study revealed that educational materials were not effective mechanisms to change resident behavior and knowledge. Previous literature has indicated educational sessions to be an efficient strategy to enhance resident behavior, whereas other researches have not. O’Brien found that educational intervention may be used to improve documentation of a proper foot examination. Findings of Tinsley were consistent with O’Brien’s study (23). Tinsley indicated that educational intervention which is conducted by a multidisciplinary team can improve resident performance about charting (7).
Unlike previous studies, Socolar showed that directed educational campaign did not seem to improve medical record documentation significantly. Socolar argued that chart audits and tailored feedback may not be the best way to improve physician behavior; credits in continuing medical education and use of structured records may be more likely to be effective (8). Previous studies believed in the possible effect of staging residents on their behavior (7).
If educational intervention occurred in the first year, their behaviors would improve as they progressed, and their charting may have improved according to their growing experience (7). Employing positive incentive programs for timely record completion may provide another strategy to improve chart documentation. Pines indicated that after implementation of incentive method, chart documentation increased significantly from 2.86 and 3.04 to 3.31, and this improvement was maintained 3 months after the plan (9). Another study emphasized the role of physician engagement and awareness about patient safety risk and financial impact of miscoding to enhance physician chart documentation behavior (24).
Varelas argued that the quality of documentation depends on the practice setting, physician and patient characteristics and measures used. In this study, the impact of an appointed Neurointensivist (NI) on medical record documentation in Neurological Intensive Care Unit (NICU) was examined. The results of the study revealed a significant improvement (from 32.5 % to 57.5%) in medical record documentation (25). Farzandipour indicated that the accurate medical record requires support of medical record committees at hospitals (26). Karami collected related factors in medical record documentation and solutions from physicians and managers viewpoints and realized that physicians and administrators believed in audit and control as an effective strategy to enhance medical records documentation (27). Smith also insisted on the initial training program enhances the skills of doctors and medical staff to record. In this regard, 10 major medical problem should be considered in training (16).
In this context, AHIMA suggests a variety of best practices in medical record documentation including using incentive program, redesigning forms; periodically analyzing records, and establishing physicians preferred appointment day and time to facilitate their access to complete medical record (16).
5. CONCLUSION
Whereas the quality of documentation differs based on physician, patient and practice setting utilizing single intervention in terms of education does not enhance medical charting.
Employing combination of best practice efforts including trying out education intervention at the beginning of physician course i.e. internship may improve their behavior as the year passes. Applying targeted strategy focus on problematic areas and existing gap such as knowledge insufficiency, tailored feedback, incentive programs, etc may enhance physicians’ behavior about chart documentation.
Experience obtained in this study showed that the detection of the training program should be accompanied by the following. Documentation in the form of pamphlets and guides are provided to physicians, residents, as well as educational posters for the tips be installed.
We hope this can be enhanced skills and knowledge in the medical record documentation.
Acknowledgments
The authors thank Sh. Zare, T. Baniasadi, and F. Ghovvatti, for their great help in data analysis. In addition, the authors thank all the coders who participated in the study.
Financial Support
The research was support from the vice chancellor for research at Hormozgan University of Medical Sciences in Bandarabbas, Iran.
Conflict of interest
None declared.
REFERENCES
- 1.Sakharkar BM. Principles of hospital administration and planning. Bangalore: Medical Publisher’s; 1998. [Google Scholar]
- 2.Davis N, La Cour M. Introduction to Health information technology. Philadelphia: WB Saunders Company; 2002. [Google Scholar]
- 3.Huffman E. Health Information Management. Tenth Edition. Berwyn, Illinois: Physicians’ Record Company; 1994. [Google Scholar]
- 4.Mann R, Williams J. Standards in medical record keeping. Clin Med. 2003;3(4):329–332. doi: 10.7861/clinmedicine.3-4-329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Belcher DW, Berg AO, Inui TS. Practical approaches to providing better preventive care: are physicians a problem or a solution? Am J Preu Med. 1988;4:27–48. [PubMed] [Google Scholar]
- 6.Fox RD, Mazimanian PE, Putnam RW. Changing and Learning in the Lives of Physicians. New York, NY: Praeger; 1989. [Google Scholar]
- 7.Tinsley JA. An educational intervention to improve residents’ inpatient charting. Acad Psychiatry. 2004;28(2):136–139. doi: 10.1176/appi.ap.28.2.136. [DOI] [PubMed] [Google Scholar]
- 8.Socolar RR, Raines B, Chen-Mok M, Runyan DK, Green C, Paterno S. Intervention to improve physician documentation and knowledge of child sexual abuse: a randomized, controlled trial. Pediatrics. 1998;101(5):817–824. doi: 10.1542/peds.101.5.817. [DOI] [PubMed] [Google Scholar]
- 9.Pines JM, Reiser RC, Brady JW, Braithwaite SA, Ghaemmaghami CA, Cardella K, et al. The effect of performance incetives on resident documentattion in an emergency medicine residency program. The Journal of emergency medicine. 2007;32(3):315–319. doi: 10.1016/j.jemermed.2006.07.028. [DOI] [PubMed] [Google Scholar]
- 10.Soumerai SB, Avorn J. Principles of educational outreach (academic detailing) to improve clinical decision making. JAMA. 1990;263:549–556. [PubMed] [Google Scholar]
- 11.Davis DA, Thomson MA, Oxman AD, Haynes RB. Changing physician performance: a systematic review of the effect of continuing medical education strategies. JAMA. 1995;274:700–705. doi: 10.1001/jama.274.9.700. [DOI] [PubMed] [Google Scholar]
- 12.Audet AM, Greenfield S, Field M. Medical practice guidelines: current activities and future directions. Ann Intern Med. 1990;113:709–714. doi: 10.7326/0003-4819-113-9-709. [DOI] [PubMed] [Google Scholar]
- 13.Lomas J, Enkin M, Anderson GM, Hannah WJ, Vayda E, Singer J. Opinion Leaders vs. audit and feedback to implement practice guidelines. JAMA. 1991;265:2202–2207. [PubMed] [Google Scholar]
- 14.Fatzinger P, Kammer A, Garrett M. Development and use of preprinted forms and adhesive labels in medical record charting. J AM Diet Assoc. 1992;92:982–985. [PubMed] [Google Scholar]
- 15.Humphreys T, Shofer FS, Jacobson S, Coutifaris C, Stemhagen A. Preformatted charts improve documentation in emergency department. Ann Emerg Med. 1992;21:534–540. doi: 10.1016/s0196-0644(05)82520-x. [DOI] [PubMed] [Google Scholar]
- 16.AHIMA body of knowledge. Best Practices in Medical Record Documentation and Completion. Available from: http://library.ahima.org/xpedio/groups/public/documents/ahima/bok1_000043.hcsp?dDocName=bok1_000043 . [2012 Feb 4].
- 17.Balaghafari A, Siamian H, Aligolbandi K, Zakeezadeh M, Kahooei M, Yazdani Charati J, et al. Determine knowledge, attitude and performance of medical students toward the educational qualifications of the medical records of Mazandaran University of Medical Sciences and Health Services. 2006;15(49):77–84. [Persian] [Google Scholar]
- 18.Ebrahimi P. Study of the Rate Of Commitment to The Standards In Medical Record Department of Social Security Hospitals Located In Tehran. [Dissertation] Iran: Iran University of Medical Sciences; 1997. [Google Scholar]
- 19.Asadi F. Evaluation of quality of patient records in educational hospital of Iran university of medical sciences. [Dissertation] Iran: Iran University of Medical Sciences; 1998. [Google Scholar]
- 20.Hajavi A, Azar FE, Meidani Z. Medical records standards in selected countries and Iran: a comparative study. New J (Inst Health Rec Inf Manag) 2005 Feb;46(1):4, 6. [PubMed] [Google Scholar]
- 21.Mashoufee M, Amanee F, Rostamee KH. Detailed evaluation of the teaching hospitals of Ardabil University of medical sciences. Journal of Ardabil University of Medical Sciences. 2007;4(1):43–49. [Persian] [Google Scholar]
- 22.Moghaddasi H, Hoseini A, Shahi M. Study of how to organize health care information in hospitals affiliated to Medical and Health Services Universities in Tehran. Journal of Paramedical Sciences. 2003;3(7):357–362. [Persian] [Google Scholar]
- 23.O’Brien KE, Chandramohan V, Nelson DA, Fisher JR, et al. Effect of a physiciandirected educational campaign on performance of proper diabetic foot exams in an outpatient setting. J Gen Iintern Med. 2003;18:258–265. doi: 10.1046/j.1525-1497.2003.10662.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nallasivan S, Gillott T, Kamath S, Blow L, Goddard V. Physician involvement enhances coding accuracy to ensure national standards: an initiative to improve awareness among new junior trainees. J R Coll Physicians Edinb. 2011 Jun;41(2):106–108. doi: 10.4997/JRCPE.2011.220. [DOI] [PubMed] [Google Scholar]
- 25.Varelas PN, Spanaki MV, Hacein-Bey L. Documentation in medical records improves after a neurointensivist’s appointment. Neurocrit Care. 2005;3(3):234–236. doi: 10.1385/NCC:3:3:234. [DOI] [PubMed] [Google Scholar]
- 26.Farzandipour M, Asef Zadeh S. Evaluation of recording diagnosis principals in Kashan University’s Hospitals. Fayz. 2004;8(31):36–44. [Google Scholar]
- 27.Karami M, Shokrizadeh Arani L. Related Factors in Medical Records Documentation Quality and Presenting Solutions from Managers’ and Physicians’ Viewpoints Occupied in Hospitals Affiliated to Kashan University of Medical Sciences. Iranian Journal of Medical Education. 2010;9(4):356–364. [Google Scholar]