Abstract
Objective
The increased use of bypass surgery in the treatment of ischemic cerebrovascular diseases requires a better understanding of the superficial temporal artery (STA) anatomy. This study is to describe the gross anatomy of STA in adult Korean population with respect to cranial surgery and to provide basic anatomic data for bypass surgery.
Methods
The study evaluated retrospectively 35 patients who visited the neurosurgery department at a single institution. For each patient, both the left and right STA (70 vessels) were evaluated by a 3-dimensional computed tomographic angiogramfor diameter and anatomic relationships to external landmarks.
Results
Of 70 STAs, 69 had a bifurcation. Among these, 57 (82.6%) were above the superior margin of the zygomatic arch. The STA bifurcation was 53.2 ± 5.9 mm posterior to the keyhole, 9.5 ± 5.3 mm anterior to the posterior margin of condylar process of the mandible, and 21.7 ± 15.8 mm superior to the superior margin of the zygomatic arch. The inner diameter of the STA was 1.8 ± 0.5 mm at the superior margin of the zygomatic arch, and 1.4 ± 0.4 mm and 1.4 ± 0.5 mm for frontal and parietal branches, respectively. The 75.7% of frontal and 66.7% of parietal branches were suitable for microvascular anastomosis.
Conclusion
This present study demonstrated the STA in Korean adults, which may benefit the clinician in dealing with the surgical procedures related to this STA.
Keywords: Carotid artery, External, Temporal arteries
INTRODUCTION
The superficial temporal artery (STA) is one of the terminal branches of the external carotid artery (ECA). It supplies the face and scalp together with other branches of the ECA. The STA is one of the primary bypass conduits used to distally perfuse the brain in ischemic cerebrovascular disease or an intracranial complex lesion, and for this reason, the importance of understanding the anatomy of the STA is growing. Ethnic anatomic differences may exist for the STA,2) but the gross anatomy of the STA in Korean adult population has not been reported in detail.
The outer diameter of STA has been generally investigated by cadaver studies,1-5) and only 1 study reports the inner diameter by the use of conventional angiogram.7) The objective of this study was to evaluate the distance of STA bifurcation from the superior margin of the zygomatic arch, keyhole, and posterior margin of mandibular condyle in adult Korean population. Additionally, the inner diameters of STA were evaluated, and suitable branches for microvascular anastomosis were investigated.3),7)
METHODS
Thirty five patients who visited the neurosurgery department at our institution due to vascular diseases were evaluated retrospectively in this study. In each patient, the both left and right STAs were evaluated, for a total of 70 STAs.
The location of the STA bifurcation around the zygomatic arch was classified as one of the following: above the superior margin of the zygomatic arch, over the zygomatic arch, or below the inferior margin of the zygomatic arch.
The distance of STA bifurcation were also evaluated from other cranial landmarks, for example the superior margin of the zygomatic arch, posterior margin of condylar process of the mandible, and keyhole (Fig. 1). The inner diameter of STA was measured at the superior margin of the zygomatic arch, 1 cm above the superior margin of the zygomatic arch, 1 cm below bifurcation, and 1 cm distal from bifurcation to the frontal and parietal branches. To analyze suitable sites for bypass surgery, the inner diameter of STA branches were also measured at a point 7 cm distal from the superior margin of the zygomatic arch.
Fig. 1.
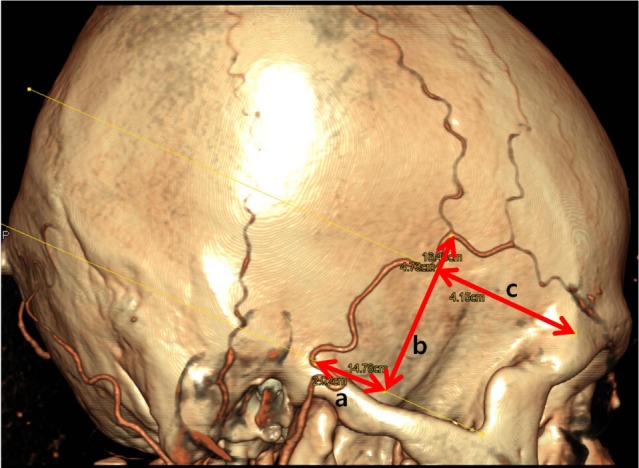
Location of the superficial temporal artery (STA) bifurcation. The relationship between STA and pericranial structures. (a: distance from the posterior margin of the mandibular condyle, b: distance from the superior margin of the zygomatic arch, c: distance from the keyhole).
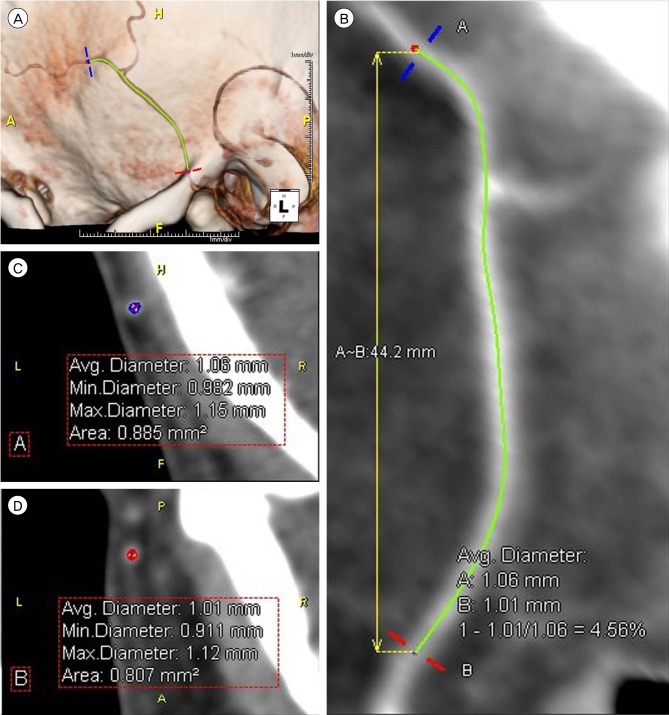
The images were obtained using a 3-dimensional computed tomographic angiogram (3D CTA) (Siemens Definition AS plus 128 channel CT) system. Pre-scan contrast consisting 50 cc of iohexol (Bonorex, Dai Han Pharm. Co. LTD., Seoul, Korea) was injected into the cephalic vein at 5 cc/sec, and the scan was commenced after 17 seconds. A program, Aquarius iNtuition edition ver. 4.4.6 (TeraRecon Inc., Foster, CA, USA), was used to measure the diameter of the STA (Fig. 2). Because histographic adjustment alters the vessel dimensions, source images were processed and respective measurements made without histographic adjustment. Statistical analysis was performed using SPSS 12.0 KO for Windows (SPSS Inc., Chicago, IL, USA). Null hypotheses of no difference were rejected if p values were less than 0.05.
Fig. 2.
Anatomic dimensions of superficial temporal artery (STA). Using the data from 3-dimensional computed tomography angiogram, the length and diameter of each STA was measured without histographic adjustment. (A) If 2 points (blue and red) were assigned, (B) the program automatically calculated the length between these 2. (C, D) In addition, the average diameter was calculated automatically for these points.
RESULTS
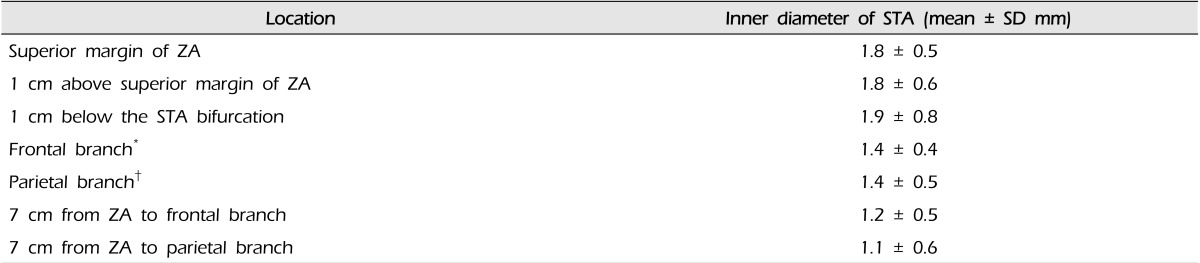
The mean age of the 35 subjects was 58.9 years (± 10.8) with a range from 35 to 82. Among the 70 studied, 69 STAs had at least 1 bifurcation with 1 STA having only the frontal branch. Fifty-seven (82.6%) STAs had bifurcations above the superior margin of the zygomatic arch; 7 (10.1%) over the zygomatic arch; and 5 (7.2%) had bifurcations below the inferior margin of the zygomatic arch (Table 1).
Table 1.
The location of STA bifurcation
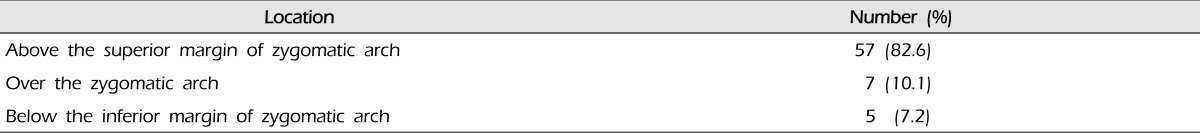
Sixty nine STA had bifurcation among 70, 1 had only frontal branch. STA= superficial temporal artery.
The location of STA bifurcation was 9.5 (± 5.3) mm anterior to the posterior margin of the mandibular condyle, 21.7 (± 15.8) mm superior to the superior margin of the zygomatic arch, and 53.2 (± 5.9) mm posterior to the keyhole (Table 2, Fig. 1).
Table 2.
The location of STA bifurcation relative to pericranial structures
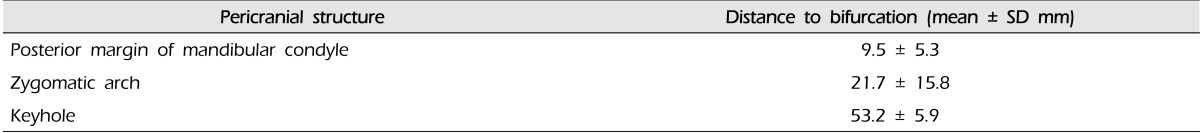
STA= superficial temporal artery; SD= standard deviation.
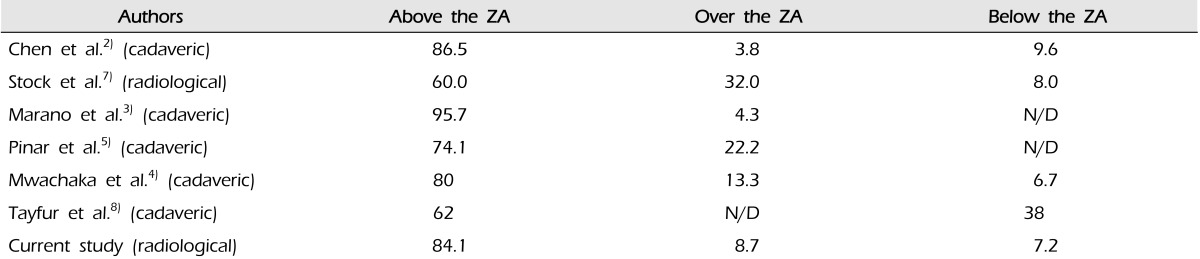
The mean inner diameter of STAs was 1.8 ± 0.5 mm at the superior margin of the zygomatic arch, 1.8 ± 0.6 mm at 1 cm above the superior margin of the zygomatic arch, and 1.9 ± 0.8 mm at 1 cm below the bifurcation. The diameters of the frontal and parietal branches were 1.4 ± 0.4 mm and 1.4 ± 0.5 mm at 1 cm distal from bifurcation, respectively. The diameter of the same frontal and parietal branches were 1.2 ± 0.5 mm and 1.1 ± 0.6 mm at 7 cm distal from the superior margin of the zygomatic arch, respectively (Table 3).
Table 3.
Inner diameter of STA
*Frontal branch was measured at 1 cm distal from bifurcation to frontal branch, †Parietal branch was measured at 1 cm distal from bifurcation to parietal branch. STA= superficial temporal artery; SD= standard deviation; ZA= zygomatic arch.
Suitable branches of STA for bypass surgery are defined as having a diameter larger than 1 mm with a length greater than 70 mm from the superior margin of the zygomatic arch.3),7) By this criteria, 53/70 (75.7%) of the frontal branches of the STA were suitable, and 46/69 (66.7%) of the parietal branches were suitable in this study. Additionally, 33/70 (47.1%) of STAs had both suitable branches.
DISCUSSION
The superficial temporal artery arises from the external carotid artery. It runs along the posterior margin of the condylar process of mandible, and crosses the posterior root of the zygomatic process of the temporal bone.1),9) Above the zygomatic arch, it divides into 2 large terminal branches. The anterior branch is called the frontal branch and courses anterosuperiorly. The posterior branch is called the parietal branch and is directed posterosuperiorly.6) During cranial surgery, understanding its anatomic relationship with specific landmarks of the pericranial region is helpful in identifying the location of both the artery itself and the point of bifurcation.
The STA usually bifurcates at a point above the superior margin of the zygomatic arch, and the results of our study are similar to others from the literature regarding STA anatomy (Table 4). Mwachaka et al.4) used the zygomatic arch, lateral canthus, and the tragus as a land mark. Chen et al.2) used the zygomatic process and external auditory canal. In this study, posterior margin of the mandible condyle, superior margin of the zygomatic arch, and keyhole were used as 3 landmarks to detect the location of the STA bifurcation, because these are readily identifiable in the operative field. In this study, the standard deviations for the location measurements were relatively high, and reveal that the STA anatomy has many variations. However, this approximation is still adequate in understanding STA anatomy and in identifying the location of bifurcation, helpful in preserving the STA during a cranial operation.
Table 4.
Bifurcation point of the STA in literature (%)
STA= superficial temporal artery; ZA= zygomatic arch; N/D= no data.
The diameter of the STA at superior margin of the zygomatic arch was 1.8 ± 0.5 mm. The diameters of STA at the point of bifurcation is variable, and this diameter was measured at a point 1 cm below the bifurcation, where it was slightly larger (1.9 ± 0.8 mm) than at the super margin of zygomatic arch. As the STA passes through the connective tissue around the zygomatic arch, it takes on a hairpin shape to allow flexibility for the movements of mastication. This appears to be why the distal artery has a larger diameter than that of the proximal portion. Furthermore, 12 STAs in this study were found to bifurcate over or below the zygomatic arch. In these cases, the proximal STA bifurcation has a larger diameter than it does at the distal zygomatic arch. In fact, among the 57 STAs with bifurcations above the zygomatic arch, the diameter at 1 cm below the bifurcation was 1.7 ± 0.5 mm. Some studies have found that the diameter of the parietal branch is larger than that of the frontal branch. However, we did not find any significant difference in the diameter of frontal and parietal branches.
In this study, the STA diameter at the zygomatic arch was 1.8 ± 0.5 mm, but others have reported the STA diameter at the same location to be between 2.0 mm to 2.7 mm (Table 5). This difference can be explained by the differences in study design. In previous reports, these measurements were obtained in cadaver studies with the STA expanded by preservative fluids, whereas contrasted CT angiogram in live human subjects was used in our study. In our case, the STA measurement may have been made during either systole or diastole; and therefore, the measurements made on a pulsating artery could be smaller than the artificially expanded artery from cadaver studies. Furthermore, the study measurements on CT images were for inner diameter of the artery, whereas the measurements made in cadaver studies was that of the outer diameter and included the thickness of the vessel wall into the overall diameter. In a study by Stock et al.,7) the average diameter of STA at the zygomatic arch was 2.0 ± 0.3 mm in cadavers and was 1.9 ± 0.7 mm in a radiologic study in live human subjects. In that study, the radiologic diameters were smaller by 5% at the zygomatic arch, 18% at the frontal branch, and 28% at the parietal branch, when compared with those measurements from cadavers. Chen et al.2) reported a cadaveric study on STA anatomy in Chinese population. In that study, the STA diameter was 2.1 ± 0.5 mm at the zygomatic arch, 1.6 ± 0.2 mm at the frontal branch, and 1.7 ± 0.2 mm at the parietal branch (Table 5). The STA measurements in this study of Korean population were smaller than the Chinese equivalent by 14% at the zygomatic arch, 12% at the frontal branch, and 18% at the parietal branch, respectively, at the zygomatic arch, frontal and parietal branches. When taking into consideration the difference between inner and outer diameter measurements, the anatomic dimensions of STA appears similar across these 2 populations. Furthermore, STA diameters in the East Asian population, which includes Chinese or Korean ethnic groups, appear to be less than that of western populations.
Table 5.
Diameters of STA (mm)
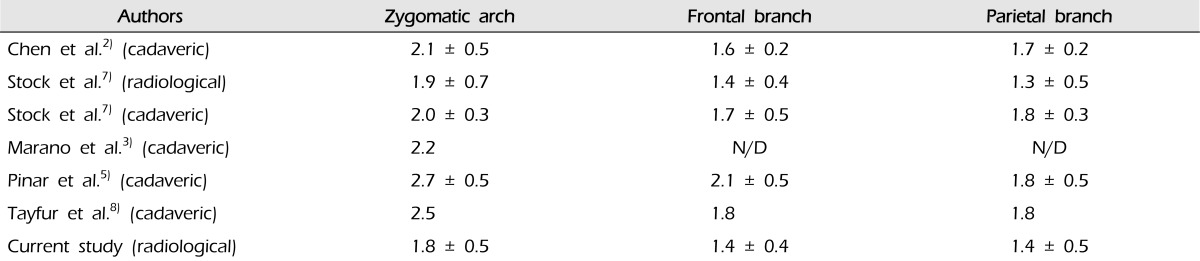
Stock et al.7)(radiological) and current study measured inner diameters of the superficial temporal artery of living people, but other's measured outer diameters of cadavers.
Suitable branches of STA for bypass surgery are defined as having a diameter larger than 1 mm with a length greater than 70 mm from the superior margin of the zygomatic arch.3),7) By these criteria, 75.7% of the frontal branches and 65.7% of the parietal branches were suitable for bypass surgery in this population. In comparison, Marano et al.3) and Pinar et al.5) reported higher rates of suitability in their populations (Table 6). This discrepancy suggests that a smaller proportion of Korean patients requiring bypass operation may have a suitable STA compared to patients elsewhere. Further, we measured the inner diameter of the STA branch, so the thickness of the vessel walls presumably accounts for some parts of the difference.
Table 6.
Percentage of STA suitable for use in bypass (%)
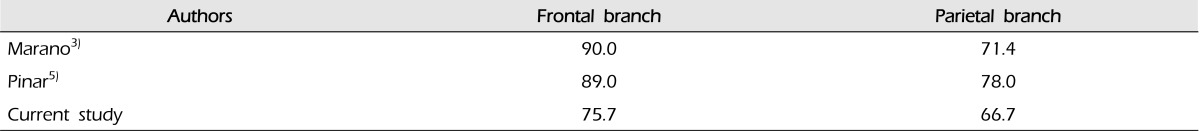
In our study, one case did not have a parietal branch. Thus, the proportion of frontal branches was 53 out of 70, whereas that of parietal branches was 46/69. STA= superficial temporal artery.
The rate of suitable branch of the frontal STA was bigger than the parietal branch (Table 6). However, there was no significant difference between them.
To save the STA during cranial surgery, we drew the imaginary line of the STA considering the relationship with pericranial structures and CTA, then dissected carefully from the distal part. We undermined over it pulling the skin by forcep, if it met STA trunk or branch. Saving STA trunk is critically important, and the skin incision would be posterior to STA trunk rather than anterior at tragus level.
The limitation of this study is selection of patients. Among the patients evaluated in this study, there were 13 with hemorrhagic diseases, 8 ischemic diseases, 11 with unruptured aneurysms, and 3 with meningiomas. Most patients had vascular disease, and more studies are needed whether patients with vascular disease have more atherosclerosis.
CONCLUSION
The location of STA bifurcation was 9.5 ± 5.3 mm anterior to the posterior margin of the mandible condyle, 21.7 ± 15.8 mm superior to the superior margin of the zygomatic arch, and 53.2 ± 5.9 mm posterior to the keyhole. The diameter of STA measured in the adult Korean population is less than that published for Western populations. However, our result is similar to the findings reported in the Chinese population. Considering the high standard deviations of STA anatomy, 3D CTA study might be helpful in the preoperative setting. Even if the image modality is not available however, a better understanding of the STA anatomy in its relationship to the landmark structures would help to preserve this important artery during a cranial operation.
References
- 1.Abul-Hassan HS, von Drasek Ascher G, Acland RD. Surgical anatomy and blood supply of the fascial layers of the temporal region. Plast Reconstr Surg. 1986 Jan;77(1):17–28. [PubMed] [Google Scholar]
- 2.Chen TH, Chen CH, Shyu JF, Wu CW, Lui WY, Liu JC. Distribution of the superficial temporal artery in the Chinese adult. Plast Reconstr Surg. 1999 Oct;104(5):1276–1279. doi: 10.1097/00006534-199910000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Marano SR, Fischer DW, Gaines C, Sonntag VK. Anatomical study of the superficial temporal artery. Neurosurgery. 1985 Jun;16(6):786–790. doi: 10.1227/00006123-198506000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Mwachaka P, Sinkeet S, Ogeng'o J. Superficial temporal artery among Kenyans: Pattern of branching and its relation to pericranial structures. Folia Morphol (Warsz) 2010 Feb;69(1):51–53. [PubMed] [Google Scholar]
- 5.Pinar YA, Govsa F. Anatomy of the superficial temporal artery and its branches: Its importance for surgery. Surg Radiol Anat. 2006 Jun;28(3):248–253. doi: 10.1007/s00276-006-0094-z. [DOI] [PubMed] [Google Scholar]
- 6.Sinna R, Hajji H, Qassemyar Q, Perignon D, Benhaim T, Havet E. Anatomical background of the perforator flap based on the deep branch of the superficial circumflex iliac artery (SCIP Flap): A cadaveric study. Eplasty. 2010 Jan;10:e11. [PMC free article] [PubMed] [Google Scholar]
- 7.Stock AL, Collins HP, Davidson TM. Anatomy of the superficial temporal artery. Head Neck Surg. 1980 Jul-Aug;2(6):466–469. doi: 10.1002/hed.2890020604. [DOI] [PubMed] [Google Scholar]
- 8.Tayfur V, Edizer M, Magden O. Anatomic bases of superficial temporal artery and temporal branch of facial nerve. J Craniofac Surg. 2010 Nov;21(6):1945–1947. doi: 10.1097/SCS.0b013e3181f4ee6a. [DOI] [PubMed] [Google Scholar]
- 9.Yonenaga K, Tohnai I, Mitsudo K, Mori Y, Saijo H, Iwai T, et al. Anatomical study of the external carotid artery and its branches for administration of superselective intra-arterial chemotherapy via the superficial temporal artery. Int J Clin Oncol. 2011 Dec;16(6):654–659. doi: 10.1007/s10147-011-0238-y. [DOI] [PubMed] [Google Scholar]