Abstract
Purpose
A possible complication after total disc replacement (TDR) is subsidence, presumably caused by asymmetric implantation, implant undersizing or reduced bone quality. This study aims to quantify the degree of subsidence of an SB Charité TDR, and investigate whether undersizing is related to subsidence.
Methods
A custom developed software package (Mathworks) reconstructed 3D bone-implant geometry. A threshold for subsidence was determined by comparing penetrated bone volume (PBV) and rotation angles. Inter- and intra-observer reproducibilities were calculated. Subsidence was correlated to undersizing.
Results
High inter- and intra-observer correlation coefficients were found for the method (R > 0.92). Subsidence was quantified as PBV 700 mm3 combined with a rotation angle >7.5°. A reduced risk of subsidence was correlated to >60 and >62 % of the bony endplate covered by the TDR endplate for L4 and L5, respectively.
Conclusions
A reproducible method to determine undersizing was developed. Thresholds were determined related to a reduced risk of subsidence.
Keywords: Total disc replacement, Subsidence, Undersizing, Penetrated bone volume, Rotation angle
Introduction
Low back pain caused by degenerative disc disease (DDD) is a major health problem in Western society [1–3]. If conservative treatment fails, a surgical intervention may be considered. Besides spinal fusion, total disc replacement (TDR) is increasingly used as a surgical treatment. In a recent review, a wide range (10–40 %) of complications after TDR implantation has been reported [4]. Subsidence of the TDR implant into the bony endplate of the vertebrae appeared to be a relatively frequent complication [4–6]. For example, we reported on a patient group with failed SB Charité III TDR implants (Link, Germany; DePuy, MA) [6–8], of which 39 out of 75 patients (52 %) showed clinically determined subsidence [6].
It is assumed that a mismatch in size between a TDR and the vertebra may cause subsidence. Gstoettner et al. [9] studied the mismatch between vertebral endplates and the size of the TDR implant using CT scans [9, 10]. Although at level L4–L5 an inappropriate size match (>10 mm difference in width between bony endplate and TDR endplate) was measured in 97.6 % of the vertebral endplates in anteroposterior (AP) direction, and in 78 % of the vertebral endplates in mediolateral direction, no evidence was found that a mismatch truly causes subsidence [9].
To quantify subsidence, Lee et al. [11] measured the angle between the endplate of a ProDisc-L TDR (Synthes, PA) and the endplate of the vertebra immediately after implantation surgery and during follow-up using lateral radiographs. They found that subsidence was correlated to an angular mismatch of >5° on lateral radiographs at follow-up, as compared to immediately postoperative radiographs.
We hypothesized that subsidence of the Charité TDR could be related to a mismatch in size between the TDR implant and the vertebra. Due to undersizing of the implant, the TDR endplate is covering the weaker central bone instead of the stronger peripheral bony ring. To test this hypothesis, an accurate and objective quantification of subsidence and undersizing is needed. The first purpose of this study was to develop a method to quantify the amount of subsidence and undersizing from plain radiographs, and to relate these results to the clinical diagnosis of subsidence. The second goal was to investigate whether the quantified undersizing and subsidence of the SB Charité TDR are related.
Materials and methods
Patient selection
Forty-two patients with an L4–L5 SB Charité III TDR, who consulted our outpatient clinic with recurrent or persistent low back pain, were included (Table 1).The TDRs had been implanted elsewhere. The most recent plain anteroposterior (AP) and lateral radiographs taken during routine evaluation were included in this retrospective study, with a mean implantation time of 10 years (range 1–19 years).
Table 1.
Patients characteristics
| N | |
|---|---|
| Sex (f/m) | 19/23 |
| Age (mean, range) | 41 years, 33–56 years |
| Time in vivo (mean, range) | 10 years, 1–19 years |
| Number of operated levels | |
| Single level | 26 |
| Two levels | 15 |
| Three levels | 1 |
Time in vivo represents time from TDR implantation to last plain radiograph
Age age at time of implantation in years
Quantifying subsidence
A custom developed software package implemented in Matlab (Matlab R2009b, Mathworks, MA) was developed to simultaneously display both AP and lateral radiographs.
A 3D graphical representation of a TDR was translated and rotated manually by the operator until its outline matched the outline of the TDR in both radiographs (Fig. 1). Next, the operator identified the most lateral left and right points of the bony endplate on the AP radiograph and the most anterior and posterior points of the bony endplate on the lateral radiograph (Fig. 2). In this manner, a plane was defined which represents the 3D position of the bony endplates.
Fig. 1.
a Orientation of the metal endplate for L4 shown in a 3D view and b projections of the orientation on AP and lateral radiographs (red line)
Fig. 2.
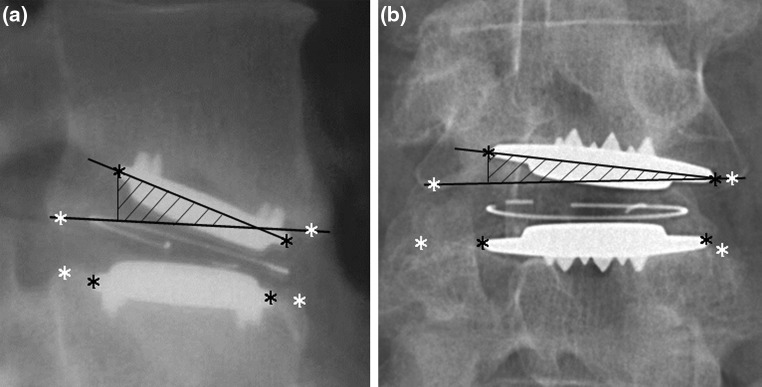
a Angle between endplate and bony endplate (α lateral) on lateral radiograph. The shading on a and b represents the calculated penetrated bone volume (PBV).The penetrated part of the TDR endplate was perpendicularly projected on the plane representing the bony endplate and the penetrated volume was calculated by integration of the orthogonal distance between the TDR endplate and this projection over the projected endplate area. b Rotation around the x-axis is measured on AP radiograph (α AP). The bony endplate of the vertebra was defined as the most superior-anterior point till the most superior-posterior point
Based on these measurements two variables were defined to classify subsidence:
The volume of bone that has been penetrated by the implant due to subsidence (penetrated bone volume, PBV): by projecting the TDR endplate on the plane representing the bony endplate, the penetrated volume was calculated (Fig. 2). For these calculations, the TDR endplate was represented as a rectangle, defined by its most lateral, anterior and posterior points.
Rotation angles of the TDR implant relative to the bony endplate [αAP and αlateral, expressed in degrees (º)]: rotation angles were calculated as the angle between a line that connects the indicated points on the bony endplate and a line that connects the indicated points on the TDR endplate for both radiographs (Fig. 2).
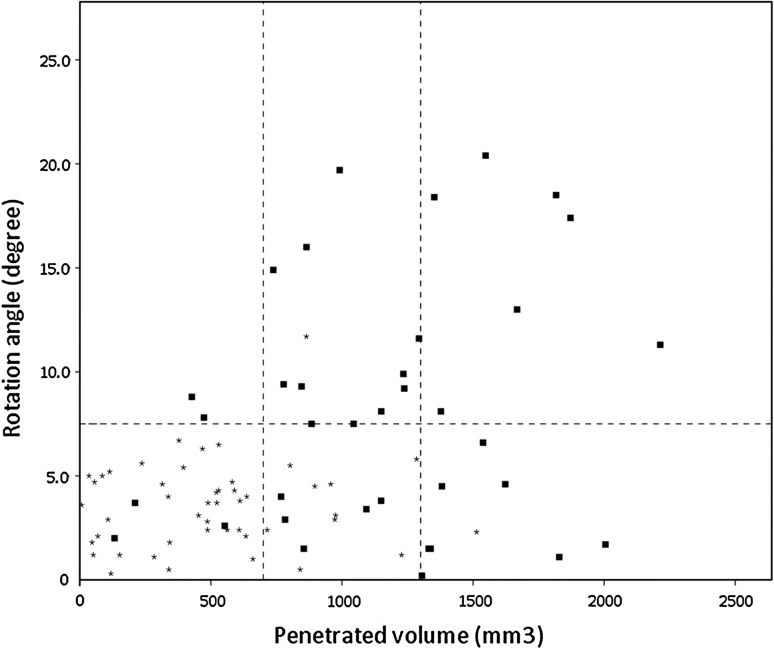
Based on the AP and lateral radiographs, clinical subsidence was determined by the judgment of an experienced orthopaedic surgeon (PW). Thresholds for PBV and α beyond which subsidence was to be defined, were iteratively determined by minimizing the false positive (FP) and false negative (FN) classifications compared to the clinical judgment. To do so, the PBV and α of each case were plotted in a scatter plot and classified for subsidence according to the orthopaedic surgeon’s estimate. An optimum between FP and FN cases was obtained by adjusting the threshold for PBV in steps of 100 mm3 from 0 to the maximum measured PBV. At the same time, a threshold for rotation angle was determined by adjusting the threshold in steps of 0.5° from 0 to the maximum measured rotation angle. For each combination, the number of FP and FN was determined. A combination of thresholds then was sought that would minimize the sum of the FP and FN cases. If different combinations of thresholds were found that could minimize the sum of FP and FN cases to the same degree, the combination that would minimize the FN cases most was selected.
Areal undersizing index
Using the same software package Matlab, an areal undersizing index (AUI) was defined to quantify mismatch in area of the bony endplate of the vertebra (Avertebra) and that of the metal endplate of the TDR implant (ATDR). The AUI was calculated according to:
 |
The shape of the vertebral endplate was assumed to be an ellipse fitted through the four points defined at the bony endplate earlier. For the TDR endplate a rectangular shape was assumed.
For accurate measurements of ATDR and Avertebra, AP and lateral radiographs should be taken perpendicular to each other. In our series, to avoid an overestimation of ATDR, cases with a rotation of the TDR around the longitudinal-axis of more than 15°, as determined by fitting the outline of a TDR onto the plain radiographs, were excluded.
Reliability
To determine the inter-observer reliability of this method, three observers measured all radiographs on L4 and L5. Two observers measured twice to determine the intra-observer reliability. For these observers, the mean of both measured AUI was used for further analyses.
Correlation coefficients between the measurements (inter- as well as intra-observer) were calculated.
Statistics
Using SPSS 19.0, independent sample and paired t-tests were used to test means. Inter- and intra-observer correlation coefficients were calculated by Intra Correlation Coefficient (ICC). The association of categorical values was tested by Chi square test. A significance level of p < 0.05 was used.
Results
Quantifying subsidence
By combining threshold values for PBV and rotation angle, an objective way to classify subsidence was obtained. There was a significant correlation (p < 0.01) between the scores given by the orthopaedic surgeon and those by the computer model for both L4 and L5. With these thresholds, subsidence was defined if a PBV of ≥1,300 mm3 was measured, independent on the rotation angle. Furthermore, subsidence was also defined if a PBV between 700 and 1,300 mm3 was found, in combination with a rotation angle of ≥7.5° on either the AP or lateral radiographs (Fig. 3).
Fig. 3.
Graphical representation of the rotation angle of lateral and AP radiographs versus PBV for L4 and for L5 of the 42 included patients. The asterisk represent the patient without clinical subsidence and the squares dots with subsidence according to the orthopaedic surgeon’s impression. The dotted lines represent the threshold values for angle (7.5º) and penetrated bone volume (700 and 1,300 mm3). Below these thresholds there is virtually no subsidence as estimated by clinical judgment
For the lower endplate of L4 and the upper endplate of L5, in 11 and in 17 cases subsidence was classified, respectively. For level L5, one patient was excluded due to projection of fusion instrumentation onto level L4–L5, resulting in an unclear view of L5. In nine cases (all L5) only a PBV of ≥1,300 mm3 was measured (parallel subsidence), while in the other 19 cases a rotation angle of ≥7.5° combined with a minimum PBV of ≥1,300 mm3 (angular subsidence) was measured.
Compared to the classification of clinically relevant subsidence by the orthopaedic surgeon, a sensitivity (Se) of 91 % (10/11 × 100 %) for L4 and 94 % (16/17 × 100 %) for L5 was obtained. For both levels the specificity (Sp) was 84 % (26/31 × 100 %) and 75 % (18/24 × 100 %), respectively (Table 2).
Table 2.
Measured subsidence versus clinical subsidence as classified by an orthopaedic surgeon, per level
| Measured subsidence L4 | ||||
|---|---|---|---|---|
| Clinical subsidence L4 | + | − | Total | |
| + | 10 | 5 (false positive) | 15 | |
| − | 1 (false negative) | 26 | 27 | |
| Total | 11 | 31 | 42 | |
| Measured subsidence L5 | ||||
|---|---|---|---|---|
| Clinical subsidence L5 | + | − | Total | |
| + | 16 | 6 (false positive) | 22 | |
| − | 1 (false negative) | 18 | 19 | |
| Total | 17 | 24 | 41 | |
Reliability
Eight L4 cases and seven L5 cases had a rotation angle of >15° around the longitudinal-axis and were excluded for AUI measurements. The mean AUI of all 34 patients per observer, per level, is given in Table 3. The mean AUI between parallel and angular subsidence was comparable (p = 0.90).
Table 3.
AUI between bony and metal endplate for vertebra L4 and L5 per observer, given as mean AUI with standard deviation (SD) and range of observations
| Observer | L4 | L5 |
|---|---|---|
| Mean ± SD (range) | Mean ± SD (range) | |
| 1 | 0.34 ± 0.11 (0.10–0.51) | 0.34 ± 0.11 (0.09–0.56) |
| 2 | 0.39 ± 0.13 (0.12–0.57) | 0.38 ± 0.13 (0.10–0.67) |
| 3 | 0.35 ± 0.11 (0.11–0.53) | 0.35 ± 0.11 (0.09–0.58) |
The inter-observer values are shown in Table 4. High correlation coefficients between the observers were found (R ≥ 0.96, p < 0.01).
Table 4.
Differences between inter-observers for vertebra L4 and L5, including the inter-observer correlation coefficient, given as mean value per observer and p value between both observers
| Observer | L4 | L5 | ||
|---|---|---|---|---|
| Mean obs | Correlation coefficient r (p value) | Mean obs | Correlation coefficient r (p value) | |
| 1–2 | 0.34–0.39 | 0.97 (<0.01) | 0.34–0.38 | 0.97 (<0.01) |
| 2–3 | 0.39–0.35 | 0.96 (<0.01) | 0.38–0.35 | 0.98 (<0.01) |
| 3–1 | 0.35–0.34 | 0.98 (<0.01) | 0.35–0.34 | 0.98 (<0.01) |
Intra-observer reliability of L4 indicated that both measurements were comparable (R ≥ 0.93, p < 0.01, Table 5). For L5 high intra-observer correlation coefficients were found for both levels (R ≥ 0.92, p < 0.01).
Table 5.
Mean AUI of measurement 1 and 2 for vertebra L4 and L5 per observer (intra-observer), given as mean value per observer and p value between both measurements
| Observer | L4 | L5 | ||
|---|---|---|---|---|
| Mean 1–2 | Correlation coefficient r (p value) | Mean 1–2 | Correlation coefficient r (p value) | |
| 1 | 0.34–0.35 | 0.95 (<0.01) | 0.32–0.36 | 0.92 (<0.01) |
| 3 | 0.35–0.35 | 0.93 (<0.01) | 0.35–0.36 | 0.92 (<0.01) |
Undersizing versus subsidence
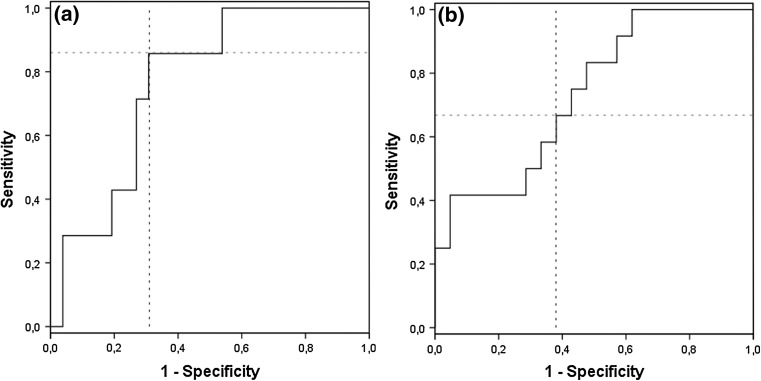
Using receiver operating characteristics techniques by analysing the AUI versus measured subsidence, a threshold value of 0.40 for AUI on L4 and 0.38 for L5 was obtained. In this way, a balance between maximum sensitivity and specificity scores was obtained for AUI as a predictor of subsidence. For L4 a Se of 86 % and Sp of 69 % (p = 0.02), and for L5 a Se of 67 % and Sp of 62 % (p = 0.11) between AUI and measured subsidence of the TDR was obtained (Fig. 4).
Fig. 4.
a Receiver operating characteristics (ROC) curve of AUI vs. measured subsidence for vertebra L4, with a sensitivity of 0.86 and specificity of 0.69. b ROC curve of AUI vs. measured subsidence for vertebra L5, with a sensitivity of 0.67 and specificity of 0.62. With a ROC curve it is possible to determine a threshold value for AUI to derive the optimal balance between sensitivity and specificity in relationship to subsidence. The striped lines indicate the sensitivity and specificity of the used threshold values
Subsidence was related to (under)sizing as follows: if more than 60 % (one minus threshold value 0.40) of the bony endplate of L4 was covered by the TDR endplate, a reduced risk of subsidence was observed. For L5, at least 62 % (1 − 0.38) of the bony endplate had to be covered to reduce the risk.
Discussion
At present, there is no clear evidence to what extent undersizing of a TDR contributes to its subsidence [12, 13]. Therefore, the current study designed a method to quantify subsidence, and to determine whether undersizing of the SB Charité TDR is related to subsidence.
A reliable method to measure subsidence of a TDR at level L4–L5 from plain radiographs was developed, with high inter- and intra-observer correlation coefficients (R ≥ 0.92). Subsidence was quantified using thresholds for PBV and rotation angles between TDR and bony endplate. Furthermore, subsidence was shown to be related to undersizing of the SB Charité TDR. A reduced risk of subsidence was found if more than 60 % (L4) or 62 % (L5) of the area of the bony endplate of the vertebra was covered by the TDR endplate.
Previously, Lee et al. [11] defined subsidence as an increase in angle of >5° between the TDR endplate and bony endplate [11]. It should be noted that parallel subsidence which we measured in nine cases, which may be only visible on AP radiographs, could not be detected by their method. In addition, if the TDR had migrated nearly parallel to the vertebral endplate into the vertebra, subsidence was not measured either, while in reality there could have been substantial subsidence. In the present study, by combining the rotation angle with PBV, cases where the TDR was migrated parallel into the vertebra were detected as well.
Gstoettner et al. [9] defined a distance of 5 mm between TDR implant endplate and vertebral endplate on either side as maximum allowed undersizing distance to prevent subsidence (10 mm in total). Using CT data, a mismatch was noted in 97.6 % with regard to the AP diameter. The mediolateral diameter was measured on two locations on CT scans, demonstrating a mismatch in mediolateral diameter in 51.2 and 78 % of the endplates [9]. Using their defined 5 mm distance method, we found in our series a mismatch in mediolateral diameter in 13 out of 42 cases for L4 and in 8 out of 41 cases for L5 on lateral radiographs. AP radiographs showed a 90 % mismatch both for L4 and L5 (38/42 and 37/41 cases, respectively). These percentages were lower on lateral and higher on AP radiographs compared to the results of Gsoettner et al. [9], probably caused by differences in the definition of the bony endplate.
The present method to measure subsidence and AUI can easily be implemented in a clinical setting to be used for preoperative templating of a TDR of the appropriate size. Two surgeons, without experience with the software package, measured after a short instruction. Both surgeons measured independent of each other and derived similar results. The same thresholds for AUI could be used for all observers. From these results, it may be concluded that there is no learning curve for this method and only one measurement is enough to derive accurate and reliable data. The introduction of a (semi)automated detection method is not possible because, in most vertebrae, it would be difficult to automate the selection of points due to the presence or absence of multiple areas with high densities (grey values on radiographs), different window settings (difference in grey values between two patients), or over projection on vertebra L5 (AP view only) [14].
The method to measure the presence of subsidence is suitable for all lumbar levels up to L5. Unfortunately, L5–S1 could not be measured reliably due to over-projection of L5 onto the sacrum with poor visibility of bony landmarks on plain radiographs. This over-projection will interfere with the selection of predefined points on the radiographs (point could not be visible due to over-projection), resulting in unreliable values for AUI and the definition of subsidence. To avoid this problem, special AP-projections should be made to visualize the L5–S1 disc space. Using a CT-scan would also overcome this problem for L5–S1, however, scattering of the metal endplates would make it difficult to quantify subsidence reliably.
There are some limitations in the current study. First, because patients had been operated elsewhere no direct postoperative radiographs were available. As the direct postoperative position of the SB Charité TDR was unknown, it was impossible to compare our results with the method of Lee et al. [11]. More importantly, it was impossible to investigate whether malpositioning or migration of the TDR may have caused subsidence. Second, to simplify the calculations, we assumed the shape of the TDR to be a rectangle, which implies that the area of the TDR is slightly overestimated. As a result of that the AUI we calculated was slightly underestimated and the PBV was slightly overestimated. A more accurate representation of the endplate geometry can be derived from the TDR database and will be implemented in a future version. Third, the X-rays were made in two different hospitals and scanned digital as well as conventional radiographs were included. Therefore, it was not possible to validate the X-rays and to calculate the individual measurement error. Fourth, it was assumed that the radiographs were taken perpendicular to each other. However, as all radiographs were taken during regular patient care, it is possible that the angle between both radiographs was not exactly 90°. Large discrepancies, however, could be detected since in that case the fit of the TDR outline would not fit both radiographs at the same time. Small discrepancies could not be detected but will not have affected the results substantially. A possible solution would be the use of a biplanar radiography. Furthermore, future studies should verify the thresholds in a fresh data set of patients with a SB Charité TDR with no back or leg pain symptoms as well as newer designs of TDRs, since our method was based on patient with clinical problems after receiving a SB Charité TDR. It is important to know whether the presence of subsidence is related to signs and symptoms for clinical relevance.
In conclusion, a reliable method was developed to measure subsidence and AUI between the vertebral endplate and metal endplate of the TDR implant from plain AP and lateral radiographs. High inter- and intra-observer correlation coefficients were obtained. Our results showed that subsidence appear to be related to undersizing of the SB Charité TDR in this symptomatic patient group.
Conflict of interest
None.
References
- 1.Manchikanti L. Epidemiology of low back pain. Pain Physician. 2000;3(2):167–192. [PubMed] [Google Scholar]
- 2.Rubin DI. Epidemiology and risk factors for spine pain. Neurol Clin. 2007;25(2):353–371. doi: 10.1016/j.ncl.2007.01.004. [DOI] [PubMed] [Google Scholar]
- 3.Walker BF. The prevalence of low back pain: a systematic review of the literature from 1966 to 1998. J Spinal Disord. 2000;13(3):205–217. doi: 10.1097/00002517-200006000-00003. [DOI] [PubMed] [Google Scholar]
- 4.van den Eerenbeemt KD, Ostelo RW, van Royen BJ, Peul WC, van Tulder MW. Total disc replacement surgery for symptomatic degenerative lumbar disc disease: a systematic review of the literature. Eur Spine J. 2010;19(8):1262–1280. doi: 10.1007/s00586-010-1445-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blumenthal S, McAfee PC, Guyer RD, Hochschuler SH, Geisler FH, Holt RT, Garcia R, Jr, Regan JJ, Ohnmeiss DD. A prospective, randomized, multicenter Food and Drug Administration investigational device exemptions study of lumbar total disc replacement with the CHARITE artificial disc versus lumbar fusion: part I: evaluation of clinical outcomes. Spine. 2005;30(14):1565–1575. doi: 10.1097/01.brs.0000170587.32676.0e. [DOI] [PubMed] [Google Scholar]
- 6.Punt IM, Visser VM, van Rhijn LW, Kurtz SM, Antonis J, Schurink GW, van Ooij A. Complications and reoperations of the SB Charite lumbar disc prosthesis: experience in 75 patients. Eur Spine J. 2008;17(1):36–43. doi: 10.1007/s00586-007-0506-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Maat GH, Punt IM, van Rhijn LW, Schurink GW, van Ooij A. Removal of the Charite lumbar artificial disc prosthesis: surgical technique. J Spinal Disord Tech. 2009;22(5):334–339. doi: 10.1097/BSD.0b013e3181761d0c. [DOI] [PubMed] [Google Scholar]
- 8.van Ooij A, Oner FC, Verbout AJ. Complications of artificial disc replacement: a report of 27 patients with the SB Charite disc. J Spinal Disord Tech. 2003;16(4):369–383. doi: 10.1097/00024720-200308000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Gstoettner M, Heider D, Liebensteiner M, Bach CM. Footprint mismatch in lumbar total disc arthroplasty. Eur Spine J. 2008;17(11):1470–1475. doi: 10.1007/s00586-008-0780-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Putzier M, Funk JF, Schneider SV, Gross C, Tohtz SW, Khodadadyan-Klostermann C, Perka C, Kandziora F. Charite total disc replacement—clinical and radiographical results after an average follow-up of 17 years. Eur Spine J. 2006;15(2):183–195. doi: 10.1007/s00586-005-1022-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee CS, Chung SS, Oh SK, You JW. Significance of angular mismatch between vertebral endplate and prosthetic endplate in lumbar total disc replacement. J Spinal Disord Tech. 2010;24(3):183–188. doi: 10.1097/BSD.0b013e3181eb5214. [DOI] [PubMed] [Google Scholar]
- 12.Goel VK, Faizan A, Palepu V, Bhattacharya S. Parameters that effect spine biomechanics following cervical disc replacement. Eur Spine J. 2012;21(Suppl 5):S688–S699. doi: 10.1007/s00586-011-1816-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thaler M, Hartmann S, Gstottner M, Lechner R, Gabl M, Bach C. Footprint mismatch in total cervical disc arthroplasty. Eur Spine J. 2012 doi: 10.1007/s00586-012-2594-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Verdonck B, Nijlunsing R, Gerritsen FA, Cheung J, Wever DJ, Veldhuizen A, Devillers S, Makram-Ebeid S. Computer assisted quantitative analysis of deformities of the human spine. Comput Sci. 1998;1496:822–831. [Google Scholar]