Abstract
Purpose
Traumatic ligament injuries of the craniovertebral junction, either isolated or associated with bone avulsion or fracture, often lead to death. These injuries are rare and underrated but are increasingly seen in emergency departments due to the improvement in initial on-scene management of accidents. Vertical atlantoaxial dislocation (AAD) is a specific lesion that was barely reported. Based on our experience, our goal was to systematically investigate the prevalence and prognosis of traumatic vertical AAD and discuss its management.
Methods
All cervical CT scans performed at our institution between 2006 and 2010 for cervical trauma in adults were retrospectively reviewed. Based on the measurement of lateral mass index (LMI), defined as the gap between C1 and C2 articular facets, we identified three cases of traumatic vertical AAD in 300 CT scans. Their medical records were investigated.
Results
The incidence of vertical AAD was 1 % in the exposed population. One case was an isolated vertical AAD and two were associated with a type II odontoid fracture. We report the first case in the literature of unilateral vertical AAD. Two patients died rapidly; the survivor was treated with occipitocervical fixation. Specific maneuvers were used for immobilization and reduction.
Conclusions
This study found a not insignificant incidence of vertical AAD and a high lethality rate. LMI appears to be a relevant radiological criterion for this diagnosis, for which traction is contraindicated. Associated neurological or vascular damage should be suspected and investigated. In our experience, spinal surgical fixation is required because of major instability.
Keywords: Cervical spine, Trauma, Atlantoaxial dislocation
Introduction
The upper cervical spine (occiput to C2) classically accounts for one-third of all cervical spine injuries [1]. Most cases concern violent trauma in young adults, specifically road accidents, and often lead to death [2]. The upper cervical spine is particularly vulnerable to traumatic injury because of its great mobility, mostly at the C1–C2 joint. In an autopsy series, 24.4 % of patients whose death was attributable to traffic accidents had radiological lesions of the upper cervical spine [3]. Odontoid and C1 arch fractures are common (about 91 % of 69 patients with C1–C2 injuries in the study by Bohlman [1]), but ligament lesions, whether or not they are associated with bony fracture, must be recognized and specifically treated because of their instability.
Traumatic atlantooccipital dislocation (AOD) accounts for 0.7–1 % of all cervical spine injuries [1, 4], and atlantoaxial dislocation (AAD) 2.7 %, when all types and varieties are combined [1]. Yüksel et al. [5] found in their biomechanical study that vertical distraction could induce either AOD or AAD, depending on the anatomy of the ligaments surrounding the C1–C2 and atlantooccipital joints. AAD lesions can be described by their mechanism, as Traynelis did for AOD: translation (anterior [6], posterior [7–9], or lateral [10]), distraction [11–13], or rotation, either with pure ligament damage or associated with C1 and/or C2 fracture. Nonetheless, these mechanisms are usually combined, i.e., lateral with rotatory [14] or anterior with vertical [15]. The mechanism of isolated traumatic vertical distraction is mentioned hardly at all. Only three reported cases involve pure traumatic vertical AAD [11–13]. This injury can also occur without any trauma; this is most likely in cases of pre-existing anomalies of the C1–C2 joint, such as rheumatoid arthritis or ankylosing spondylitis [16], which can lead to basilar invagination by weakening the occipitocervical ligaments and facet capsules. A few cases have been associated with other superior cervical spine fractures [17–20]. It must be noted that pure anterior [6], vertical, or lateral [10] AAD is more likely to occur in odontoid pseudarthrosis or malformation or rheumatoid arthritis, and rotatory AAD in children [21].
Because of their severity and lethal outcomes, and the difficulties of diagnosis, cases of vertical AAD are rarely seen in emergency departments and probably underestimated. Most patients probably die early of cardiorespiratory dysfunction, low vascular cerebral flow, spinal cord hematoma or rupture, or from other severe body injuries. However, this same severity and risk of sudden death require that ligament damage to the upper cervical spine be kept in mind and recognized to enable treatment and prevent death. The purpose of this paper was to investigate the series of vertical AAD in our institution over the past few years and report on the management and outcome of these few cases.
Methods
To identify cases of vertical AAD, we reviewed 300 consecutive computed tomography (CT) scans performed for cervical trauma in adults for a 5-year period running backward from December 31, 2010. The criterion for vertical AAD was a lateral mass index (LMI) greater than 2.6 mm, as defined by Gonzalez et al. [22]. LMI is the longest distance between the lateral masses of C1 and C2, when measured perpendicular to the joint space on coronal images on the right and left sides. The C1–C2 joint space was measured on each side and the case was selected if the criterion was met. Three cases were identified. The medical history of each is reported below.
Results
Case 1
A 27-year-old man riding a motorbike and wearing a helmet collided with a car in January 2007. He was found unconscious with a Glasgow coma scale (GCS) of 3 and no cardiac activity. Clinical examination after resuscitation (intubation and intravenous adrenalin) and admission to our hospital revealed unresponsive bilateral mydriasis and chest and abdominal trauma. The whole-body CT scan showed a retroperitoneal hematoma due to renal and splenic injuries, extensive cerebral edema, and meningeal bleeding. It also showed a noticeable isolated vertical AAD with an LMI of 11 mm on both sides (Fig. 1). The CT scan did not use contrast product at the cervical spine, and no information was recorded about the vertebral arteries. The patient underwent splenectomy to cope with the bleeding; however, no cervical surgery was attempted because of hemodynamic instability. The patient died despite resuscitation.
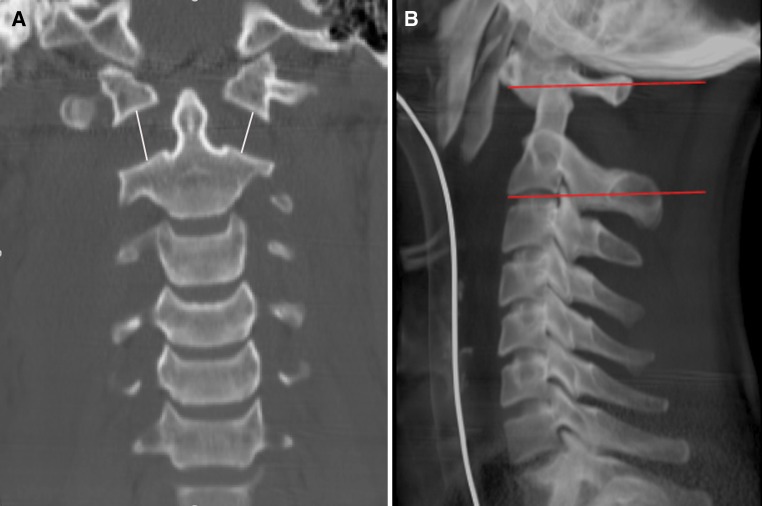
Fig. 1.
Case 1: wide bilateral AAD; the vertical C1–C2 gap (LMI) measured 11 mm. a Coronal CT reconstruction. b Lateral scoot view
Case 2
A 76-year-old man suddenly fell out of a tree from a height of 4 m in June 2010. Cardiorespiratory arrest was detected upon examination and the patient underwent attempted resuscitation. He was hemodynamically stabilized and remained in a coma (GCS 3). Cervical imaging (CT scan and MRI) showed C1 ring and type II odontoid fractures with a unilateral right AAD (LMI 5.5 mm) (Fig. 2). Associated lesions included dissection of the left vertebral artery at the junction of the V3 and V4 segments and rupture of the spinal cord at the C1–C2 level. The family and staff agreed that extraordinary lifesaving measures should not be performed, and the patient died 48 h later.
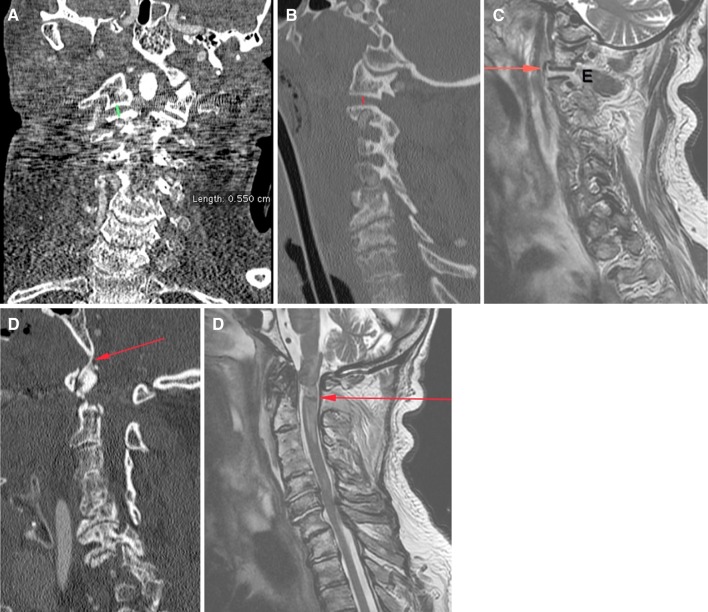
Fig. 2.
Case 2: right unilateral AAD. a Frontal CT scan reconstructions with a right LMI at 5.5 mm. b, c Parasagittal CT scan reconstructions and MRI showing the tear of the anterior facet capsule (arrow) and articular effusion (E). d Sagittal CT images showing the associated type II horizontal fracture of the odontoid. Note the calcification of the apical ligament (arrow). e Early sagittal MRI image in T2 sequence c showing the spinal cord rupture
Case 3
A 45-year-old woman with her seat belt fastened was involved in a high-speed car accident in November 2009. The vehicle turned over after a left impact causing severe head trauma. On the emergency team’s arrival on the scene, she was unconscious (GCS 4) and in hemorrhagic shock that required on-site intubation, perfusion, and vasoactive drugs. The initial neurological examination revealed the loss of deep tendon reflexes without abnormal reflexes of the cerebral trunk except a bilateral convergent squint. Standard X-rays and CT scans with contrast product (Fig. 3) showed a subdural hematoma and subarachnoid hemorrhage but no brain herniation, a left hemothorax due to several rib fractures, splenic fracture leading to hemoperitoneum, fractures of the left scapula, the left distal radius and several transverse processes, associated with a complex sacral fracture, a B-type fracture (according to the Magerl classification) of the third thoracic vertebrae and a fracture of the odontoid with a vertical AAD (7 mm for right LMI, 4.4 mm for the left). MRI examination showed cerebral trunk ischemia, no spinal cord compression or contusion but disruption of the facet capsules (Fig. 4) with articular effusion and a left atlantooccipital subluxation.
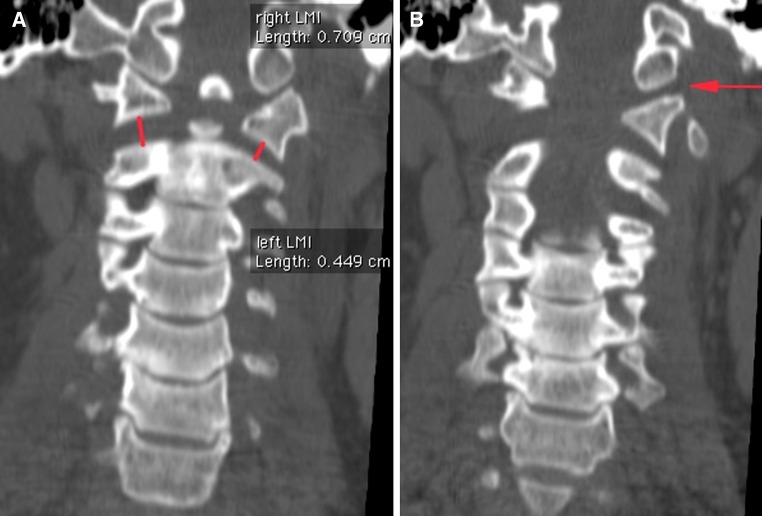
Fig. 3.
Case 3: CT scan. a, b Frontal reconstruction showing type II odontoid fracture and vertical AAD greater than 5 mm and left AOD
Fig. 4.
Case 3: MRI. a Right parasagittal image showing the articular effusion concerning C1–C2 joint. b Left parasagittal image showing the articular effusion concerning C1–C2 and C0–C1 joints. c Mid-sagittal image evidenced tears in the C0-dens ligaments (arrow) and the posterior union elements (star). Note the type B T3 fracture
After splenectomy, the patient underwent gentle skull compression with a Mayfield halo to reduce the AAD. C0–C3 occipitocervical fusion was performed the same day. The Mayfield Skull tong was used to maintain axial compression on the cervical spine during the procedure. Preoperative observations showed a large tear of posterior ligaments with a subarachnoid hematoma and a traumatic breach of the dura mater, as well as disruption of the facet capsules. A postoperative CT scan (Fig. 5) showed reduction of the AAD.
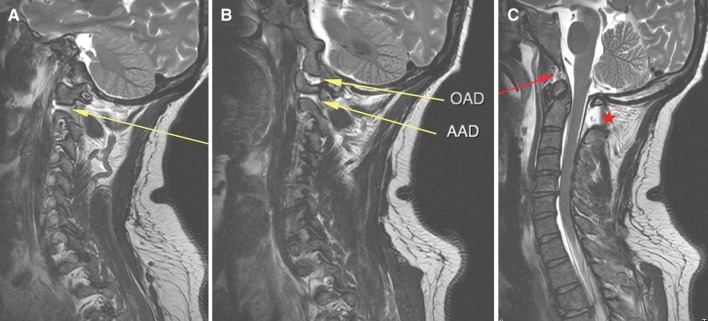
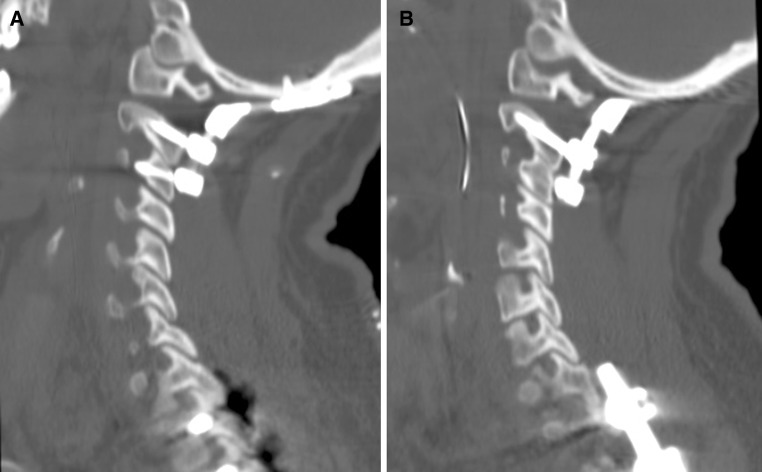
Fig. 5.
Case 3: postoperative CT scan showing the reduction of the bilateral AAD. a Right parasagittal; b left parasagittal. Note the incomplete reduction of the associated AOD
Over several weeks in the intensive care unit, complicated by pneumonia, the patient recovered cognitive functions but remained paralyzed on the right side with a slow recovery that did not exceed 2/5, associated with left facial nerve palsy. She had not recovered from bilateral paralysis of the abducens nerves and had diplopia.
At 12 months, her functional ability had improved significantly. She could walk 40 m with help. The neurological examination showed recovery of right hemiparesis, scored at 3–4/5. Treatment by alternating eye covering and by botulinum toxin injection led to regression of the diplopia. She also recovered normal urologic function.
Discussion
In this study, we estimated the prevalence of vertical AAD by conducting a systematic review of the CT scans for cervical trauma in our hospital. We found three cases, for an overall prevalence rate of 1 % for vertical AAD among all cases of adult cervical spine trauma. This is actually not the true prevalence in the general population. One case was a unilateral vertical dislocation, a type that has not previously been reported, to our knowledge. The survival rate of only one of three cases reminds us of the severity of the lesion and the importance of the initial care.
This prevalence rate must nonetheless be interpreted in light of the likelihood that some patients died before any radiological examination and others may have had only X-rays. In addition, reduced dislocation and severe strain are difficult to diagnose, especially when other more common injuries are simultaneously present. Magnetic resonance imaging is the gold standard to verify suspected C1–C2 vertical distraction injuries suggested on CT. Bohlman [1] found a 7.3 % prevalence of AAD among all cervical spine injuries—2.7 % pure AAD and 4.7 % combined with an odontoid fracture. The percentage of vertical AAD was not specified, nor was its mechanism described. The failure to clearly define the population and the inclusion criteria means that the prevalence estimate is not fully reliable. Finally, Bohlman’s inclusion of children (11 of the 69 patients with C1–C2 injuries) may explain the higher prevalence.
For diagnosis, McRae’s or Chamberlain’s line is usually used to define the vertical relation between the atlas and the axis in cases of basilar invagination (herniation of odontoid into the cranium). Ranawat’s line [23] is the distance between the center of the C2 pedicle to a line connecting the anterior and posterior C1 arches defined on plain radiographs. The vertical atlantoaxial index [24] is a ratio obtained from a mid-sagittal CT scan: the distance between a line drawn through the lower endplate of C2 and a parallel line tangential to the lower border of the anterior arch of the atlas is divided by the distance between the first line and another tangential to the superior margin of the dens. Vertical dislocation is associated with a ratio greater than 0.8. Nevertheless, those indexes cannot be used when AAD is combined with fracture of either C1 or C2. Gonzalez et al. [22] introduced the LMI to serve the same purpose for atlantoaxial distraction injuries as CCI (distance between the occipital condyle and the superior articular facet of the atlas) serves for vertical AOD when it exceeds 2 mm on frontal scan reconstructions. LMI greater than 2.6 mm suggests vertical C1–C2 distraction. The distance measured in our three cases was greater than 4 mm. Nonetheless, to avoid over diagnosis of distraction injuries, it is essential to identify any cup-shaped joint space that might be present. Our literature review found only nine cases [11–13] of vertical traumatic AAD, three isolated vertical AAD with no bony lesions, one case associated with an atlas lesion [17], and five with odontoid fractures [18–20] (Table 1). Gonzalez et al. [22] described six cases of vertical AAD diagnosed in 1 year: one patient died very quickly, another case was a child with a conservative treatment, three cases were isolated AAD, and the last one was associated with a C1 arch fracture.
Table 1.
Literature review: demographic, clinical, radiographic features, treatment and outcome
| Series | Age (years)/sex/circumstances | Clinical examination | Radiographic findings | Immediate management and outcome | Definitive procedure performed |
|---|---|---|---|---|---|
| Weiner and Brower [11] | 40/F/pedestrian pursued by a car | Tetraparesis | Vertical AAD with atlas occipitalization | External compression | C1–C2 articular screws, fusion and C0–C2 wires Neurological improvement (ambulation possible) |
| Payer et al. [13] | 64/M/scooter accident | Unknown | Vertical AAD | Death | |
| Ramaré et al. [12] | 62/M/car accident | Monoparesis due to brachial plexus stretching | Vertical AAD | External reduction by axial compression | C0–C4 fixation, C1–C2 arthrodesis No neurological deficit subordinate to AAD |
| Carroll et al. [17] | 19/F/car accident | Neurologically intact | Anterior and vertical AAD with fracture of the C1 anterior arch | Halo vest 6 weeks, no neurological complication | Philadelphia collar 12 weeks, no instability and no pain at 5 years follow-up |
| Przybylski and Welch [18] | 35/M/traffic accident | Neurologically intact | AAD with type III odontoid fracture | Traction: neurological deterioration (quadriplegia) | Posterior C0–C4 fusion, no improvement |
| Kirkpatrick et al. [19] | 65/F/car accident | Incomplete quadriplegia, bilateral abducens nerve palsies | Vertical AAD with type III odontoid fracture | Halo, persistent vertical distraction | C1–C2 arthrodesis, sublaminar cables |
| 39/F/car accident | Neurologically intact | Vertical AAD with type III odontoid fracture | Halo, quadriplegia | C1–C2 transarticular screw fixation, C5 tetraplegic | |
| 29/F/car accident | Unknown | Vertical AAD with type III odontoid fracture and C1 burst fracture | Halo, persistent distraction | C1–C2 transarticular screw fixation, neurological status not available | |
| Jea et al. [20] | 73/F/car accident | Quadriparesis, bilateral abducens nerve palsies | Vertical AAD with type III odontoid fracture | Cervical collar, no complication | C1–C2 arthrodesis, no neurological improvement |
No paper has reported a unilateral vertical dislocation as in our case #2 (76-year-old man). Bilateral or unilateral vertical AAD would be more appropriate terms than those generally used for articular lesions of the lower cervical spine. Unilateral vertical AAD might be explained by a distractive mechanism applied to a cervical spine already tilted to one side, either spontaneously during an accident or due to asymmetrical cervical osteoarthritis. Unilateral damage seems as unstable and dangerous as bilateral lesions in terms of neurological complications, as seen in patient #2, who had a spinal cord rupture and died soon after injury. Unilateral vertical AAD must be treated in a manner similar to its bilateral counterpart: traction should be avoided and fixation is required.
Two of our patients died. The cases reported in the literature are generally survivors. Indeed, of the nine cases previously reported, only one patient died. Neither prognosis nor survival rates could be determined. Gonzalez et al. [22] reported one death among five adults. Nevertheless, our results suggest that among patient able to undergo CT, the probability of survival is about one-third.
Although most of these patients were not attended by spine surgeon, because of their rapid fatal outcomes, the 1 % prevalence of documented vertical AAD in the population in our series of traumatic injuries leads us to consider that any such patient is at risk of vertical AAD. This suspicion of vertical AAD and our concern about the potential complications of traction together require that the initial care be especially attentive. Botelho et al. [15] reported a case in 1997 of anterior AAD with a C1 anterior arch fracture. Skull traction with 4.02 lbs (1.5 kg) led to irreducible vertical AAD and patient death. Two points must be stressed: first, as in any cervical trauma, intubation must be performed cautiously to prevent any aggravation of cardiorespiratory function. If intubation is needed, the jaw-thrust maneuver seems safer than extension and traction. Secondly, skull traction is simply forbidden [15, 18]: X-rays at least or CT scan must be done first to diagnose AAD.
The specific vascular or neurological lesions due to instability are severe. Early complications in our series included the dissection of the vertebral artery and contusion or even rupture of the spinal cord. Seven cases in the literature reported neurological outcomes (Table 1): of 3 initially tetraparetic patients, one improved; four patients had no initial neurological impairment, although halo treatment caused secondary worsening. This suggests that vertical AAD lesions are highly unstable and can induce an “all-or-nothing” neurological state—tetraparesis or nothing. In this context, MRI, contrast CT, or arteriography are indicated. The neurological dysfunction in the surviving patient in our short series is noticeable. This patient suffered from cerebral trunk ischemia that can cause several related syndromes. Foville’s syndrome produces ipsilateral horizontal gaze, facial nerve palsies, and contralateral hemiparesis. Our patient suffered from right hemiparesis, left facial nerve palsy, and bilateral abducens nerves paralysis, which do not correspond to such a central injury. Bilateral abducens palsy after head trauma has been described after basilar fracture of the skull, after cervical injuries with or without cervical fracture [25], and after skull traction (in 2 children) [26]. Its long course from the brainstem to the eye makes the abducens nerve vulnerable to strain injury [27, 28]. A cadaveric study [29] observed injuries at several sites: a dural entry point, the petrous apex, and the lateral wall of the internal carotid artery.
No real guidelines about initial care and treatment-related issues have been established for vertical AAD, probably due to the rarity of diagnosed cases. With the progress of three-dimensional imaging (CT scan and MRI reconstructions) and improvement in on-scene management, the incidence of vertical AAD might increase. Cervical traction is reported to lead to neurological deterioration and death, because it either reproduces the vertical distraction [15, 18] or creates new injury by excessive stretching. Traction immobilization is usual in cases of cervical spine trauma, but must be avoided in cases of vertical AAD. Given the not insignificant incidence of AAD, routine cervical lateral X-rays for all traffic victims might be considered, if possible before intubation. We acknowledge the implications and the difficulties of implementing such a procedure.
Reduction among the reported survivors of vertical AAD was performed externally by applying firm axial pressure on the head. Manually controlled axial compression can be carried out initially or under fluoroscopy [11]. The major instability in vertical AAD and the need for axial compression to achieve and maintain reduction indicate that orthopedic treatment with a halo cast or cervical collar is inappropriate in these cases. A consensus exists about the indications for surgical fixation. The five cases in the literature treated by halo had to undergo surgical fixation first [18–20] because of instability or neurological worsening (Table 1). Like Gonzalez et al. [22], we would recommend C1–C2 arthrodesis if possible (in the absence of AOD and of C1 or C2 fractures contraindicating short fixation). Temporary additional occipital-C3 fixation might be performed to improve primary stability as in the case reported by Ramaré et al. [12], to facilitate nursing in the intensive care unit.
Conclusion
Distraction injuries at the atlantoaxial junction are not as rare as the literature suggests (about 1 % in our study) and most commonly result in death. Vertical AAD can be uni- or bilateral. LMI >2.6 mm diagnoses this trauma on a standard CT scan (coronal images). When possible, MRI is reliable for assessing the ligament injuries of the upper cervical spine. It is essential to be aware that traction can lead to irreversible damage. Immediate reduction can be achieved by manual axial compression under fluoroscopy. Surgical fixation is recommended to prevent the instability associated with vertical AAD. Occipitocervical or C1–C2 arthrodesis is indicated.
Conflict of interest
None.
References
- 1.Bohlman HH. Acute fractures and dislocations of the cervical spine. An analysis of three hundred hospitalized patients and review of the literature. J Bone Joint Surg Am. 1979;61(8):1119–1142. [PubMed] [Google Scholar]
- 2.Davis D, Bohlman H, Walker AE, Fisher R, Robinson R. The pathological findings in fatal craniospinal injuries. J Neurosurg. 1971;34(5):603–613. doi: 10.3171/jns.1971.34.5.0603. [DOI] [PubMed] [Google Scholar]
- 3.Alker GJ, Jr, Oh YS, Leslie EV. High cervical spine and craniocervical junction injuries in fatal traffic accidents: a radiological study. Orthop Clin North Am. 1978;9(4):1003–1010. [PubMed] [Google Scholar]
- 4.Dickman CA, Papadopoulos SM, Sonntag VK, Spetzler RF, Rekate HL, Drabier J. Traumatic occipitoatlantal dislocations. J Spinal Disord. 1993;6(4):300–313. doi: 10.1097/00002517-199306040-00004. [DOI] [PubMed] [Google Scholar]
- 5.Yüksel KZ, Yüksel M, Gonzalez LF, Baek S, Heiserman JE, Sonntag VKH, et al. Occipitocervical vertical distraction injuries: anatomical biomechanical, and 3-tesla magnetic resonance imaging investigation. Spine. 2008;33(19):2066–2073. doi: 10.1097/BRS.0b013e31817e2cfc. [DOI] [PubMed] [Google Scholar]
- 6.Yin Q, Ai F, Zhang K, Chang Y, Xia H, Wu Z, et al. Irreducible anterior atlantoaxial dislocation: one-stage treatment with a transoral atlantoaxial reduction plate fixation and fusion. Report of 5 cases and review of the literature. Spine. 2005;30(13):E375–E381. doi: 10.1097/01.brs.0000168374.84757.d5. [DOI] [PubMed] [Google Scholar]
- 7.Jamshidi S, Dennis MW, Azzam C, Karim N. Traumatic posterior atlantoaxial dislocation without neurological deficit: case report. Neurosurgery. 1983;12(2):211–213. doi: 10.1227/00006123-198302000-00014. [DOI] [PubMed] [Google Scholar]
- 8.Wong DA, Mack RP, Craigmile TK. Traumatic atlantoaxial dislocation without fracture of the odontoid. Spine. 1991;16(5):587–589. doi: 10.1097/00007632-199105000-00021. [DOI] [PubMed] [Google Scholar]
- 9.Neumann U, Urbanski H, Riedel K. Posterior atlantoaxial dislocation without fracture of the odontoid. A case report. J Bone Joint Surg Am. 2003;85-A(7):1343–1346. doi: 10.2106/00004623-200307000-00023. [DOI] [PubMed] [Google Scholar]
- 10.Nakamura T, Ishikawa K, Matsubara S, Okajima K. Lateral atlantoaxial dislocation. Spine. 1991;16(2):245–247. [PubMed] [Google Scholar]
- 11.Weiner BK, Brower RS. Traumatic vertical atlantoaxial instability in a case of atlanto-occipital coalition. Spine. 1997;22(9):1033–1035. doi: 10.1097/00007632-199705010-00019. [DOI] [PubMed] [Google Scholar]
- 12.Ramaré S, Lazennec JY, Camelot C, Saillant G, Hansen S, Trabelsi R. Vertical atlantoaxial dislocation. Eur Spine J. 1999;8(3):241–243. doi: 10.1007/s005860050166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Payer M, Wetzel S, Kelekis A, Jenny B. Traumatic vertical atlantoaxial dislocation. J Clin Neurosci. 2005;12(6):704–706. doi: 10.1016/j.jocn.2004.03.043. [DOI] [PubMed] [Google Scholar]
- 14.Spoor AB, Diekerhof CH, Bonnet M, Oner FC. Traumatic complex dislocation of the atlanto-axial joint with odontoid and C2 superior articular facet fracture. Spine. 2008;33(19):E708–E711. doi: 10.1097/BRS.0b013e31817c140d. [DOI] [PubMed] [Google Scholar]
- 15.Botelho RV, de Souza Palma AM, Abgussen CM, Fontoura EA. Traumatic vertical atlantoaxial instability: the risk associated with skull traction. Case report and literature review. Eur Spine. 2000;J 9(5):430–433. doi: 10.1007/s005860000166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hensinger RN. Osseous anomalies of the craniovertebral junction. Spine. 1986;11(4):323–333. doi: 10.1097/00007632-198605000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Carroll EA, Gordon B, Sweeney CA, Joy S, Connolly PJ. Traumatic atlantoaxial distraction injury: a case report. Spine. 2001;26(4):454–457. doi: 10.1097/00007632-200102150-00026. [DOI] [PubMed] [Google Scholar]
- 18.Przybylski GJ, Welch WC. Longitudinal atlantoaxial dislocation with type III odontoid fracture. Case report and review of the literature. J Neurosurg. 1996;84(4):666–670. doi: 10.3171/jns.1996.84.4.0666. [DOI] [PubMed] [Google Scholar]
- 19.Kirkpatrick JS, Sheils T, Theiss SM. Type-III dens fracture with distraction: an unstable injury. A report of three cases. J Bone Joint Surg Am. 2004;86-A(11):2514–2518. [PubMed] [Google Scholar]
- 20.Jea A, Tatsui C, Farhat H, Vanni S, Levi AD. Vertically unstable type III odontoid fractures: case report. Neurosurgery. 2006;58(4):E797. doi: 10.1227/01.NEU.0000208555.34661.CD. [DOI] [PubMed] [Google Scholar]
- 21.Pang D. Atlantoaxial rotatory fixation. Neurosurgery. 2010;66(3 Suppl):161–183. doi: 10.1227/01.NEU.0000365800.94865.D4. [DOI] [PubMed] [Google Scholar]
- 22.Gonzalez LF, Fiorella D, Crawford NR, Wallace RC, Feiz-Erfan I, Drumm D, et al. Vertical atlantoaxial distraction injuries: radiological criteria and clinical implications. J Neurosurg Spine. 2004;1(3):273–280. doi: 10.3171/spi.2004.1.3.0273. [DOI] [PubMed] [Google Scholar]
- 23.Ranawat CS, O’Leary P, Pellicci P, Tsairis P, Marchisello P, Dorr L. Cervical spine fusion in rheumatoid arthritis. J Bone Joint Surg Am. 1979;61(7):1003–1010. [PubMed] [Google Scholar]
- 24.Kulkarni AG, Goel AH. Vertical atlantoaxial index: a new craniovertebral radiographic index. J Spinal Disord Tech. 2008;21(1):4–10. doi: 10.1097/BSD.0b013e31804856d7. [DOI] [PubMed] [Google Scholar]
- 25.Rowe F. Prevalence of ocular motor cranial nerve palsy and associations following stroke. Eye (Lond) 2011;25(7):881–887. doi: 10.1038/eye.2011.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pinches E, Thompson D, Noordeen H, Liasis A, Nischal KK. Fourth and sixth cranial nerve injury after halo traction in children: a report of two cases. J AAPOS. 2004;8(6):580–585. doi: 10.1016/j.jaapos.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 27.Schneider RC, Johnson FD. Bilateral traumatic abducens palsy. A mechanism of injury suggested by the study of associated cervical spine fractures. J Neurosurg. 1971;34(1):33–37. doi: 10.3171/jns.1971.34.1.0033. [DOI] [PubMed] [Google Scholar]
- 28.Takagi H, Miyasaka Y, Kuramae T, Ohwada T, Tsunoda M. Bilateral traumatic abducens nerve palsy without skull fracture or intracranial hematoma-a report of 3 cases and consideration of the mechanism of injury (author’s transl) No Shinkei Geka. 1976;4(10):963–969. [PubMed] [Google Scholar]
- 29.Sam B, Ozveren MF, Akdemir I, Topsakal C, Cobanoglu B, Baydar CL, et al. The mechanism of injury of the abducens nerve in severe head trauma: a postmortem study. Forensic Sci Int. 2004;140(1):25–32. doi: 10.1016/j.forsciint.2003.11.020. [DOI] [PubMed] [Google Scholar]