Abstract
Purpose
The aim of this current study was to analyze the clinical outcomes after Discover cervical disc replacement and its effects on maintaining cervical lordosis and range of motion (ROM). The possible factors influencing postoperative ROM were analyzed.
Method
27 men and 28 women with a mean age of 46.4 ± 8.7 years were prospectively followed up for 2 years. Clinical outcomes were assessed using Japanese Orthopedic Association (JOA), Neck Disability Index (NDI), visual analog scale (VAS) and Odom’s criteria. Radiographic information including segment and overall alignment, functional spinal unit (FSU) and overall ROM, and disc heights were prospectively collected during the follow-up. The correlations between the postoperative FSU ROM at last follow-up and influencing factors were analyzed.
Results
Mean NDI, JOA and VAS scores showed statistical improvements at last follow-up. Anterior migration of the prosthesis was detected in six cases. Heterotopic ossification was observed in ten patients. Mean FSU angle, endplate angle of the treated level and mean overall cervical alignment were all improved significantly at last follow-up (P < 0.001). However, mean FSU ROM of the treated segment significantly decreased postoperatively (P = 0.008), while mean overall ROM showed no significant differences. A significant correlation was found between preoperative FSU ROM and postoperative FSU ROM by the Pearson correlation coefficient (r = 0.325, P = 0.034). Multiple linear regression analysis confirmed that preoperative FSU ROM contributed independently to a model with a coefficient of determination of 0.37 (P = 0.034).
Conclusions
In the 2 years follow-up, the Discover cervical disc arthroplasty has provided satisfactory clinical outcomes. It was able to substantially restore segment and overall cervical alignment while partially maintaining segment and overall cervical ROM. Additionally, we found that postoperative FSU ROM positively correlated with preoperative FSU ROM.
Keywords: Cervical artificial disc, Cervical disc arthroplasty, Range of motion, Factor analysis
Introduction
In recent years, cervical disc replacement (CDR) has become popular as an alternative to anterior cervical discectomy and fusion (ACDF). Its theoretical and observed advantages include a more physiologic distribution of range of motion (ROM), reduced adjacent level stresses and a lowered rate of adjacent segment degeneration (ASD). Currently, there are many commercially available artificial discs with different biomechanical properties. Some prostheses have shown increased ROM postoperatively [1–4], while others have shown no change [5–7] or decreased ROM [8–10]. Interestingly, some prostheses have been shown to aid in restoration of cervical lordosis postoperatively [11–14], while others have shown no change [2, 4] or trend toward kyphosis [5, 15, 16]. As a newly developed device, few reports about the Discover artificial cervical disc (DePuy Spine, Raynham, MA, USA) arthroplasty have been published. The purpose of this study was to prospectively study the clinical outcomes of the Discover disc CDR, specifically its effects on maintaining cervical lordosis and ROM. The factors influencing postoperative ROM were analyzed.
Materials and methods
Patient population
From June 2009 to June 2010, we performed the Discover disc CDR in 71 select patients in our institution. The prospective study was approved by our institutional research board. Patient selection was based on inclusion and exclusion criteria (Table 1). Fifty-five patients who were successfully followed for 2 years were included in this study, which corresponded to a follow-up compliance of 77.5 % (55/71). There were 27 male and 28 female patients with a mean age of 46.4 ± 8.7 years (range: 26–67 years). Four patients were treated at C3/4, 11 patients at C4/5, 34 patients at C5/6 and 6 patients at C6/7. There were 16 radiculopathy, 31 myelopathy and 8 combined patients. All the patients were well informed about the features and the current indication of the Discover disc and had a strong desire to undergo CDR.
Table 1.
Patient selection criteria
| Criteria |
|---|
| Inclusion |
| 21–70 years of age |
| Single-level symptomatic cervical disc disease between C3 and C7 |
| Failed non-surgical treatment of at least 6 weeks, or subject has progressive symptoms of nerve root or spinal cord compression |
| Minimum Neck Disability Index score of ≥30 % (15/50) |
| Exclusion |
| Cervical instability defined by translation on flexion–extension radiographs of 3 mm or 11° compared with adjacent level |
| Non-mobility of the level to be treated |
| Fused adjacent level to the level to be treated |
| Axial neck pain as the solitary symptom |
| Prior surgery at target levels |
| Metabolic bone disease or endocrine disorder affecting osteogenesis |
| Pre-existing neurological abnormalities other then deficits produced from the spinal lesion |
| Alcohol or drug abuse |
| Pregnant or wishing to become pregnant within 5 years |
| Traumatic injury of spine |
| HIV, metastatic cancer, presence of infection, morbid obesity, significant psychological disease or allergy to a metal alloy or polyethylene |
Device design
The Discover artificial cervical disc (DePuy Spine, Raynham, MA, USA) is an MRI-compatible ball-and-socket device comprising a titanium alloy superior endplate that articulates with an ultrahigh molecular weight polyethylene core that is mechanically fixed to the inferior titanium alloy endplate. It features a spherical bearing that allows for motion in all rotational directions. The prosthesis has 7° lordosis to allow for restoration of sagittal alignment in the cervical spine. Immediate fixation is provided by six, 1 mm teeth that project from each endplate. Long-term fixation is provided by the teeth and a layer of porous titanium plasma spray (TPS) and hydroxyapatite (HA) coated on each endplate.
Surgical technique
A standard right-sided anterior approach was routinely performed. The surgical techniques were similar to those for a routine anterior cervical decompression. Implantation of the device was performed according to the manufacturer’s specifications. The posterior longitudinal ligaments (PLL) were completely removed in all cases. Endplate preparation corresponded to the lordotic design of the implant, which reflected the normal anatomic state. Any remaining superior posterior osteophytes overhanging the endplate were removed to avoid the potential for postoperative translation. All cases were treated by two senior authors.
Clinical and radiographic evaluation
Evaluations were performed preoperatively, at 1 week, 3 and 6 months and 2 years postoperatively. For the clinical evaluation, Japanese Orthopedic Association (JOA), Neck Disability Index (NDI), visual analog scale (VAS) for neck pain and Odom’s criteria were assessed. All patients were asked to complete questionnaires before surgery and at each follow-up examination. The NDI and VAS scores varied from 0 to 100. The preoperative scores were compared with the scores at the last follow-up. Complications during the follow-up were recorded.
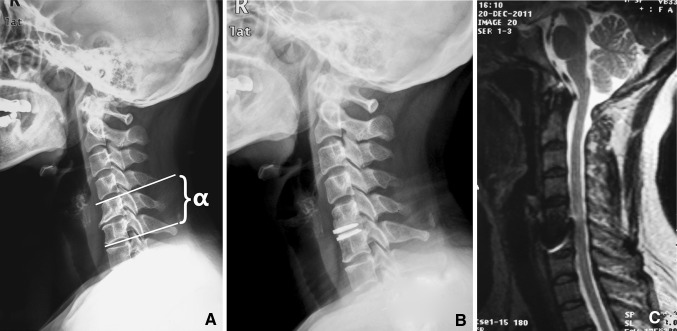
Radiographic measurement data were collected by two observers. Each of them measured twice, and the mean value was used for analysis. The functional spinal unit (FSU) angle and endplate angle of the operative segment, and the overall sagittal alignment (C2–C7) were measured on lateral radiographs in the neutral position. The FSU angle was determined by the angle of intersection of tangential lines drawn along the superior endplate of the cephalad vertebral body and the inferior endplate of the caudal body (Fig. 1a). The postoperative endplate angle was defined as the angle between the superior and inferior articulating surfaces of the Discover discs. The FSU and overall (C2–C7) ROMs were measured on the dynamic flexion and extension X-rays. Disc space height was measured digitally at the surgical level through the midpoint of the upper and lower endplates. Lordosis was shown as a positive value, and kyphosis was shown as a negative value. It should be noted that because there were 12 patients’ images whose inferior endplates of C7 could not been seen, we presented the statistics of overall cervical lordosis (C2–7) and overall ROM (C2–7) from the remaining 43 patients. Radiographic measurements were performed on source-digitalized images using IMPAX imaging software (Agfa version, Mitra Imaging Inc.).
Fig. 1.
A 46-year-old female, whose FSU angle (α) of the treated segment was −2.5° preoperatively and 8.4° at last follow-up, endplate angle of the treated segment was −2.3° preoperatively and 8° at the last follow-up, and overall alignment was −7.4° preoperatively and 5.8° at the last follow-up. a Preoperative lateral X-ray. b 2-year postoperative lateral X-ray. c 1-year postoperative MRI
Statistical analysis
Statistical analyses were performed by a professional medical statistical consultant. Statistical analysis was performed using SPSS software 17.0 (SPSS Inc, Chicago, IL). A Paired t test was used for paired values. Further, we used data from the 43 patients whose lower endplate of C7 could be seen to analyze factors that may influence postoperative FSU ROM. The correlations between the postoperative FSU ROM at last follow-up and influencing factors, including age, sex, preoperative FSU, endplate angle, overall alignment, FSU and overall ROM, disc height, NDI, JOA and VAS were analyzed by the Pearson correlation. Those variables were further evaluated using the multiple regression analysis method (for postoperative FSU ROM). P < 0.05 was considered as statistically significant.
Results
Clinical evaluation
Clinical values are provided in Table 2. The mean JOA had improved significantly from 11.8 ± 2.0 preoperatively to 15.4 ± 1.2 at the last follow-up (P < 0.001), with an average improvement rate of 66.5 ± 31.7 %. Statistically significant reductions in both NDI and VAS were noted in this group. The mean NDI was 37.3 ± 14.3 preoperatively and 13.7 ± 10.9 at the last follow-up (P < 0.001). The mean VAS for neck pain score was 64.4 ± 15.1 preoperatively and decreased to 17.4 ± 13.3 at the last follow-up (P < 0.001). According to Odom’s scale, there were 32 excellent cases, 13 good cases, 7 fair cases and 3 poor cases. Good to excellent results were attained in 81.8 % of these patients.
Table 2.
Preoperative clinical values and outcomes at the last follow-up
| Variables | Preoperative period | Last follow-up | P |
|---|---|---|---|
| JOA | 11.8 ± 2.0 | 15.4 ± 1.2 | <0.001 |
| NDI | 37.3 ± 14.3 | 13.7 ± 10.9 | <0.001 |
| VAS | 64.4 ± 15.1 | 17.4 ± 13.3 | <0.001 |
JOA Japanese Orthopedic Association, NDI Neck Disability Index, VAS visual analog scale for neck pain
Radiographic outcomes
Radiologic values are provided in Table 3. The sagittal alignments were well restored in most cases. The mean endplate angle improved from 3.8 ± 3.8° preoperatively to 6.7 ± 5.4° at the last follow-up (P < 0.001). Improvement of endplate angle was seen in 46 cases. The mean FSU angle improved from 1.3 ± 5.9° preoperatively to 5.2 ± 6.6° at the last follow-up (P < 0.001). Improvement of FSU angle was seen in 43 cases. The mean overall sagittal alignment improved from 13.8 ± 8.9° preoperatively to 16.4 ± 8.0° at the last follow-up (P < 0.05).
Table 3.
Preoperative radiologic values and outcomes at the last follow-up
| Variables | Preoperative period | Last follow-up | P |
|---|---|---|---|
| Endplate angle (°) | 3.8 ± 3.8 | 6.7 ± 5.4 | <0.001 |
| FSU angle (°) | 1.3 ± 5.9 | 5.2 ± 6.6 | <0.001 |
| Overall alignment (°)a | 13.8 ± 8.9° | 16.4 ± 8.0° | =0.042 |
| FSU ROM (°) | 10.8 ± 5.3 | 8.4 ± 6.3 | =0.008 |
| Overall ROM (°)a | 38.4 ± 14.4 | 37.7 ± 12.3 | =0.703 |
| Disc height (mm) | 6.2 ± 0.9 | 8.4 ± 0.7 | <0.001 |
FSU functional spine unit, ROM range of motion
aIndicates those data were from the 43 patients whose inferior endplates of C7 could be seen
Both mean FSU and overall ROM parameters demonstrated a decrease in the follow-up. The mean FSU ROM decreased significantly from 10.8 ± 5.3° preoperatively to 8.4 ± 6.3° at the last follow-up (P = 0.008), and increase of ROM was seen in only 17 cases. The mean overall ROM decreased from 38.4 ± 14.4° preoperatively to 37.7 ± 12.3° at the last follow-up (P = 0.703). The mean disc height increased from 6.2 ± 0.9 mm preoperatively to 8.4 ± 0.7 mm at the last follow-up.
Complications
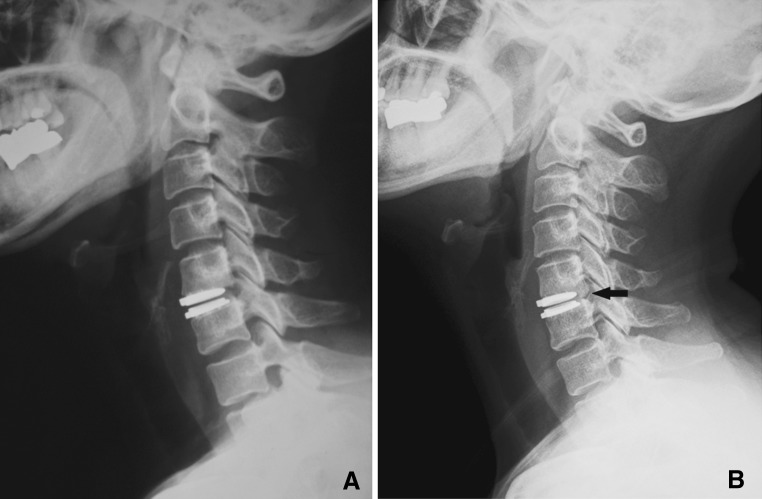
Dysphagia was detected in four patients, which was probably due to traction or irritation of the superior laryngeal nerve during surgery and was relieved in a month without any special treatment. Anterior migration of the prosthesis was detected in six cases (Fig. 2). Adjacent segment degeneration occurred in four patients, whose neurological symptoms were relieved after receiving medical treatment. Heterotopic ossification (HO) was observed in ten patients (Fig. 3). According to McAfee’s classification [17], there were five Grade I cases and five Grade II cases. Complications such as neurological deterioration, implant subsidence and fractured vertebrae were not observed. Revision surgery was not required in any case.
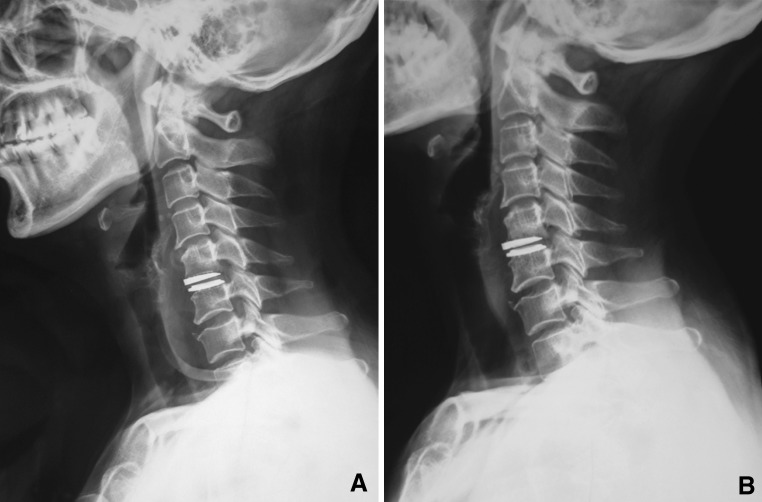
Fig. 2.
A 51-year-old female, who was found with 0.21 cm migration of the superior endplate of the Discover disc at the last follow-up; a immediately after surgery; b 2 years after surgery
Fig. 3.
A 50-year-old female, who was found with mild migration of prosthesis and Grade II HO (arrow) at the last follow-up, which might be caused by inadequate insertion depth; a immediately after surgery; b 2 years after surgery
Correlation analysis and multiple regression linear analysis
The results were from the 43 patients whose inferior endplates of C7 could be seen. A significant correlation was found between preoperative FSU ROM and postoperative FSU ROM by the Pearson correlation coefficient (r = 0.325, P = 0.034). Multiple linear regression analysis confirmed that preoperative FSU ROM contributed independently to a model with a coefficient of determination of 0.37 (P = 0.034) (Table 4).
Table 4.
Results of multiple regression linear analysis
| Variables | β | S β | t | P |
|---|---|---|---|---|
| Constant | 4.64 | 2.11 | 2.20 | 0.034 |
| Preoperative FSU ROM | 0.37 | 0.17 | 2.20 | 0.034 |
β partial regression coefficient, S β standard error of mean
Discussion
The effectiveness of CDR in treating cervical degenerative disc diseases has been confirmed in many studies [4, 6, 8, 18, 19]. CDR can maintain the motion of the treated segment and contribute to physiological alignment of the treated segment and overall cervical spine. The current widely used cervical artificial discs include Bryan, Prestige, ProDisc-C, PCM, etc., whose clinical effects and biomechanics have been well studied. As a newly established device, the Discover disc has only been in use in the clinic for a few years. Until now, few reports on the clinical application of Discover disc have been published. Du et al. [4] first reported the early follow-up outcomes of the Discover disc CDR, and demonstrated that it increased the FSU motion and maintained the FSU angle postoperatively. Patients achieved good clinical outcome and no complications occurred during or after the surgeries. In our study, with proper selection of patients and adequate neural decompression, the clinical outcomes have so far been satisfactory. According to Odom’s criteria, good to excellent results were achieved in 81.8 % (45/55) patients; however, some complications were identified. Migration of the prosthesis was found in six patients (10.9 %), which seemed to be frequent, although they were without any adverse clinical symptoms and no prosthesis needed to be removed. Because fixation may be the key to the long-term success of CDR, long-term fixation of the Discover disc is provided by teeth and a layer of TPS and HA. The causes of migration and the osseointegration at the bone–implant surface deserve further study. We would like to suggest an increase in the area of TPS and HA layers at each endplate of the Discover disc. HO was found in ten cases of Grade I or II (18.2 %) at the last follow-up, and its incidence was obviously less than in other studies [20–22].
Because the contribution of sagittal balance to operative and adjacent segmental longevity is likely to be more important than preservation of ROM [15], artificial cervical discs are expected to maintain cervical lordosis. Restoration of cervical lordosis after CDR was reported in many papers [11–14], although most artificial cervical discs are not intended to restore lordosis. In our study, the average FSU angle improved by 2.9°, endplate angle of the treated level by 3.9° and overall cervical alignment by 2.6° at the 2-year follow-up (Fig. 1). One possible reason is that the unique 7° lordosis design of the Discover disc may well restore cervical lordosis. Thus, the Discover disc may be a good candidate for patients with preoperative poor cervical alignment who wish to undergo CDR. It has been reported that spinal malalignment after CDR, such as with the Bryan disc, is likely due to design limitations [15]. Pickett et al. [5] reported that all patients implanted with the Bryan disc (n = 14) developed segmental kyphosis persisting for more than 6 months. Similarly, Fong et al. [15] reported that 90 % of patients (n = 10) had kyphosis through the operative level demonstrating a mean change in angle of −9° and a tendency toward FSU kyphosis. Losses of FSU angle were also detected in 12 cases (21.8 %) in our group, which may be caused by multi-factors including surgical techniques, prosthesis design or patient factors. In some of our cases, although intraoperative fluoroscopy confirmed that the discs were positioned correctly, these were found to be asymmetric immediately after surgery. We assume that cervical spine position during the surgical procedure and change of cervical kinematics after recovery from anesthesia may explain this phenomenon. However, kyphosis through the arthroplasty segment was thought to have no influence on clinical outcomes as well as range of motion in early follow-up [5, 15].
Motion preservation is a fundamental benefit of CDR. Most authors [1–10, 12, 19] observed the effect of general motion preservation at the implanted level regardless of the specific prosthesis design. In those studies, some groups have shown an increased motion [1–4], whereas others have shown no change [5–7] or decreased motion [8–10]. In contrast to Du et al. [4], CDR with the Discover disc was able to maintain a mean of 8.4 ± 6.3° of FSU ROM at the 2-year follow-up in our group, which was significantly less than the preoperative ROM (P = 0.008). It seems that the Discover disc can only partially maintain motion at the implanted level. Additionally, the mean overall ROM also decreased at the last follow-up in our study, though this difference did not reach statistical significance.
A number of factors have been attributed to the variability of ROM after CDR. Rabin et al. [2] reported that the greater the lordosis introduced between the prosthesis’ endplates, the more limited the segmental ROM will be. Kang et al. [3] found that disc height increments showed a significant correlation with segmental ROM, and disc height increments less than 4.0 mm could increase segmental ROM. Peng et al. [23] found that patients with more than 5 mm of postoperative disc height had significantly higher postoperative ROM than those with less than 5 mm disc height. In our study, we found no correlation between sagittal balance parameters, clinical parameters and FSU ROM. The only correlation observed was between preoperative FSU ROM and postoperative FSU ROM, which showed that postoperative FSU ROM positively correlated with preoperative FSU ROM and was also confirmed in some studies [24, 25]. This indicates that preoperative FSU ROM is an important prognostic factor for CDR in terms of motion preservation. As the preoperative FSU ROM of the patient decreased, cervical spondylosis including disc degeneration, contracture of spinal ligaments and facet capsules as well as facet arthrosis was advanced. CDR only focuses on the spondylosis in the anterior portion of the cervical spine, ignoring the problems in the posterior portion. Posterior spondylosis of cervical spine may contribute to less FSU ROM postoperatively. Thus, careful evaluation of cervical spondylosis as well as FSU ROM before CDR is necessary. Tian et al. [24] suggested that a poor preoperative ROM is a contraindication for Bryan cervical disc arthroplasty. However, severe restrictions in segmental ROM preoperatively were not always found to be associated with decreases in segmental ROM after CDR [3]. Five of six patients with preoperative FSU ROM less than 5° gained improvement of FSU ROM after CDR in our group. Therefore, this indication may not be an absolute contraindication for the Discover CDR. We assume, with adequate decompression, that in cases without severe posterior spondylosis of cervical spine the Discover CDR will improve segment ROM. Furthermore, studies focusing on other factors affecting segmental ROM in CDR are warranted.
There are some limitations in this study including the lack of a control group, the limited follow-up and the absence of an assessment of adjacent segment motion. A comparative study with other kinds of artificial cervical discs may provide further insights into the characteristics of different prostheses. Moreover, this study addresses only flexion/extension ROM and does not characterize the biomechanical behavior of the Discover disc in axial rotation and lateral bending. Other factors influencing postoperative ROM such as disc insertion angle, disc insertion depth and implant size were not analyzed in this study.
Conflict of interest
None of the authors has any potential conflict of interest. No funds were received in support of this work.
Footnotes
J. Li and L. Liang contributed equally to this paper.
References
- 1.Chang UK, Kim DH, Lee MC, Willenberg R, Kim SH, Lim J. Range of motion change after cervical arthroplasty with ProDisc-C and prestige artificial discs compared with anterior cervical discectomy and fusion. J Neurosurg Spine. 2007;7(1):40–46. doi: 10.3171/SPI-07/07/040. [DOI] [PubMed] [Google Scholar]
- 2.Rabin D, Bertagnoli R, Wharton N, Pickett GE, Duggal N. Sagittal balance influences range of motion: an in vivo study with the ProDisc-C. Spine J: Off J N Am Spine Soc. 2009;9(2):128–133. doi: 10.1016/j.spinee.2008.01.009. [DOI] [PubMed] [Google Scholar]
- 3.Kang KC, Lee CS, Han JH, Chung SS. The factors that influence the postoperative segmental range of motion after cervical artificial disc replacement. Spine J: Off J North Am Spine Soc. 2010;10(8):689–696. doi: 10.1016/j.spinee.2010.04.016. [DOI] [PubMed] [Google Scholar]
- 4.Du J, Li M, Liu H, Meng H, He Q, Luo Z. Early follow-up outcomes after treatment of degenerative disc disease with the Discover cervical disc prosthesis. Spine J: Off J North Am Spine Soc. 2011;11(4):281–289. doi: 10.1016/j.spinee.2011.01.037. [DOI] [PubMed] [Google Scholar]
- 5.Pickett GE, Mitsis DK, Sekhon LH, Sears WR, Duggal N. Effects of a cervical disc prosthesis on segmental and cervical spine alignment. Neurosurg Focus. 2004;17(3):E5. doi: 10.3171/foc.2004.17.3.5. [DOI] [PubMed] [Google Scholar]
- 6.Sasso RC, Smucker JD, Hacker RJ, Heller JG. Artificial disc versus fusion: a prospective, randomized study with 2-year follow-up on 99 patients. Spine. 2007;32(26):2933–2940. doi: 10.1097/BRS.0b013e31815d0034. [DOI] [PubMed] [Google Scholar]
- 7.Sasso RC, Best NM, Metcalf NH, Anderson PA. Motion analysis of Bryan cervical disc arthroplasty versus anterior discectomy and fusion: results from a prospective, randomized, multicenter, clinical trial. J Spinal Disord Tech. 2008;21(6):393–399. doi: 10.1097/BSD.0b013e318150d121. [DOI] [PubMed] [Google Scholar]
- 8.Nabhan A, Ahlhelm F, Shariat K, Pitzen T, Steimer O, Steudel WI, Pape D. The ProDisc-C prosthesis: clinical and radiological experience 1 year after surgery. Spine. 2007;32(18):1935–1941. doi: 10.1097/BRS.0b013e31813162d8. [DOI] [PubMed] [Google Scholar]
- 9.Park DK, Lin EL, Phillips FM. Index and adjacent level kinematics after cervical disc replacement and anterior fusion: in vivo quantitative radiographic analysis. Spine. 2011;36(9):721–730. doi: 10.1097/BRS.0b013e3181df10fc. [DOI] [PubMed] [Google Scholar]
- 10.Nabhan A, Ahlhelm F, Pitzen T, Steudel WI, Jung J, Shariat K, Steimer O, Bachelier F, Pape D. Disc replacement using Pro-Disc C versus fusion: a prospective randomised and controlled radiographic and clinical study. Eur Spine J: Off Pub Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc. 2007;16(3):423–430. doi: 10.1007/s00586-006-0226-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anakwenze OA, Auerbach JD, Milby AH, Lonner BS, Balderston RA. Sagittal cervical alignment after cervical disc arthroplasty and anterior cervical discectomy and fusion: results of a prospective, randomized, controlled trial. Spine. 2009;34(19):2001–2007. doi: 10.1097/BRS.0b013e3181b03fe6. [DOI] [PubMed] [Google Scholar]
- 12.Ahn PG, Kim KN, Moon SW, Kim KS. Changes in cervical range of motion and sagittal alignment in early and late phases after total disc replacement: radiographic follow-up exceeding 2 years. J Neurosurg Spine. 2009;11(6):688–695. doi: 10.3171/2009.7.SPINE0946. [DOI] [PubMed] [Google Scholar]
- 13.Barrey C, Champain S, Campana S, Ramadan A, Perrin G, Skalli W. Sagittal alignment and kinematics at instrumented and adjacent levels after total disc replacement in the cervical spine. Eur Spine J: Off Pub Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc. 2012;21(8):1648–1659. doi: 10.1007/s00586-012-2180-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guerin P, Obeid I, Gille O, Bourghli A, Luc S, Pointillart V, Vital JM. Sagittal alignment after single cervical disc arthroplasty. J Spinal Disord Tech. 2012;25(1):10–16. doi: 10.1097/BSD.0b013e31820f916c. [DOI] [PubMed] [Google Scholar]
- 15.Fong SY, DuPlessis SJ, Casha S, Hurlbert RJ. Design limitations of Bryan disc arthroplasty. Spine J: Off J N Am Spine Soc. 2006;6(3):233–241. doi: 10.1016/j.spinee.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 16.Johnson JP, Lauryssen C, Cambron HO, Pashman R, Regan JJ, Anand N, Bray R. Sagittal alignment and the Bryan cervical artificial disc. Neurosurg Focus. 2004;17(6):E14. doi: 10.3171/foc.2004.17.6.14. [DOI] [PubMed] [Google Scholar]
- 17.McAfee PC, Cunningham BW, Devine J, Williams E, Yu-Yahiro J. Classification of heterotopic ossification (HO) in artificial disk replacement. J Spinal Disord Tech. 2003;16(4):384–389. doi: 10.1097/00024720-200308000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Garrido BJ, Taha TA, Sasso RC. Clinical outcomes of Bryan cervical disc arthroplasty a prospective, randomized, controlled, single site trial with 48-month follow-up. J Spinal Disord Tech. 2010;23(6):367–371. doi: 10.1097/BSD.0b013e3181bb8568. [DOI] [PubMed] [Google Scholar]
- 19.Goffin J, Van Calenbergh F, van Loon J, Casey A, Kehr P, Liebig K, Lind B, Logroscino C, Sgrambiglia R, Pointillart V. Intermediate follow-up after treatment of degenerative disc disease with the Bryan cervical disc prosthesis: single-level and bi-level. Spine. 2003;28(24):2673–2678. doi: 10.1097/01.BRS.0000099392.90849.AA. [DOI] [PubMed] [Google Scholar]
- 20.Heidecke V, Burkert W, Brucke M, Rainov NG. Intervertebral disc replacement for cervical degenerative disease—clinical results and functional outcome at two years in patients implanted with the Bryan cervical disc prosthesis. Acta Neurochir. 2008;150(5):453–459. doi: 10.1007/s00701-008-1552-7. [DOI] [PubMed] [Google Scholar]
- 21.Beaurain J, Bernard P, Dufour T, Fuentes JM, Hovorka I, Huppert J, Steib JP, Vital JM, Aubourg L, Vila T. Intermediate clinical and radiological results of cervical TDR (Mobi-C) with up to 2 years of follow-up. Eur Spine J: Off Pub Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc. 2009;18(6):841–850. doi: 10.1007/s00586-009-1017-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Suchomel P, Jurak L, Benes V, 3rd, Brabec R, Bradac O, Elgawhary S. Clinical results and development of heterotopic ossification in total cervical disc replacement during a 4-year follow-up. Eur Spine J: Off Pub Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc. 2010;19(2):307–315. doi: 10.1007/s00586-009-1259-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Peng CW, Quirno M, Bendo JA, Spivak JM, Goldstein JA. Effect of intervertebral disc height on postoperative motion and clinical outcomes after Prodisc-C cervical disc replacement. Spine J: Off J N Am Spine Soc. 2009;9(7):551–555. doi: 10.1016/j.spinee.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 24.Tian W, Han X, Liu B, Li Q, Hu L, Li ZY, Yuan Q, He D, Xing YG. Clinical and radiographic results of cervical artificial disc arthroplasty: over three years follow-up cohort study. Chin Med J. 2010;123(21):2969–2973. [PubMed] [Google Scholar]
- 25.Kim SW, Paik SH, Castro PA, Baek SW, Shin DJ, Kwak YH, Ju YS. Analysis of factors that may influence range of motion after cervical disc arthroplasty. Spine J: Off J N Am Spine Soc. 2010;10(8):683–688. doi: 10.1016/j.spinee.2010.04.027. [DOI] [PubMed] [Google Scholar]