Abstract
Purpose
The effectiveness of vertebral augmentation techniques is a currently highly debated issue. The biomechanical literature suggests that cement filling volumes may play an important role in the “dosage” of vertebral augmentation and its pain alleviating effect. Good clinical data about filling volumes are scarce and most patient series are small. Therefore, we investigated the predictors of pain alleviation after balloon kyphoplasty in the nationwide SWISSspine registry where cement volumes are also recorded.
Methods
All single-level vertebral fractures with no additional fracture stabilization and availability of at least one follow-up within 6 months after surgery were included. The following potential predictors were assessed in a multivariate logistic regression model with the group’s average pain alleviation of 41 points on VAS as the desired outcome: patient age, patient sex, diagnosis, preoperative pain, level of fracture, type of fracture, age of fracture, segmental kyphotic deformity, cement volume, vertebral body filling volume, and cement extrusions.
Results
There were 194 female and 82 males with an average age of 70.4 and 65.3 years, respectively. Female patients were about twice as likely for achieving the average pain relief compared to males (p = 0.04). The preoperative pain level was the strongest predictor in that the likelihood for achieving an at least 41-point pain relief increased by about 8 % with each additional point of preoperative pain (p < 0.001). A thoraco-lumbar fracture had a three times higher odds for the average pain relief compared with a lumbar fracture (p = 0.03). An A.3.1 fracture only had about a third of the probability for average pain relief compared with an A.1.1 fracture (p = 0.004). Cement volumes up to 4.5 ml only had an approximately 40 % chance for a minimum 41-point pain alleviation as compared with cement volumes of at least 4.5 ml (p = 0.007). In addition, the relationship between cement volume and pain alleviation followed a dose-dependent pattern.
Conclusions
Cement volume was revealed as a significant predictor for pain relief in BKP. Cement volume was the third most important influential covariate and the most important modifiable and operator dependent one. The clear dose-outcome relationship between cement filling volumes and pain relief additionally supports these findings. Cement volumes of >4.5 ml seem to be recommendable for achieving relevant pain alleviation. Patient sex and fracture type and location were further significant predictors and all these covariates should be recorded and reported in future studies about the pain alleviating effectiveness of vertebral augmentation procedures.
Keywords: Kyphoplasty, Predictors, Pain relief, Cement volume, SWISSspine
Introduction
One of the currently highly debated issues in spinal surgery is the effectiveness of vertebral augmentation techniques such as vertebroplasty (VP) or balloon kyphoplasty (BKP). Both surgical procedures are applied for treatment of osteoporotic vertebral fractures with the goal of relieving pain and realigning the fractured vertebral body to some extent. During VP bone cement is percutaneously injected into a fractured vertebra to stabilize it, which is the main goal of the procedure. Kyphoplasty is a variation of VP that attempts to achieve more realignment and less cement extrusion by creating a void with an expandable balloon that is filled with bone cement after balloon removal. Both procedures, however, aim at an immediate and clinically relevant pain relief as their main goal.
The two investigations [1, 2] comparing VP to “sham” operations published in the New England Journal of Medicine (NEJM) indicated that VP is no more effective than injection of local anaesthetic at the pedicle entry site, i.e., a facet joint infiltration. In view of the widespread use of vertebral augmentation techniques, their newly questioned effectiveness has already had implications for clinical guidelines and reimbursement policies.
Other authors have meanwhile pointed out that these findings are clearly at odds with the previously published clinical investigations which indicate a significant clinical benefit of vertebral augmentation procedures, such as vertebro- and kyphoplasty over conservative treatment [3, 4]. In addition, new RCTs like the Vertos II trial confirm the results from observational studies [5]. This discrepancy can only reasonably have two explanations: the placebo effect has been severely underestimated in previously published investigations or the application of the vertebral augmentation was insufficient compared to other studies. The very basic foundation of any RCT is to ensure that all patients in the treatment arm have actually received the treatment in a manner that may be presumed to be effective, a fact that we propose to refer to as “clinical validity”. VP is a complex procedure to investigate with an RCT as there are considerable variables in conducting the actual procedure. Besides the technique of insertion of the delivery needle, the injection or dosage of the “active agent”—generally, polymethylmethacrylate (PMMA)—is modifiable to a great extent and entirely operator dependent. The instillation of PMMA into the fractured vertebral body improves the mechanical properties and is presumed to provide pain relief by reducing painful loading and abnormal micromotion. Clearly, a minimal amount of PMMA will have no appreciable effect and likewise an excessive amount hardens the vertebral body beyond its original state and may have an adverse effect on adjacent osteoporotic vertebrae and additionally cause extravasations. Boszczyk [6] has summarized biomechanical data demonstrating that a minimum necessary cement volume is required for achieving an appreciable biomechanical effect. At the same time, the information about filling volumes in the two NEJM RCTs was either incomplete, insufficiently detailed or pointed at filling volumes that were too small for reaching the above-described biomechanical stabilization of the treated VBs in the lower thoracic and lumbar spine.
Large observational studies like registries documenting numerous covariates and representing the “natural dosing” of a surgical intervention in the day-to-day clinical setting represent excellent possibilities for analyzing procedural or patient characteristics with an influence on the outcome [7]. Since 2005, BKP procedures and outcomes have been documented in a government mandated Swiss nationwide registry. The setup and details of “SWISSspine” have previously been published [8]. The current study hypothesized that cement volume had a significant influence on pain alleviation after BKP.
Materials and methods
Initiated in March 2005, the SWISSspine registry is ongoing to the present. Following the principle of “coverage with evidence generation” its purpose is to provide evidence of the safety and what Archie Cochrane described as “efficiency” of BKP, that is, its performance in the clinical setting [9]. This term is nowadays rather referred to as “effectiveness”, being high on external validity but at the expense of internal validity like, for example, careful controls. The Institute for Evaluative Research in Medicine at the University of Bern (IEFM), an international leader in the field of registry implementation, was mandated to serve as technology provider and organizer of the SWISSspine registry. Documentation forms and outcome instruments that are used for the BKP arm of the SWISSspine registry are the following:
Primary intervention form (surgeon administered),
Follow-up form (surgeon administered),
Euroqol-5D (EQ-5D) general Quality of Life (QoL) form (patient assessment),
North American Spine Society disease specific (NASS) QoL form (patient assessment) with VAS,
Comorbidity questionnaire (patient assessment),
Two patient consent forms (one remains at the treatment center and one at IEFM),
One annotation form about the registry and its purpose (also signed by patient).
At the time of surgery, the primary intervention form is completed by the surgeon. Informed consent about participation in the registry has to be given by the patient as well as completed EQ-5D, NASS, and comorbidity questionnaires. During follow-ups at 3 months, 1 year, and annually thereafter, questionnaires are completed by the surgeon. Patients are again asked to complete the EQ-5D and NASS questionnaires.
Inclusion criteria
Inclusion criteria for the analysis were a single-level vertebral fracture treated with BKP and no additional fracture stabilization, and availability of at least one follow-up within 6 months after surgery. Pre- and postoperative information documented by the surgeon and information about disease specific quality of life (NASS incl. pain VAS) as recorded by the patient needed to be available for feeding these covariates into the multivariate logistic regression. The group`s average back pain alleviation of 41 points on VAS 0-100 was used as the success or failure criterion. Influence of the following covariates on achieving or not achieving 41 points of pain alleviation was assessed:
Patient age
Patient sex
Diagnosis
Preoperative pain
Level of fracture
Type of fracture
Age of fracture
Segmental kyphosis angle
Cement volume
VB filling volume
Extrusions
Patient age was used as a continuous and sex as a categorized variable. Based on previous findings presence or absence of a pharmacologically treated depression or preoperative general quality of life (EQ-5D score) was not included in the model [8]. The level of the monosegmental fracture or rather localization of the treatment was categorized into three groups: (1) thoracic vertebral bodies Th4–Th10, (2) thoraco-lumbar vertebrae Th11–L2, (3) lumbar vertebrae L3–L5. Fracture types were categorized as A.1.1, A.1.2, A.3.1 or other. Preoperative segmental kyphotic angles were categorized according to the SWISSspine BKP forms into none, 10°–15°, 16°–20°, 21°–25°, 26°–30°, >30°. Fracture age was detailed as less or more than 8 weeks since onset of symptoms. Cement extrusions were recorded as present or not present, independent of direction of extrusion or several extrusions from one and the same fracture site. Cement volumes were categorized according to the SWISSspine BKP case report forms into <3, 3–4.5, 4.6–6, 6.1–7.5, and >7.5 ml but for the final model they were converted into a binary format with ≤4.5 and >4.5 ml. Vertebral body filling volumes (%) were calculated in a sex and level adjusted way by using the mean values of the above mentioned cement volume categories (1.5, 3.75, 5.3, 6.8, 9 ml) and dividing them by the respective vertebral body volumes published by Limthongkul et al. [10].
Statistical analysis
A multivariate logistic regression model was built with pain alleviation greater or smaller than 41 points on VAS as the outcome. The above-described covariates were fed into the model and the significant ones were identified with backward elimination. The level of significance was set to α = 0.05. All statistical analyses were conducted using SAS 9.2 (SAS Institute Inc, Cary, NC, USA).
Results
Patient characteristics
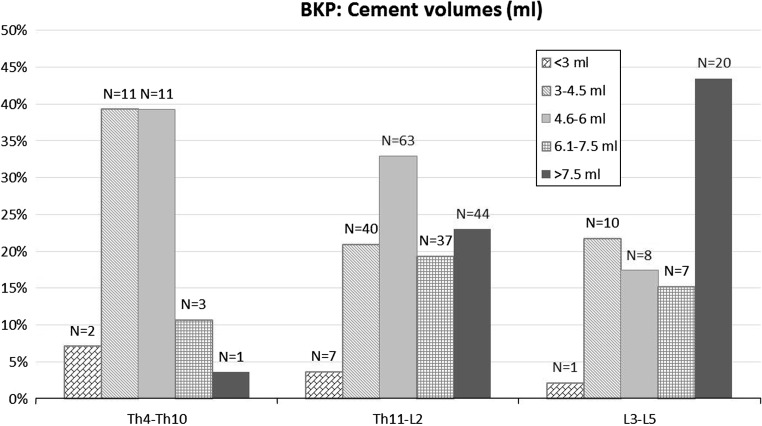
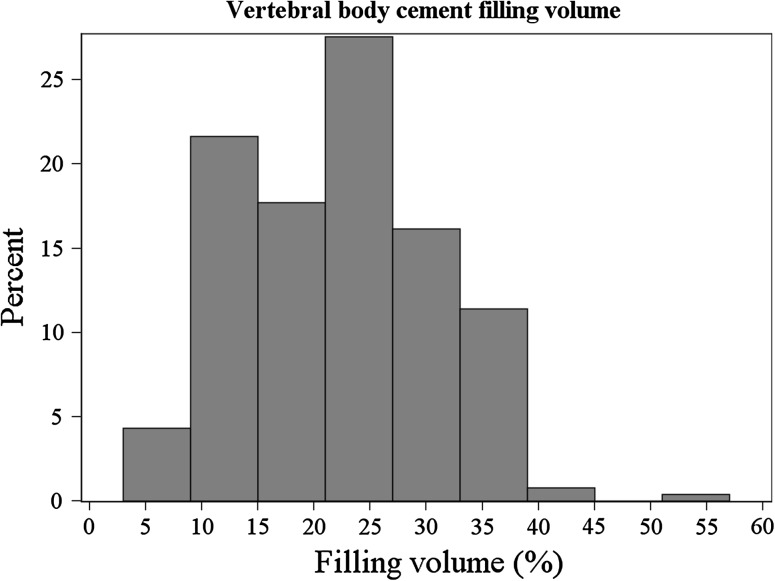
There were 194 female and 82 male with an average age of 70.4 and 65.3 years, respectively. 61 % of cases were treated for an osteoporotic fracture, 36.4 % for a traumatic one, and 2.6 % for a lytic fracture. Stratified by sex, 68.3 % of women had an osteoporotic fracture, 29.1 % a traumatic one and 2.6 % a lytic fracture. In men the distribution was 43.8, 53.8 and 2.4 %, respectively. The average follow-up time was 106 days. Mean preoperative pain level was 69.3 points on VAS 0–100, the postoperative one was 28.7. Stratified by sex mean preoperative pain levels were 71 (female) and 65.2 (male) points. The mean postoperative pain levels were 27.1 (female) and 32.4 (male) points. Cement volumes between 3 and 6 ml were predominantly used in the thoracic spine, those between 4.6 and 6 ml in the thoraco-lumbar junction, and those >7.5 ml in the lumbar spine (Fig. 1). Overall distribution of cement volume categories with extrusion and fracture type rates are shown in Fig. 2. Mean vertebral body filling volumes were 22.1 % (min 5.1 %, max 44.3 %) with one outlier having received 9 ml of cement with a filling volume of 56.3 % (Fig. 3). There were cement extrusions in a total of 27.2 % of cases. 10.6 % of fractures were located between Th4 and 10, 71.8 % between Th11 and L2, and 17.6 % between L3 and L5. There were 200 fractures treated earlier than 8 weeks after their occurrence, and 76 treated later than 8 weeks.
Fig. 1.
Distribution of cement volume categories across three spinal levels
Fig. 2.
Overall distribution of cement volume categories and related extrusion and fracture type rates. “Other” fracture types not shown
Fig. 3.
Distribution of approximated cement filling volumes, adjusted for sex and spinal level
Predictors for pain alleviation of at least 41 VAS points
While patient age did not have a significant influence on achieving the average pain relief of 41 points, patient sex did. Female patients were about twice as likely for achieving this amount of pain relief compared to males (p = 0.04). The preoperative pain level was the strongest predictor in that the likelihood for achieving an at least 41 point pain relief increased by about 8 % with each additional point of preoperative pain (p < 0.001) (Table 1).
Table 1.
Possible predictors for pain alleviation of at least 41 VAS points in BKP
| Predictor | p value | OR | 95 % CI |
|---|---|---|---|
| Age of patient | 0.27 | n.s | n.a. |
| Sex of patient | 0.04* | 2.09: female vs male | 1.05–4.02 |
| Fracture diagnosis | 0.45 | n.s. | n.a. |
| Preoperative pain | <0.001* | 1.08 per additional preoperative point on VAS | 1.06–1.10 |
| Fracture type | 0.004* | 0.23: A.3.1 vs A.1.1 | 0.07–0.74 |
| Fracture age | 0.31 | n.s | n.a. |
| Fracture location | 0.03* | 3.04: Th11–L1 vs L3–L5 | 1.3–7.1 |
| Segmtl. kyphosis angle | 0.13 | n.s. | n.a. |
| Cement volume | 0.007* | 0.36: ≤4.5 vs >4.5 ml | 0.17–0.76 |
| VB filling volume | 0.58 | n.s. | n.a. |
| Cement extrusion | 0.67 | n.s. | n.a. |
n.s. not significant, n.a. not applicable
* Significant predictor
Fracture characteristics
The location of fracture, simplified as thoracic, thoraco-lumbar or lumbar, and the fracture type both had an influence on pain relief. A thoraco-lumbar fracture had an about three times higher likelihood for achieving the average pain relief compared with a lumbar fracture (p = 0.03), and an A.3.1 fracture did only have about a third of the probability compared with an A.1.1 fracture (p = 0.004). The fracture etiology and vertebral body fracture deformation, expressed as segmental kyphotic angle, did not have a significant influence, neither did fracture age (Table 1).
Operator-dependent covariates
A cement extrusion did not influence the odds for achieving the average pain relief. Cement volume, however, did. Volumes up to 4.5 ml only had an approximately 40 % chance for a minimum 41 point pain alleviation as compared with cement volumes of more than 4.5 ml (p = 0.009) (Table 1). The relationship between cement volume and pain alleviation followed a dose-dependent pattern as illustrated in Table 2. The percentage of patients with a pain relief of at least 41 points increased from 20 to 68.1 % in proportion with the increase in cement volume up to 7.5 ml. Also, mean and median pain alleviation levels increased with each cement volume category and were the highest in the volume class of 6–7.5 ml. Cement volumes between 4.5 and 7.5 ml seem to be the ideal filling volumes for pain alleviation in BKP. Finally, vertebral body filling volumes did not have a significant influence on pain relief, neither as a continuous nor as a categorized covariate.
Table 2.
Distribution of cement volumes and extents of pain alleviation
| Cement volume (ml) | % of sample | Mean pain alleviation VAS (pts) | Median pain alleviation VAS (pts) | % of cases with pain alleviation >41 VAS points within stratum (%) |
|---|---|---|---|---|
| <3 | 0.03 | 27 | 35 | 20 |
| 3–4.5 | 23.1 | 40 | 40 | 46.8 |
| 4.6–6 | 30.6 | 40 | 50 | 53.7 |
| 6.1–7.5 | 17.5 | 50 | 60 | 68.1 |
| >7.5 | 25 | 37 | 40 | 47.8 |
Discussion
The hypothesis of the current study was confirmed and cement volume was revealed as a significant predictor for pain relief in BKP. With the exception of the preoperative pain level of the patient and the fracture type, cement volume was the third most important influential covariate and the most important modifiable and operator-dependent one. The clear dose–outcome relationship between cement filling volumes and pain relief additionally supports these findings.
Patient sex was another patient characteristic significantly influencing postoperative pain levels. Fracture specific predictors for pain relief were fracture type and fracture location. Patient age, fracture age and etiology, segmental kyphotic deformity, cement filling volume, and presence or absence of extrusions did not significantly influence pain relief.
To the best of our knowledge this is the first study revealing cement volume as a significant covariate in the complex interplay of factors that may or may not lead to clinically relevant pain relief after vertebral augmentation with BKP. Only one other study investigated on this issue and concluded that “pain and disability scores improved pre- to posttreatment, even were low cement volumes are used”. This study by Ioannou et al. [11], did, however, only investigate on 20 patients and focused on the significance of pre- to postoperative pain relief, and not, as the current study did, on the probability for reaching what could be considered the benchmark of pain relief, i.e., the average pain alleviation of a large patient sample. The preoperative kyphosis, representing the extent of fracture related vertebral body deformation, may intuitively be considered as an important factor determining the amount of injectable cement volume and therefore influencing the interplay between absolute cement volume and pain relief, but it could not be revealed as a significant predictor with our data. This may also have to do with only the segmental kyphosis being available for analysis, whereas the local kyphosis would have been the more precise measure. Instead, fracture location and to an even more significant extent fracture type are further predictors for pain relief. We could not find any article investigating the role of the spinal level in BKP pain relief but static and load issues are the most probable explanations why lumbar VBs had less BKP benefits than thoraco-lumbar ones. Finally, the less traumatic cranial endplate impression fractures (A.1.1) seem to have a significantly better prognosis regarding pain relief than cranial burst fractures (A.3.1) and the influence of fracture type on pain may overshadow that of the preoperative local kyphosis or vertebral body filling volume. The literature is also scarce regarding this topic but remaining instability after burst fracture or cement rather distributing between the fracture parts instead within them may be possible explanations.
Most other studies focused on the role of cement volume in VP and the large majority of them dealt with mechanical behavior, stiffness and stress distribution. Despite its subtitle “Only Small Cement Volumes Are Required to Normalize Stress Distributions on the Vertebral Bodies”, Luo et al. [12] concluded that “3.5 ml of PMMA largely restored normal stress distributions to fractured and adjacent vertebral bodies, but 7 ml were required to restore motion segment stiffness and load-sharing between the vertebral bodies and neural arch”. Molloy et al. [13] applied cement volumes between 2 and 8 ml and found weak correlations between percentage of fill and restored strength and stiffness. On average, restoration of strength and stiffness required vertebral body cement fills of 16.2 and 29.8 %, respectively. Finally, Liebschner et al. developed a finite element model of L1, filled it with volumes between 1 and 7 ml and showed that only a small amount of bone cement (14 % fill or 3.5 cm3) was necessary to restore stiffness of the damaged vertebral body to the predamaged value. Use of a 30 % fill increased stiffness by more than 50 % compared with the predamaged value. He concluded that greater filling can result in substantial increase in stiffness well beyond the intact level. Such overfilling also renders the system more sensitive to the placement of the cement because asymmetric distributions with large fills can promote single-sided load transfer [14]. Looking at the approximated mean filling volume of 22.1 % in the current study, real life vertebral body filling volumes with BKP were well within those researched in biomechanical experiments and models. Despite minimum levels going down to 5 %, the normal distribution of the cement filling volume curve was probably responsible for this covariate not becoming a significant predictor for pain relief.
The literature about outcome predictors for BKP is scarce and rather focuses on preoperative diagnostics and patient selection in a sense that cases with a bone edema detectable on MRI or scintigraphy were experiencing very good pain relief [15, 16]. Investigations for VP are more numerous. Alvarez was the first author to look for predictors of outcome of percutaneous VP in the clinical setting. He retrospectively analyzed his own series of 278 cases and found ASA score and extent of vertebral body height loss to be significant predictors for clinical success in a multivariate regression analysis [17]. Kaufmann et al. retrospectively looked at clinical outcomes of 158 cases from 1 week up to 2 years after surgery and concluded that there was no significant association between the volume of cement injected and the clinical outcomes for post-procedure pain and medication use. VP surgeons need not feel compelled to achieve particular cement volumes injected in the pursuit of better clinical outcomes, but should strive to achieve the maximal safe filling of individual vertebral bodies [18]. Alvarez included single and multilevel cases which does add statistical complexity to the predictor search and Kaufmann used cement volume as a continuous covariate instead of a categorized one, as we had to do. In addition, there were not too many cases with really low cement volumes in his sample. This makes it more difficult to find significance in relation with the primary outcome parameter or to find an exact threshold level for a clinically effective cement volume.
Kaufmann did not find associations between cement filling volume and likelihood for cement extrusions in VP [18]. Ren et al. [19], however, revealed cement volume and vertebral wall incompetence as significant predictors for cement leakage in BKP in their multivariate model of 171 vertebral bodies. In our study, extrusion rates varied between 22 and 30 % in the different volume categories and a separate analysis on the same monosegmental sample (submitted for publication) revealed patient sex as highly significant and cement volume as borderline significant leakage predictor. Women were more likely to show leakage and cement volumes above 4.5 ml were more likely than volumes below 4.5 ml. The probably most influential factor on leakage, cement viscosity, had not been assessed in any of the above cited studies and was not recorded on the SWISSspine forms. It seems, however, of more interest in VP where the use of highly viscous cements leads to lower extrusion rates comparable with those of BKP [20]. This was previously confirmed by Rapan et al. and Anselmetti et al. [21, 22] who found significantly less extravasations and related complications in patients treated with high viscous cement.
Aspired cement volumes need to be put in relation to the volumes of vertebral bodies which increase the more caudally they are located (31 % L3–5 fractures in volume category >7.5 ml) and the type of fracture may also have an influence (33.3 % A3.1 fractures in volume category >7.5 ml). However, the overall distribution of vertebral body filling volumes was very homogeneous.
Weaknesses and strengths
SWISSspine is an observational study which was not designed for the current analysis and did not have any data monitoring and validation mechanisms. On the other hand, the crudeness of the cement volume categories may result in relatively reliable estimates and there was no obvious reason for the surgeons to document them in a dishonest manner. The real life nationwide setting and the large number of patients and health care providers contributing data to the SWISSspine data pool increase the external validity of our findings with an admittably limited internal validity. Registry data help in generating hypotheses which need to be challenged in more controlled study designs if possible.
Conclusion
Cement volume was revealed as a significant modifiable predictor for pain alleviation in BKP. However, instead of striving for maximum filling volumes, surgeons need to be aware of the increased risk of cement extrusions. Cement types with higher viscosity may help apply the procedure with a sufficiently high “dosage” without increasing harm for the patient. Cement volumes >4.5 ml seem to be recommendable for achieving relevant pain alleviation.
Acknowledgments
We are thankful to the Swiss Spine Society and the SWISSspine registry group who made this research possible by populating the database with their valuable and much appreciated entries. The Kyphoplasty group contributing data to the current study is comprised of the 47 following surgeons (in order of case contribution): Maestretti G (70 cases), Forster T (64 cases), Schueler M (59 cases), Sgier F (58 cases), Aebi M (50 cases), Beele B (39 cases), Bärlocher C (32 cases), Kroeber M (28 cases), Schaeren S (26 cases), Broger I (24 cases), Blay M (23 cases), Etter C (21 cases), Mueller U (20 cases), Mueller K (20 cases), Berlemann U (19 cases), Binkert C (14 cases), Moulin P (12 cases), Lutz T (11 case), Sheikh-Sarraf B (9 cases), Schwarz U (9 cases), Heimberger K (8 cases), Kuehlling F (8 cases), Morard M (7 cases), Otten P (7 cases), Stoll T (7 cases), Kunz S (6 cases), Martinez R (6 cases), Tessitore E (6 cases), Jeanneret B (5 cases), Payer M (5 cases), Baur M (4 cases), Hamburger C (4 cases), Markwalder T (4 cases), Hausmann O (3 cases), Schirm A (3 cases), Van Dommelen K (3 cases), Heinzelmann M (2 cases), Panche T (2 cases), Schwarzenbach O (2 cases), Wanner G (2 cases), Bachmann M (1 case), Bothmann M (1 case), Koehler M (1 case), Ramadan A (1 case), Schizas C (1 case), Vernet O (1 case), Witzmann A (1 case).
There was no external source of funding for the current study.
Conflict of interest
None.
Footnotes
On behalf of the SWISSspine Registry Group.
References
- 1.Buchbinder R, Kallmes D, Glasziou P (2010) Vertebroplasty versus conservative treatment for vertebral fractures. Lancet 376:2070–2071; author reply 2071–2072. doi:10.1016/S0140-6736(10)62288-X [DOI] [PubMed]
- 2.Kallmes DF, Comstock BA, Heagerty PJ, Turner JA, Wilson DJ, Diamond TH, Edwards R, Gray LA, Stout L, Owen S, Hollingworth W, Ghdoke B, Annesley-Williams DJ, Ralston SH, Jarvik JG. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med. 2009;361:569–579. doi: 10.1056/NEJMoa0900563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aebi M. Vertebroplasty: about sense and nonsense of uncontrolled “controlled randomized prospective trials”. Eur Spine J. 2009;18:1247–1248. doi: 10.1007/s00586-009-1164-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bono CM, Heggeness M, Mick C, Resnick D, Watters WC., 3rd North American Spine Society: newly released vertebroplasty randomized controlled trials: a tale of two trials. Spine J. 2010;10:238–240. doi: 10.1016/j.spinee.2009.09.007. [DOI] [PubMed] [Google Scholar]
- 5.Klazen CA, Lohle PN, de Vries J, Jansen FH, Tielbeek AV, Blonk MC, Venmans A, van Rooij WJ, Schoemaker MC, Juttmann JR, Lo TH, Verhaar HJ, van der Graaf Y, van Everdingen KJ, Muller AF, Elgersma OE, Halkema DR, Fransen H, Janssens X, Buskens E, Mali WP. Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): an open-label randomised trial. Lancet. 2010;376:1085–1092. doi: 10.1016/S0140-6736(10)60954-3. [DOI] [PubMed] [Google Scholar]
- 6.Boszczyk B. Volume matters: a review of procedural details of two randomised controlled vertebroplasty trials of 2009. Eur Spine J. 2010;19:1837–1840. doi: 10.1007/s00586-010-1525-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Melloh M, Roder C, Staub LP, Zweig T, Barz T, Theis JC, Muller U. Randomized-controlled trials for surgical implants: are registries an alternative? Orthopedics. 2011;34:161. doi: 10.3928/01477447-20110124-03. [DOI] [PubMed] [Google Scholar]
- 8.Diel P, Reuss W, Aghayev E, Moulin P, Roder C. SWISSspine-a nationwide health technology assessment registry for balloon kyphoplasty: methodology and first results. Spine J. 2010;10:961–971. doi: 10.1016/j.spinee.2009.08.452. [DOI] [PubMed] [Google Scholar]
- 9.Cochrane AL. Archie Cochrane in his own words. Selections arranged from his 1972 introduction to “Effectiveness and efficiency: random reflections on the health services” 1972. Control Clin Trials. 1989;10:428–433. doi: 10.1016/0197-2456(89)90008-1. [DOI] [PubMed] [Google Scholar]
- 10.Limthongkul W, Karaikovic EE, Savage JW, Markovic A. Volumetric analysis of thoracic and lumbar vertebral bodies. Spine J. 2010;10:153–158. doi: 10.1016/j.spinee.2009.11.018. [DOI] [PubMed] [Google Scholar]
- 11.Ioannou M, Roumeliotis G, Limaxis E, Theodorou O (2010) Efficacy and safety of balloon kyphoplasty-are high cement volumes required? Internet J Minim Invasive Spinal Technol 5(Supplement III to IJMIST IV). doi:10.5580/22af
- 12.Luo J, Daines L, Charalambous A, Adams MA, Annesley-Williams DJ, Dolan P. Vertebroplasty: only small cement volumes are required to normalize stress distributions on the vertebral bodies. Spine (Phila Pa 1976) 2009;34:2865–2873. doi: 10.1097/BRS.0b013e3181b4ea1e. [DOI] [PubMed] [Google Scholar]
- 13.Molloy S, Mathis JM, Belkoff SM. The effect of vertebral body percentage fill on mechanical behavior during percutaneous vertebroplasty. Spine (Phila Pa 1976) 2003;28:1549–1554. [PubMed] [Google Scholar]
- 14.Liebschner MA, Rosenberg WS, Keaveny TM. Effects of bone cement volume and distribution on vertebral stiffness after vertebroplasty. Spine (Phila Pa 1976) 2001;26:1547–1554. doi: 10.1097/00007632-200107150-00009. [DOI] [PubMed] [Google Scholar]
- 15.Grafe I, Nöldge G, Weiss C, Libicher M, Baier M, Nawroth P, Meeder P-J, Wiedenhöfer B, Kasperk C. Prediction of immediate and long-term benefit after kyphoplasty of painful osteoporotic vertebral fractures by preoperative MRI. Eur J Trauma Emerg Surg. 2011;37:7. doi: 10.1007/s00068-010-0050-9. [DOI] [PubMed] [Google Scholar]
- 16.Karam M, Lavelle WF, Cheney R. The role of bone scintigraphy in treatment planning, and predicting pain relief after kyphoplasty. Nucl Med Commun. 2008;29:247–253. doi: 10.1097/MNM.0b013e3282f30598. [DOI] [PubMed] [Google Scholar]
- 17.Alvarez L, Perez-Higueras A, Granizo JJ, de Miguel I, Quinones D, Rossi RE. Predictors of outcomes of percutaneous vertebroplasty for osteoporotic vertebral fractures. Spine (Phila Pa 1976) 2005;30:87–92. doi: 10.1097/00007632-200501010-00016. [DOI] [PubMed] [Google Scholar]
- 18.Kaufmann TJ, Trout AT, Kallmes DF. The effects of cement volume on clinical outcomes of percutaneous vertebroplasty. AJNR Am J Neuroradiol. 2006;27:1933–1937. [PMC free article] [PubMed] [Google Scholar]
- 19.Ren H, Shen Y, Zhang YZ, Ding WY, Xu JX, Yang DL, Cao JM. Correlative factor analysis on the complications resulting from cement leakage after percutaneous kyphoplasty in the treatment of osteoporotic vertebral compression fracture. J Spinal Disord Tech. 2010;23:e9–e15. doi: 10.1097/BSD.0b013e3181c0cc94. [DOI] [PubMed] [Google Scholar]
- 20.Georgy BA. Clinical experience with high-viscosity cements for percutaneous vertebral body augmentation: occurrence, degree, and location of cement leakage compared with kyphoplasty. AJNR Am J Neuroradiol. 2010;31:504–508. doi: 10.3174/ajnr.A1861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rapan S, Jovanovic S, Gulan G, Boschi V, Kolarevic V, Dapic T. Vertebroplasty—high viscosity cement versus low viscosity cement. Coll Antropol. 2010;34:1063–1067. [PubMed] [Google Scholar]
- 22.Anselmetti GC, Zoarski G, Manca A, Masala S, Eminefendic H, Russo F, Regge D. Percutaneous vertebroplasty and bone cement leakage: clinical experience with a new high-viscosity bone cement and delivery system for vertebral augmentation in benign and malignant compression fractures. Cardiovasc Intervent Radiol. 2008;31:937–947. doi: 10.1007/s00270-008-9324-6. [DOI] [PubMed] [Google Scholar]