Abstract
Purpose
The use of percutaneous iliosacral screw fixation as a treatment of sacroiliac joint pain has been reported to be successful. This study was a prospective single surgeon series to evaluate the short-term outcomes of patients who underwent percutaneous sacroiliac joint stabilisation.
Methods
Between July 2004 and February 2011, 73 patients underwent percutaneous sacroiliac joint fusion in our unit. All patients completed a short form (SF)-36 questionnaire, visual analogue pain score and Majeed scoring questionnaire prior to treatment and at last follow-up.
Results
55 patients (9 male and 46 female) completed follow-up. The average follow-up period was for 36.18 months (range 12–84). The mean preoperative SF-36 scores were 26.59 for physical health and 40.38 for mental health. The mean postoperative SF-36 scores were 42.93 for physical health and 52.77 for mental health. The mean visual analogue pain scores were 8.1 preoperative and 4.5 postoperative. The mean pelvic specific scoring were 36.9 preoperative and 64.78 postoperative. We noted that patients who had previous instrumented spinal surgery did significantly worse than those who had not. We had two nerve root-related complications.
Conclusion
We conclude that in selected patient group who respond positively to CT-guided injection, a percutaneous SI joint stabilisation is beneficial in effecting pain relief and functional improvement.
Keywords: Sacroiliac joint stabilisation, Percutaneous, Sacroiliac joint pain, Failed back syndrome, Sacroiliac joint pain
Introduction
The sacroiliac joint as a cause of lower back and buttock pain is often undiagnosed. Some studies have found up to 22.5 % of referred nonspecific back pain to be sourced to the sacroiliac joint [1]. Although it is prudent to exhaust all nonsurgical means in the treatment of sacroiliac joint pain, there remains a group of patients who do not improve without surgical intervention. Open procedures for sacroiliac joint fusion are major undertakings, with large incisions and notable complications [2]. Percutaneous iliosacral screw fixation has long been considered a safe and predictable treatment for the management of disrupted sacroiliac joints with unstable pelvic ring injuries [3]. The use of percutaneous iliosacral screw fixation as a treatment of sacroiliac joint pain has been reported to be successful [1, 4, 5], however, these studies have small patient numbers. We have been undertaking elective percutaneous sacroiliac joint stabilisation in our institution for several years, and we report our experience in using this technique.
Methods
Our unit is a tertiary referral centre for spine and pelvic pathology. For the majority of the time this study was underway, the senior author was the only surgeon surgically intervening for sacroiliac joint disease in our region with a patient population of approximately 3,000,000. A total of 73 patients underwent percutaneous sacroiliac joint stabilisation in our unit by a single surgeon, between July 2004 and February 2011. All patients completed a short form (SF)-36 questionnaire [6] to record general mental and physical health, a visual analogue pain score and a pelvic specific questionnaire (Majeed scoring system) [7] prior to treatment. Routinely, the patient was followed-up at 6 weeks, 3 months, 6 months and 1 year, with anteroposterior (Barsony view), inlet and outlet radiographs being taken at 6 months and 1 year. The patients were then followed yearly for a clinical assessment. The final outcome was recorded by postal questionnaire with a mean follow-up of 36 months (range 12–84 months). There were 55 patients who completed follow-up questionnaires, 18 were lost to follow-up despite telephone and secondary postal requests.
Diagnosis
The majority of the patients had been referred to our tertiary referral unit having already undergone investigation and conservative management under the care of other secondary care physicians and surgeons. Therefore, there was a significant period of elapsed time from symptom onset and being managed under our care. A corroborative history and physical assessment gave an indication that the sacroiliac joint was the source of pain; however, the evidence of provocative tests in the diagnosis of sacroiliac joints is limited [8]. On history, the patients generally complained of buttock pain with referral of pain to ipsilateral posterior thigh. The patient’s endurance capacity for standing, walking and sitting was also diminished. The most symptomatic of patients could not load their ipsilateral ischium for any prolonged length and would fidget whilst sitting. Clinical examination included palpation over the sacroiliac joints and combination of iliac gapping/distraction test [9], iliac compression/approximation test [9], Patrick test [9], posterior pelvic pain provocation test [9], Gaenslen test [10], Drop test [11] and the active straight leg raising test. Patients had a varied combination of positivity amongst these tests. Plain radiographs, CT, isotope bone scans and MRI investigations have poor evidence in identifying sacroiliac joint syndrome [12]. However, plain radiographs were helpful in the patients with arthritis and to exclude other pathology. The gold standard in diagnostic accuracy of sacroiliac joint disease is a CT-guided sacroiliac joint injection of both local anaesthetic and steroid [12]. A positive result from a CT-guided sacroiliac joint injection was crucial to being considered for percutaneous stabilisation. Patients were seen 3–6 months post-CT-guided intra-articular injection to assess their clinical outcome and symptom control. At diagnosis, referral was made to our physiotherapy department for specific sacroiliac joint rehabilitation. The indication for sacroiliac joint stabilisation was considered if the patient reported severe unrelenting pain relating to the sacroiliac joint for over a year duration, despite initial significant improvement with CT-guided injection and exhaustive conservative management including sacroiliac joint specific rehabilitation. All women of childbearing age were counselled prior to surgery on the possible risks peril-natal and were told to discuss with their obstetricians the need for elective caesarean section if they were to conceive.
Surgical technique
Preoperative CT performed during guided sacroiliac joint injection was helpful in illustrating any sacral dysmorphism and planning the operation. The size of the sacral ala safe corridor was measured to ensure that the anchorage cage size was appropriate. The patient was positioned supine on a radiolucent table, with a 100-ml bag of normal saline placed under the lumber lordosis. Sacroiliac joint fusion was undertaken using the technique described by Khurana et al. [4]. A 2.5-mm guide wire was inserted percutaneously through the bony corridor of the sacral ala into the body of the S1 vertebrae under image intensifier guidance, with constant confirmation of safe wire progression on lateral, anteroposterior, inlet and outlet views. With confirmation of the wires safe placement, a 20-mm incision was placed around the wire and blunt dissection was done to bone. An 8/10 mm cannulated drill was placed over the wire, then the bony corridor was tapped and a hollow modular anchorage screw, 10/12 mm (Aescalup Ltd, Tuttlingen, Germany), which is a plasma-sprayed titanium cage, was inserted until tight. The hollow modular anchorage screw was filled with a bone substitute (DBX, Demineralised Bone Matrix, Synthes Inc., West Chester, PA, USA) prior to insertion. Most patients typically needed two interrupted nylon sutures for closure. Postoperatively, the patient was allowed to bear weight within the limits of pain with the use of crutches for the first 2 weeks.
We have not encountered any patient so far that we declined surgery for technical reasons. We did not undertake surgery on any patient that did not have a positive response to CT-guided injection. We have not performed the procedure on any patient who had significant displacement of the sacroiliac joint post trauma, and we believe that this may be technically very difficult as the screw diameter and length (sizes available: width 8, 10 and 12 mm, length 50, 54 and 58 mm) may not be feasible in small offset sacral ala safe corridor. Another technical note that did arise was in the treatment of patients with rheumatoid arthritis. In these cases, the bone was found to be very soft and extra caution is recommended when introducing any instrument.
Analysis
The SF-36, visual analogue score and Majeed scoring questionnaires were analysed using Predictive Analytic Software 18 (PASW 18, SPSS Inc., Chicago, IL). Dependent non-parametric variables were compared using Wilcoxon’s signed-ranks test and independent non-parametric variables were tested using the Mann–Whitney test. A p value <0.05 was considered significant.
Results
A total of 55 patients were included in this study. The average follow-up period was 36.18 months (range 12–84 months). There were significantly more women, with 46 females and 9 males being included. The age of the patients ranged from 30 to 86 years, with a mean of 56.95 years. All causes of sacroiliac joint pathology were included in this study (including post-pregnancy dysfunction, sacroiliac osteoarthritis, chronic trauma and inflammatory arthropathy). A separate subgroup of patients was identified, accounting for 40 % (n = 22) of the overall patient group; these were the patients who had undergone previous instrumented spinal surgery (Fig. 1).
Fig. 1.

An anteroposterior radiograph illustrating the metal work of previous instrumented spinal surgery prior to a right sacroiliac joint fusion. This radiograph was taken 6 months post percutaneous sacroiliac joint fusion
For all patients, the mean preoperative SF-36 scores were 26.59 for physical health and 40.38 for mental health. The mean postoperative SF-36 scores were 42.93 for physical health and 52.77 for mental health. The mean visual analogue pain scores were 8.1 preoperative and 4.5 postoperative. The mean pelvic specific scores were 36.9 preoperative and 64.78 postoperative. Using the non-parametric Wilcoxon’s signed-ranks test for dependent variables, the significance (2-tailed) for comparison of SF-36, visual analogue pain and Majeed scores were all statistically significant with p values <0.001. This information is displayed in Table 1.
Table 1.
A summary of the overall scores
| Mean | SD | Wilcoxon signed-ranks test | |
|---|---|---|---|
| SF-36 | |||
| PCS preoperative | 26.59 | 15.23 | 0.000 |
| PCS postoperative | 42.93 | 22.68 | |
| MCS preoperative | 40.38 | 19.71 | 0.000 |
| MCS postoperative | 52.77 | 23.56 | |
| VAS (1–10) | |||
| Pain preoperative | 8.05 | 1.90 | 0.000 |
| Pain postoperative | 4.48 | 2.81 | |
| Majeed (0–100) | |||
| Preoperative | 36.18 | 15.08 | 0.000 |
| Postoperative | 64.78 | 20.18 | |
SF-36 short form-36, VAS visual analogue score, PCS physical health, MCS mental health
Looking more critically into this data, the subgroup of patients who had undergone previous instrumented spinal surgery had significantly worse outcomes than those who had not. The patients who had had previous instrumented spinal surgery made statistically significant improvements in their SF-36, visual analogue pain and Majeed scores, but these improvements were unlikely to be clinically significant (Table 2). In separating this data from the overall group, we find the patients who had not undergone previous spinal surgery showed much greater improvements in their postoperative scores. The mean difference between pre and postoperative SF-36 scores, visual analogue pain scores and Majeed scores are illustrated in Table 2, showing the significant difference between the aetiology of joint degeneration and instrumented spinal surgery.
Table 2.
Differences between those who have previously spinal surgery and those who have not
| Difference in means between pre and postoperative | SD | Mann–Whitney | |
|---|---|---|---|
| SF-36 | |||
| PCS-no spinal | 21.91 | 22.36 | 0.007 |
| PCS-spinal | 7.98 | 11.10 | |
| MCS-no spinal | 17.69 | 25.34 | 0.027 |
| MCS-spinal | 4.46 | 10.41 | |
| VAS (1–10) | |||
| Pain-no spinal | −4.85 | 2.89 | 0.001 |
| Pain-spinal | −1.76 | 2.24 | |
| Majeed (0–100) | |||
| No spinal | 32.76 | 16.16 | 0.021 |
| Spinal | 22.36 | 17.76 | |
SF-36 short form-36, VAS visual analogue score, PCS physical health, MCS mental health, No spinal no previous spinal surgery, Spinal previous spinal surgery
Breaking down the data into the number of patients who got worse, remained the same or improved post procedure found that for the sacroiliac joint degeneration group had 2 patients who worsened in the physical health section of the SF-36 questionnaire, 4 which remained the same and 27 which improved. Again for the sacroiliac joint degeneration group, in the mental health section of the SF-36, 6 worsened, 1 remained the same and 26 improved. For the same group of patients, none worsened in the visual analogue pain score, 2 remained the same and 31 improved. Similar values were seen in the Majeed scoring, with 1 that worsened, 0 remained the same and 32 improved. The post spinal surgery group faired significantly worse. In this group, 5 patients worsened in the physical health section of the SF-36 questionnaire, 5 remained the same and 12 improved. In the mental health section of the SF-36, 5 worsened, 4 remained the same and 13 improved. For this group of patients, 1 patient worsened in the visual analogue pain score, 7 remained the same and 14 improved. In regards to the Majeed scoring, there were 2 that worsened, 3 remained the same and 17 improved.
In the overall patient group, intraoperative blood loss was negligible. We had two complications of nerve pain immediately postoperatively, requiring return to theatre. There were no cases of wound infection, superficial or deep, bleeding or vascular injury, deep vein thrombosis, pulmonary embolism or late failure.
Discussion
We have found percutaneous iliosacral screw fixation, a very successful procedure in improving both pain and function in patients with sacroiliac joint disease. In the immediate postoperative period, patients describe their pelvis as feeling “more stable” and describe their sitting position to be greatly improved and dramatically less painful. For this reason, we have seen much larger improvements in the pelvic specific scoring questionnaires as compared to the general SF-36 forms. Patients with sacroiliac joint disease present with considerable pain and morbidity, with preoperative SF-36 scores falling way below that for both knee and hip arthritis in patients requiring arthroplasty surgery [13, 14]. Pain scores reported are also considerably worse than in patients with knee and hip arthritis [14]. The improvements in SF-36 forms and visual analogue pain scores following surgery fair well in comparison with hip and knee arthroplasty. In our initial technical report [4], the improvements in SF-36 and Majeed scoring are similar to what we have found in this study excluding the spinal surgery patients, which gives us encouragement that at the benefits seen at 12 months is continuing at an average of 36 months. Only a small number of patients worsened or remained the same in all the scoring systems used in this study. The majority of patients improved following the procedure even those in the post spinal surgery group, illustrating the benefits of this procedure.
The majority of the patients in this study were women (9 male, 46 female). This is a product of the increase in preponderance in women of rheumatoid arthritis [15], sacroiliac joint pain [12, 16] and the number of postpartum patients seen. This is representative of our experience of clinic attendances since we have provided a pelvic pain service. There were 5 postpartum patients treated in this study, of which 3 responded to follow-up questionnaires and was thus included in the final 55 patients. In general, the patients we treat postpartum have symphysis pubis dysfunction. These patients do not get referred from obstetricians until at least 6 months postpartum as the patients symptoms will usually improve by this time. If the patients have ongoing symphyseal instability with positive flamingo views then symphyseal stabilisation is undertaken. In this study, the patients encountered postpartum were chronic symphysis pubis dysfunction where the anterior ring instability had led to posterior ring degeneration. There was a minimum period of 4 years postpartum to sacroiliac joint investigation in all the postpartum patients seen in this study.
The two complications reported in this series were nerve injuries. Case 1 involved a 54-year-old female who underwent a right sacroiliac joint fusion for sacroiliac joint osteoarthritis. The patient complained of severe radicular symptoms involving the S1 dermatome immediately postoperative, without any abnormality of motor power. The patient was investigated using both CT and MRI, revealing encroachment on the S1 foramen without direct nerve impingement. The offending screw was repositioned resulting in resolution of pain within 6 weeks. This patient has been very pleased with her subsequent outcome. Case 2 involves a 30-year-old female who suffered greatly with chronic pelvic instability post-pregnancy of 5 years duration. She had undergone anterior symphysis pubis stabilisation 6 months previously; nevertheless, she continued to complain of pain in both her sacroiliac joints. Following positive response from CT-guided injections, both sacroiliac joints were stabilised at the same time, the right side being successful; however, the left resulted in severe radicular symptoms with no motor dysfunction of the L5 nerve root. CT and MRI revealed that some of the threads of the anchorage screw had breached the sacral ala and lay anterior to the sacrum, in close proximity to the nerve root, with cortical fragmentation around the nerve but no impingement; this is illustrated in Fig. 2. The patient underwent L5 nerve root block, which was successful in pain relief for 12 months. The pain, however, returned and it was felt that removal of the screw was required. An attempt at removing the screw was made 14 months post index operation, however, fusion had occurred and the screw was incorporated within this bone. This patient is to undergo L5 nerve displacement and neurolysis, as described by Weil et al. [17]. Nerve injury is an expected risk with such a small safe corridor [17, 18] and preoperative CT was utilised to reduce this risk. The second complication has emphasised the need to alter the position of the metal work early as if temporised you are unlikely to be able to remove the anchorage screw after 6 months. Superior gluteal artery injury has been reported in the literature in using percutaneous iliosacral screw fixation, although we did not experience any issues of this nature [19]. In comparison to open sacroiliac joint fusion, the complication profile is acceptable [20].
Fig. 2.
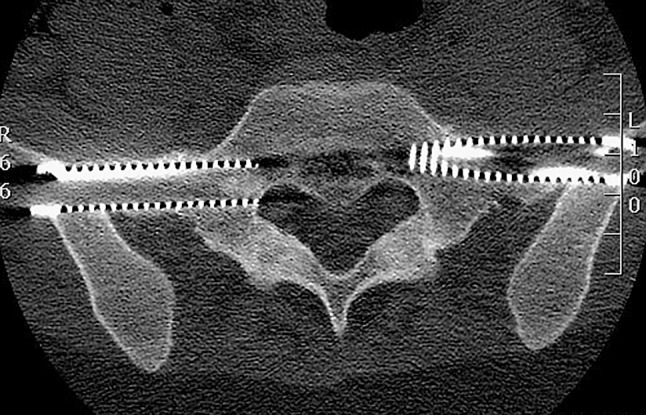
An axial view CT through the S1 sacral ala 6 months post bilateral percutaneous sacroiliac joint fusion. On the right side, the screw placement is ideal and shows a channel of bone transverse through the metal cage across the joint. The left anchorage screw breaches the sacral ala and lies in close proximity to the L5 nerve root
The prevalence of sacroiliac joint involvement in post fusion low back pain ranges from 29 to 40 % [21, 22]. This is likely to be due to transfer of motion from the fused segment to the next mobile intact segment, which in the case of lumbar-sacral fusion would be the sacroiliac joint. Studies by both Gates [23] and Onsel showed increased activity in the sacroiliac joint by single photon emission computed tomography and bone scintigraphy in patients following lumbar laminectomy and fusion. In addition, Ivanov [24] illustrated in a finite element study that lumbar fusion lead to increased angular motion at the sacroiliac joint. Thus, it is not surprising that 40 % of our patient group had previously undergone prior instrumented lumbar surgery. These patients, however, faired significantly worse than those who had not had prior lumbar surgery in this study. This was despite a successful preoperative CT-guided intra-articular sacroiliac joint injection. Postoperatively, these patients continued to describe significant pain, although some described the pain to have changed in nature. There are a few possible reasons for this. First, a proportion of these patients may have developed epidural fibrosis during their index operation, which will continue as a source of radicular pain [25]. In addition, some studies have indicated that 86 % of continued pain following lumbar surgery is myofascial in origin [26]. Lastly, chronic pain could be related to failed back surgery, which would not be affected by sacroiliac joint fusion [27]. Such patients may have a positive response to CT-guided injections as there are reports that even these targeted injections may cause a local perineural block [28]. We hypothesise that the multifactorial origins of pain in these patients result in an inferior outcome.
Many of the patients in the lumbar surgery group were investigated for sacroiliac joint pain after suffering persisting pain following their lumbar back surgery. It is unclear whether their response to a CT-guided sacroiliac joint injection was due to the anaesthetic block of a degenerate sacroiliac joint or due to perineural/localised infiltration of anaesthetic as these injections have an unknown specificity [28]. Although beyond the scope of this study, it would be interesting to see whether these patients had developed sacroiliac joint pain after a lumbar fusion or whether the sacroiliac joint was a source of pain prior to their lumbar surgery. Our study does show, however, that these patients on average show a statistically significant improvement, but not clinically significant improvement following sacroiliac joint stabilisation.
Symptomatic non-union following sacroiliac joint fusion has been reported to be as high as 60 % (9 out of 15) at a mean follow-up of 39 months [29]. We could not justify the irradiation and financial cost of performing postoperative CT scans on our patients, thus we cannot guarantee union. With a mean follow-up of 36 months, we saw no lucency around any screw and progressive sclerosis within the joints on sequential plain radiographs as illustrated in Fig. 3. Some patients did undergo CT pelvic scans for other reasons (most commonly assessment of the contralateral SI joint), all of which showed a column of bone bridging the cartilaginous component of the sacroiliac joint. We had no incidence of metalwork failure. Patients felt their pelvis to be stable immediately postoperative, and we had no incidence where any patient felt this stability was lost.
Fig. 3.

Anteroposterior radiograph 7 years post bilateral sacroiliac joint fusion illustrating sclerosis of both sacroiliac joints with no loosening of hardware. This patient remains very satisfied
In this investigation, we endeavoured to reduce bias, however, some limitations remained. This study is a prospective single surgeon outcome study. All patients who underwent elective sacroiliac joint fusion were included for analysis, removing any inclusion selection bias; however, we had a 24.7 % (n = 18) loss to follow-up despite our best efforts of attempting contact. To reduce reviewer bias, an independent researcher collected the follow-up data. Another limitation to this study was the use of follow-up questionnaires only on their last follow-up, without a predetermined time for follow-up analysis, thus we cannot comment if there was any change in patients’ results overtime.
Conclusion
Percutaneous iliosacral screw fixation, is a very successful procedure in improving both the pain and function in patients with sacroiliac joint disease and is a reliable procedure to provide an immediate structural fixation and with good mid-term results post procedure.
Conflict of interest
None.
References
- 1.Wise CL, Dall BE. Minimally invasive sacroiliac arthrodesis: outcomes of a new technique. J Spinal Disord Tech. 2008;21(8):579–584. doi: 10.1097/BSD.0b013e31815ecc4b. [DOI] [PubMed] [Google Scholar]
- 2.Smith-Peterson MN. Arthrodesis of the sacroiliac joint. A new method of approach. J Orthop Surg. 1921;3:400–405. [Google Scholar]
- 3.Shuler TE, Boone DC, Gruen GS, Peitzman AB. Percutaneous iliosacral screw fixation: early treatment for unstable posterior pelvic ring disruptions. J Trauma. 1995;38(3):453–458. doi: 10.1097/00005373-199503000-00031. [DOI] [PubMed] [Google Scholar]
- 4.Khurana A, Guha AR, Mohanty K, Ahuja S. Percutaneous fusion of the sacroiliac joint with hollow modular anchorage screws: clinical and radiological outcome. J Bone Joint Surg Br. 2009;91(5):627–631. doi: 10.1302/0301-620X.91B5.21519. [DOI] [PubMed] [Google Scholar]
- 5.Al-Khayer A, Hegarty J, Hahn D, Grevitt MP. Percutaneous sacroiliac joint arthrodesis: a novel technique. J Spinal Disord Tech. 2008;21(5):359–363. doi: 10.1097/BSD.0b013e318145ab96. [DOI] [PubMed] [Google Scholar]
- 6.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483. doi: 10.1097/00005650-199206000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Majeed SA. Grading the outcome of pelvic fractures. J Bone Joint Surg Br. 1989;71(2):304–306. doi: 10.1302/0301-620X.71B2.2925751. [DOI] [PubMed] [Google Scholar]
- 8.Hansen HC, McKenzie-Brown AM, Cohen SP, Swicegood JR, Colson JD, Manchikanti L. Sacroiliac joint interventions: a systematic review. Pain Physician. 2007;10(1):165–184. [PubMed] [Google Scholar]
- 9.Albert H, Godskesen M, Westergaard J. Evaluation of clinical tests used in classification procedures in pregnancy-related pelvic joint pain. Eur Spine J. 2000;9(2):161–166. doi: 10.1007/s005860050228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gaenslen FJ. Sacroiliac arthrodesis: indications, author’s technique and end-results. J Am Med Assoc. 1927;89:2031–2035. doi: 10.1001/jama.1927.02690240023008. [DOI] [Google Scholar]
- 11.Robinson HS, Brox JI, Robinson R, Bjelland E, Solem S, Telje T. The reliability of selected motion- and pain provocation tests for the sacroiliac joint. Man Ther. 2007;12(1):72–79. doi: 10.1016/j.math.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 12.Simopoulos TT, Manchikanti L, Singh V, Gupta S, Hameed H, Diwan S, Cohen SP. A systematic evaluation of prevalence and diagnostic accuracy of sacroiliac joint interventions. Pain Physician. 2012;15(3):E305–E344. [PubMed] [Google Scholar]
- 13.Johansson HR, Bergschmidt P, Skripitz R, Finze S, Bader R, Mittelmeier W. Impact of preoperative function on early postoperative outcome after total hip arthroplasty. J Orthop Surg (Hong Kong) 2010;18(1):6–10. doi: 10.1177/230949901001800102. [DOI] [PubMed] [Google Scholar]
- 14.Baumann C, Rat AC, Osnowycz G, Mainard D, Cuny C, Guillemin F. Satisfaction with care after total hip or knee replacement predicts self-perceived health status after surgery. BMC Musculoskelet Disord. 2009;10:150. doi: 10.1186/1471-2474-10-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brennan P, Silman A. Why the gender difference in susceptibility to rheumatoid arthritis? Ann Rheum Dis. 1995;54(9):694–695. doi: 10.1136/ard.54.9.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.DePalma MJ, Ketchum JM, Saullo TR. Multivariable analyses of the relationships between age, gender, and body mass index and the source of chronic low back pain. Pain Med. 2012;13(4):498–506. doi: 10.1111/j.1526-4637.2012.01339.x. [DOI] [PubMed] [Google Scholar]
- 17.Weil YA, Nousiainen MT, Helfet DL. Removal of an iliosacral screw entrapping the L5 nerve root after failed posterior pelvic ring fixation: a case report. J Orthop Trauma. 2007;21(6):414–417. doi: 10.1097/BOT.0b013e3180cab6b5. [DOI] [PubMed] [Google Scholar]
- 18.Tonetti J, Cazal C, Eid A, Badulescu A, Martinez T, Vouaillat H, Merloz P. Neurological damage in pelvic injuries: a continuous prospective series of 50 pelvic injuries treated with an iliosacral lag screw. Rev Chir Orthop Reparatrice Appar Mot. 2004;90(2):122–131. doi: 10.1016/S0035-1040(04)70033-1. [DOI] [PubMed] [Google Scholar]
- 19.Marmor M, Lynch T, Matityahu A. Superior gluteal artery injury during iliosacral screw placement due to aberrant anatomy. Orthopedics. 2010;33(2):117–120. doi: 10.3928/01477447-20100104-26. [DOI] [PubMed] [Google Scholar]
- 20.Buchowski JM, Kebaish KM, Sinkov V, Cohen DB, Sieber AN, Kostuik JP. Functional and radiographic outcome of sacroiliac arthrodesis for the disorders of the sacroiliac joint. Spine J. 2005;5(5):520–528. doi: 10.1016/j.spinee.2005.02.022. [DOI] [PubMed] [Google Scholar]
- 21.Katz V, Schofferman J, Reynolds J. The sacroiliac joint: a potential cause of pain after lumbar fusion to the sacrum. J Spinal Disord Tech. 2003;16(1):96–99. doi: 10.1097/00024720-200302000-00015. [DOI] [PubMed] [Google Scholar]
- 22.Maigne JY, Planchon CA. Sacroiliac joint pain after lumbar fusion. A study with anesthetic blocks. Eur Spine J. 2005;14(7):654–658. doi: 10.1007/s00586-004-0692-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gates GF, McDonald RJ. Bone SPECT of the back after lumbar surgery. Clin Nucl Med. 1999;24(6):395–403. doi: 10.1097/00003072-199906000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Ivanov AA, Kiapour A, Ebraheim NA, Goel V. Lumbar fusion leads to increases in angular motion and stress across sacroiliac joint: a finite element study. Spine. 2009;34(5):E162–E169. doi: 10.1097/BRS.0b013e3181978ea3. [DOI] [PubMed] [Google Scholar]
- 25.Cinotti G, Roysam GS, Eisenstein SM, Postacchini F. Ipsilateral recurrent lumbar disc herniation. A prospective, controlled study. J Bone Joint Surg Br. 1998;80(5):825–832. doi: 10.1302/0301-620X.80B5.8540. [DOI] [PubMed] [Google Scholar]
- 26.Teixeira MJ, Yeng LT, Garcia OG, Fonoff ET, Paiva WS, Araujo JO. Failed back surgery pain syndrome: therapeutic approach descriptive study in 56 patients. Rev Assoc Med Bras. 2011;57(3):282–287. doi: 10.1016/S0104-4230(11)70060-4. [DOI] [PubMed] [Google Scholar]
- 27.Bokov A, Isrelov A, Skorodumov A, Aleynik A, Simonov A, Mlyavykh S. An analysis of reasons for failed back surgery syndrome and partial results after different types of surgical lumbar nerve root decompression. Pain Physician. 2011;14(6):545–557. [PubMed] [Google Scholar]
- 28.Saal JS. General principles of diagnostic testing as related to painful lumbar spine disorders: a critical appraisal of current diagnostic techniques. Spine. 2002;27(22):2538–2545. doi: 10.1097/00007632-200211150-00027. [DOI] [PubMed] [Google Scholar]
- 29.Schutz U, Grob D. Poor outcome following bilateral sacroiliac joint fusion for degenerative sacroiliac joint syndrome. Acta Orthop Belg. 2006;72(3):296–308. [PubMed] [Google Scholar]


