Abstract
Purpose
The AO Spine Classification Group was established to propose a revised AO spine injury classification system. This paper provides details on the rationale, methodology, and results of the initial stage of the revision process for injuries of the thoracic and lumbar (TL) spine.
Methods
In a structured, iterative process involving five experienced spine trauma surgeons from various parts of the world, consecutive cases with TL injuries were classified independently by members of the classification group, and analyzed for classification reliability using the Kappa coefficient (κ) and for accuracy using latent class analysis. The reasons for disagreements were examined systematically during review meetings. In four successive sessions, the system was revised until consensus and sufficient reproducibility were achieved.
Results
The TL spine injury system is based on three main injury categories adapted from the original Magerl AO concept: A (compression), B (tension band), and C (displacement) type injuries. Type-A injuries include four subtypes (wedge-impaction/split-pincer/incomplete burst/complete burst); B-type injuries are divided between purely osseous and osseo-ligamentous disruptions; and C-type injuries are further categorized into three subtypes (hyperextension/translation/separation). There is no subgroup division. The reliability of injury types (A, B, C) was good (κ = 0.77). The surgeons’ pairwise Kappa ranged from 0.69 to 0.90. Kappa coefficients κ for reliability of injury subtypes ranged from 0.26 to 0.78.
Conclusions
The proposed TL spine injury system is based on clinically relevant parameters. Final evaluation data showed reasonable reliability and accuracy. Further validation of the proposed revised AO Classification requires follow-up evaluation sessions and documentation by more surgeons from different countries and backgrounds and is subject to modification based on clinical parameters during subsequent phases.
Keywords: Spinal injury classification, Thoracolumbar, Consensus development, Reliability, Accuracy
Introduction
For more than half a century, a contribution to the understanding of thoracic and lumbar (TL) spinal fractures has been made by outlining the importance of the mechanism of injury [1], developing different mechanistic concepts (2- [2] and 3-column concepts [3]), and Magerl’s definition of three basic, progressive, pathomorphological criteria: (A) compression, (B) distraction, and (C) axial torque. The latter classification is comprehensive and built on a hierarchical system, however, it has been criticized for its detail [4]. In addition, its present form has neither been systematically validated nor revised to improve on its reliability, accuracy (validity), and clinical applicability [5, 6].
The AO Spine Classification Group (AOSCG) was established with the aim to propose a uniform spine injury classification system, using the current Magerl AO system as a starting point, with the goal of addressing traumatic spinal injuries of the entire spinal column in a manner that would be useful for clinical practice and research [7, 8]. This paper presents the first validation phase of the proposed classification system for thoracolumbar (TL) spinal injuries, as a revision of the original Magerl AO classification system. Its clinical application is illustrated using case examples to outline its characteristics and radiographic morphological appearance.
Materials and methods
This revision process conformed to the guidelines of the first of three validation phases as outlined by Audigé et al. [8]. The first validation phase consists of an iterative consensus development and scientific evaluation process. The second phase could allow for adaptations based on clinical modifiers, but with a subsequent primary goal of being evaluated within a multicenter agreement study, to ensure that future users with varying expertise can understand and agree on the proposed classification system. The third phase, involving prospective clinical documentation, can then be implemented to support future recommendations for patient care based on the classification. We present the revised thoracolumbar AO spine injury classification, which has already reached completion of this phase 1 development process. Specific classification systems for the other spine regions are being developed in the same way for upper cervical spine (C0–C2), subaxial cervical spine (C3–C7), and sacral spine (S1–S5 including coccyx).
Based on the CG discussions and the available literature, we have decided that it should be possible to define the general characteristics of injury patterns as modes of mechanical failures of the spinal column, which can be used for all four anatomic regions with specific adaptations. Three major modes of failure of spinal column integrity were identified by ascending severity:
Type-A injuries: failure under axial compression of the anterior elements with intact posterior constraining elements
Type-B injuries: failure of the posterior constraining elements
Type-C injuries: failure of anterior and posterior elements leading to displacement
There are here two important differences with the Magerl AO system. First of all, type-B injuries are not defined as ‘elongation’ injuries but as injuries to posterior constraints. This is meant to reduce the confusion between A- and B-type injuries and is more easily applicable to injuries outside the TL region. Second is the redefinition of the type C as ‘discernible displacement’. Definition of type C as ‘rotational injuries’ in the original Magerl AO classification caused uncertainties in some compression fractures with slight rotational deformities of the TL spine. Furthermore, with this redefinition, it is more easily applicable to regions outside the TL spine.
Separate detailed classification systems for each spine region will be presented in subsequent papers, along with typical and difficult case examples as well as an in-depth discussion on the rationale for inclusion of specific diagnostic items in the system.
Under the guidance of a coordinating methodologist, five experienced spine trauma surgeons from three continents followed a structured consensus process by which successive revisions of the Magerl AO System were evaluated during sessions in which the surgeons independently classified consecutive cases of spine injuries according to a previously agreed upon draft system. Agreement data were analyzed for reliability using the Kappa coefficient and for accuracy using latent class analysis. The reasons for disagreements were examined systematically during review meetings. At each iterative step, the system was revised until a consensus was reached. The data were analyzed to assess the classification’s reliability and accuracy as well as to identify disagreement issues, which needed to be addressed. This process was completed when surgeons reached unanimous consensus on the proposed system and was supported by the evaluation results.
Five face-to-face meetings and four evaluation sessions were necessary to achieve consensus in the TL system. The results of the final session are presented here. The case series included 110 cases representing a random selection of 60 % of the whole case collection of TL injuries as well as all additional cases diagnosed with either a B or C injury in the first two sessions (19 cases). This last session was conducted using the final draft, incorporating the changes made at previous sessions, and surgeons were blinded to previous fracture codes.
The analyses were conducted by first considering only the injury type (A, B, C). Because several injuries could be coded in any of the cases, data were collapsed at the patient level and each case was classified as having “only A-type injuries”, “a B-type (with or without A-type) injury but without C-type injury”, or “with a C-type injury”. The coding of injury subtypes was implemented separately for each type A, B, and C as identified by latent class modeling, a useful technique in the absence of any reference-standard classification. For type-A injuries, only cases with single vertebral body (VB) fractures (disregarding the B and C coding) were included to ensure that the surgeons were assessing the same injury. A similar approach was used for type-B and type-C injuries by including only cases with single injuries and disregarding any type-A injury codes.
Results
Classification of thoracolumbar spinal injuries
The three basic types of Magerl AO were rephrased and adapted for the purposes of clarity and better reproducibility. They were defined as ‘major modes of failure of the spinal TL column integrity’ and listed in ascending severity as:
Type-A injuries: failure under axial compression of the anterior elements with intact posterior constraining elements
Type-B injuries: failure of the posterior constraining elements (tension band or PLC injuries in case of TL spine)
Type-C injuries: failure of anterior and posterior elements leading to displacement
Type-A injuries can either be isolated fractures (e.g., L2) or occur in combination with failure of the posterior tension band (type-B injuries), and/or displacement (type-C) injuries. B- and C-type injuries usually involve a motion segment and are coded accordingly (e.g., T12/L1). Multilevel injuries should be classified separately and listed according to severity. In this classification, isolated spinous or transverse process injuries without implication on spinal mechanical stability are not included.
Type-A injuries: compression injuries of anterior elements
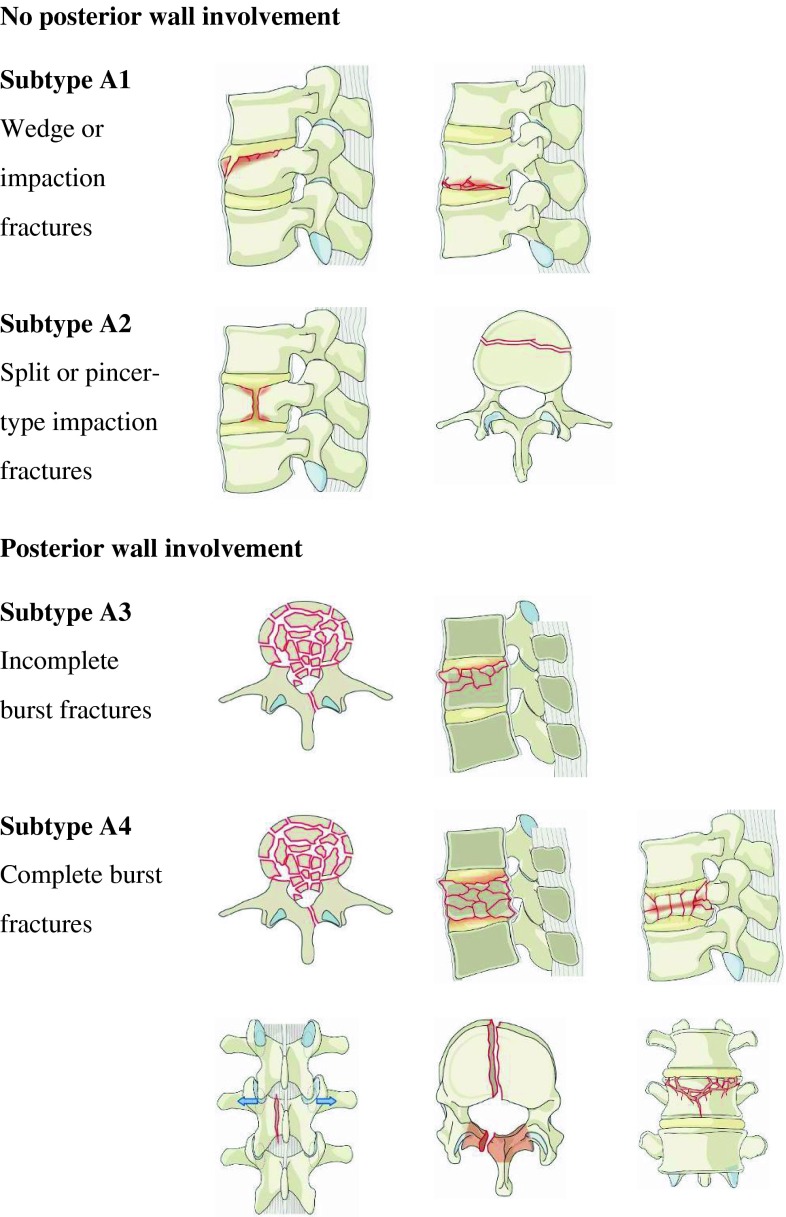
Type A denotes failure of the anterior elements (vertebral body disc) under compression. Posterior constraining elements (in the case of TL injuries these are facet joints and posterior osseo-ligamentous structures) remain intact. In TL spine, type-A injuries are thus represented by compression injuries with vertebral body fracture with neither disruption of posterior constraining elements nor any signs of displacement or dislocation. They are further divided into four subtypes (Fig. 1). There are no further subgroupings as no evidence has been found that the subgroups in the Magerl AO scheme had any clinical relevance. There was sufficient evidence and consensus within the CG on the relevance of the subgroups of A3 fractures (A 3.1 vs. A 3.2 and A 3.3), which were subsequently clustered into two separate subtypes (A3 and A4).
Fig. 1.
Type-A compression injuries of the vertebral body
Subtype A1 injuries are wedge or impaction fractures that are characterized by a fracture of a single endplate without involvement of the posterior wall of the vertebral body.
Comment Cancellous bone near the upper or lower endplate is compressed and will result in a wedge-shaped VB, associated with loss of height of the anterior wall. The posterior wall of the VB remains intact, indicating that there is no violation of the spinal canal. Compression fractures can be located at the cranial or caudal endplates and may have asymmetrical aspects leading to the appearance of a lateral wedge.
Subtype A2 injuries are split or pincer-type fractures that are characterized by a fracture of both end plates without involvement of the posterior wall of the VB.
Comment They include split fracture of the VB in any plane involving both endplates but with an intact posterior wall.
Subtype A3 injuries are VB fractures affecting a single endplate, associated with the involvement of the posterior wall. They are commonly called ‘burst fractures’. As a result of the increase in the interpedicular distance, sagittal fractures of the lamina can occur. These correspond to the A 3.1 category of the Magerl AO system.
Comment Bony injury will be associated with varying degrees of fracture fragmentation. Partial comminution of the VB will usually be associated with some height loss. In addition, posterior wall involvement with retropulsed bone elements can cause spinal canal encroachment with subsequent neurological deficits. The PLC and the facet joints remain intact despite possible vertical fractures through the lamina. This vertical lamina fracture is a distinct feature commonly associated with burst type injuries. It is important to differentiate this from type-B injuries with horizontal osseo-ligamentous disruption of the PLC or facet joints with consequent tension band failure.
Subtype A4 injuries represent VB fractures involving both endplates with the involvement of the posterior cortex. They are similar to A3 injuries, but both endplates are involved by either an associated split fracture or comminution of the whole VB. These correspond to the A 3.2 and A 3.3 categories of the Magerl AO system.
Comment This subcategory was created to distinguish between incomplete (A3) and complete (A4) burst fractures because of the higher magnitude of bony destruction in complete burst fractures and its mechanical and clinical consequences with the involvement of the entire VB, including greater degree of height loss and possibly of spinal canal encroachment. The importance of A3–A4 distinction has been shown by the load-sharing classification. The incidence of neurological injury is the highest of all A subtypes.
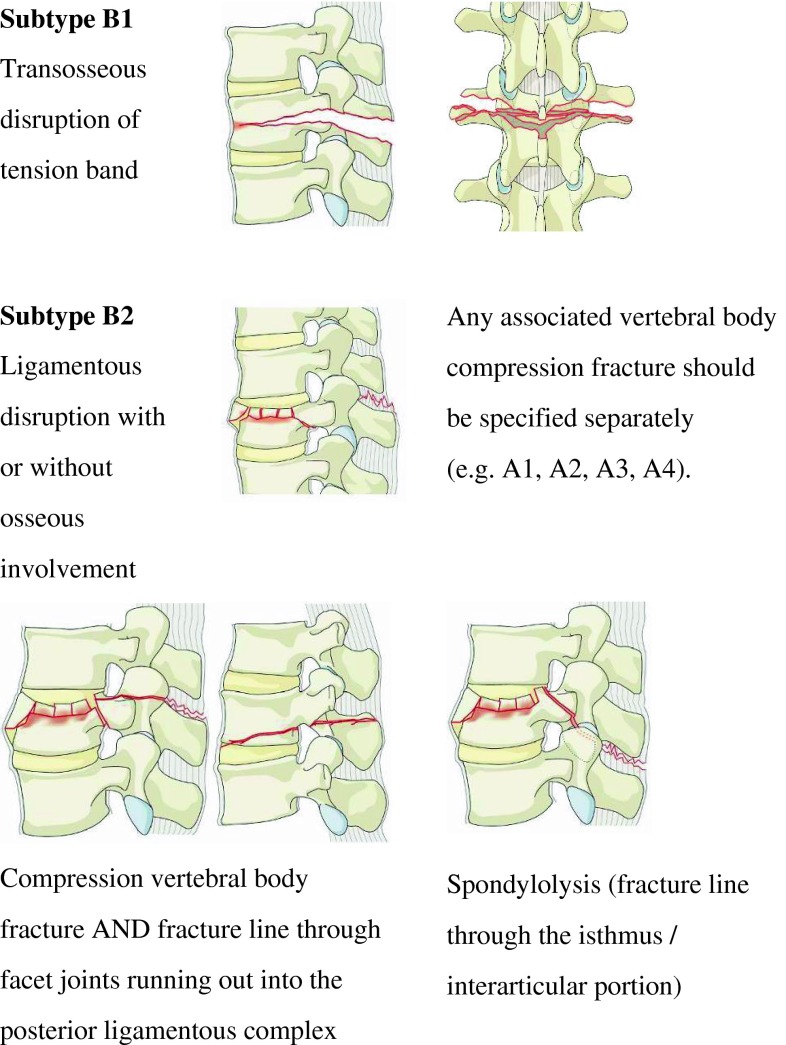
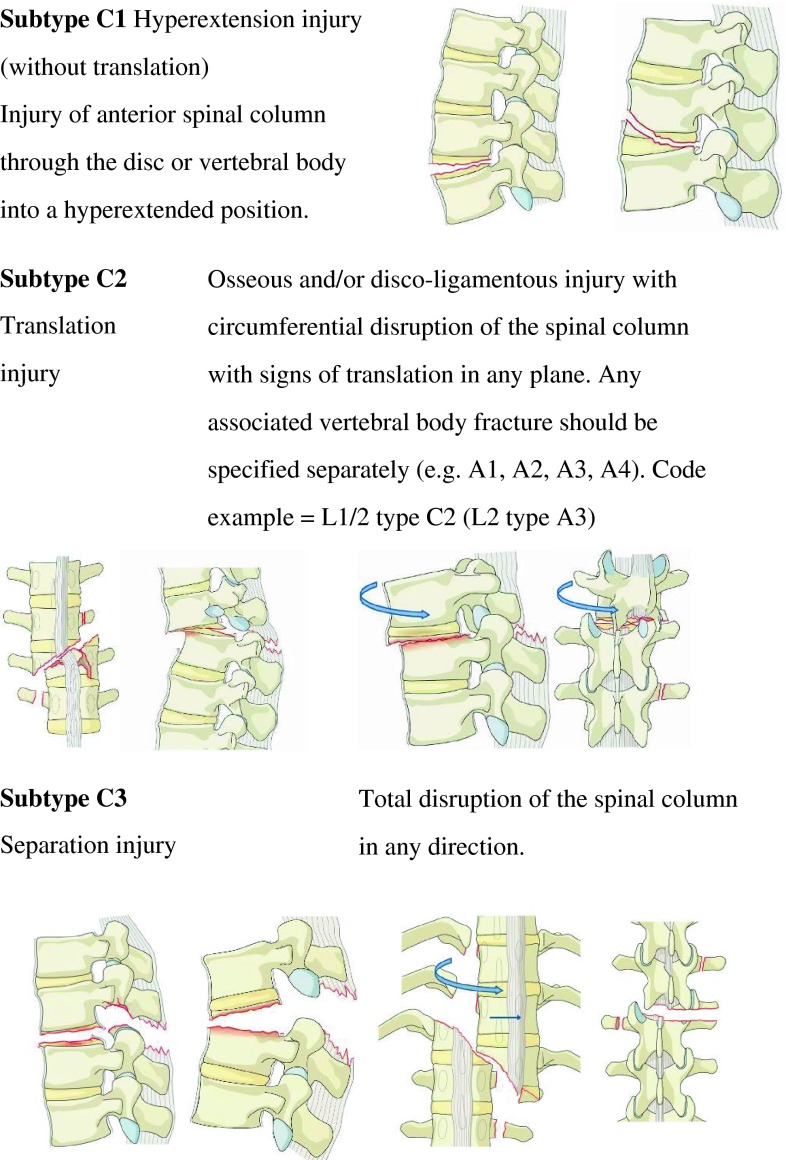
Type-B injuries: tension band injury
Type B denotes failure of the posterior constraining elements. In the case of TL spine, these constraints are facet joints and posterior ligamentous structures resisting the kyphosing forces. Thus, they are also called ‘tension band’ or PLC (posterior ligamentous complex) injuries in the TL spine. They are frequently seen in combination with type-A fractures of the VB. They are further divided in two subtypes (Fig. 2).
Fig. 2.
Type-B tension band injuries
Subtype B1 injuries are mono-segmental trans-osseous tension band failures.
Comment These are the classic ‘Chance’ fractures. There is no substantial VB compression fracture. These injuries are unique due to the presence of a horizontal fracture that extends across the vertebral body and the pedicles.
Subtype B2 injuries are all other types of disruption of the posterior tension band with or without posterior osseous involvement. Any associated VB fracture should be specified separately according to the type-A subdivision (i.e. A1, A2, A3, A4) as illustrated in Fig. 3.
Fig. 3.
Type-C displacement injuries
Comment Usually a flexion-distraction mechanism will result in an associated VB compression injury that should be classified separately. Fracture lines can be seen through posterior bony elements, e.g., facet joints, the interarticular portion of isthmus (spondylolytic injuries), or the spinous process extending to the interspinous ligaments. Facet fractures or subluxation with consequent kyphotic deformity of the involved motion segment(s) can also be seen. Without close attention to the clinical signs of ligamentous failure such as marked tenderness of posterior elements during physical examination, a palpable interspinous gap, pronounced gibbus, and consistent interpretation of the characteristic radiographic features of this injury type, one can easily miss or misinterpret B-type injuries for a type-A injury. In doubtful cases, MRI evaluation may be helpful.
Type-C injuries: displacement injury
Type-C injuries are characterized by the displacement of cranial relative to caudal parts of the spinal column in any plane (Fig. 4)
Fig. 4.
Diagnostic algorithm for the classification of TL injuries
Subtype C1 injuries affect the anterior spinal column through the disc or VB, resulting in a hyperextension deformity.
Comment Hyperextension will cause failure of the anterior spinal column, e.g., through the intervertebral disk or VB. Thus, the displacement is located anteriorly. The spine is in a hyperextended position but there is a posteriorly located hinge preventing complete dislocation (translational displacement). However, the fracture may run through the posterior elements, too. Hyperextension injuries, which were type B3 in the Magerl AO system, were introduced into the C-type category because these injury types are seen more frequently especially in ankylotic spine and are considered to be highly unstable. This also lends clarity to the definition of type-B injuries without the need for the ambiguous mechanistic concept of ‘elongation,’ which was part of the original Magerl AO system.
Subtype C2 injuries are osseous and/or disco-ligamentous injuries with circumferential disruption of the spinal column resulting in signs of translation in any plane (usually a combination of rotation and translation). Any associated VB fracture should be specified separately (e.g., A1, A2, A3, A4).
Comment A typical coding sample would be L1/L2–C2 (L2–A3) indicating that translation is located at the L1/L2 level with an associated incomplete burst fracture of L2. This injury can be associated with additional signs of rotation such as a unilateral facet fracture or subluxation.
Subtype C3 injuries result in a complete separation of the cranial and caudal parts of the spinal column.
Comment These injuries are highly unstable because of the complete separation of both the anterior and posterior osseo-ligamentous elements. Due to the total disruption of the spinal column and complete separation between proximal and distal parts, the configuration of the spinal column may appear different in diagnostic images taken at different times. Usually a high-energy trauma is the underlying mechanism of these injuries, which can be associated with life-threatening vascular complications in addition to neurological damage.
Final evaluation session
Based on the surgeons’ classification, the proportion of injuries in the random sample series involving a single vertebra ranged from 76 to 82 %. Between 15 and 17 % of the cases were reported to have at least one type-B injury. The proportion of cases with a type-C injury ranged from 6 to 7 %.
Full agreement with regard to fracture type was achieved among the five surgeons in 91 (83 %) of the cases; the overall Kappa coefficient was 0.77 (Table 1). For classifying a “type-A only” injury, the category-specific Kappa was 0.81. The surgeons’ pairwise Kappa ranged from 0.69 to 0.90 (n = 10; median 0.76). Classification accuracies for type A, B, and C injuries ranged from 93 to 99 % (median 96 %), 84 to 98 % (median 90 %), and 72 to 96 % (median 84 %), respectively (Table 2).
Table 1.
Distribution of injuries and Kappa coefficients of reliability for coding the injury type at the patient level
| Type | n (%)a | Kappa |
|---|---|---|
| Number of surgeons per case | 5 | |
| A Compression fracture(s) only | 87 (79 %) | 0.81 |
| B Tension band injury (without C-type) | 15 (14 %) | 0.71 |
| C Displacement injury | 8 (7 %) | 0.81 |
| All cases | 110 | 0.77 |
Because several injuries could be coded in any of the cases, data were collapsed at the patient level and each case was classified as having “only A-type injuries” (A), “a B-type injury (with or without A type) excluding a C-type injury” (B), or “with at least a C-type injury” (C)
aEstimation of case distribution by latent class analysis
Table 2.
Latent class analysis and surgeons’ accuracy in classifying injury types at the patient level (n = 110)
| Likely injury type | |||
|---|---|---|---|
| A | B | C | |
| Cluster 1 | Cluster 2 | Cluster 3 | |
| Cluster size (%) | 78.4 | 14.1 | 7.5 |
| Surgeon 1 | |||
| A Compression fracture(s) (%) | 95.5 | 8.5 | 3.2 |
| B Tension band injury (%) | 4.4 | 91.3 | 0.7 |
| C Displacement injury (%) | 0.0 | 0.2 | 96.2 |
| Surgeon 2 | |||
| A Compression fracture(s) (%) | 97.8 | 2.2 | 3.2 |
| B Tension band injury (%) | 1.0 | 97.7 | 24.6 |
| C Displacement injury (%) | 1.2 | 0.1 | 72.2 |
| Surgeon 3 | |||
| A Compression fracture(s) (%) | 95.4 | 15.8 | 3.2 |
| B Tension band injury (%) | 4.6 | 84.0 | 12.7 |
| C Displacement injury (%) | 0.0 | 0.1 | 84.2 |
| Surgeon 4 | |||
| A Compression fracture(s) (%) | 98.8 | 9.6 | 3.2 |
| B Tension band injury (%) | 1.2 | 90.3 | 12.6 |
| C Displacement injury (%) | 0.0 | 0.1 | 84.2 |
| Surgeon 5 | |||
| A Compression fracture(s) (%) | 93.0 | 16.2 | 3.0 |
| B Tension band injury (%) | 5.8 | 83.6 | 12.7 |
| C Displacement injury (%) | 1.2 | 0.2 | 84.3 |
| Classification accuracies | |||
| Median (%) | 95.5 | 90.3 | 84.2 |
| Range | 93.0–98.8 | 83.6–97.7 | 72.2–96.2 |
Surgeons classified a further 86 cases having only one type-A fracture as identified by latent class analysis. Among the five surgeons, full agreement concerning the fracture subtype of type-A compression fractures was reached in 60 (70 %) cases. The overall Kappa coefficient for this classification was 0.78 with an A4 category-specific Kappa coefficient of 0.85 (Table 3). The surgeons’ pairwise Kappa ranged from 0.69 to 0.89 (n = 10; median 0.77). Classification data for fracture subtyping were consistent with the occurrence of three clusters of cases after excluding the only A2 subtype fracture from the analysis (Table 4). Classification accuracies ranged from 85 to 96 % (median 90 %) for A1, 66 to 94 % (median 90 %) for A3, and 93 to 99 % (median 99 %) for A4 fracture subtypes.
Table 3.
Distribution of injuries and Kappa coefficients of reliability for coding injury subtypes for each TL injury type
| Type | Subtype | n a | Kappa |
|---|---|---|---|
| Number of raters | 2–5 | ||
| A Compression fractures | |||
| 1 Wedge/impaction | 31 (36 %) | 0.80 | |
| 2 Split/pincer type | 1 (1 %) | 0.44 | |
| 3 Incomplete burst | 24 (28 %) | 0.73 | |
| 4 Complete burst | 30 (35 %) | 0.85 | |
| Overall | 0.78 | ||
| B Tension band injuries | |||
| 1 Trans-osseous disruption | 1 (5 %) | ||
| 2 Ligamentous disruption | 21 (95 %) | ||
| Overall | 22 | 0.28 | |
| C Displacement injuries | |||
| 1 Hyperextension injury | 2 (15 %) | ||
| 2 Translation injury | 11 (85 %) | ||
| 3 Separation injury | 0 (0 %) | ||
| Overall | 13 | 0.62 | |
The sample of A-type fractures included all cases with a single compression fracture and with or without B- or C-type injury within the random sample of 110 cases. The sample of B- and C-type injuries included all such injuries identified within the complete TL case series
aEstimation of case distribution by the majority of surgeons
Table 4.
Latent class analysis and surgeons’ accuracy in classifying subtypes of A-type compression fractures (n = 86)
| Likely injury subtype | |||
|---|---|---|---|
| A1 | A3 | A4 | |
| Cluster 1 | Cluster 2 | Cluster 3 | |
| Cluster size (%) | 36.3 | 28.5 | 35.3 |
| Surgeon 1 | |||
| 1 Wedge/impaction (%) | 92.0 | 6.9 | 3.8 |
| 2 Split/pincer type (%) | 7.3 | 5.1 | 3.5 |
| 3 Incomplete burst (%) | 0.3 | 77.2 | 0.2 |
| 4 Complete burst (%) | 0.5 | 10.8 | 92.5 |
| Surgeon 2 | |||
| 1 Wedge/impaction (%) | 89.8 | 0.5 | 0.4 |
| 2 Split/pincer type (%) | 0.0 | 0.0 | 0.0 |
| 3 Incomplete burst (%) | 9.8 | 94.9 | 0.4 |
| 4 Complete burst (%) | 0.4 | 4.6 | 99.3 |
| Surgeon 3 | |||
| 1 Wedge/impaction (%) | 90.4 | 4.4 | 0.4 |
| 2 Split/pincer type (%) | 0.0 | 0.0 | 0.0 |
| 3 Incomplete burst (%) | 9.2 | 91.0 | 0.5 |
| 4 Complete burst (%) | 0.4 | 4.6 | 99.2 |
| Surgeon 4 | |||
| 1 Wedge/impaction (%) | 95.5 | 5.5 | 0.4 |
| 2 Split/pincer type (%) | 0.0 | 0.0 | 3.3 |
| 3 Incomplete burst (%) | 4.1 | 89.8 | 0.3 |
| 4 Complete burst (%) | 0.5 | 4.7 | 96.0 |
| Surgeon 5 | |||
| 1 Wedge/impaction (%) | 84.7 | 17.2 | 0.4 |
| 2 Split/pincer type (%) | 3.6 | 0.0 | 0.0 |
| 3 Incomplete burst (%) | 0.2 | 57.7 | 0.2 |
| 4 Complete burst (%) | 11.5 | 25.0 | 99.4 |
| Classification accuracies | |||
| Median (%) | 90.4 | 89.9 | 99.2 |
| Range | 84.7–95.6 | 57.7–94.9 | 92.5–99.4 |
Only one case was clearly identified as an A2 (split/pincer type) fracture by the surgeons. Hence, this analysis was implemented after excluding this case. The model was consistent with three fracture classes including A1, A3 and A4 fractures. Incorrect classification into the A2 category was, however, possible
In classifying 22 type-B displacement fractures according to the subtypes B1 (trans-osseous disruption) and B2 (ligamentous disruption), surgeons were in full agreement with 13 (59 %) cases. The overall Kappa coefficient was 0.28; only one certain B1 injury was likely to have been included in the sample (Table 3) making the evaluation if this distinction was unreliable. Surgeons were in full agreement for the classification of ten type-C injuries (77 %; n = 13), and the overall Kappa coefficient was 0.62. Only two cases were likely to be C1 (hyperextension) injuries, and there were no C3 (separation) injuries as determined by the majority of surgeons (Table 3). The surgeons’ pairwise Kappa coefficients ranged from 0.30 to 1.00. Sample sizes and case distributions did not allow the implementation of latent class analysis of injury subtypes for B- and C-type injuries.
Diagnostic and coding process
The revised classification system presented above focuses on the morphological characteristics of injuries within the TL spine. To be comprehensive, morphological characterization should include a combination of all identified injuries with their localization.
Location of injuries
All A-type compression injuries and the subtype B1 injuries (trans-osseous disruption of the posterior tension band) are located at the level of a single vertebra. Their location is thus designated by the involved vertebra traditionally designated with a letter (T or L) and a number (1 through 12) according to the involved spinal region: T, thoracic (T1–T12) and L, lumbar (L1–L5) in the present system.
All C-type displacement injuries and the subtype B2 (ligamentous disruption of the posterior tension band) involve motion segments by definition and thus, are located at the specified level of the involved motion segment. Motion segment injuries are coded by assigning letters and numbers of adjacent vertebral levels as described above, e.g., L1/L2 is the motion segment between vertebra L1 and L2.
Multi-segmental, multilevel, and any associated VB fractures should be specified separately. The most severe injury should be coded first followed by the additional injuries (C to A type in descending order). To ensure a comprehensive description of all injuries, all TL vertebrae and motion segments should be systematically examined and injuries classified from T1 to L5. Hence, the surgeon can easily identify injuries of adjacent vertebrae and motion segments, e.g., L1/L2–C2 (L2–A3).
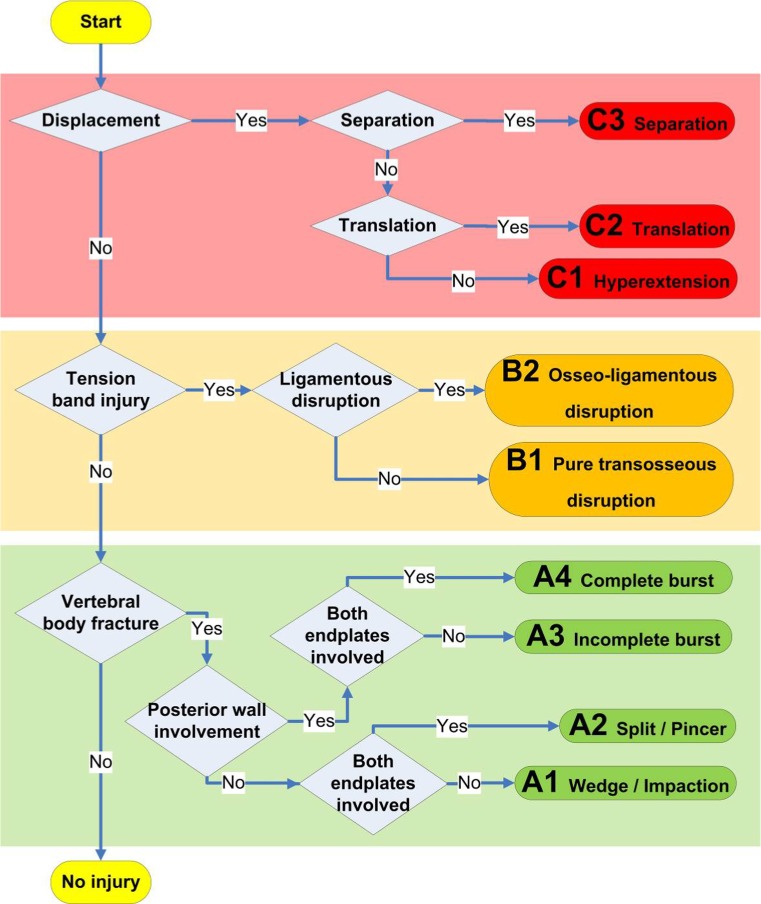
Diagnostic algorithm and final coding
A systematic diagnostic and coding approach is required to ensure that no injury is disregarded or misdiagnosed. The first step in the process is to ask which anatomical region is injured and secondly, which motion segment and/or VB is injured?
Four anatomical spine regions were defined including the TL region (T1–L5). For the TL spine in the present system, a diagnostic algorithm is proposed to guide the classification process (Fig. 5). Every VB and its motion segments should be assessed similarly to avoid misdiagnoses.
Fig. 5.
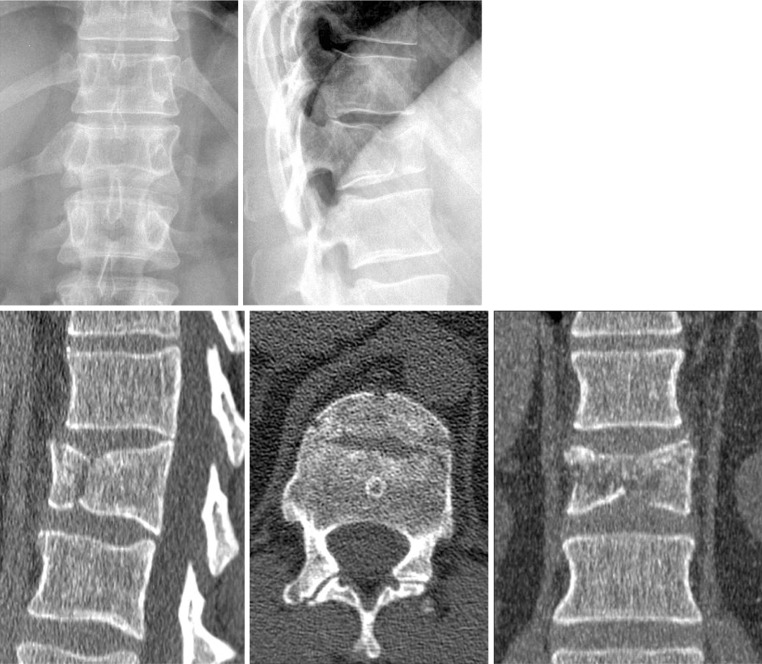
Case example of a wedge/impaction fracture (A1). Code: L1–A1 [upper row conventional radiographs in AP (left) and lateral (right) views of the TL spine centered on the L1-type-A1 injury, lower row corresponding CT scans with sagittal (left), axial (middle), and coronal (right) reconstructions of L1]
The first main question to be asked is: are there any signs of displacement? If yes, then a type-C injury is diagnosed. In the case of signs of separation, a subtype C3 is coded; alternately, signs of translation should be looked for. If these signs are observed, a subtype C2 is coded. Only signs of hyperextension lead to a subtype C1 coding.
The second main question addresses: is there a tension band injury? If yes, then a type-B injury is diagnosed. In case of a classic “Chance” type fracture that involves a three-column bony tension failure, a subtype B1 is coded.
Any motion segment with negative answers to these first two questions will be considered uninjured. The third and last main question applies to a vertebral body: is there a VB fracture? If yes, then the posterior wall should initially be examined for signs of involvement, which would indicate a VB burst fracture; a subtype A4 coding will be made if both endplates of the vertebra are involved, otherwise the fracture has a subtype A3 coding. Without posterior wall involvement, a subtype A2 coding is made if both endplates of the vertebra are involved; otherwise the vertebra has a subtype A1 fracture.
Clinical case examples
A number of representative case examples are presented. Images are chosen for the purpose of outlining the decision-making process and application of the TL classification system.
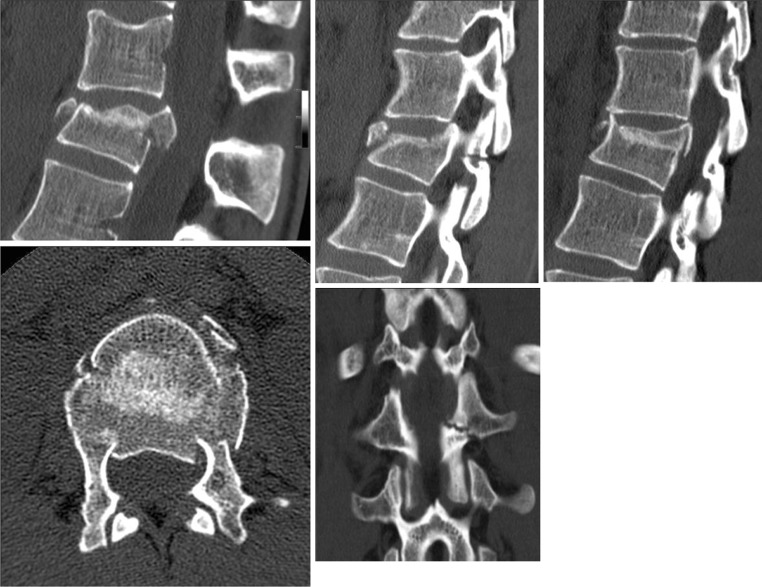
Case example 1: wedge/impaction fracture (A1)
This is an example of an L1-type-A1 fracture (Fig. 6). The fracture is characterized by a compressed superior endplate in the anterior third of the VB resulting in minimal wedging. The anteroposterior (AP) and lateral alignment of the TL spine is preserved, there is no displacement or translation, and the posterior elements are intact. The posterior wall of the L1 vertebra remains intact without any height loss. The axial CT shows several fracture lines. There is no soft tissue swelling or hematoma. Note that the CT reconstructions show a Schmorl’s node of the L2 upper endplate adjacent to the acute injury of L1.
Fig. 6.
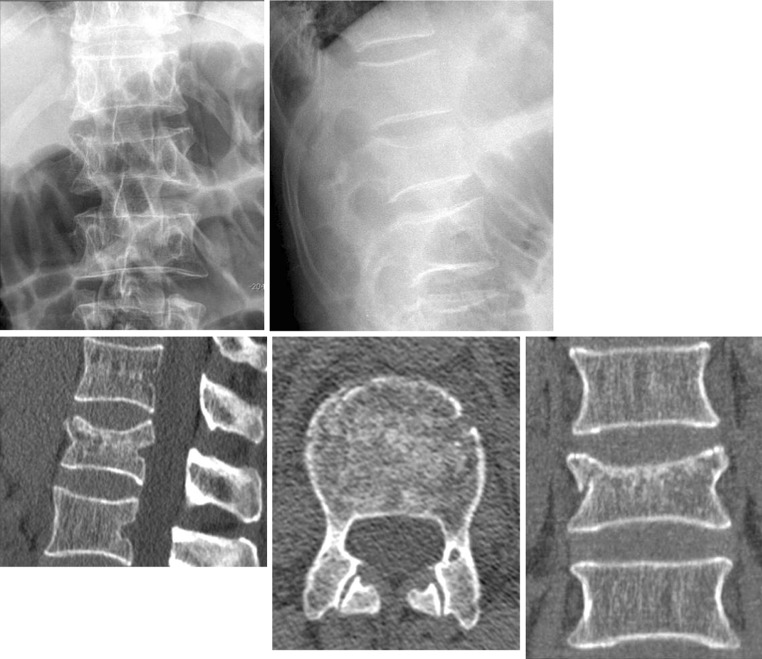
Example of a split/pincer fracture (A2). Code: T12–A2 [upper row conventional radiographs in AP (left) and lateral (right) views of the TL spine centered on T12 with a type A2 (split/pincer fracture), lower row corresponding CT scans with sagittal (left), axial (middle), and coronal (right) reconstructions of the T12 injury]
Case example 2: split/pincer fracture (A2)
This case is classified as a T12 split/pincer fracture subtype A2 (Fig. 7). The correct diagnosis is obtained following the treatment algorithm, if a split fracture can be appreciated in conventional radiographs in the AP or lateral view. There is slight wedging associated with the injury and a fracture line extends into both endplates of T12. At the same time, tension band injury has to be excluded in this case with congruent facet joints of T11/T12 and T12/L1 without signs of subluxation. The posterior and anterior wall alignment of VBs T11–L2 is unremarkable. There are no marked soft tissue swelling or other indirect signs of posterior ligamentous injury in the CT reconstructions. The CT images confirm involvement of both endplates without any involvement of the posterior wall. A coronal split is the dominant morphologic feature of this fracture and can be seen in all three planes. The absence of posterior wall involvement is what distinguishes an A2 (split/pincer) from an A4 (complete burst) fracture, despite some fragmentation and impression of both endplates seen in the coronal reconstruction below.
Fig. 7.
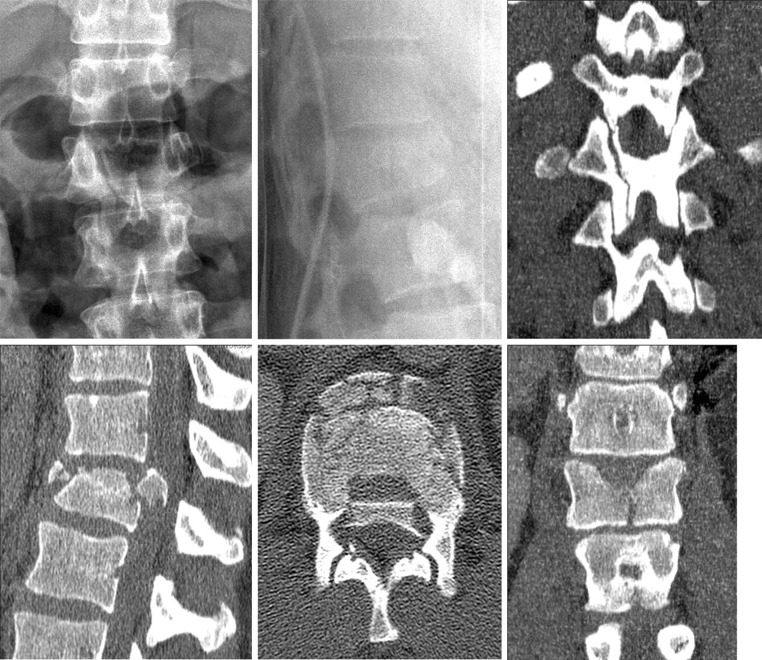
Example of an incomplete burst fracture (A3). Code: L1–A3 [upper row conventional radiographs in AP (left) and lateral (right) views of the TL spine centered on L1, lower row corresponding CT scans with sagittal (left), axial (middle), and coronal (right) reconstructions of the L1 incomplete burst fracture]
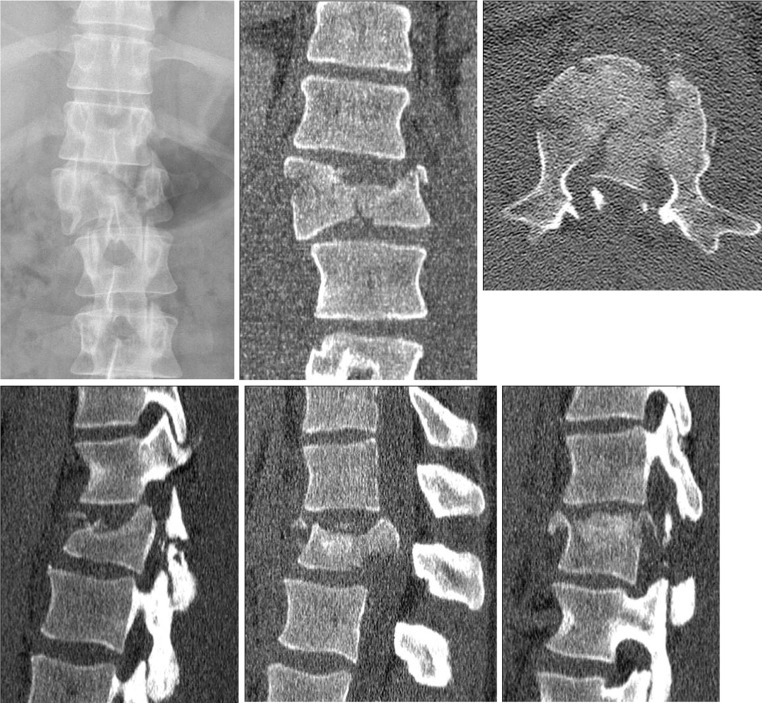
Case example 3: incomplete burst fracture (A3)
The main radiographic features of incomplete burst fractures are the presence of VB compression affecting only one endplate, and with posterior wall involvement. Fragmented upper endplates, height loss and/or VB wedging with fissures or retropulsed bony fragments into the posterior wall with spinal canal encroachment are commonly seen. There is no failure of the posterior tension band, despite there often being a vertical split fracture through the posterior arch or lamina.
Conventional AP (left) and lateral (right) radiographic views of the TL spine centered on L1 show an A3-type incomplete burst fracture (Fig. 8). The AP view demonstrates a height loss of the VB with respect to the adjacent intact vertebrae. In addition, there is minor widening of the upper half of the VB. The lateral view shows some wedging of L1. The facet joints and other posterior elements remain intact. CT reconstructions demonstrate the incomplete burst fracture with height loss, widening, and slight spinal canal narrowing. Of note, this case has a prominent exit of the basi-vertebral veins that can be seen as a single large aperture at the surface of the posterior wall in every VB in the sagittal reconstructions, which should not be mistaken for a fracture. The lower half of the VB and posterior elements is not injured.
Fig. 8.
Example of a complete burst fracture (A4). Code: T12–A4 [upper row conventional radiographs in AP (left) and lateral (middle) views of the TL spine centered on T12 with a type A4 (complete burst fracture), with a coronal CT reconstruction (right) of the posterior arch showing a vertical split, lower row corresponding CT scans with sagittal (left), axial (middle), and coronal (right) reconstructions of the T12-type-A4 injury]
Case example 4: complete burst fracture (A4)
Complete burst fractures are differentiated from incomplete fractures by the involvement of both endplates, a clinically relevant distinction that may considerably impact treatment decisions. The other radiographic characteristics remain similar to incomplete fractures, e.g., posterior wall involvement, spinal canal encroachment, and an intact posterior tension band. The degree of fragmentation, height loss, and kyphotic deformity may vary and also depends on the fracture location.
Conventional AP and lateral radiographs show a subtype A4 fracture of T12 with a coronal CT reconstruction of the posterior arch showing a vertical split (Fig. 9). Sagittal and axial CTs further support this classification. The degree of fragmentation is more pronounced than in the previously illustrated A3 subtype. The retropulsed bone fragment causes considerable spinal canal narrowing, and both endplates are affected as seen best on the coronal reconstruction of the VB.
Fig. 9.
Example of a trans-osseous disruption of a tension band injury (B1). Code: L1–B1 [upper row sagittal CT reconstructions of a pure trans-osseous disruption of tension band injury (B1) showing the extension of the fracture line through both pedicles (left and right images) and the L1 vertebral body (middle), lower scale-up of images above]
Case example 5: trans-osseous disruption of tension band injury (B1)
This case illustrates a subtype B1 injury at T11 and is defined as a monosegmental pure osseous failure of the posterior tension band (Fig. 10). Pure trans-osseous tension band failure is less common than ligamentous posterior tension band failure. The sagittal CT reconstruction shows a horizontal split through the spinous process of T11.
Fig. 10.
Example of an osseo-ligamentous disruption of a tension band injury (B2). Code: T12/L1–B2 (L1–A3) [upper row CT reconstructions of ligamentous disruption at the T12/L1 motion segment (left). Additional osseous component with left-sided horizontal facet fracture (middle) as well as right-sided facet joint incongruence with subluxation (right), lower row axial CT cut through the L1-type-A3 vertebral body fracture (left). Coronal reconstructions show the left-sided facet fracture extending through the pars interarticularis (middle)]
Case example 6: ligamentous disruption of tension band injury (B2)
This case has a type-B injury at the T12/L1 motion segment, defined as having a failure of tension band without displacement (Fig. 11). A VB fracture is also diagnosed and should be specified in the code separately. Subtype B2 lesions consist of ligamentous disruptions of the PLC with or without osseous involvement (e.g., avulsion fractures) causing posterior tension band failure. Essential components of a tension band injury can be identified on CT reconstructions. First of all, there is marked widening of the interspinous distance between T12 and L1 vertebrae and secondly, there is bilateral facet joint incongruence and widening, in conjunction with a horizontal left-sided facet fracture. The L1 VB fracture is a subtype A3 (incomplete burst fracture).
Fig. 11.
Example of a hyperextension injury (C1). Code: T12–C1 [upper row conventional radiographs of lateral (left) and AP (right) views of the TL spine centered on T12 with a type-C1 hyperextension injury. Note the bridging anterior ossification as commonly seen in DISH Syndrome, lower row corresponding CT scans with sagittal (left), coronal (middle), and axial reconstructions through the vertebral body of T12 showing the proximal and distal spinal column in a hyperextended position]
Case example 7: hyperextension injury (C1)
In the case of displacement in any plane, a type-C injury is diagnosed. This example illustrates a C1-subtype injury at T12, characterized by a disruption of the T12 vertebra causing a hyperextension deformity position. Note the bridging anterior ossification typical of diffuse idiopathic skeletal hyperostosis (DISH) as these injuries are most commonly seen in patients with ankylosing spine conditions.
Case example 8: translation injury (C2)
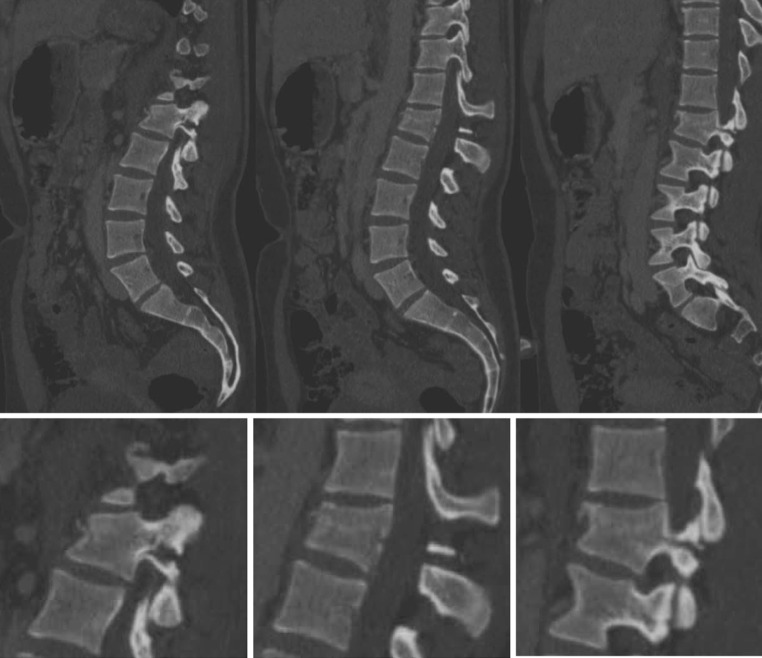
Translation of the spinal column in any direction implies a circumferential disruption of osseous and/or disco-ligamentous structures. Along with the similar compression and flexion–distractive forces that are seen with type-A and B injuries, respectively, translation injuries may also result from rotational forces with signs of an associated shear injury to the vertebral body, fracture or avulsion of transverse processes, or injury to other non-spinal structures such as ribs or soft tissues. This example shows a T12/L1, subtype C2 translational injury illustrated on the AP radiograph and on CT images, which show marked offset of the lateral VB cortices (Fig. 12). An associated subtype A4 complete burst fracture is diagnosed at the L1 level with a large posterior wall retropulsed fragment into the spinal canal causing significant spinal canal encroachment. Corresponding sagittal CT reconstructions confirm failure of the anterior and posterior column with bilateral facet fractures.
Fig. 12.
Example of a translation injury (C2). Code: T12/L1–C2 (L1–A4) [upper row translational injury as seen on an AP radiograph of a T12/L1 subtype C2 with L1 subtype A4 injury (left). Coronal (middle) and axial (right) CT cuts show marked set-off of the lateral vertebral body walls and a burst fracture with a large retropulsed bony posterior wall fragment into the spinal canal causing significant spinal canal encroachment at the L1 level, lower row corresponding sagittal CT reconstructions at the left facet joint (left), mid-sagittal (middle), and right facet joint (right). Failure of the anterior as well as posterior column with bilateral facet fractures]
Case example 9: separation injury (C3)
Separation (subtype C3) injuries of the spinal column represent the most severe unstable injuries within the classification scheme. Sagittal, coronal, and axial CT images show a T6/7 C3 injury (Fig. 13). The spinal column is completely separated as seen in all three images. In addition, there are several air inclusions within the spinal canal and surrounding soft tissues secondary to associated pulmonary injury.
Fig. 13.
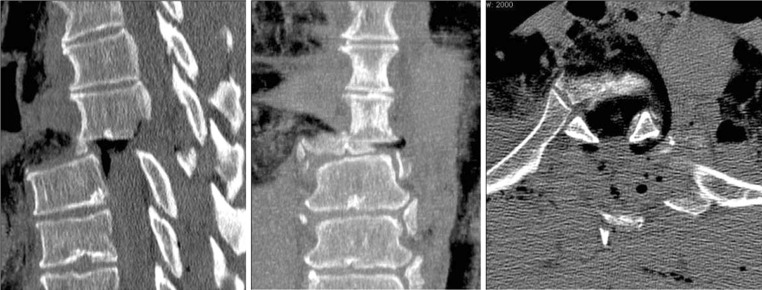
Example of separation injury (C3). Code: T6/T7–C3 [sagittal (left), coronal (middle), and axial (right) CT cuts of a T6/T7 C3 injury of the thoracic spine. The spinal column is completely separated as seen in all three images]
Discussion
Although many spinal fracture classifications and severity measures have been developed [9] there is still no universally accepted system. No single classification system has been able to fully describe the injury severity, pathogenesis, and biomechanical inciting forces while addressing all clinical, neurological and radiological characteristics [10].
At present, there are no guidelines published for the development of spinal injury classifications [11]. In line with the AO philosophy and other successfully validated long-bone injury classifications [12], we believe that the characterization and categorization of TL injuries should primarily be based on morphological characteristics that can be reliably identified on diagnostic images. For this reason, the newly presented spine TL injury classification based on the older Magerl AO classification provides clear descriptions regarding the injury characteristics of the vertebral column and is primarily based on the assessment of multiplanar CT scans, which are nowadays routinely performed for the diagnostic workup at most trauma centers [13].
The AOSCG was established in 2007. The objective was to develop a system for the whole spinal column by way of systematic critical analysis. It was decided to start with the thoracolumbar region and to validation of the 1994 Magerl Classification. The group was formed by spine trauma surgeons from various geographical and clinical backgrounds to facilitate the identification of cross-cultural differences in training and understanding of basic clinical concepts and definitions.
A clear distinction has to be made between severity measures, treatment algorithms, and classification systems as recently outlined by van Middendorp et al. [11]. Other medical prognostic factors, co-morbidities, and neurological deficits also have an impact on treatment decisions, but need to be classified separately and thus are not integrated into the present classification system. Not only the imaging modalities but also treatment methods for TL injuries continue to change over time. Previous classification schemes have been criticized for being either too simple or overly complex and insufficiently reproducible. Both the Denis [3] and the Magerl AO classification systems [14] have been used extensively during the past decades but had only moderate reliability and repeatability according to Wood et al. [4]. A tendency for well-trained spine surgeons to classify the same fracture differently after repeated testing caused some concern in that study [4]. On the other hand, as a validation tool, the study was considered limited by the lack in the basic understanding and differentiation between Magerl AO type-A (compression) and obvious rotational (type C) injuries among some of the 19 participating raters [6]. Independent studies found inter-observer reliability Kappa coefficients of 0.33 [15] and 0.62 [5] for the three main injury types (A, B, C) only.
Diagnostic imaging modalities and varying image quality can have a major impact on a spine trauma classification and result in showing different degree of detail with regard to osseous and/or disco-ligamentous structures involved in the specific injury. While earlier classification systems such as those of Böhler [16], Nicoll [17], or Watson-Jones [18] relied on plain radiographs only, ongoing imaging advances have improved our ability to detect and outline the osseo-ligamentous morphology of spinal injuries [13]. In some cases, accurate classification is possible with the CT scans or plain radiographs only. Other situations, such as with primary disco-ligamentous injuries, may require additional imaging such as MRI to appreciate the full extent of the injury. Therefore, MRI images were considered as supplementary modality in this study. In fact, MRI images show a significantly higher sensitivity in identifying bony lesions and more importantly, are able to clearly distinguish posterior complex or ligamentous lesions in comparison to CT images [19]. In addition, a fat-suppressed T2-weighted sagittal sequence of an MRI is considered a highly sensitive, specific, and accurate method for evaluating PLC injuries [20].
The final classification session demonstrated reliability of this revised classification system; with Kappa coefficients above 0.70 for all fracture types (A, B, C) and the subtypes of type A. Such a level of agreement is rarely obtained when classifying fractures [21] including spine injuries [5, 15], and was considered acceptable at this stage of the development process. From a clinical standpoint, the evaluation of ligamentous injuries can be a major challenge for treating physicians and is an essential component to reliably defining spinal instability. Several authors have emphasized this difficulty and the importance of avoiding the complications resulting from missed posterior ligamentous injuries, which can cause painful residual deformity secondary to a posterior tension band failure [15, 22]. One of the main goals of the revised TL spine classification was to rearrange the classification categories and injury descriptions in a clinically relevant manner that emphasizes how type-A injuries can be part of the more severe B- and C-type lesions and may influence the treatment of these injuries. This system of combining types B and C with the basic type-A subtypes also eliminates the need for complicated subgroupings that add a degree of complexity to the classification system which is likely to exceed its clinical relevance. While almost all patients with type-A injuries are likely to be identified by spine surgeons, a proportion of patients with either B- or C-type injuries will be misdiagnosed from plain radiographs and CT scans alone. Our results suggest that the rate of incorrect classification for type-C injuries is limited to about 3 % misidentified as type-A fractures, while another 13–25 % was misidentified as type-B injuries, the latter of which would probably have less important clinical consequences. The rate of missed type-B TL spine lesions has been reported to be as high as 29 % [22] and remains a matter of concern. Our results showed a rate of type-B lesion misclassification ranging between 2 and 16 % among our surgeons. The reliability in our final assessment for type-B injuries is high in comparison to previously published reports [22]. It seems that clear definitions and separate coding of the VB fractures (subtypes of type A) in our system may help to overcome this problem. Median classification accuracies were approximately 90 % for all categories. While this may be considered high, the clinical consequence of fracture misclassification for any patient in terms of treatment and outcome cannot yet be fully appreciated until clinical studies using the classification are implemented.
In 2005, a group of spine trauma surgeons organized as Spine Trauma Study Group (STSG) started publishing a series of papers regarding the development and initial assessment of a new classification system and severity score, the so-called thoracolumbar injury severity score (TLISS) [23, 24]. After a revision process, this ultimately resulted in TLICS (thoracolumbar injury classification and severity score), which was based on three major variables derived from imaging studies and clinical evaluation: (1) the presumed mechanism of injury based on fracture morphology; (2) the integrity of the PLC; and (3) the neurologic status of the patient [24]. Specific point values within each category were assigned according to the severity of injury. Based on the final score, a treatment algorithm and proposal for non-operative or operative treatment is made [24–26].
To date, the TLISS/TLICS has neither been used nor tested independently in larger clinical case series. Uncertainty also remains as to whether the final score is adequately formulated. To date, reliability and validity tests have only been published by STSG members [28, 29] or reports with a limited number of pre-selected clinical cases [28]. In the future, incorporating a validated morphological classification as proposed in this study may enhance the clinical usefulness of injury severity scoring systems.
Within our group, considerable emphasis was placed on developing appropriate descriptions and graphical illustrations that established specific morphologic injury characteristics that would reliably distinguish one injury subgroup from another, e.g., osseous vs. ligamentous tension band injuries (B type). Another example involves a consensus decision to reserve a separate subcategory for complete burst fractures (A4 subtype), in which both endplates were fractured, in addition to incomplete burst fractures (A3 subtype) in which only one endplate is involved. This distinction is important and has significant implications for further treatment [30].
The STSG concept suggested multiple clinical qualifiers such as comorbidities and individual situations that cannot be objectively weighted in a point value [26]. These qualifiers still, however, need to be assessed on an independent basis for every individual by the health care provider or treating physician during the evaluation, which was beyond the scope of this development phase. For this reason, we did not include neurological status as part of this revised AO spine injury classification system. Nevertheless, the neurological status is absolutely relevant for a complete assessment in terms of the patient’s functional status and injury prognosis and may be incorporated during subsequent development phases. In the future, our scheme can therefore be combined with such tools to establish a spinal injury severity scoring system, such as the TLICS.
In general, the main concern of contemporary classification systems for TL injuries is that they are limited either by excessive complexity or the lack of inclusiveness [10, 27]. Many original reports describing common TL injury classifications lack a rigorous scientific foundation [10]. This revised AO spine injury classification represents an improvement with regard to a more structured, less complex classification scheme that still takes into account the inherent variability of spinal column injuries and every major mode of failure.
This system is the outcome of a major, time-consuming scientific process to fulfill the requirements set by the AOSCG. There are several distinctive features that set it apart from previous injury classifications [9]:
AOSCG
In contrast to individual researchers, clinicians or self-selected working groups, the AOSCG is composed of a core membership of experienced spine surgeons nominated from various geographical and cultural environments. This facilitates the exchange of cross-cultural differences in training and understanding of basic clinical concepts and definitions.
Evidence-based approach vs. “eminence-based” decisions
All stages and steps of this study followed a well-defined methodological pathway [8]. This classification system is based on the first phase of a concept with sound statistical validation process including three clearly defined consecutive phases as described previously. Implementation of all three steps will guarantee a truly evidence-based approach toward an internationally accepted and usable classification system.
Study administration and monitoring
The guidance of clinical expertise and surgeons’ input was provided by an independent professional research organization (AOCID). This process involved support in terms of the administration of regular conferences, meetings and classification sessions, provision of an anonymized, large consecutive case series of TL injuries, data distribution, and continuous study monitoring, all of which represents a means of quality control by an independent third party.
Expertise in fracture classification
The AOSCG can build on over 50 years of experience in fracture classification by the AO Foundation including the highly influential Magerl AO scheme for spinal injuries and a growing community of spine surgeons—an ideal platform of valuable feedback of members throughout the world.
The revised AO spine TL injury classification system is clinically relevant according to the outcome of an objectively guided international consensus reached during a first phase of development. Final phase 1 evaluation data demonstrated that it is reasonably reliable and accurate. At this stage of development, the predictive clinical value of the proposed system will require follow-up evaluation sessions and documentation performed by a large number of surgeons from different countries.
This system is a compromise, as are all classification systems. Many spine surgeons are likely to question its lack of detail for their purposes, or state that it does not provide them the immediate clinical application they seek. We also understand that the similarities and differences with the original Magerl AO scheme may lead to confusion by those accustomed to this scheme. This is particularly true with respect to the thoracolumbar spine, where we felt the existing Magerl AO classification has the greatest applicability and therefore required the least revision. We believe, however, that this system is a valuable tool for documenting spine injuries and can be more easily applied, with some variation, to the remainder of the spine. It will therefore help to start a process by which more valid clinical research on injuries throughout the entire spine can be carried out. This system will continue to evolve with increasing validity and clinical relevance during an active process of assessment, reassessment, and refinement, with a view toward integrating clinical factors that have a direct impact on treatment. The evaluation and validation of this system is an ongoing process. Only a global team effort will achieve the final goal of a clinically relevant, comprehensive spine injury classification, which can potentially be incorporated into more advanced spinal injury severity scoring systems in the future.
Acknowledgments
The spine injury classification project was funded by the AO Foundation and its AOSpine Specialty. The authors would like to greatly thank Mary Anne Smith (AOSpine International) for the administrative support as well as Jecca Reichmuth and her colleagues at AO Education (Publishing) for the preparation of illustrations. The authors are grateful to all surgeons (as listed below in alphabetic order) who participated and provided fruitful support in any of the successive review meeting or classification sessions : Anderson P.A., USA; Bellabarba C., USA; Blauth M., Austria; Cisneros F.A., Mexico; Dai L.-Y., China; Hadley M., USA; Magerl F., Austria; Marré B., Chile; Matta J., Colombia; Oner C., The Netherlands; Reinhold M., Austria; Schnake K., Germany; van Middendorp J., The Netherlands; Zhou F., China. We would also like to greatly thank Melissa Wilhelmi for editing support of this manuscript.
Conflict of interest
None.
References
- 1.Holdsworth F. Fractures, dislocations, and fracture-dislocations of the spine. J Bone Jt Surg (Am) 1970;52:1534–1551. [PubMed] [Google Scholar]
- 2.Whitesides TE., Jr Traumatic kyphosis of the thoracolumbar spine. Clin Orthop Relat Res. 1977;128:78–92. [PubMed] [Google Scholar]
- 3.Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine. 1983;8:817–831. doi: 10.1097/00007632-198311000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Wood KB, Khanna G, Vaccaro AR, Arnold PM, Harris MB, Mehbod AA. Assessment of two thoracolumbar fracture classification systems as used by multiple surgeons. J Bone Jt Surg (Am) 2005;87:1423–1429. doi: 10.2106/JBJS.C.01530. [DOI] [PubMed] [Google Scholar]
- 5.Oner FC, Ramos LM, Simmermacher RK, Kingma PT, Diekerhof CH, Dhert WJ, Verbout AJ. Classification of thoracic and lumbar spine fractures: problems of reproducibility. A study of 53 patients using CT and MRI. Eur Spine J. 2002;11:235–245. doi: 10.1007/s00586-001-0364-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aebi M. Classification of thoracolumbar fractures and dislocations. Eur Spine J. 2010;19:S2–S7. doi: 10.1007/s00586-009-1114-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Audigé L. Development and validation of a new generation for spine injury classification. In: Chapman JR, Dettori JR, Norvell DC, editors. Spine classification and severity measures. 1. Stuttgart: Thieme; 2009. pp. 503–507. [Google Scholar]
- 8.Audigé L, Bhandari M, Hanson B, Kellam J. A concept for the validation of fracture classifications. J Orthop Trauma. 2005;19:404–409. doi: 10.1097/01.bot.0000155310.04886.37. [DOI] [PubMed] [Google Scholar]
- 9.Chapman JR, Dettori JR, Norvell DC. Spine classifications and severity measures. Stuttgart: Thieme; 2009. [Google Scholar]
- 10.Mirza SK, Mirza AJ, Chapman JR, Anderson PA. Classifications of thoracic and lumbar fractures: rationale and supporting data. J Am Acad Orthop Surg. 2002;10:364–377. doi: 10.5435/00124635-200209000-00008. [DOI] [PubMed] [Google Scholar]
- 11.van Middendorp JJ, Audigé L, Hanson B, Chapman JR, Hosman AJ. What should an ideal spinal injury classification system consist of? A methodological review and conceptual proposal for future classifications. Eur Spine J. 2010;19:1238–1249. doi: 10.1007/s00586-010-1415-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Slongo T, Audigé L, AO Pediatric Classification Group Fracture and dislocation classification compendium for children: the AO pediatric comprehensive classification of long bone fractures (PCCF) J Orthop Trauma. 2007;21:S135–S160. doi: 10.1097/00005131-200711101-00020. [DOI] [PubMed] [Google Scholar]
- 13.Diaz JJ, Jr, Cullinane DC, Altman DT, et al. Practice management guidelines for the screening of thoracolumbar spine fracture. J Trauma. 2007;63:709–718. doi: 10.1097/TA.0b013e318142d2db. [DOI] [PubMed] [Google Scholar]
- 14.Magerl F, Aebi M, Gertzbein SD, Harms J, Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3:184–201. doi: 10.1007/BF02221591. [DOI] [PubMed] [Google Scholar]
- 15.Blauth M, Bastian L, Knop C, Lange U, Tusch G. Inter-observer reliability in the classification of thoraco-lumbar spinal injuries. Orthopade. 1999;28:662–681. doi: 10.1007/s001320050397. [DOI] [PubMed] [Google Scholar]
- 16.Böhler L. Die Technik der Knochenbruchbehandlung. Wien: Maudrich; 1951. [Google Scholar]
- 17.Nicoll EA. Fractures of the dorso-lumbar spine. J Bone Jt Surg (Br) 1949;31:376–394. [PubMed] [Google Scholar]
- 18.Watson-Jones R. The results of postural reduction of fractures of the spine. J Bone Jt Surg (Am) 1938;20:567–586. [Google Scholar]
- 19.Grunhagen J, Egbers HJ, Heller M, Reuter M. Comparison of spine injuries by means of CT and MRI according to the classification of Magerl. Rofo. 2005;177:828–834. doi: 10.1055/s-2005-858198. [DOI] [PubMed] [Google Scholar]
- 20.Lee HM, Kim HS, Kim DJ, Suk KS, Park JO, Kim NH. Reliability of magnetic resonance imaging in detecting posterior ligament complex injury in thoracolumbar spinal fractures. Spine. 2000;25:2079–2084. doi: 10.1097/00007632-200008150-00012. [DOI] [PubMed] [Google Scholar]
- 21.Audigé L, Bhandari M, Kellam J. How reliable are reliability studies of fracture classifications? A systematic review of their methodologies. Acta Orthop Scand. 2004;75:184–194. doi: 10.1080/00016470412331294445. [DOI] [PubMed] [Google Scholar]
- 22.Schnake KJ, Von Scotti F, Haas NP, Kandziora F. Type-B injuries of the thoracolumbar spine: misinterpretations of the integrity of the posterior ligament complex using radiologic diagnostics. Unfallchirurg. 2008;111:977–984. doi: 10.1007/s00113-008-1503-z. [DOI] [PubMed] [Google Scholar]
- 23.Vaccaro AR, Lehman RA, Jr, Hurlbert RJ, et al. A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine. 2005;30:2325–2333. doi: 10.1097/01.brs.0000182986.43345.cb. [DOI] [PubMed] [Google Scholar]
- 24.Lee JY, Vaccaro AR, Lim MR, et al. Thoracolumbar injury classification and severity score: a new paradigm for the treatment of thoracolumbar spine trauma. J Orthop Sci. 2005;10:671–675. doi: 10.1007/s00776-005-0956-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schweitzer KM, Jr, Vaccaro AR, Lee JY, Grauer JN. Confusion regarding mechanisms of injury in the setting of thoracolumbar spinal trauma: a survey of The Spine Trauma Study Group (STSG) J Spinal Disord Tech. 2006;19:528–530. doi: 10.1097/01.bsd.0000211219.28566.d0. [DOI] [PubMed] [Google Scholar]
- 26.Vaccaro AR, Zeiller SC, Hulbert RJ, et al. The thoracolumbar injury severity score: a proposed treatment algorithm. J Spinal Disord Tech. 2005;18:209–215. [PubMed] [Google Scholar]
- 27.Whang PG, Vaccaro AR, Poelstra KA, et al. The influence of fracture mechanism and morphology on the reliability and validity of two novel thoracolumbar injury classification systems. Spine. 2007;32:791–795. doi: 10.1097/01.brs.0000258882.96011.47. [DOI] [PubMed] [Google Scholar]
- 28.Patel AA, Vaccaro AR, Albert TJ, et al. The adoption of a new classification system: time-dependent variation in interobserver reliability of the thoracolumbar injury severity score classification system. Spine. 2007;32:E105–E110. doi: 10.1097/01.brs.0000254107.57551.8a. [DOI] [PubMed] [Google Scholar]
- 29.Raja RY, Fisher C, Wilsey J, et al. Agreement between orthopedic surgeons and neurosurgeons regarding a new algorithm for the treatment of thoracolumbar injuries: a multicenter reliability study. J Spinal Disord Tech. 2006;19:477–482. doi: 10.1097/01.bsd.0000211237.14211.21. [DOI] [PubMed] [Google Scholar]
- 30.Reinhold M, Knop C, Beisse R, et al. Operative treatment of traumatic fractures of the thorax and lumbar spine. Part II: surgical treatment and radiological findings. Unfallchirurg. 2009;112:149–167. doi: 10.1007/s00113-008-1538-1. [DOI] [PubMed] [Google Scholar]